INNOPRAN (propranolol hydrochloride 120 mg) Dailymed
Generic: propranolol hydrochloride
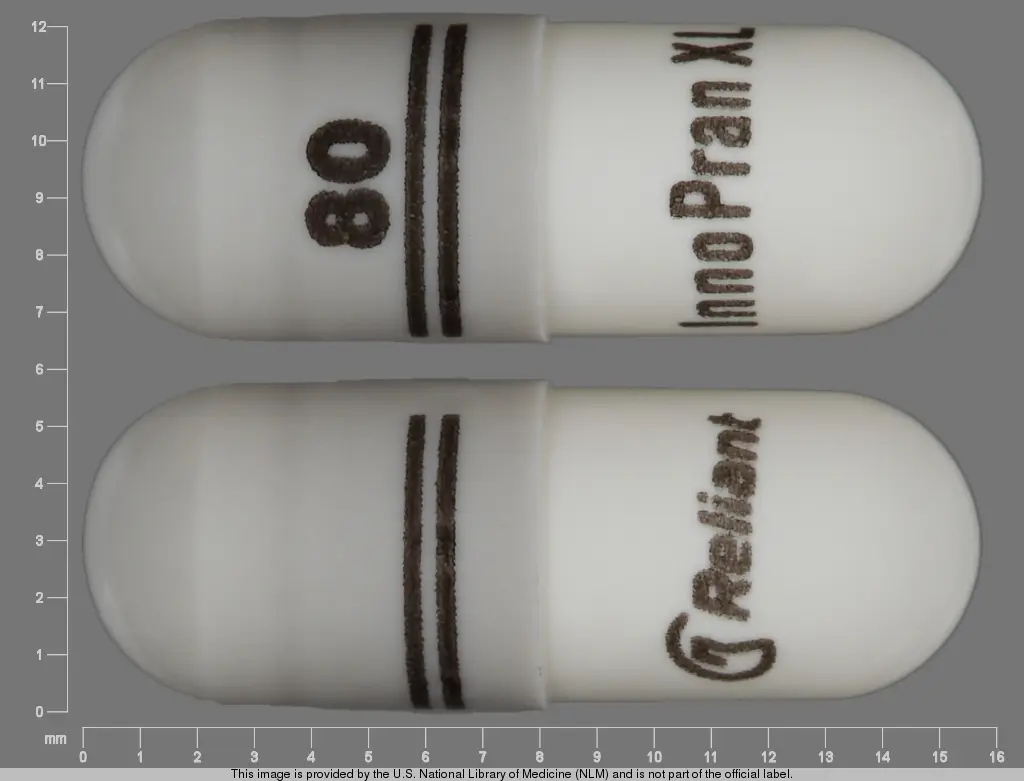
IMPRINT: 80 INNOPRAN XL
SHAPE: capsule
COLOR: grey
All Imprints
propranolol hydrochloride 80 mg - 80 innopran xl capsule grey
propranolol hydrochloride 120 mg - 120 innopran xl capsule grey
Go PRO for all pill images
Description
INNOPRAN XL (propranolol hydrochloride) is a nonselective, beta-adrenergic receptor-blocking agent for oral administration, available as an extended release product. INNOPRAN XL is available as 80-mg and 120-mg capsules which contain sustained-release beads. Each of the beads contains propranolol hydrochloride and is coated with dual membranes. These membranes are designed to retard release of propranolol hydrochloride for several hours after ingestion followed by the sustained release of propranolol.
The active ingredient in INNOPRAN XL is a synthetic beta-adrenergic receptor-blocking agent chemically described as 1-(Isopropylamino)-3-(1-naphthyloxy)-2-propanol hydrochloride. Its structural formula is:
![]()
Propranolol hydrochloride is a stable, white, crystalline solid, which is readily soluble in water and ethanol. Its molecular weight is 295.81. Each capsule for oral administration contains sugar spheres, ethylcellulose, povidone, hypromellose phthalate, diethyl phthalate, hypromellose, polyethylene glycol, gelatin, titanium dioxide, and black iron oxide. In addition, INNOPRAN XL 120 mg capsules contain yellow iron oxide.
Clinical Pharmacology
General
Propranolol is a nonselective, beta-adrenergic receptor-blocking agent possessing no other autonomic nervous system activity. It specifically competes with beta-adrenergic receptor-stimulating agents for available receptor sites. When access to beta-receptor sites is blocked by propranolol, chronotropic, inotropic, and vasodilator responses to beta-adrenergic stimulation are decreased proportionately. At dosages greater than required for beta blockade, propranolol also exerts a quinidine-like or anesthetic-like membrane action, which affects the cardiac action potential. The significance of the membrane action in the treatment of arrhythmias is uncertain.
Mechanism of Action
The mechanism of the antihypertensive effect of propranolol has not been established. Among factors that contribute to the antihypertensive action are: (1) decreased cardiac output, (2) inhibition of renin release by the kidneys, and (3) diminution of tonic sympathetic nerve outflow from vasomotor centers in the brain. Although total peripheral resistance may increase initially, it readjusts to or below the pretreatment level with chronic use of propranolol. Effects of propranolol on plasma volume appear to be minor and somewhat variable.
Pharmacokinetics and Drug Metabolism
Absorption
Propranolol is highly lipophilic and is almost completely absorbed after oral administration. However, it undergoes high first-pass metabolism by the liver and on average, only about 25% of propranolol reaches the systemic circulation.
A single-dose, food-effect study in 36 healthy subjects showed that a high fat meal administered with INNOPRAN XL at 10 p.m., increased the lag time from 3 to 5 hours and the time to reach the maximum concentration from 11.5 to 15.4 hours, under fed conditions, with no effect on the AUC (see DOSAGE AND ADMINISTRATION).
Following multiple-dose administration of INNOPRAN XL at 10 p.m. under fasting conditions, the steady state lag time was between 4 and 5 hours and propranolol peak plasma concentrations were reached approximately 12 to 14 hours after dosing. Propranolol trough levels were achieved 24 to 27 hours after dosing, and persisted for 3 to 5 hours after the next dose. The elimination half-life of propranolol was approximately 8 hours.
The plasma levels of propranolol showed dose-proportional increases after single and multiple administration of 80-, 120-, and 160-mg of INNOPRAN XL.
At steady state, the bioavailability of a 160-mg dose of INNOPRAN XL and propranolol hydrochloride long-acting capsules did not differ significantly.
Distribution
Approximately 90% of circulating propranolol is bound to plasma proteins (albumin and alpha1 acid glycoprotein). The binding is enantiomer-selective. The S-isomer is preferentially bound to alpha1 glycoprotein and the R-isomer preferentially bound to albumin. The volume of distribution of propranolol is approximately 4 liters.
Metabolism and Elimination
Propranolol is extensively metabolized with most metabolites appearing in the urine. Propranolol is metabolized through 3 primary routes: Aromatic hydroxylation (mainly 4-hydroxylation), N-dealkylation followed by further side-chain oxidation, and direct glucuronidation. It has been estimated that the percentage contributions of these routes to total metabolism are 42%, 41%, and 17%, respectively, but with considerable variability between individuals. The 4 major metabolites are propranolol glucuronide, naphthyloxylactic acid, and glucuronic acid and sulfate conjugates of 4-hydroxy propranolol.
In vitro studies have indicated that the aromatic hydroxylation of propranolol is catalyzed mainly by polymorphic CYP2D6. Side-chain oxidation is mediated mainly by CYP1A2 and to some extent by CYP2D6. 4-hydroxy propranolol is a weak inhibitor of CYP2D6.
Propranolol is also a substrate for CYP2C19 and a substrate for the intestinal efflux transporter, p-glycoprotein (p-gp). Studies suggest however that p-gp is not dose-limiting for intestinal absorption of propranolol in the usual therapeutic dose range.
In healthy subjects, no difference was observed between CYP2D6 extensive metabolizers (EMs) and poor metabolizers (PMs) with respect to oral clearance or elimination half-life. Partial clearance to 4-hydroxy propranolol was significantly higher and to naphthyloxylactic acid was significantly lower in EMs than PMs.
Enantiomers
Of the 2 enantiomers of propranolol, the S-enantiomer blocks beta adrenergic receptors. In normal subjects receiving oral doses of racemic propranolol, S-enantiomer concentrations exceeded those of the R-enantiomer by 40 to 90% as a result of stereoselective hepatic metabolism.
Special Populations
Pediatric
The pharmacokinetics of INNOPRAN XL have not been investigated in patients younger than 18 years of age.
Geriatric
The pharmacokinetics of INNOPRAN XL have not been investigated in patients older than 65 years. In a study of 12 elderly (62 to 79 years old) and 12 young (25 to 33 years old) healthy subjects, the clearance of the S-enantiomer of propranolol was decreased in the elderly. Additionally, the half-lives of both R- and S-propranolol were prolonged in the elderly compared with the young (11 hours versus 5 hours).
Gender
In a dose-proportionality study, the pharmacokinetics of INNOPRAN XL were evaluated in 22 male and 14 female healthy volunteers. Following single doses under fasting conditions, the mean AUC and Cmax were about 49% and 16% higher for females across the dosage range. The mean elimination half-life was longer in females than in males (11 hours versus 7.5 hours).
Race
A study conducted in 12 white and 13 African-American male subjects taking propranolol showed, that at steady state, the clearance of R- and S-propranolol were about 76% and 53% higher in African-Americans than in whites, respectively.
Renal Insufficiency
The pharmacokinetics of INNOPRAN XL have not been evaluated in patients with renal insufficiency. In a study conducted in 5 patients with chronic renal failure, 6 patients on regular dialysis, and 5 healthy subjects, who received a single oral dose of 40 mg of propranolol, the peak plasma concentrations (Cmax) of propranolol in the chronic renal failure group were 2- to 3-fold higher (161¬Ī41 ng/mL) than those observed in the dialysis patients (47¬Ī9 ng/mL) and in the healthy subjects (26¬Ī1 ng/mL). Propranolol plasma clearance was also reduced in the patients with chronic renal failure.
Chronic renal failure has been associated with a decrease in drug metabolism via down regulation of hepatic cytochrome P450 activity.
Propranolol is not significantly dialyzable.
Hepatic Insufficiency
The pharmacokinetics of INNOPRAN XL have not been evaluated in patients with hepatic impairment. However, propranolol is extensively metabolized by the liver. In a study conducted in 7 patients with cirrhosis and 9 healthy subjects receiving 80-mg oral propranolol every 8 hours for 7 doses, the steady-state unbound propranolol concentration in patients with cirrhosis was increased 3-fold in comparison to controls. In cirrhosis, the half-life increased to 11 hours compared to 4 hours (see PRECAUTIONS).
Drug Interactions
Interactions with Substrates, Inhibitors or Inducers of Cytochrome P450 Enzymes
Because propranolol’s metabolism involves multiple pathways in the cytochrome P450 system (CYP2D6, 1A2, 2C19), administration of INNOPRAN XL with drugs that are metabolized by, or affect the activity (induction or inhibition) of one or more of these pathways may lead to clinically relevant drug interactions (see PRECAUTIONS, Drug Interactions).
Plasma propranolol levels may increase with acute alcohol consumption and decrease upon chronic alcohol use.
Blood levels and/or toxicity of propranolol may be increased by administration of INNOPRAN XL with substrates or inhibitors of CYP2D6, such as amiodarone, cimetidine, delavudin, fluoxetine, paroxetine, quinidine, and ritonavir. No interactions were observed with either ranitidine or lansoprazole.
Blood levels and/or toxicity of propranolol may be increased by administration of INNOPRAN XL with substrates or inhibitors of CYP1A2, such as imipramine, cimetidine, ciprofloxacin, fluvoxamine, isoniazid, ritonavir, theophylline, zileuton, zolmitriptan, and rizatriptan.
Blood levels and/or toxicity of propranolol may be increased by administration of INNOPRAN XL with substrates or inhibitors of CYP2C19, such as fluconazole, cimetidine, fluoxetine, fluvoxamine, teniposide, and tolbutamide. No interaction was observed with omeprazole.
Blood levels of propranolol may be decreased by administration of INNOPRAN XL with inducers such as rifampin. Cigarette smoking also induces hepatic metabolism and has been shown to increase up to 100% the clearance of propranolol, resulting in decreased plasma concentrations.
Cardiovascular Drugs
The concomitant administration of propranolol and propafenone increased propranolol average steady-state plasma concentrations (213%), AUC (113%), Cmax (83%), Tmax (55%), and T¬Ĺ (30%), and significantly decreased plasma levels of 4-hydroxy-propranolol. Co-administration of propranolol and propafenone did not produce any significant change in propafenone pharmacokinetics. While the therapeutic range for propranolol is wide, a reduction in dosage may be necessary during concomitant administration with propafenone.
The metabolism of propranolol is reduced by co-administration of quinidine, leading to a 2-to 3-fold increase in blood concentrations and greater degrees of clinical beta-blockade.
Concomitant administration of propranolol with lidocaine, bupivacaine or mepivacaine has been reported to decrease the clearance of these amide anesthetics significantly, resulting in higher serum concentrations of the anesthetic.
The mean Cmax and AUC of propranolol are increased respectively, by 50% and 30% by co-administration of nisoldipine and by 80% and 47%, by co-administration of nicardipine.
The mean Cmax and AUC of nifedipine are increased by 64% and 79%, respectively, by co-administration of propranolol.
Propranolol does not affect the pharmacokinetics of verapamil and norverapamil. Verapamil does not affect the pharmacokinetics of propranolol.
Non-Cardiovascular Drugs
Co-administration of propranolol with cimetidine, a non-specific CYP450 inhibitor, increased propranolol concentrations by about 40%. Co-administration with aluminum hydroxide gel (1,200 mg) resulted in a 50% decrease in propranolol concentrations.
Co-administration of metoclopramide with propranolol did not have a significant effect on propranolol’s pharmacokinetics.
Benzodiazepines
Propranolol can inhibit the metabolism of diazepam, resulting in increased concentrations of diazepam and its metabolites. Diazepam does not alter the pharmacokinetics of propranolol.
The pharmacokinetics of oxazepam, triazolam, lorazepam, and alprazolam are not affected by co-administration of propranolol.
Lipid Lowering Drugs
Co-administration of cholesteramine or colestipol with propranolol resulted in up to a 50% decrease in propranolol concentrations.
Co-administration of propranolol with lovastatin or pravastatin decreased 20% to 25% the AUC of both, but did not alter their pharmacodynamics. Propranolol did not have an effect on the pharmacokinetics of fluvastatin.
Migraine Drugs
Administration of zolmitriptan or rizatriptan with propranolol resulted in increased concentrations of zolmitriptan (AUC increased by 56% and Cmax by 37%) or rizatriptan (the AUC and Cmax were increased by 67% and 75%, respectively).
Neuroleptic Drugs
Co-administration of propranolol at doses greater than or equal to 160 mg/day resulted in increased thioridazine plasma concentrations ranging from 50% to 370% and increased thioridazine metabolites concentrations ranging from 33% to 210%.
Co-administration of chlorpromazine with propranolol resulted in increased plasma levels of both drugs (70% increase in propranolol concentrations).
Theophylline
Co-administration of theophylline with propranolol decreases theophylline oral clearance by 33% to 52%.
Warfarin
Concomitant administration of propranolol and warfarin has been shown to increase warfarin bioavailability and increase prothrombin time.
Pharmacodynamics and Clinical Effects
Hypertension
In a double-blind, parallel dose-response study in patients with mild-to-moderate hypertension (n=434), doses of INNOPRAN XL from 80 to 640 mg were taken once daily at approximately 10 p.m. INNOPRAN XL significantly lowered sitting systolic and diastolic blood pressure when measurements were taken approximately 16 hours later. The placebo-subtracted diastolic blood pressure effect for the 80- and 120-mg doses was -3.0 and -4.0 mm Hg, respectively. Higher doses of INNOPRAN XL (160, 640 mg) had no additional blood pressure lowering effect when compared with 120 mg. The antihypertensive effects of INNOPRAN XL were seen in the elderly (‚Č•65 years old) and men and women. There were too few non-white patients to assess the efficacy of INNOPRAN XL in these patients.
Indications And Usage
Hypertension
INNOPRAN XL is indicated in the management of hypertension; it may be used alone or in combination with other antihypertensive agents.
Contraindications
Propranolol is contraindicated in 1) cardiogenic shock; 2) sinus bradycardia, sick sinus syndrome, and greater than first-degree block unless a permanent pacemaker is in place; 3) bronchial asthma; and 4) in patients with known hypersensitivity to propranolol hydrochloride.
Warnings
Cardiac Failure
Sympathetic stimulation may be a vital component supporting circulatory function in patients with congestive heart failure, and its inhibition by beta-blockade may precipitate more severe failure. Although beta-blockers should be avoided in overt congestive heart failure, some have been shown to be highly beneficial when used with close follow-up in patients with a history of failure who are well compensated and are receiving additional therapies, including diuretics as needed. Beta-adrenergic blocking agents do not abolish the inotropic action of digitalis on heart muscle.
Boxed Warning section
Angina Pectoris: There have been reports of exacerbation of angina and, in some cases, myocardial infarction, following abrupt discontinuance of propranolol therapy. Therefore, when discontinuance of propranolol is planned, the dosage should be gradually reduced over at least a few weeks, and the patient should be cautioned against interruption or cessation of therapy without a physician’s advice. If propranolol therapy is interrupted and exacerbation of angina occurs, it is usually advisable to reinstitute propranolol therapy and take other measures appropriate for the management of angina pectoris. Since coronary artery disease may be unrecognized, it may be prudent to follow the above advice in patients considered at risk of having occult atherosclerotic heart disease who are given propranolol for other indications.
Hypersensitivity and Skin Reactions
Hypersensitivity reactions, including anaphylactic/anaphylactoid reactions, have been associated with the administration of propranolol (see ADVERSE REACTIONS).
Cutaneous reactions, including Stevens-Johnson syndrome, toxic epidermal necrolysis, exfoliative dermatitis, erythema multiforme, and urticaria, have been reported with use of propranolol (see ADVERSE REACTIONS).
Nonallergic Bronchospasm (e.g., Chronic Bronchitis, Emphysema)
In general, patients with bronchospastic lung disease should not receive beta-blockers. Propranolol should be administered with caution in this setting since it may block bronchodilation produced by endogenous and exogenous catecholamine stimulation of beta-receptors.
Major Surgery
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery; however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Propranolol is a competitive inhibitor of beta-receptor agonists, and its effects can be reversed by administration of such agents, e.g., dobutamine or isoproterenol. However, such patients may be subject to protracted severe hypotension.
Diabetes and Hypoglycemia
Beta-adrenergic blockade may prevent the appearance of certain premonitory signs and symptoms (pulse rate and blood pressure changes) of acute hypoglycemia, especially in labile insulin-dependent diabetics. In these patients, it may be more difficult to adjust the dosage of insulin.
Propranolol therapy, particularly in infants and children, diabetic or not, has been associated with hypoglycemia especially during fasting, as in preparation for surgery. Hypoglycemia has been reported with propranolol use after prolonged physical exertion and in patients with renal insufficiency.
Thyrotoxicosis
Beta-adrenergic blockade may mask certain clinical signs of hyperthyroidism. Therefore, abrupt withdrawal of propranolol may be followed by an exacerbation of symptoms of hyperthyroidism, including thyroid storm. Propranolol may change thyroid-function tests, increasing T4 and reversing T3, and decreasing T3.
Wolff-Parkinson-White Syndrome
Beta-adrenergic blockade in patients with Wolff-Parkinson-White syndrome and tachycardia has been associated with severe bradycardia requiring treatment with a pacemaker. In one case, this resulted after an initial dose of 5-mg propranolol.
Precautions
General
Propranolol should be used with caution in patients with impaired hepatic or renal function. INNOPRAN XL is not indicated for the treatment of hypertensive emergencies.
Beta-adrenergic receptor blockade can cause reduction of intraocular pressure. Patients should be told that INNOPRAN XL may interfere with the glaucoma screening test. Withdrawal may lead to a return of intraocular pressure.
Myopathy
Caution should be exercised when administering propranolol to patients with underlying skeletal muscle disease. Isolated cases of exacerbation of myopathy and myotonia have been reported.
Risk of Anaphylactic Reaction
While taking beta-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
Clinical Laboratory Tests
In patients with hypertension, use of propranolol has been associated with elevated levels of serum potassium, and serum transaminases and alkaline phosphatase. In severe heart failure, the use of propranolol has been associated with increases in blood urea nitrogen.
Drug Interactions
Caution should be exercised when INNOPRAN XL is administered with drugs that have an effect on CYP2D6, 1A2, or 2C19 metabolic pathways. Co-administration of such drugs with propranolol may lead to clinically relevant drug interactions and changes on its efficacy and/or toxicity (see CLINICAL PHARMACOLOGY, Drug Interactions).
Plasma propranolol levels may increase with acute alcohol consumption and decrease upon chronic alcohol use.
Cardiovascular Drugs
ACE Inhibitors
When combined with beta-blockers, ACE inhibitors can cause hypotension, particularly in the setting of acute myocardial infraction.
The antihypertensive effects of clonidine may be antagonized by beta-blockers. INNOPRAN XL should be administered cautiously to patients withdrawing from clonidine.
Alpha Blockers
Prazosin has been associated with prolongation of first dose hypotension in the presence of beta-blockers.
Postural hypotension has been reported in patients taking both beta-blockers and terazosin or doxazosin.
Antiarrhythmics
Propafenone has negative inotropic and beta-blocking properties that can be additive to those of propranolol.
Quinidine increases the concentration of propranolol and produces greater degrees of clinical beta-blockade and may cause postural hypotension.
Amiodarone is an antiarrhythmic agent with negative chronotropic properties that may be additive to those seen with ő≤-blockers such as propranolol.
The clearance of lidocaine and bupivacaine are significantly reduced with administration of propranolol. Lidocaine and bupivacaine toxicity has been reported following coadministration with propranolol. (see also PRECAUTIONS, Drug Interactions, Non-Cardiovascular Drugs, Anesthetic Agents)
Caution should be exercised when administering INNOPRAN XL with drugs that slow A-V nodal conduction, e.g. digitalis, lidocaine, and calcium channel blockers.
Calcium Channel Blockers
Caution should be exercised when patients receiving a beta-blocker are administered a calcium-channel-blocking drug with negative inotropic and/or chronotropic effects. Both agents may depress myocardial contractility or atrioventricular conduction.
There have been reports of significant bradycardia, heart failure, and cardiovascular collapse with concurrent use of verapamil and beta-blockers.
Co-administration of propranolol and diltiazem in patients with cardiac disease has been associated with bradycardia, hypotension, high degree heart block, and heart failure.
Digitalis Glycosides
Both digitalis glycosides and beta-blockers slow atrioventricular conduction and decrease heart rate. Concomitant use can increase the risk of bradycardia.
Inotropic Agents
Patients on long-term therapy with propranolol may experience uncontrolled hypertension if administered epinephrine as a consequence of unopposed alpha-receptor stimulation. Epinephrine is therefore not indicated in the treatment of propranolol overdose (see OVERDOSAGE).
Isoproterenol and Dobutamine
Propranolol is a competitive inhibitor of beta-receptor agonists, and its effects can be reversed by administration of such agents, e.g., dobutamine or isoproterenol. Also, propranolol may reduce sensitivity to dobutamine stress echocardiography in patients undergoing evaluation for myocardial ischemia.
Reserpine
Patients receiving catecholamine-depleting drugs, such as reserpine and INNOPRAN XL, should be closely observed for excessive reduction of resting sympathetic nervous activity, which may result in hypotension, marked bradycardia, vertigo, syncopal attacks, or orthostatic hypotension.
Non-Cardiovascular Drugs
Anesthetic Agents
Methoxyflurane and trichloroethylene may depress myocardial contractility when administered with propranolol.
The clearance of local amide anesthetics (e.g., lidocaine, bupivacaine, mepivacaine) is reduced with administration of propranolol. Lidocaine and bupivacaine toxicity has been reported following coadministration with propranolol. Caution should be exercised when amide anesthetic agents are administered concomitantly with propanolol.
Antidepressants
The hypotensive effects of MAO inhibitors or tricyclic antidepressants may be exacerbated when administered with beta-blockers by interfering with the beta-blocking activity of propranolol.
Neuroleptic Drugs
Hypotension and cardiac arrest have been reported with the concomitant use of propranolol and haloperidol.
Non-Steroidal Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDS) have been reported to blunt the antihypertensive effect of beta-adrenoreceptor blocking agents.
Administration of indomethacin with propranolol may reduce the efficacy of propranolol in reducing blood pressure and heart rate.
Thyroxine
Thyroxine may result in a lower than expected T3 concentration when used concomitantly with propranolol.
Warfarin
Propranolol when administered with warfarin increases the concentration of warfarin. Prothrombin time, therefore, should be monitored.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In dietary administration studies in which mice and rats were treated with propranolol HCl for up to 18 months at doses of up to 150 mg/kg/day, there was no evidence of drug-related tumorigenesis. On a body surface area basis, this dose in the mouse and rat is, respectively, about equal to and about twice the maximum recommended human oral daily dose (MRHD) of 640 mg propranolol HCl. In a study in which both male and female rats were exposed to propranolol HCl in their diets at concentrations of up to 0.05% (about 50 mg/kg body weight and less than the MRHD), from 60 days prior to mating and throughout pregnancy and lactation for 2 generations, there were no effects on fertility. Based on differing results from Ames tests performed by different laboratories, there is equivocal evidence for a genotoxic effect of propranolol HCl in bacteria (S. typhimurium strain TA 1538).
Pregnancy
Pregnancy Category C
In a series of reproductive and developmental toxicology studies, propranolol was given to rats by gavage or in the diet throughout pregnancy and lactation. At doses of 150 mg/kg/day, but not at doses of 80 mg/kg/day (equivalent to the MRHD on a body surface area basis), treatment was associated with embryotoxicity (reduced litter size and increased resorption rates) as well as neonatal toxicity (deaths). Propranolol HCI also was administered (in the feed) to rabbits (throughout pregnancy and lactation) at doses as high as 150 mg/kg/day (about 5 times the maximum recommended human oral daily dose). No evidence of embryo or neonatal toxicity was noted.
There are no adequate and well-controlled studies in pregnant women. Intrauterine growth retardation, small placentas, and congenital anomalies have been reported for neonates whose mothers received propranolol HCl during pregnancy. Neonates whose mothers received propranolol HCl at parturition have exhibited bradycardia, hypoglycemia, and/or respiratory depression. Adequate facilities for monitoring such infants at birth should be available. INNOPRAN XL should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
Propranolol is excreted in human milk. Caution should be exercised when INNOPRAN XL is administered to a nursing woman.
Pediatric Use
Safety and effectiveness of propranolol in pediatric patients have not been established.
Geriatric Use
Clinical studies of INNOPRAN XL did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Adverse Reactions
Adverse events occurring at a rate of ‚Č•3%, excluding those reported more commonly in placebo, encountered in the INNOPRAN XL placebo-controlled hypertension trials and plausibly related to treatment are shown in Table 1.
Table 1. Treatment Emergent Adverse Events Reported In ‚Č•3% of Subjects
INNOPRAN XL
Placebo
80 mg
120 mg
Body System
(N=88)
(N=89)
(N=85)
Fatigue
3 (3.0%)
4 (5.0%)
6 (7.0%)
Dizziness (except vertigo)
2 (2.0%)
6 (7.0%)
3 (4.0%)
Constipation
0
3 (3.0%)
1 (1.0%)
The following adverse events were observed and have been reported with use of formulations of sustained- or immediate-release propranolol.
Cardiovascular
Bradycardia; congestive heart failure; intensification of AV block; hypotension; paresthesia of hands; thrombocytopenic purpura; arterial insufficiency, usually of the Raynaud type.
Central Nervous System
Light-headedness, mental depression manifested by insomnia, lassitude, weakness, fatigue; reversible mental depression progressing to catatonia; visual disturbances; hallucinations; vivid dreams; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics. For immediate-release formulations, fatigue, lethargy, and vivid dreams appear dose related.
Gastrointestinal
Nausea, vomiting, epigastric distress, abdominal cramping, diarrhea, constipation, mesenteric arterial thrombosis, ischemic colitis.
Allergic
Hypersensitivity reactions, including anaphylactic/anaphylactoid reactions; pharyngitis and agranulocytosis; erythematous rash, fever combined with aching and sore throat, laryngospasm, and respiratory distress.
Respiratory
Bronchospasm.
Hematologic
Agranulocytosis, nonthrombocytopenic purpura, thrombocytopenic purpura.
Skin
Stevens-Johnson syndrome; toxic epidermal necrolysis; exfoliative dermatitis; erythema multiforme; urticaria.
Musculoskeletal
Myopathy, myotonia (see PRECAUTIONS).
Autoimmune
In extremely rare instances, systemic lupus erythematosus has been reported.
Miscellaneous
Alopecia, LE-like reactions, psoriasiform rashes, dry eyes, male impotence, and Peyronie’s disease have been reported rarely. Oculomucocutaneous reactions involving the skin, serous membranes, and conjunctivae reported for a beta blocker (practolol) have not been associated with propranolol.
Dosage And Administration
INNOPRAN XL should be administered once daily at bedtime (approximately 10 p.m.) and should be taken consistently either on an empty stomach or with food. The starting dose is 80 mg but dosage should be individualized and titration may be needed to a dose of 120 mg. In the clinical trial, doses of INNOPRAN XL above 120 mg had no additional effects on blood pressure (see CLINICAL PHARMACOLOGY, Pharmacodynamics and Clinical Effects). The time needed for full antihypertensive response is variable, but is usually achieved within 2 to 3 weeks.
Overdosage
Most overdoses of propranolol are mild and respond to supportive care.
Propranolol is not significantly dialyzable. In the event of overdose or exaggerated response, the following measures should be employed.
Hypotension and bradycardia have been reported following propranolol overdose and should be treated appropriately. Glucagon can exert potent inotropic and chronotropic effects and may be particularly useful for the treatment of hypotension or depressed myocardial function after a propranolol overdose.
Glucagon should be administered as 50-150 mcg/kg intravenously followed by continuous drip of 1-5 mg/hour for positive chronotropic effect. Isoproterenol, dopamine or phosphodiesterase inhibitors may also be useful. Epinephrine, however, may provoke uncontrolled hypertension. Bradycardia can be treated with atropine or isoproterenol. Serious bradycardia may require temporary cardiac pacing.
The electrocardiogram, pulse, blood pressure, neurobehavioral status and intake and output balance must be monitored. Isoproterenol and aminophylline may be used for bronchospasm.
How Supplied
INNOPRAN XL (propranolol hydrochloride) Extended Release Capsules
Each gray/white capsule, imprinted with ‚Äú80‚ÄĚ, 2¬†segmented bands, ‚ÄúInnoPran XL‚ÄĚ, and the Reliant logo, contains 80¬†mg of propranolol hydrochloride in bottles of 30¬†(NDC¬†0173-0790-01), bottles of 100¬†(NDC¬†0173-0790-02).
Each gray/off-white capsule, imprinted with ‚Äú120‚ÄĚ, 3¬†segmented bands, ‚ÄúInnoPran XL‚ÄĚ, and the Reliant logo, contains 120¬†mg of propranolol hydrochloride in bottles of 30 (NDC 0173-0791-01), bottles of 100¬†(NDC¬†0173-0791-02).
Store at 25¬ļC¬†(77¬ļF); excursions permitted to 15¬†and 30¬ļC¬†(59¬†and 86¬ļF) [see USP Controlled Room Temperature] in a tightly closed container.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2010 GlaxoSmithKline. All rights reserved.
December 2010
INN:7PI
Principal Display Panel
NDC 0173-0790-01
InnoPran XL¬ģ
(propranololHCl)
Extended Release Capsules
80 mg
Rx only
30 Capsules
Usual Dose: One capsule daily at bedtime. See package insert for full prescribing information.
Store at 25oC (77oF); excursions permitted to 15o ‚Äď 30oC (59o ‚Äď 86oF) [See USP Controlled Room Temperature]. Keep tightly closed.
GlaxoSmithKline
RTP, NC 27709
Made in Italy
Rev. 10/10
10000000084993
![]()
Principal Display Panel
NDC 0173-0791-01
InnoPran XL¬ģ
(propranololHCl)
Extended Release Capsules
120 mg
Rx only
30 Capsules
Usual Dose: One capsule daily at bedtime. See package insert for full prescribing information.
Store at 25oC (77oF); excursions permitted to 15o ‚Äď 30oC (59o ‚Äď 86oF) [See USP Controlled Room Temperature]. Keep tightly closed.
GlaxoSmithKline
RTP, NC 27709
Made in Italy
Rev. 10/10
10000000084995
![]()
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site