Levomilnacipran (levomilnacipran hydrochloride 80 mg) Dailymed
Generic: levomilnacipran is used for the treatment of Depressive Disorder, Major
IMPRINT: AN 414
SHAPE: capsule
COLOR: yellow
All Imprints
24 hr levomilnacipran 120 mg extended release oral capsule - an 455 capsule pink
24 hr levomilnacipran 20 mg extended release oral capsule - an 411 capsule yellow
24 hr levomilnacipran 80 mg extended release oral capsule - an 437 capsule pink
24 hr levomilnacipran 40 mg extended release oral capsule - an 414 capsule yellow
Boxed Warning
Warning: Suicidal Thoughts And Behaviors
Go PRO for all pill images
Warning: Suicidal Thoughts And Behaviors
Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors [see Warnings and Precautions ( 5.1 ) ] .
Levomilnacipran is not approved for use in pediatric patients [see Use in Specific Populations (8.4)].
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
See full prescribing information for complete boxed warning.
Increased risk of suicidal thoughts and behavior in pediatric and young adult patients taking antidepressants. Closely monitor all antidepressant-treated patients for clinical worsening and emergence of suicidal thoughts and behaviors (5.1 ). Levomilnacipran is not approved for use in pediatric patients (8.4 ).
Recent Major Changes Section
Warnings and Precautions (5.1)                                      10/2019
Warnings and Precautions (5.2)                                      10/2019
Warnings and Precautions (5.5)                                      10/2019
Warnings and Precautions (5.6)                                      10/2019
Warnings and Precautions (5.11)                                    10/2019
Dosage and Administration, Use of levomilnacipran with Other MAOIs such as
Linezolid or Methylene Blue - Removed(2.6)                         03/2023
Warnings and Precautions, Elevated Blood Pressure(5.3)    03/2023
Warnings and Precautions(5.2 ,5.5)                                       08/2023
1 Indications And Usage
Levomilnacipran is indicated for the treatment of major depressive disorder (MDD) in adults [see Clinical Studies (14)].
Limitation of Use:  Levomilnacipran extended-release capsules are not approved for the management of fibromyalgia. The efficacy and safety of levomilnacipran extended-release capsules for the management of fibromyalgia have not been established.
Levomilnacipran is a serotonin and norepinephrine reuptake inhibitor (SNRI) indicated for the treatment of Major Depressive Disorder (MDD) in adults(1) .
Limitation of Use: Levomilnacipran extended-release capsules are not approved for the management of fibromyalgia. The efficacy and safety of  levomilnacipran extended-release capsules for the management of fibromyalgia have not been established(1) .
2 Dosage And Administration
- Recommended dosage: 40 mg to 120 mg once daily with or without food
(2.1) .- Initial dosage is 20 mg once daily for 2 days and then increase to 40 mg once daily
(2.1) .- Based on clinical response and tolerability, increase dose in increments of 40 mg at intervals of 2 or more days
(2.1) .- The maximum recommended dosage is 120 mg once daily
(2.1) .- Take capsules whole; do not open, chew or crush
(2.1) .- Renal impairment
(2.3) :
- Severe renal impairment: Maximum recommended dosage is 40 mg once daily.
- Moderate renal impairment: Maximum recommended dosage is 80 mg once daily.
- Discontinuation: Reduce dose gradually whenever possible
(2.4) .2.1 Recommended Dosage
The recommended dosage range for levomilnacipran extended-release capsule is 40 mg to 120 mg once daily, with or without food. Levomilnacipran extended-release capsules should be initiated at 20 mg once daily for 2 days and then increased to 40 mg once daily. Based on clinical response and tolerability, levomilnacipran extended-release capsules may be increased in increments of 40 mg at intervals of 2 or more days. The maximum recommended dosage is 120 mg once daily.
Take levomilnacipran extended-release capsules at approximately the same time each day. Swallow levomilnacipran extended-release capsules whole; do not open, chew, or crush the capsule.
2.2 Screen for Bipolar Disorder Prior to Starting Levomilnacipran Extended-Release Capsules
Prior to initiating treatment with levomilnacipran extended-release capsules or another antidepressant, screen patients for a personal or family history of bipolar disorder, mania, or hypomania [see Warnings and Precautions (5.8)].
2.3 Dosage Recommendations for Patients with Renal Impairment
- End stage renal disease (ESRD): Levomilnacipran extended-release capsules are not recommended;
- Severe renal impairment (creatinine clearance of 15 mL/min to 29 mL/min), the dosage should not exceed 40 mg once daily;
- Moderate renal impairment (creatinine clearance of 30 mL/min to 59 mL/min), the dosage should not exceed 80 mg once daily;
- Mild renal impairment (creatinine clearance of 60 mL/min to 89 mL/min): no dosage adjustment recommended   [see Use in Specific Populations (8.7)].
2.4 Discontinuing of Treatment with Levomilnacipran Extended-Release Capsules
Discontinuation symptoms have been reported with discontinuation of serotonergic drugs such as levomilnacipran extended-release capsules. Gradual dose reduction is recommended, instead of abrupt discontinuation, whenever possible. Monitor patients for these symptoms when discontinuing levomilnacipran extended-release capsules. If intolerable symptoms occur following a dose decrease or upon discontinuation of treatment, consider resuming the previously prescribed dose and decreasing the dose at a more gradual rate [see Warnings and Precautions (5.10)].
2.5 Switchinga Patient To or From a Monoamine Oxidase Inhibitor (MAOI) Intended to TreatPsychiatric Disorders
At least 14 days must elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with levomilnacipran extended-release capsules. Conversely, at least 7 days should be allowed after stopping levomilnacipran extended-release capsules before starting an MAOI antidepressant [see Contraindications (4)].
2.6Dosage Recommendations for Use with StrongCYP3A4 Inhibitors
The maximum recommended dosage of levomilnacipran extended-release capsules should not exceed 80 mg once daily when used with strong CYP3A4 inhibitors [see Drug Interactions (7.1)].
3 Dosage Forms And Strengths
Levomilnacipran extended-release capsules are available as 20 mg, 40 mg, 80 mg and 120 mg extended-release capsules.
Levomilnacipran extended-release capsules, 20 mg are supplied as size ‚Äė4‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on yellow cap and ‚Äú411‚ÄĚ on white body of the capsules with black ink, filled with white to off-white pellets.
Levomilnacipran extended-release capsules, 40 mg are supplied as size ‚Äė3‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on yellow cap and ‚Äú414‚ÄĚ on yellow body of the capsules with black ink, filled with white to off-white¬†pellets.
Levomilnacipran extended-release capsules, 80 mg are supplied as size ‚Äė2‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on pink cap and ‚Äú437‚ÄĚ on white body of the capsules with black ink, filled with white to off-white pellets.
Levomilnacipran extended-release capsules, 120 mg are supplied as size ‚Äė1‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on pink cap and ‚Äú455‚ÄĚ on pink body of the capsules with black ink, filled with white to off-white pellets.
- Extended-release capsules: 20 mg, 40 mg, 80 mg and 120 mg (
3 ).
4 Contraindications
Levomilnacipran is contraindicated:
- in patients with hypersensitivity to levomilnacipran, milnacipran HCl, or to any excipient in the formulation.
- with the use of MAOIs intended to treat psychiatric disorders with levomilnacipran or within 7 days of stopping treatment with levomilnacipran is contraindicated because of an increased risk of serotonin syndrome. The use of levomilnacipran within 14 days of stopping an MAOI intended to treat psychiatric disorders is also contraindicated [see Dosage and Administration (2.5) and Warnings and Precautions (5.2)].
Starting levomilnacipran in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue is also contraindicated because of an increased risk of serotonin syndrome [see Dosage and Administration (2.6) and Warnings and Precautions (5.2)].
- Hypersensitivity to levomilnacipran, milnacipran HCl, or any excipient in the levomilnacipran extended-release capsules formulation (
4 ).
- Do not use MAOIs intended to treat psychiatric disorders with levomilnacipran or within 7 days of stopping treatment with levomilnacipran. Do not use levomilnacipran within 14 days of stopping an MAOI intended to treat psychiatric disorders. In addition, do not start levomilnacipran in a patient who is being treated with linezolid or intravenous methylene blue (
4 ).
5 Warnings And Precautions
- Serotonin Syndrome: Increased risk when co-administered with other serotonergic agents, but also when taken alone. If it occurs, discontinue levomilnacipran and serotonergic agents and initiate supportive treatment  (
5.2 ).- Elevated Blood Pressure and Heart Rate: Control hypertension before initiating therapy with levomilnacipran. Monitor blood pressure regularly during treatment (
5.3 ,5.4 ).- Increased Risk of Bleeding: Concomitant use of NSAIDs, aspirin, other antiplatelet drugs, warfarin, and other anticoagulants may increase this risk (
5.5 ).- Angle Closure Glaucoma: Angle closure glaucoma has occurred in patients with untreated anatomically narrow angles treated with antidepressants (
5.6 ).- Urinary Hesitation or Retention: Can occur. If such symptoms occur, discontinue levomilnacipran or consider other appropriate medical intervention (
5.7 ).- Activation of Mania/Hypomania: Screen patients for bipolar disorder, Caution patients about risk of activation of mania/hypomania. (
5.8 ).- Seizures: Can occur. Use with caution in patients with a seizure disorder (
5.9 ).- Discontinuation Syndrome: Taper dose when possible and monitor for discontinuation symptoms (
5.10 ).- Hyponatremia: Can occur in association with SIADH (
5.11 ).- Sexual Dysfunction: Levomilnacipran may cause symptoms of sexual dysfunction (
5.12 ). 5.1 SuicidalThoughts and Behaviors in Adolescents and Young Adults
In pooled analyses of placebo-controlled trials of antidepressant drugs (SSRIs and other antidepressant classes) that included approximately 77,000 adult patients and 4,500 pediatric patients, the incidence of suicidal thoughts and behaviors in antidepressant-treated patients aged 24 years and younger was greater than in placebo-treated patients. There was considerable variation in risk of suicidal thoughts and behaviors among drugs, but there was an increased risk identified in young patients for most drugs studied. There were differences in absolute risk of suicidal thoughts and behaviors across the different indications, with the highest incidence in patients with MDD. The drug-placebo differences in the number of cases of suicidal thoughts and behaviors per 1,000 patients treated are provided in Table 1.
Table 1: Risk Differences of the Number of Patients of Suicidal Thoughts and Behavior in the Pooled Placebo-Controlled Trials of Antidepressants in Pediatric * and Adult Patients
Age Range
Drug-Placebo Difference in Number of Patients of Suicidal Thoughts or Behaviors per 1,000 Patients Treated
Increases Compared to Placebo
< 18 years old
14 additional patients
18 to 24 years old
5 additional patients
Decreases Compared to Placebo
25 to 64 years old
1 fewer patient
‚Č• 65 years old
6 fewer patients
*Levomilnacipran is not approved for use in pediatric patients.
It is unknown whether the risk of suicidal thoughts and behaviors in children, adolescents, and young adults extends to longer-term use, i.e. beyond four months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with MDD that antidepressants delay the recurrence of depression and that depression itself is a risk factor for suicidal thoughts and behaviors.
Monitor all antidepressant-treated patients for any indication for clinical worsening and emergence of suicidal thoughts and behaviors, especially during the initial few months of drug therapy, and at times of dosage changes. Counsel family members or caregivers of patients to monitor for changes in behavior and to alert the healthcare provider. Consider changing the therapeutic regimen, including possibly discontinuing levomilnacipran, in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.
5.2 Serotonin Syndrome
Serotonin-norepinephrine reuptake inhibitors (SNRIs), including levomilnacipran, can precipitate serotonin syndrome, a potentially life-threatening condition. The risk is increased with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, meperidine, methadone, tryptophan, buspirone, amphetamines, and St. John’s Wort) and with drugs that impair metabolism of serotonin, i.e. MAOIs  [see Contraindications (4), Drug Interactions (7.1)]. Serotonin syndrome can also occur when these drugs are used alone.
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
The concomitant use of levomilnacipran with MAOIs is contraindicated. In addition, do not initiate levomilnacipran in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection). If it is necessary to initiate treatment with a MAOI such as linezolid or intravenous methylene blue in a patient taking levomilnacipran, discontinue levomilnacipran before initiating treatment with the MAOI [see Dosage and Administration (2.5, 2.6) and Contraindications (4), Drug Interactions (7.1)].
Monitor all patients taking levomilnacipran for the emergence of serotonin syndrome. Discontinue treatment with levomilnacipran and any concomitant serotonergic agents immediately if the above events occur and initiate supportive symptomatic treatment. If concomitant use of levomilnacipran with other serotonergic drugs is clinically warranted, inform patients of the increased risk for serotonin syndrome and monitor for symptoms.
5.3 Elevated Blood Pressure
SNRIs, including levomilnacipran, have been associated with increases in blood pressure. Blood pressure should be measured prior to initiating treatment and periodically throughout levomilnacipran treatment. Pre-existing hypertension should be controlled before initiating treatment with levomilnacipran. Caution should be exercised in treating patients with pre-existing hypertension, cardiovascular, or cerebrovascular conditions that might be compromised by increases in blood pressure. For patients who experience a sustained increase in blood pressure while receiving levomilnacipran, discontinuation or other appropriate medical intervention should be considered.
Table 2 shows the mean changes in blood pressure, sustained hypertension, and upward shifts in hypertensive status that were observed in levomilnacipran-treated adult patients in the short-term placebo-controlled studies.
Table 2: Blood Pressure Mean Changes, Sustained Hypertension, and Upward Shifts in Hypertensive Status with Levomilnacipran (in Adults)
Placebo
Levomilnacipran
40 to 120 mg/day
Mean change from baseline to end of treatment, mm Hg
Systolic blood pressure (SBP)
-0.4
3.0
Diastolic blood pressure (DBP)
-0.0
3.2
Sustained Hypertension, % of patients
Broad Criteria:
SBP ‚Č• 140 mm Hg and an increase ‚Č• 15 mm Hg OR
DBP ‚Č• 90 mm Hg and an increase ‚Č• 10 mm Hg for at least 3 consecutive visits
1.2
1.8
Strict Criteria:
SBP ‚Č• 140 mm Hg and an increase ‚Č• 15 mm Hg AND
DBP ‚Č• 90 mm Hg and an increase ‚Č• 10 mm Hg for at least 3 consecutive visits
0.1
0.3
Upward Shifts in Hypertensive Statusa, % of patients
Normal/ Pre-hypertensive ‚Üí Stage I/ Stage II
7.1
10.4
a Normal Blood Pressure: SBP < 120 mm Hg and DBP < 80 mm Hg
Pre-hypertension: SBP ‚Č• 120 mm Hg and ‚ȧ 139 mm Hg or DBP ‚Č• 80 mm Hg and ‚ȧ 89 mm Hg
Stage I hypertension: SBP ‚Č• 140 mm Hg and ‚ȧ 159 mm Hg or DBP ‚Č• 90 mm Hg and ‚ȧ 99 mm Hg
Stage II hypertension: SBP ‚Č• 160 mm Hg or DBP ‚Č• 100 mm Hg
In the short-term, placebo-controlled MDD studies in adults, the mean increase from initiation of treatment in systolic BP was 3 mm Hg and diastolic BP was 3.2 mm Hg, as compared to no change in the placebo group. There were no dose-related changes in systolic and diastolic blood pressure observed.
In adult patients exposed to one-year, open-label treatment of levomilnacipran (doses range from 40 mg to 120 mg once daily), the mean change from initiation of treatment in systolic BP was 3.9 mm Hg and diastolic BP was 3.1 mm Hg.
In short-term, placebo- and active-controlled MDD studies in pediatric patients 7 years to less than 18 years of age, treatment with levomilnacipran was associated with the occurrence of new-onset hypertension (two systolic and/or diastolic BP measurements in the stage I hypertension range and/or one measurement in the stage II range) in 36.2% of treated patients compared with 20.7% of patients randomized to placebo. Elevations in either systolic or diastolic BP leading to measures at or above the stage II hypertension threshold occurred in 12.1% of pediatric patients treated with levomilnacipran and 7.5% of patients randomized to placebo. Sustained hypertension (three or more consecutive systolic or diastolic BP measurements at or above the stage I hypertension threshold) occurred in 15% of pediatric patients treated with levomilnacipran and 4% of patients randomized to placebo. The safety and effectiveness of levomilnacipran have not been established in pediatric patients for the treatment of MDD.
In the short-term, placebo-controlled studies in adults, 11.6% of patients met orthostatic hypotension criteria (SBP or DBP) in the levomilnacipran group compared to 9.7% in the placebo group. Orthostatic reductions of blood pressure ‚Č• 10 mm Hg in DBP occurred in 5.8%, 6.1% and 9.8% of levomilnacipran-treated patients with doses of 40, 80 and 120 mg/day respectively, compared to 6.2% of placebo-treated patients.
Concomitant use of levomilnacipran with drugs that increase blood pressure and heart rate has not been evaluated and such combinations should be used with caution. Effects of levomilnacipran on blood pressure in patients with significant hypertension or cardiac disease have not been systematically evaluated. Levomilnacipran should be used with caution in these patients.
5.4 Elevated Heart Rate
SNRIs, including levomilnacipran, have been associated with increased heart rate. Heart rate should be measured prior to initiating treatment and periodically throughout levomilnacipran treatment. Pre-existing tachyarrhythmias and other cardiac disease should be treated before starting therapy with levomilnacipran. For patients who experience a sustained increase in heart rate while receiving levomilnacipran, discontinuation or other appropriate medical intervention should be considered.
In short-term clinical studies, levomilnacipran treatment was associated with a mean increase in heart rate of 7.4 beats per minute (bpm) compared to a mean decrease of 0.3 bpm in placebo-treated patients. Heart rate increase in levomilnacipran-treated patients receiving doses of 40 mg, 80 mg and 120 mg was 7.2, 7.2, and 9.1 bpm.
Levomilnacipran has not been systematically evaluated in patients with a cardiac rhythm disorder.
5.5 Increased Risk of Bleeding
Drugs that interfere with serotonin reuptake, including levomilnacipran, may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), warfarin, and other anticoagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Based on data from the published observational studies, exposure to SNRIs, particularly in the month before delivery, has been associated with a less than 2-fold increase in the risk of postpartum hemorrhage [see Use in Specific Populations (8.1)].  Bleeding events related to SSRIs and SNRIs have ranged from ecchymosis, hematoma, epistaxis, and petechiae to life-threatening hemorrhages.
Inform patients about the increased risk of bleeding associated with the concomitant use of levomilnacipran and NSAIDs, aspirin, or other drugs that affect coagulation [see Drug Interactions (7.1)].
5.6 Angle Closure Glaucoma
The pupillary dilation that occurs following use of many antidepressant drugs including levomilnacipran may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
Avoid use of antidepressants, including levomilnacipran, in patients with anatomically narrow angles.
5.7Urinary Hesitation or Retention
The noradrenergic effect of SNRIs including levomilnacipran, can affect urethral resistance. In the controlled short-term studies, urinary hesitation occurred in 4%, 5% and 6% of levomilnacipran-treated patients receiving doses of 40, 80 and 120 mg, respectively, compared to no patients in the placebo group. Caution is advised in the use of levomilnacipran in patients prone to obstructive urinary disorders. If symptoms of urinary hesitation, urinary retention, or dysuria develop during treatment with levomilnacipran, consideration should be given to the possibility that they might be drug-related, and discontinuation or other appropriate medical intervention should be considered.
5.8Activation of Mania/Hypomania
Symptoms of mania/hypomania were reported in 0.2% of levomilnacipran-treated patients and 0.2% of placebo-treated patients in clinical studies. Activation of mania/hypomania has also been reported in a small proportion of patients with mood disorders who were treated with other antidepressants. Prior to initiating treatment with levomilnacipran, screen patients for any personal or family history of bipolar disorder, mania, or hypomania.
5.9Seizures
One case of seizure has been reported in pre-marketing clinical studies with levomilnacipran. Levomilnacipran has not been systematically evaluated in patients with a seizure disorder. Patients with a history of seizures were excluded from clinical studies. Levomilnacipran should be prescribed with caution in patients with a seizure disorder.
5.10Discontinuation Syndrome
There have been reports of adverse events occurring upon discontinuation of serotonergic antidepressants, particularly when discontinuation is abrupt, including the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesia, such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. While these events are generally self-limiting, there have been reports of serious discontinuation symptoms.
Monitor patients for these symptoms when discontinuing levomilnacipran. Reduce the dose gradually whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, consider resuming the previously prescribed dose. Subsequently, the dose may be decreased, but at a more gradual rate [see Dosage and Administration (2.4)].
5.11Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including levomilnacipran. In many cases, hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/L have been reported. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics or who are otherwise volume depleted can be at greater risk. Levomilnacipran should be discontinued in patients with symptomatic hyponatremia and appropriate medical intervention should be instituted. Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which can lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death.
5.12 SexualDysfunction
Use of SNRIs, including levomilnacipran, may cause symptoms of sexual dysfunction [see Adverse Reactions (6.1)]. In male patients, SNRI use may result in ejaculatory delay or failure, decreased libido, and erectile dysfunction. In female patients, SNRI use may result in decreased libido and delayed or absent orgasm.
It is important for prescribers to inquire about sexual function prior to initiation of levomilnacipran and to inquire specifically about changes in sexual function during treatment, because sexual function may not be spontaneously reported. When evaluating changes in sexual function, obtaining a detailed history (including timing of symptom onset) is important because sexual symptoms may have other causes, including the underlying psychiatric disorder. Discuss potential management strategies to support patients in making informed decisions about treatment.
6 Adverse Reactions
The following adverse reactions are discussed in greater detail in other sections of the label.
- Hypersensitivity [see Contraindications (4)]
- Suicidal Thoughts and Behaviors in Adolescents and Young Adults [see Warnings and Precautions (5.1)]
- Serotonin Syndrome [see Warnings and Precautions (5.2)]
- Elevated Blood Pressure [see Warnings and Precautions (5.3)]
- Elevated Heart Rate [see Warnings and Precautions (5.4)]
- Increased Risk of Bleeding [see Warnings and Precautions (5.5)]
- Angle Closure Glaucoma [see Warnings and Precautions (5.6)]
- Urinary Hesitation or Retention [see Warnings and Precautions (5.7)]
- Activation of Mania/Hypomania [see Warnings and Precautions (5.8)]
- Seizure [see Warnings and Precautions (5.9)]
- Discontinuation Syndrome [see Warnings and Precautions (5.10)]
- Hyponatremia [see Warnings and Precautions (5.11)]
- Sexual Dysfunction [see Warnings and Precautions (5.12)]
The most common adverse reactions (incidence ‚Č• 5% and at least twice the rate of placebo) are: nausea, constipation, hyperhidrosis, heart rate increase, erectile dysfunction, ejaculation disorder, tachycardia, vomiting, and palpitations (6.1 ).
To report SUSPECTED ADVERSE REACTIONS, contact Amneal Pharmaceuticals at 1-877-835-5472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
6.1Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in clinical practice.
Patient exposure
The safety of levomilnacipran was evaluated in 3,317 patients (18 to 78 years of age) diagnosed with MDD who participated in clinical studies, representing 1,186 patient-years of exposure. Among the 3,317 levomilnacipran-treated patients, 1,583 were exposed to levomilnacipran in short-term, placebo-controlled studies. There were 825 patients who continued from short-term studies into a one-year, open-label extension study.
Of the 3,317 patients exposed to at least one dose of levomilnacipran, 895 patients were exposed to levomilnacipran for at least 6 months and 367 were exposed for one year. In these studies, levomilnacipran was given at doses ranging from 40 mg to 120 mg once daily and was given without regard to food.
Adverse reactions reported as reasons for discontinuation of treatment
In the short-term placebo-controlled pre-marketing studies for MDD, 9% of the 1,583 patients who received levomilnacipran (40 mg to 120 mg) discontinued treatment due to an adverse reaction, compared with 3% of the 1,040 placebo-treated patients in those studies. The most common adverse reaction leading to discontinuation in at least 1% of the levomilnacipran-treated patients in the short-term placebo-controlled studies was nausea (1.5%).
Common adverse reactions in placebo-controlled MDD studies
The most commonly observed adverse reactions in levomilnacipran-treated MDD patients in placebo-controlled studies (incidence ‚Č• 5% and at least twice the rate of placebo) were: nausea, constipation, hyperhidrosis, heart rate increased, erectile dysfunction, ejaculation disorder, tachycardia, vomiting, and palpitations.
Table 3 shows the incidence of adverse reactions that occurred in ‚Č• 2% of levomilnacipran-treated MDD patients and at least twice the rate of placebo in the placebo-controlled studies.
Table 3: Adverse Reactions Occurring in ‚Č• 2% of Levomilnacipran-treated Patients and at Least Twice the rate of Placebo-treated Patients¬† in Pooled MDD Studies
System Organ Class Preferred Term Placebo (N =1,040) % Levomilnacipran 40 to 120 mg/day (N = 1,583)%
Gastrointestinal disorders
Nausea
6
17
Constipation
3
9
Vomiting
1
5
Cardiac disorders
Tachycardiaa
2
6
Palpitations
1
5
Reproductive system and breast disordersb
Erectile dysfunctionc
1
6
Testicular paind
< 1
4
Ejaculation disordere
< 1
5
Investigations
Heart rate increasedf
1
6
Blood pressure increasedg
1
3
Renal and urinary disorders
Urinary hesitation
0
4
Skin and subcutaneous tissue disorders
Hyperhidrosis
2
9
Rashh
0
2
Vascular disorders
Hot flush
1
3
Hypotensioni
1
3
Hypertensionj
1
3
Metabolism and nutrition disorders
Decreased appetite
1
3
a Tachycardia also includes: sinus tachycardia and postural orthostatic tachycardia syndrome
b Percentage is relative to the number of patients in the associated demographic sex category. Fewer than 2% of levomilnacipran-treated MDD female patients in placebo-controlled clinical studies reported adverse events related to sexual function.
c Erectile dysfunction includes: erectile dysfunction, organic erectile dysfunction and psychogenic erectile dysfunction
d Testicular pain includes: testicular pain, epididymitis, and seminal vesiculitis
e Ejaculation disorder includes: ejaculation disorder, ejaculation delayed, ejaculation failure, and premature ejaculation
f Heart rate increased also includes: orthostatic heart rate response increased
g Blood pressure increased also includes: blood pressure systolic increased, blood pressure diastolic increased and blood pressure orthostatic increased
h Rash also includes: rash generalized, rash maculo-papular, rash erythematous and rash macular
i Hypotension also includes: orthostatic hypotension and dizziness postural
j Hypertension also includes: labile hypertension
N = number of patients in the Safety Population
Dose-related adverse reactions
In pooled data from the short-term placebo-controlled fixed-dose studies, there were no dose-related adverse reactions (greater than 2% overall incidence) in patients treated with levomilnacipran across the dose range 40 mg to 120 mg once daily, with the exception of erectile dysfunction and urinary hesitation (see Table 4).
Table 4: Dose-Related Adverse Reactions
System Organ Class Preferred Term
Placebo
(N = 362)
%
Levomilnacipran
40 mg/day
(N = 366)
%
80 mg/day
(N = 367)
%
120 mg/day
(N = 180)
%
Urinary hesitation
0
4
5
6
Erectile dysfunctiona
2
6
8
10
a Percentage is relative to the number of male patients.
N = number of patients in the Safety Population
Other adverse reactions observed in clinical studies
Other infrequent adverse reactions, not described elsewhere in the label, occurring at an incidence of < 2% in MDD patients treated with levomilnacipran were:
Cardiac disorders: Angina pectoris; Supraventricular and Ventricular extrasystoles
Eye disorders: Dry eye; Vision blurred; Conjunctival hemorrhage
General disorders: Chest pain; Thirst
Gastrointestinal disorders: Abdominal pain; Flatulence
Investigations disorders: Blood cholesterol increased; Liver function test abnormal
Nervous System disorders: Migraine; Paraesthesia; Syncope; Extrapyramidal disorder
Psychiatric disorders: Agitation; Anger; Bruxism; Panic attack; Tension; Aggression
Renal and Urinary disorder: Pollakiuria; Hematuria; Proteinuria
Respiratory, thoracic and mediastinal disorders: Yawning
Skin and subcutaneous tissue disorders: Dry skin; Pruritus; Urticaria
6.2 Post-marketing Experience
The following adverse reaction has been identified during post-approval use of levomilnacipran or other selective serotonin and norepinephrine reuptake inhibitors. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiac disorders: Takotsubo cardiomyopathy
Respiratory, thoracic and mediastinal disorders: Anosmia, Hyposmia
7 Drug Interactions
- Strong CYP3A4 inhibitors:  Maximum recommended dosage is 80 mg once daily (
7 ).7.1 DrugsHaving Clinically Important Interactions with Levomilnacipran
Table 5 includes clinically important drug interactions with levomilnacipran.
Table 5: Clinically Important Drug Interactions with Levomilnacipran
Monoamine Oxidase Inhibitors (MAOIs)
Clinical Impact:
Concomitant use of SSRIs and SNRIs including levomilnacipran with MAOIs increases the risk of serotonin syndrome.
Intervention:
Concomitant use of levomilnacipran is contraindicated:
· With an MAOI intended to treat psychiatric disorders or within 7 days of stopping treatment with levomilnacipran.
· Within 14 days of stopping an MAOI intended to treat psychiatric disorders
· In a patient who is being treated with linezolid or intravenous methylene blue
[see Dosage and Administration ( 2.5 , 2.6 ), Contraindications ( 4 ) , and Warnings and Precautions ( 5.2 ) ].
Examples:
selegiline, tranylcypromine, isocarboxazid, phenelzine, linezolid, methylene blue
Other Serotonergic Drugs
Clinical Impact:
Concomitant use of levomilnacipran with other serotonergic drugs increases the risk of serotonin syndrome.
Intervention:
Monitor for symptoms of serotonin syndrome when levomilnacipran is used concomitantly with other drugs that may affect the serotonergic neurotransmitter systems. If serotonin syndrome occurs, immediately discontinue levomilnacipran and/or concomitant serotonergic drugs [see Dosage and Administration (2.5, 2.6), Contraindications (4), and Warnings and Precautions (5.2)].
Examples:
other SNRIs, SSRIs, triptans, tricyclic antidepressants, opioids, lithium, buspirone, amphetamines, tryptophan, and St. John's Wort
Drugs that Interfere with Hemostasis
Clinical Impact:
Concomitant use of levomilnacipran with an antiplatelet or anticoagulant drug may potentiate the risk of bleeding. This may be due to the effect of levomilnacipran on the release of serotonin by platelets.
Intervention:
Closely monitor for bleeding for patients receiving an antiplatelet or anticoagulant drug when levomilnacipran is initiated or discontinued [see Warnings and Precautions ( 5.5 ) ].
Examples:
NSAIDs, aspirin, and warfarin
Strong CYP3A4 Inhibitors
Clinical Impact:
Concomitant use of levomilnacipran with strong CYP3A4 inhibitors increases levomilnacipran exposure [see Pharmacokinetics ( 12.3 ) ].
Intervention:
The dose of levomilnacipran should not exceed 80 mg once daily when used with strong CYP3A4 inhibitors [see Dosage and Administration ( 2.6 ) .
Examples:
Ketoconazole, itraconazole, clarithromycin
Alcohol
Clinical Impact:
Concomitant use of levomilnacipran and alcohol may result in accelerated release of levomilnacipran.
Intervention:
Avoid concomitant use of levomilnacipran and alcohol [see Clinical Pharmacology ( 12.3 ) ].
8 Use In Specific Populations
- Pregnancy: Third trimester use may increase risk for symptoms of poor adaptation (respiratory distress, temperature instability, feeding difficulty, hypotonia, tremor, irritability) in the neonate (8.1).
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antidepressants during pregnancy. Healthcare providers are encouraged to register patients by calling the National Pregnancy Registry for Antidepressants at 1-844-405-6185 or visiting online at https://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/antidepressants.
Risk Summary
Based on data from published observational studies, exposure to SNRIs, particularly in the month before delivery, has been associated with a less than 2-fold increase in the risk of postpartum hemorrhage [see Warnings and Precautions (5.5) and Clinical Considerations].
The available data on levomilnacipran use in pregnant women are insufficient to evaluate for a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. There are risks associated with untreated depression in pregnancy and with exposure to SNRIs and SSRIs, including levomilnacipran, during pregnancy (see Clinical Considerations).
In animal reproduction studies, levomilnacipran was not associated with malformations in rats or rabbits when given during the period of organogenesis at doses up to 8 or 16 times the maximum recommended human dose (MRHD) of 120 mg on a mg/m2 basis, respectively. However, an increase in early post-natal rat pup mortality was seen at a dose equivalent to 5 times the MRHD given during pregnancy and lactation (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Women who discontinued antidepressants during pregnancy were more likely to experience a relapse of major depression than women who continued antidepressants. This finding is from a prospective, longitudinal study that followed 201 pregnant women with a history of major depressive disorder who were euthymic and taking antidepressants at the beginning of pregnancy. Consider the risk of untreated depression when discontinuing or changing treatment with antidepressant medication during pregnancy and postpartum.
Maternal Adverse Reactions
Use of levomilnacipran in the month before delivery may be associated with an increased risk of postpartum hemorrhage [see Warnings and Precautions (5.5)].
Fetal/Neonatal adverse reactions
Neonates exposed to SNRIs or SSRIs, including levomilnacipran, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These findings are consistent with either direct toxic effect of SSRIs and SNRIs or possibly, a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome [see Warnings and Precautions (5.2 and 5.10)].
Data
Animal Data
No malformations were observed when levomilnacipran was administered to pregnant rats or rabbits during the period of organogenesis at oral doses up to 100 mg/kg/day. This dose is 8 and 16 times (in rats and rabbits, respectively) the maximum recommended human dose (MRHD) of 120 mg on a mg/m2 basis. Fetal body weights were reduced in rats, and skeletal ossification was delayed in both rats and rabbits at this dose; these effects were not observed in either species at doses up to 30 mg/kg/day, 2.4 times the MRHD in rats or 5 times the MRHD in rabbits on a mg/m2 basis.
When levomilnacipran was administered to pregnant rats at an oral dose of 60 mg/kg/day, 5 times the MRHD, during organogenesis and throughout pregnancy and lactation, there was an increase in early post-natal pup mortality; no pup mortality was seen at 20 mg/kg/day, 1.6 times the MRHD on a mg/m2 basis. Among the surviving pups, pre- and post-weaning pup weight gain was reduced up to at least 8 weeks of age; however, physical and functional development, including reproductive performance of the progeny, was not affected. The effects on body weight gain were not seen at 7 mg/kg/day, 0.6 times the MRHD on a mg/m2 basis.
8.2 Lactation
Risk Summary
There are no available data on the presence of levomilnacipran in human milk; however, racemic milnacipran is present in human milk (see Data). There are no reports on the effects of levomilnacipran or milnacipran on the breastfed infant or the effects on milk production. However, there are reports of agitation, irritability, poor feeding and poor weight gain in infants exposed to SSRIs or SNRIs through breast milk (see Clinical Considerations). The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for levomilnacipran and any potential adverse effects on the breastfed child from levomilnacipran or from the underlying maternal conditions.
Clinical Considerations
Infants exposed to levomilnacipran should be monitored for agitation, irritability, poor feeding and poor weight gain.
Data
Milnacipran, a racemic mixture that contains levomilnacipran (the 1S,2R-enantiomer of milnacipran), is present in the milk of lactating women treated with milnacipran. In a lactation pharmacokinetic study with milnacipran, a single, oral dose of 50 mg milnacipran HCl tablet was administered to 8 lactating women who were at least 12 weeks postpartum and weaning their infants. The milk/plasma AUC ratio of milnacipran was 1.85 ¬Ī 0.38. The maximum estimated weight-adjusted daily infant dose for milnacipran from breast milk (assuming mean milk consumption of 150 mL/kg/day) was 5% of the maternal weight-adjusted dose based on peak plasma concentrations.
8.4 Pediatric Use
The safety and effectiveness of levomilnacipran have not been established in pediatric patients for the treatment of major depressive disorder (MDD).
The safety and efficacy of levomilnacipran were evaluated in two randomized, double-blind, placebo- and active-controlled 8-week trials in pediatric patients with MDD, one in patients 7 to 17 years of age (flexible-dose study) and the other in patients 12 to 17 years of age (fixed-dose study). The primary efficacy endpoint for both studies was the change from baseline to week 8 in the Children’s Depression Rating Scale-Revised (CDRS-R) total score. The CDRS-R assesses the severity of depression and change in depressive symptoms in children and adolescents with depression. Levomilnacipran was not superior to placebo in either study. The most commonly observed adverse reactions in pediatric patients 7 to 17 years of age randomized to levomilnacipran were similar to those observed in adults [see Adverse Reactions (6.1)].
Levomilnacipran was associated with an increase in blood pressure in placebo-and active-controlled trials in pediatric patients with MDD. Increases in blood pressure in pediatric patients treated with levomilnacipran led to a higher proportion of pediatric patients developing new-onset and sustained hypertension when compared to adults [see Warnings and Precautions (5.3)].
Antidepressants increase the risk of suicidal thoughts and behaviors in pediatric patients [see Boxed Warning, Warnings and Precautions (5.1), and  Adverse Reactions (6.1)].
Juvenile Animal Toxicity Data
In a juvenile animal study, male and female rats were treated with 10, 35, or 120 mg/kg/day of levomilnacipran by oral gavage from post-natal day 21 to 90. At 120 mg/kg/day, there was a decrease in bone mineral density in both males and females and a decrease in mean tibia length in females. These effects were not completely resolved at the end of the recovery period. There was a delay in sexual maturation in females treated with 120 mg/kg/day; however, there was no effect on fertility. The no observed adverse effect level (NOAEL) for all these findings was 35 mg/kg/day.
8.5 Geriatric Use
No dose adjustment is recommended on the basis of age [see  Clinical Pharmacology (12.3)].
Of the total number of patients in the 8-week clinical studies of levomilnacipran, 2.8% of patients were age 65 or older.
Because levomilnacipran is predominantly excreted by the kidney, renal clearance of levomilnacipran should be considered when determining the dose [see Dosage and Administration (2.3)].
SNRIs, including levomilnacipran, have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse reaction [see Warnings and Precautions (5.11)].
8.6 Hepatic Impairment
Dose adjustment is not recommended in patients with mild (Child-Pugh score of 1 to 6), moderate (Child-Pugh score of 7 to 9), or severe (Child-Pugh score of 10 to 13) hepatic impairment [see  Clinical Pharmacology (12.3) ].
8.7 Renal Impairment
Renal excretion plays a predominant role in the elimination of levomilnacipran.
Levomilnacipran is not recommended for use in patients with end stage renal disease.
Dosing adjustment is recommended for patients with moderate (creatinine clearance of 30 mL/min to 59 mL/min) or severe (creatinine clearance of 15 mL/min to 29 mL/min) renal impairment [see Dosage and Administration (2.3) and  Clinical Pharmacology (12.3)].
Dose adjustment is not recommended for patients with mild (creatinine clearance of 60 mL/min to 89 mL/min) renal impairment [see Clinical Pharmacology (12.3)].
9 Drug Abuse And Dependence
9.1Controlled Substance
Levomilnacipran is not a controlled substance.
9.2Abuse
Levomilnacipran has not been systematically studied in animals or humans for its potential for abuse. There was no evidence suggestive of drug-seeking behavior in the clinical studies. It is not possible to predict on the basis of clinical experience the extent to which a CNS active drug will be misused, diverted, and/or abused once marketed. Consequently, physicians should carefully evaluate patients for a history of drug abuse and follow such patients closely, observing them for signs of misuse or abuse of levomilnacipran (e.g., development of tolerance or drug-seeking behavior).
9.3Dependence
Levomilnacipran has not been systematically studied in animals or humans for its potential for dependence.
10 Overdosage
10.1Human Experience
There is limited clinical experience with levomilnacipran overdose in humans. In clinical studies, cases of ingestions up to 360 mg daily were reported with none being fatal.
10.2 Management of Overdose
No specific antidotes for levomilnacipran are known. In managing overdose, provide supportive care, including close medical supervision and monitoring, and consider the possibility of multiple drug involvement. In case of an overdose, consult a Certified Poison Control Center (1-800-222-1222) for up-to-date guidance and advice. The high volume of distribution of levomilnacipran suggests that dialysis will not be effective in reducing levomilnacipran plasma concentrations.
11 Description
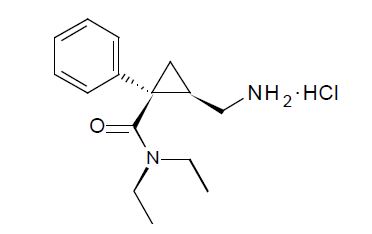
Levomilnacipran extended-release capsules contains levomilnacipran hydrochloride, a selective serotonin and norepinephrine reuptake inhibitor (SNRI), in the form of hydrochloride salt with the chemical name of levomilnacipran hydrochloride is (1S,2R)-2-(aminomethyl)-N,N-diethyl-1-phenylcyclopropanecarboxamide hydrochloride, Its molecular formula is C15H23ClN2O and its molecular weight is 282.8 g/mol. Levomilnacipran (Initial U.S. approval: 2013) is the 1S,2R-enantiomer of milnacipran. The chemical structure of levomilnacipran hydrochloride is:
Levomilnacipran extended-release capsules are intended for oral administration. Each levomilnacipran extended-release capsule contains 23, 45.9, 91.8, or 137.8 mg of levomilnacipran hydrochloride equivalent to 20, 40, 80, or 120 mg of levomilnacipran, respectively. Inactive ingredients include ethylcellulose,  hypromellose, povidone, red iron oxide (80 mg and 120 mg), sugar sphere [sucrose, starch (Biological source: maize) and purified water], talc, triethyl citrate, titanium dioxide and yellow iron oxide (20 mg and 40 mg).
Each capsule is imprinted with black pharmaceutical ink which contains black iron oxide, butyl alcohol, dehydrated alcohol, isopropyl alcohol, potassium hydroxide, propylene glycol, shellac and strong ammonia solution.
12 Clinical Pharmacology
12.1 Mechanism of Action
The exact mechanism of the antidepressant action of levomilnacipran is unknown, but is thought to be related to the potentiation of serotonin and norepinephrine in the central nervous system, through inhibition of reuptake at serotonin and norepinephrine transporters. Non-clinical studies have shown that levomilnacipran is a potent and selective serotonin and norepinephrine reuptake inhibitor (SNRI).
12.2 Pharmacodynamics
Levomilnacipran binds with high affinity to the human serotonin (5-HT) and norepinephrine (NE) transporters (Ki = 11 and 91 nM, respectively) and potently inhibits 5-HT and NE reuptake (IC50 = 16 to 19 and 11 nM, respectively). Levomilnacipran lacks significant affinity for any other receptors, ion channels or transporters tested in vitro, including serotonergic (5HT1-7), őĪ- and ő≤-adrenergic, muscarinic, or histaminergic receptors and Ca2+, Na+, K+ or Cl- channels. Levomilnacipran did not inhibit monoamine oxidase (MAO).
Cardiovascular Electrophysiology
At a dose 2.5 times the maximum recommended dose, levomilnacipran does not prolong QTc to any clinically relevant extent.
12.3 Pharmacokinetics
The concentration of levomilnacipran at steady-state is proportional to dose when administered from 25 mg to 300 mg (2.5 times the maximum recommended dosage of levomilnacipran) once daily. Steady-state concentrations of levomilnacipran are predictable from single-dose data. After daily dosing of levomilnacipran 120 mg, the mean Cmax value is 341 ng/mL, and the mean steady-state AUC value is 5196 ng·h/mL. Interconversion between levomilnacipran and its stereoisomer does not occur in humans.
Absorption
The relative bioavailability of levomilnacipran after administration of levomilnacipran extended-release capsules was 92% when compared to oral solution. The median time to peak concentration (Tmax) of levomilnacipran is 6 to 8 hours after oral administration.
Effect of Food
Levomilnacipran concentration was not significantly affected when levomilnacipran extended-release capsule was administered with food.
Distribution
Levomilnacipran is widely distributed with an apparent volume of distribution of 387 to 473 L; plasma protein binding is 22% over concentration range of 10 to 1,000 ng/mL.
Elimination
Following an oral administration, the mean apparent total clearance of levomilnacipran is 21 to 29 L/h. The apparent terminal elimination half-life of levomilnacipran is approximately 12 hours.
Metabolism
Levomilnacipran undergoes desethylation to form desethyl levomilnacipran and hydroxylation to form p-hydroxy-levomilnacipran. Both oxidative metabolites undergo further conjugation with glucuronide to form conjugates. The desethylation is catalyzed primarily by CYP3A4 with minor contribution by CYP2C8, 2C19, 2D6, and 2J2.
Excretion
Levomilnacipran and its metabolites are eliminated primarily by renal excretion. Following oral administration of 14C-levomilnacipran solution, approximately 58% of the dose is excreted in urine as unchanged levomilnacipran. N-desethyl levomilnacipran is the major metabolite excreted in the urine and accounted for approximately 18% of the dose. Other identifiable metabolites excreted in the urine are levomilnacipran glucuronide (4%), desethyl levomilnacipran glucuronide (3%), p-hydroxy levomilnacipran glucuronide (1%), and p-hydroxy levomilnacipran (1%). The metabolites are inactive [see Dosage and Administration (2.3)].
Drug Interaction Studies
Clinical Studies
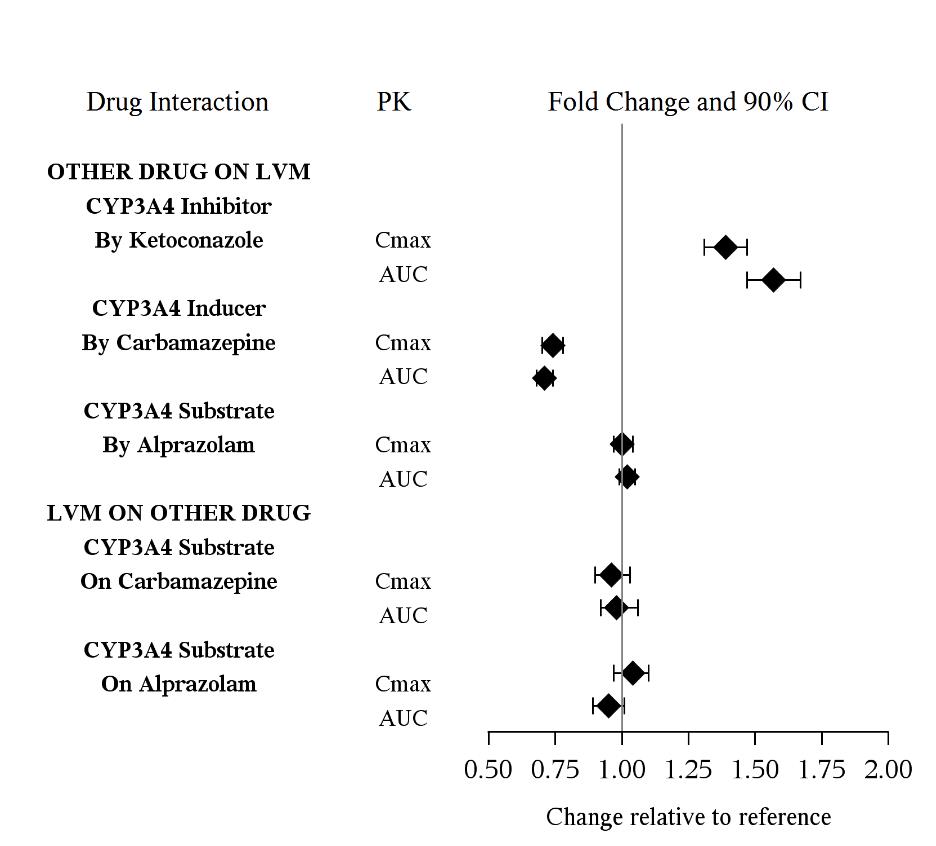
The drug interaction studies for levomilnacipran are summarized in Figure 1.
Figure 1. PK Interactions between Levomilnacipran (LVM) and Other Drugs
­­
In vitro Studies
In vitro studies suggested that CYP2C8, CYP2C19, CYP2D6, and CYP2J2 had minimal contributions to metabolism of levomilnacipran. In addition, levomilnacipran is not a substrate of BCRP, OATP1B1, OATP1B3, OAT1, OAT3, or OCT2 and is a weak substrate of P-gp.
In vitro studies have shown that levomilnacipran is not an inhibitor of CYP1A2, CYP2A6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, P-gp, OATP1B1, OATP1B3, OAT1, OAT3, or OCT2.
Alcohol
An in vitro study indicated increases of levomilnacipran release from levomilnacipran extended-release capsules (20, 40, 80, and 120 mg) at 2 hours by approximately 9.5%, 23% and 56% in the presence of 5%, 20% and 40% (v/v) alcohol, respectively. Effect of 40% alcohol resulted in nearly complete drug release in 4 hours. There is no in vivo study conducted for the effect of alcohol on drug exposure.
Specific Populations
The effect of intrinsic patient factors on the pharmacokinetics of levomilnacipran is presented in Figure 2.
Figure 2 Effect of Intrinsic Factors on Levomilnacipran PK
13 Nonclinical Toxicology
13.1Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Levomilnacipran administered by oral gavage to rats for 2 years and Tg.rasH2 mice for 6 months did not increase the incidence of tumors in either study.
Rats received levomilnacipran at doses up to 90/70 mg/kg/day (the dose was lowered in males after 45 weeks of dosing). The 90 mg/kg/day dose is 7 times the maximum recommended human dose (MRHD) of 120 mg on a mg/m2 basis.
Tg.rasH2 mice received levomilnacipran at doses up to 150 mg/kg/day.
Mutagenesis
Levomilnacipran was not mutagenic in the in vitro bacterial mutation assay (Ames test) and was not clastogenic in an in vivo micronucleus assay in rats. Additionally, levomilnacipran was not genotoxic in the in vitro mouse lymphoma (L5178Y TK+/-) cell forward mutation assay.
Impairment of Fertility
When levomilnacipran was administered orally to male and female rats before mating, through mating and up to Day 7 of gestation at doses up to 100 mg/kg/day, no effects were observed on fertility. This dose is 8 times the MRHD on a mg/m2 basis.
14 Clinical Studies
14.1 Treatment of Major Depressive Disorder
The efficacy of levomilnacipran for the treatment of major depressive disorder (MDD) was established in three 8-week randomized, double-blind, placebo-controlled studies (at doses 40 mg to 120 mg once daily) in adult (18 to 78 years of age) outpatients who met the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria for MDD. Two of the studies were fixed dose (Study 1 and Study 2) and one study was flexible dose (Study 3).
In Study 1, patients received 40 mg (n = 178), 80 mg (n = 179), or 120 mg (n = 180) of levomilnacipran once daily, or placebo (n = 176). In Study 2, patients received either 40 mg (n = 188) or 80 mg (n = 188) of levomilnacipran once daily, or placebo (n = 186). In the flexible-dose study (Study 3), patients received 40 mg to 120 mg (n = 217) of levomilnacipran once daily, or placebo (n = 217) with 21%, 34%, and 44% of levomilnacipran patients on 40 mg, 80 mg, and 120 mg, respectively at the end of their treatment.
In all three studies, levomilnacipran demonstrated superiority over placebo in the improvement of depressive symptoms as measured by the Montgomery-Asberg Depression Rating Scale (MADRS) total score (see Table 6). Levomilnacipran also demonstrated superiority over placebo as measured by improvement in the Sheehan Disability Scale (SDS) functional impairment total score.
Table 6: Summary of Results for the Primary Efficacy Endpoint MADRS
Study Number Treatment Group Mean Baseline Score (SD) LS Mean Change from Baseline (SE) Placebo-subtracted Differencea(95% CI)
Study 1
(fixed dose)
Levomilnacipran (extended-release 40 mg/day)*
36.0 (4.1)
-14.8 (1.0)
-3.2 (-5.9, -0.5)
Levomilnacipran (extended-release 80 mg/day)*
36.1 (3.9)
-15.6 (1.0)
-4.0 (-6.7, -1.3)
Levomilnacipran (extended-release 120 mg/day)*
36.0 (3.9)
-16.5 (1.0)
-4.9 (-7.6, -2.1)
Placebo
35.6 (4.5)
-11.6 (1.0)
--
Study 2 (fixed-dose)
Levomilnacipran (extended-release 40 mg/day)*
30.8 (3.4)
-14.6 (0.8)
-3.3 (-5.5, -1.1)
Levomilnacipran (extended-release 80 mg/day)*
31.2 (3.5)
-14.4 (0.8)
-3.1 (-5.3, -1.0)
Placebo
31.0 (3.8)
-11.3 (0.8)
--
Study 3 (flexible-dose)
Levomilnacipran (extended-release 40 to 120 mg/day)*
35.0 (3.6)
-15.3 (0.8)
-3.1 (-5.3, -0.9)
Placebo
35.2 (3.8)
-12.2 (0.8)
--
SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval unadjusted for multiplicity.
aDifference (drug minus placebo) in least-squares mean change from baseline to endpoint (Week 8).
* Doses statistically significantly superior to placebo.
Post-hoc analyses of the relationships between treatment outcome and age, gender, and race did not suggest any differential responsiveness on the basis of these patient characteristics.
In a maintenance study (Study 4; NCT02288325), adult patients meeting DSM-5 criteria for MDD received flexibly dosed levomilnacipran (40 mg, 80 mg, or 120 mg) once daily for 8 weeks. Responders in the initial 8-week treatment period were eligible to enter a 12-week, open-label, fixed-dose stabilization phase. At the end of stabilization, approximately half of the subjects were receiving 120 mg once daily. Three hundred twenty-four (324) patients who met the response criteria (MADRS total score ‚ȧ 12) after 20 weeks of open-label treatment were randomized to the double-blind treatment phase with levomilnacipran or placebo for 26 weeks. The primary efficacy endpoint was the time from randomization to first relapse during the double-blind phase. Relapse of depressive episode was defined as a MADRS total score ‚Č• 18 at two consecutive visits or insufficient therapeutic response as judged by the investigator. Patients on levomilnacipran experienced a statistically significantly longer time to relapse than patients on placebo (Figure 3).
Figure 3. Kaplan-Meier Estimated Proportion of Patients with Relapse for Adults with MDD (Study 4)
Note: The estimated hazard ratio (95% CI) of levomilnacipran relative to Placebo based on Cox proportional hazards model was 0.56 (95% CI: 0.33, 0.92).
16 How Supplied/storage And Handling
Levomilnacipran extended-release capsules are supplied in the following configurations:
Levomilnacipran Extended-release Capsules, 20 mg are supplied as size ‚Äė4‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on yellow cap and ‚Äú411‚ÄĚ on white body of the capsules with black ink, filled with white to off-white¬†pellets.
They are available as follows:
Bottles of 30:                        NDC 65162-411-03
Levomilnacipran Extended-release Capsules, 40 mg are supplied as size ‚Äė3‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on yellow cap and ‚Äú414‚ÄĚ on yellow body of the capsules with black ink, filled with white to off-white¬†pellets.
They are available as follows:
Bottles of 30:                        NDC 65162-960-03
Levomilnacipran Extended-release Capsules, 80 mg are supplied as size ‚Äė2‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on pink cap and ‚Äú437‚ÄĚ on white body of the capsules with black ink, filled with white to off-white¬†pellets.
They are available as follows:
Bottles of 30:                        NDC 65162-437-03
Levomilnacipran Extended-release Capsules, 120 mg are supplied as size ‚Äė1‚Äô capsules, imprinted with ‚ÄúAN‚ÄĚ on pink cap and ‚Äú455‚ÄĚ on pink body of the capsules with black ink, filled with white to off-white¬†pellets.
They are available as follows:
Bottles of 30:                        NDC 65162-455-03
Storage and Handling
All package configurations: ¬†Store at 20¬į to 25¬įC (68¬į to 77¬įF); excursions permitted between 15¬į to 30¬įC (59¬į to 86¬įF) [see USP Controlled Room Temperature].
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Suicide Thoughts and Behaviors
Advise patients and caregivers to look for the emergence of suicidal thoughts and behaviors, especially early during treatment and when the dose is adjusted up or down and instruct them to report such symptoms to the healthcare provider [see Boxed Warning and Warnings and Precautions (5.1)].
Dosing and Administration
Advise patients that levomilnacipran extended-release capsules should be swallowed whole and should not be chewed, crushed, or opened.  
Advise patients that levomilnacipran extended-release capsules can be taken with or without food.
Instruct patients if they miss a dose, to take the missed dose as soon as they remember. If it is almost time for the next dose, instruct them to skip the missed dose and take their next dose at the regular time. Advise them not to take two doses of levomilnacipran at the same time.
Concomitant Medication
Instruct patients not to take levomilnacipran with an MAOI or within 14 days of stopping an MAOI and to allow 7 days after stopping levomilnacipran before starting an MAOI [see Contraindications (4)]. Advise patients to inform their physician if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for drug-drug interactions [see Drug Interactions (7.1)].
Allergic Reactions
Advise patients to notify their healthcare provider if they develop an allergic reaction such as rash, hives, swelling, or difficulty breathing [see Contraindications (4)].
Serotonin Syndrome
Caution patients about the risk of serotonin syndrome, particularly with the concomitant use of levomilnacipran with other serotonergic agents (including triptans, tricyclic antidepressants, opioids, lithium, amphetamines, tryptophan, buspirone, and St. John’s Wort supplements) [see Warnings and Precautions (5.2) and Drug Interactions (7.1)]. Instruct patients to contact their health care provider or report to the emergency room if they experience signs or symptoms of serotonin syndrome.
Elevated Blood Pressure and Heart Rate
Advise patients that they should have regular monitoring of blood pressure and heart rate when taking levomilnacipran [see Warnings and Precautions (5.3, 5.4)].
Increased Risk of Bleeding
Caution patients about the concomitant use of levomilnacipran and NSAIDs, aspirin, warfarin, or other drugs that affect coagulation because combined use has been associated with an increased risk of bleeding. Advise patients to inform their healthcare provider if they are taking or planning to take any prescription or over-the-counter medications that increase the risk of bleeding [see Warnings and Precautions (5.5)].
Angle Closure Glaucoma
Patients should be advised that taking levomilnacipran can cause mild pupillary dilation, which in susceptible individuals, can lead to an episode of angle closure glaucoma [see Warnings and Precautions (5.6)].
Urinary Hesitation or Retention
Caution patients about the risk of urinary hesitation and retention while taking levomilnacipran, particularly in patients prone to obstructive urinary disorders. Instruct patients to consult with their healthcare provider if they develop any problems with urine flow [see Warnings and Precautions (5.7)].
Activation of Mania/Hypomania
Advise patients and their caregivers to look for signs of activation of mania/hypomania [see Warnings and Precautions (5.8)].
Seizures
Caution patients about using levomilnacipran if they have a history of a seizure disorder [see Warnings and Precautions (5.9)].
Discontinuation Syndrome
Advise patients not to abruptly stop taking levomilnacipran without first talking with their healthcare provider. Patients should be aware that discontinuation effects may occur when suddenly stopping levomilnacipran and they should monitor for discontinuation symptoms [see Warnings and Precautions (5.10)].
Hyponatremia
Advise patients that hyponatremia has been reported as a result of treatment with levomilnacipran. Advise patients of the signs and symptoms of hyponatremia [see Warnings and Precautions (5.11)].
Sexual Dysfunction
Advise patients that use of levomilnacipran may cause symptoms of sexual dysfunction in both male and female patients. Inform patients that they should discuss any changes in sexual function and potential management strategies with their healthcare provider [see Warnings and Precautions (5.12)].
Alcohol
Advise patients to avoid consumption of alcohol while taking levomilnacipran [see Drug Interactions (7.1), Clinical Pharmacology (12.3)].
Pregnancy
- Advise pregnant females to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with levomilnacipran.
- Advise patients that levomilnacipran may increase the risk of neonatal complications requiring prolonged hospitalization, respiratory support, tube feeding.
- Advise patient that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to levomilnacipran during pregnancy [see Use in Specific Populations (8.1)]
Lactation
Advise breastfeeding patients using levomilnacipran to monitor infants for sedation, agitation, irritability, poor feeding and poor weight gain and to seek medical care if they notice these signs [see Use in Specific Populations (8.2)].
Interference with Cognitive and Motor Performance
Caution patients about operating hazardous machinery, including automobiles, until they are reasonably certain that levomilnacipran therapy does not adversely affect their ability to engage in such activities.
Manufactured by: Amneal Pharmaceuticals Pvt. Ltd. Ahmedabad 382220, INDIA
Distributed by: Amneal Pharmaceuticals LLC Bridgewater, NJ 08807
Rev. 11-2023-04
Medication Guide
¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† ¬† Levomilnacipran (lee‚ÄĚ voe mil na‚Äô si pran) Extended-Release Capsules¬†¬†
What is the most important information I should know about  levomilnacipran extended-release capsules?
Levomilnacipran extended-release capsules  may cause serious side effects,  including:
- Increased risk of suicidal thoughts and actions. Levomilnacipran extended-release capsules and other antidepressant medicines may increase suicidal thoughts and actions in some people 24 years and younger, especially within the first few months of treatment or when the dose is changed. Levomilnacipran extended-release capsules are not for use in children.
- Depression or other mental illnesses are the most important causes of suicidal thoughts or actions.
How can I watch for and try to prevent suicidal thoughts and actions?
- Pay close attention to any changes, especially sudden changes in mood, behavior, thoughts, or feelings, or if you develop suicidal thoughts or actions. This is very important when an antidepressant medicine is started or when the dose is changed.
- Call your healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings or if you develop suicidal thoughts or actions.
- Keep all follow-up visits with your healthcare provider as scheduled. Call your healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call your healthcare provider  or get emergency medical help right away if you or your family member have any of the following symptoms, especially if they are new, worse, or worry you:
- attempts to commit suicide
- acting on dangerous impulses 
-  acting aggressive, being angry or violent
- thoughts about suicide or dying
- new or worse depression
- new or worsening anxiety
- panic attacks
- feeling very agitated or restless 
-  new or worse irritability
-  trouble sleeping
- an extreme increase in activity or talking (mania)
-  other unusual changes in behavior or mood
What are levomilnacipran extended-release capsules?
Levomilnacipran extended-release capsules are a prescription medicine used to treat a certain type of depression called Major Depressive Disorder (MDD) in adults.
It is not known if levomilnacipran extended-release capsules are safe and effective for use in children.
It is not known if levomilnacipran extended-release capsules are safe and effective for the management of fibromyalgia. Levomilnacipran extended-release capsules are not for use for the management of fibromyalgia.
Do not take levomilnacipran extended-release capsules if you:
- are allergic to levomilnacipran, milnacipran HCl, or any of the ingredients in levomilnacipran extended-release capsules. See the end of this Medication Guide for a complete ul of ingredients in levomilnacipran extended-release capsules.
- are taking or have taken within the last 14 days, a medicine called a monoamine oxidase inhibitor (MAOI), including the antibiotic linezolid or intravenous methylene blue.
Ask your healthcare provider or pharmacist if you are not sure if you take an MAOI, including the antibiotic linezolid or intravenous methylene blue.
Do not start taking an MAOI for at least 7 days after you stop treatment with levomilnacipran extended-release capsules.
Before taking levomilnacipran extended-release capsules, tell your healthcare provider  about all your medical conditions, including if you: 
- have or have a family history of suicide, depression, bipolar disorder, mania, or hypomania
- have high blood pressure
- have or had heart problems, including fast heartbeat, or stroke
- have or had bleeding problems
- have glaucoma (high pressure in the eye)
- have or had problems urinating (hesitation) or emptying your bladder (retention)
- have or had seizures (convulsions)
- have low sodium levels in your blood
- have or had kidney problems
- drink alcohol
- are pregnant or plan to become pregnant. Levomilnacipran extended-release capsules may harm your unborn baby. Taking levomilnacipran extended-release capsules during your third trimester of pregnancy may cause you to have an increased risk of bleeding after your delivery and may also cause your baby to be at increased risk for withdrawal symptoms, or breathing, temperature control, feeding or other problems at birth. Talk to your healthcare provider about the risks to you and your baby if you take levomilnacipran extended-release capsules during pregnancy.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with levomilnacipran extended-release capsules.
- There is a pregnancy registry for women who are exposed to levomilnacipran extended-release capsules during pregnancy. The purpose of the registry is to collect information about the health of women exposed to levomilnacipran extended-release capsules and their baby. If you become pregnant during treatment with levomilnacipran extended-release capsules, talk to your healthcare provider about registering with the National Pregnancy Registry for Antidepressants at 1-844-405-6185 or visit online at https://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/antidepressants/.
- are breastfeeding or plan to breastfeed. It is not known if levomilnacipran passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby during treatment with levomilnacipran extended-release capsules.
- If you breastfeed during treatment with levomilnacipran extended-release capsules, call your healthcare provider if your baby develops sleepiness or fussiness, or is not feeding or gaining weight well.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Levomilnacipran extended-release capsules and other medicines may affect each other causing possible serious side effects.
Levomilnacipran extended-release capsules may affect the way other medicines work and other medicines may affect the way levomilnacipran extended-release capsules works.
Especially tell your healthcare provider if you take:
- MAOIs
- medicines used to treat migraine headache known as triptans
- tricyclic antidepressants
- lithium
- tramadol, fentanyl, meperidine, methadone, or other opioids
- tryptophan
- buspirone
- amphetamines
- St. John’s Wort
- medicines that can affect blood clotting such as aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) and warfarin
- diuretics
- medicines used to treat mood, anxiety, psychotic or thought disorders, including selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs)
Ask your healthcare provider if you are not sure if you are taking any of these medicines. Your healthcare provider can tell you if it is safe to take levomilnacipran extended-release capsules with your other medicines.
Do not start or stop any other medicines during treatment with levomilnacipran extended-release capsules without talking to your healthcare provider first. Stopping levomilnacipran extended-release capsules suddenly may cause you to have serious side effects. See, ‚ÄúWhat are the possible side effects of levomilnacipran extended-release capsules?‚ÄĚ
Know the medicines you take. Keep a ul of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take levomilnacipran extended-release capsules?
- Take levomilnacipran extended-release capsules exactly as your healthcare provider tells you to take it. Do not change your dose or stop taking levomilnacipran extended-release capsules without first talking to your healthcare provider.
- Your healthcare provider may need to change the dose of levomilnacipran extended-release capsules until it is the right dose for you.
- Take levomilnacipran extended-release capsules one time each day at about the same time each day.
- Take levomilnacipran extended-release capsules with or without food.
- Swallow levomilnacipran extended-release capsules whole. Do not open, chew, or crush the levomilnacipran extended-release capsules.
- If you miss a dose of levomilnacipran extended-release capsules, take the missed dose as soon as you remember. If it is almost time for the next dose, skip the missed dose and take your next dose at the regular time. Do not take 2 doses of levomilnacipran extended-release capsules at the same time.
- If you take too much levomilnacipran extended-release capsules, call your healthcare provider or poison control center at 1-800-222-1222, or go to the nearest hospital emergency room right away. 
What should I avoid while taking levomilnacipran extended-release capsules?
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how levomilnacipran extended-release capsules affects you. Levomilnacipran extended-release capsules can cause sleepiness or may affect your ability to make decisions, think clearly, or react quickly.
- Avoid drinking alcohol during treatment with levomilnacipran extended-release capsules.
What are the possible side effects of levomilnacipran extended-release capsules?
Levomilnacipran extended-release capsules may cause serious side effects, including:
- See¬†‚ÄúWhat is the most important information I should know about levomilnacipran extended-release capsules?‚ÄĚ
- Serotonin syndrome. A potentially life-threatening problem called serotonin syndrome can happen when levomilnacipran extended-release capsules is taken with certain other medicines. See ‚ÄúDo not take levomilnacipran extended-release capsules if you.‚ÄĚ Call your healthcare provider or go to the nearest hospital emergency room right away if you have any of the following signs and symptoms of serotonin syndrome:
- agitation
- seeing or hearing things that are not real (hallucinations)
- confusion
- coma
- fast heartbeat
- blood pressure changes
- dizziness
- sweating
- flushing
- high body temperature (hyperthermia)
- tremors, stiff muscles, or muscle twitching
- loss of coordination
- seizures
- nausea, vomiting, diarrhea
- High blood pressure (hypertension). Your healthcare provider should check your blood pressure before you start and during treatment with levomilnacipran extended-release capsules. If you have high blood pressure, it should be controlled before you start treatment with levomilnacipran extended-release capsules.
- Increased heart rate. Your healthcare provider should check your heart rate before you start and during treatment with levomilnacipran extended-release capsules. If you have heart problems or problems with an abnormal heartbeat, your problems should be treated before you start treatment with levomilnacipran extended-release capsules.
- Increased risk of bleeding. Taking levomilnacipran extended-release capsules with aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), warfarin or blood thinners may add to this risk. Tell your healthcare provider right away about any unusual bleeding or bruising.
- Eye problems (angle-closure glaucoma). Levomilnacipran extended-release capsules, may cause a type of eye problem called angle-closure glaucoma in people with certain eye problems. You may want to undergo an eye examination to see if you are at risk and receive preventative treatment if you are. Call your healthcare provider if you have changes in your vision, eye pain, or swelling or redness in or around the eye.
- Problems with urination. Levomilnacipran extended-release capsules may cause you to have problems with urination including decreased urine flow and being unable to pass any urine. Tell your healthcare provider if you develop any problems with urine flow during treatment with levomilnacipran extended-release capsules.
- Manic episodes. Manic episodes may happen in people with bipolar disorder who take levomilnacipran extended-release capsules. Symptoms may include:
- greatly increased energy
- severe trouble sleeping
- racing thoughts
- reckless behavior
- unusually grand ideas
- excessive happiness or irritability
- talking more or faster than usual
 
- Seizures (convulsions).
- Discontinuation syndrome. Suddenly stopping levomilnacipran extended-release capsules may cause you to have serious side effects. Your healthcare provider may want to decrease your dose slowly. Symptoms may include:
- changes in your mood
- headache
- irritability and agitation
- tiredness
- dizziness
- problems sleeping
- electric shock sensation (paresthesia)
- hypomania
- anxiety
- ringing in your ears (tinnitus)
- confusion
- seizures
Low sodium levels in your blood (hyponatremia). Low sodium levels in your blood that may be serious and may cause death can happen during treatment with levomilnacipran extended-release capsules. Elderly people and people who take certain medicines may be at greater risk for this. Signs and symptoms may include:
- headache
- difficulty concentrating
- memory changes
- confusion
- weakness and unsteadiness on your feet which can lead to falls
 
In more severe or more sudden cases, signs and symptoms include:
- hallucinations (seeing or hearing things that are not real)
- fainting
- seizures
- coma
- stopping breathing (respiratory arrest)
 
- Sexual problems (dysfunction). Taking levomilnacipran extended-release capsules, may cause sexual problems. Symptoms in males may include:
- delayed ejaculation or inability to have an ejaculation
- decreased sex drive
- problems getting or keeping an erection
Symptoms in females may include:
- decreased sex drive
- delayed orgasm or inability to have an orgasm
Talk to your healthcare provider if you develop any changes in your sexual function or if you have any questions or concerns about sexual problems during treatment with levomilnacipran extended-release capsules. There may be treatments your healthcare provider can suggest.
The most common side effects of levomilnacipran extended-release capsules, include:
- nausea
- problems getting or keeping an erection
 
- constipation
 
- delayed ejaculation or inability to have an ejaculation
- sweating
- vomiting
- increased heart rate
- fast or irregular heartbeat (palpitations)
These are not all the possible side effects of levomilnacipran extended-release capsules.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store levomilnacipran extended-release capsules?
- Store levomilnacipran extended-release capsules at room temperature between 68¬į to 77¬įF (20¬į to 25¬įC).
- Keep levomilnacipran extended-release capsules and all medicines out of the reach of children.
General information about the safe and effective use of levomilnacipran extended-release capsules
Medicines are sometimes prescribed for purposes other than those uled in a Medication Guide. Do not use levomilnacipran extended-release capsules for a condition for which it was not prescribed. Do not give levomilnacipran extended-release capsules to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about levomilnacipran extended-release capsules that is written for healthcare professionals.
What are the ingredients in levomilnacipran extended-release capsules?
Active ingredient: levomilnacipran hydrochloride
Inactive ingredients: ethylcellulose, hypromellose, povidone, red iron oxide (80 mg and 120 mg), sugar sphere [sucrose, starch (Biological source: maize) and purified water], talc, triethyl citrate, titanium dioxide and yellow iron oxide (20 mg and 40 mg).
Each capsule is imprinted with black pharmaceutical ink which contains black iron oxide, butyl alcohol, dehydrated alcohol, isopropyl alcohol, potassium hydroxide, propylene glycol, shellac and strong ammonia solution.
For more information, go to www.amneal.com or call 1-877-835-5472.
This Medication Guide has been approved by the U.S. Food and Drug Administration. Manufactured by:
Amneal Pharmaceuticals Pvt. Ltd. Ahmedabad 382220, INDIA Distributed by:
Amneal Pharmaceuticals LLC Bridgewater, NJ 08807
Rev. 11-2023-04
Principal Display Panel
NDC 65162-411-03
Levomilnacipran Extended-Release Capsules, 20 mg
Rx only
30 Capsules
Amneal Pharmaceuticals LLC
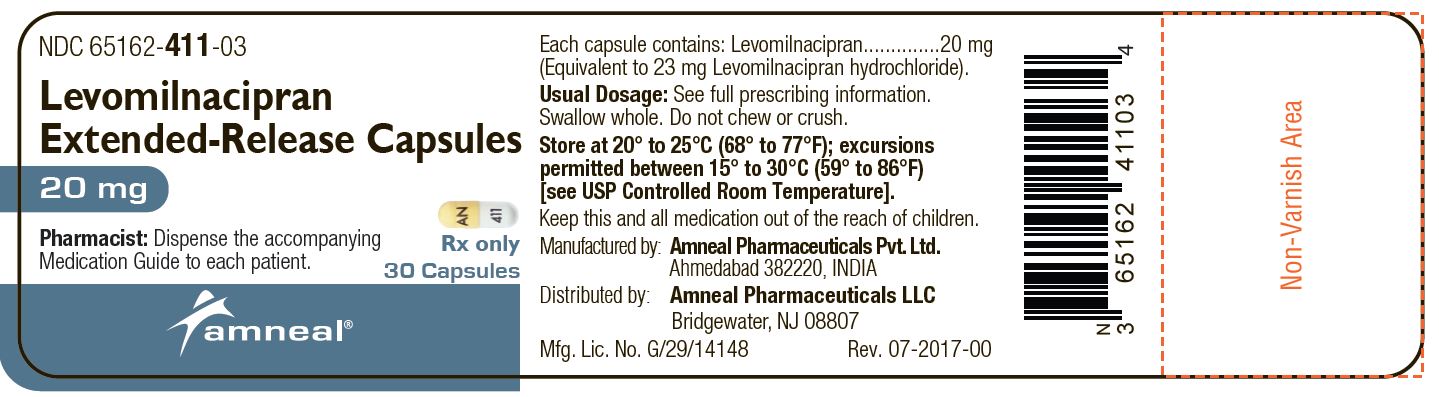
 
NDC 65162-960-03
Levomilnacipran Extended-Release Capsules, 40 mg
Rx only
30 Capsules
Amneal Pharmaceuticals LLC
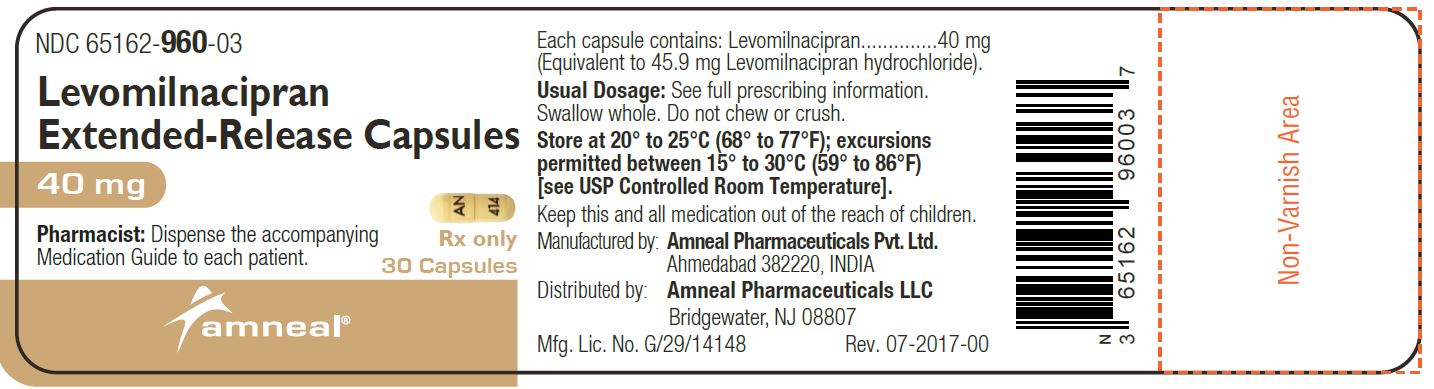
 
NDC 65162-437-03
Levomilnacipran Extended-Release Capsules, 80 mg
Rx only
30 Capsules
Amneal Pharmaceuticals LLC
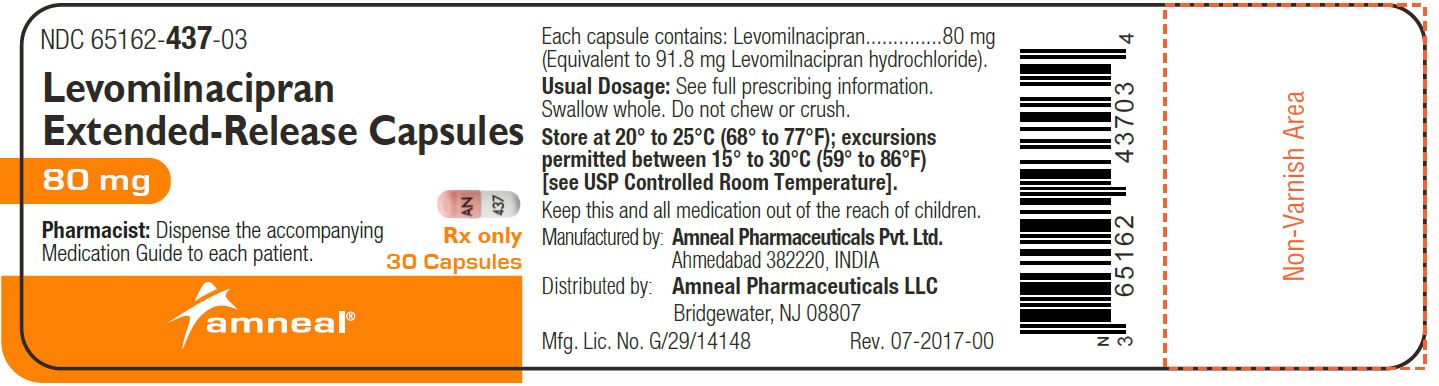
 
NDC 65162-455-03
Levomilnacipran Extended-Release Capsules, 120 mg
Rx only
30 Capsules
Amneal Pharmaceuticals LLC
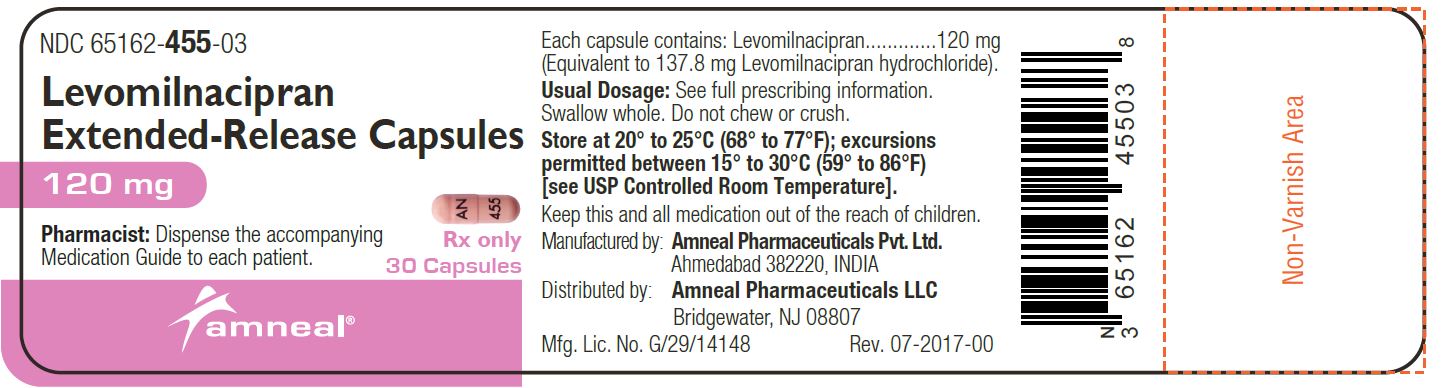
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


