Tri-Legest Fe Dailymed
Generic: norethindrone acetate and ethinyl estradiol is used for the treatment of Anemia, Hemolytic Anemia, Megaloblastic Hemochromatosis Hemosiderosis Pregnancy Complications, Hematologic Anemia, Iron-Deficiency Acne Vulgaris Breast Neoplasms Endometrial Hyperplasia Endometriosis Hypogonadism Liver Diseases Menorrhagia Osteoporosis Pregnancy Pulmonary Embolism Thromboembolism Thrombophlebitis Uterine Hemorrhage Venous Thrombosis Cerebral Arterial Diseases Coronary Artery Disease Hypertension Menopause, Premature Neoplasms, Hormone-Dependent Prostatic Neoplasms Osteoporosis, Postmenopausal Primary Ovarian Insufficiency Endometrial Neoplasms Hot Flashes Tobacco Use
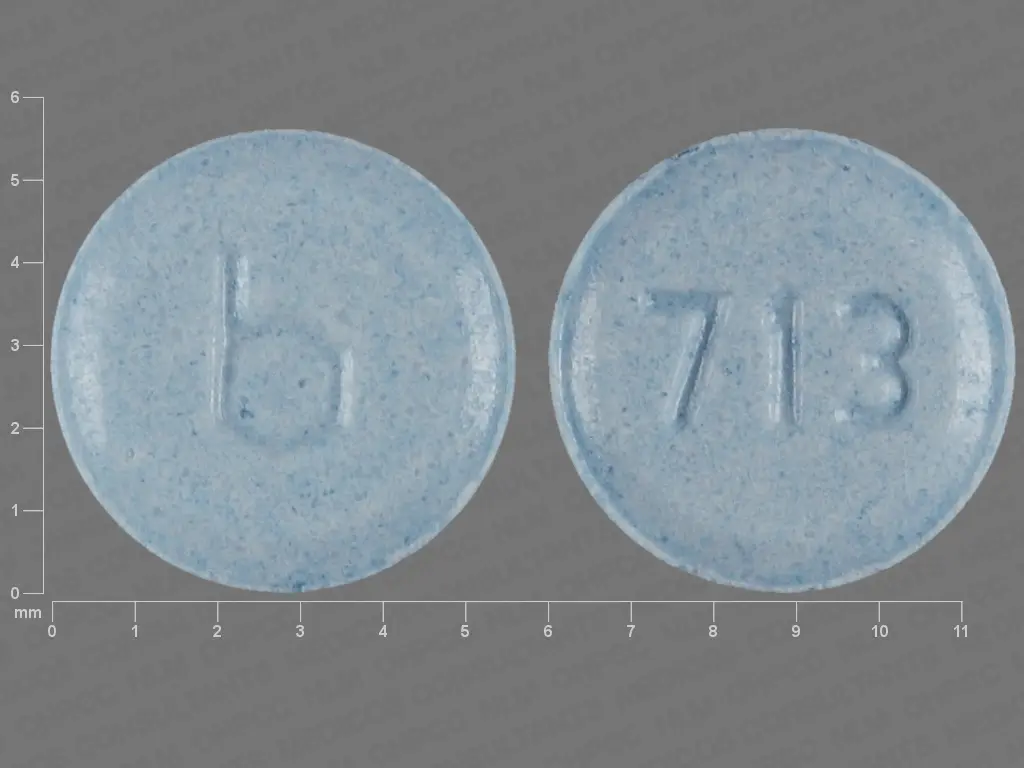
IMPRINT: B 713
SHAPE: round
COLOR: blue
All Imprints
norethindrone acetate 1 mgethinyl estradiol 20 ug - b 711 round pink
norethindrone acetate 1 mgethinyl estradiol 30 ug - b 712 round yellow
norethindrone acetate 1 mgethinyl estradiol 35 ug - b 713 round blue
- b 247 round brown
Boxed Warning
Warning: Cigarettesmoking And Serious Cardiovascular Events:
Go PRO for all pill images
Warning: Cigarettesmoking And Serious Cardiovascular Events:
Cigarette smoking increases the risk of serious cardiovascular side effects from combined oral contraceptive (COC) use. This risk increases with age, particularly in women over 35 years of age, and with the number of cigarettes smoked. For this reason, COCs, including norethindrone acetate and ethinyl estradiol tablets, are contraindicated in women who are over 35 years of age and smoke.
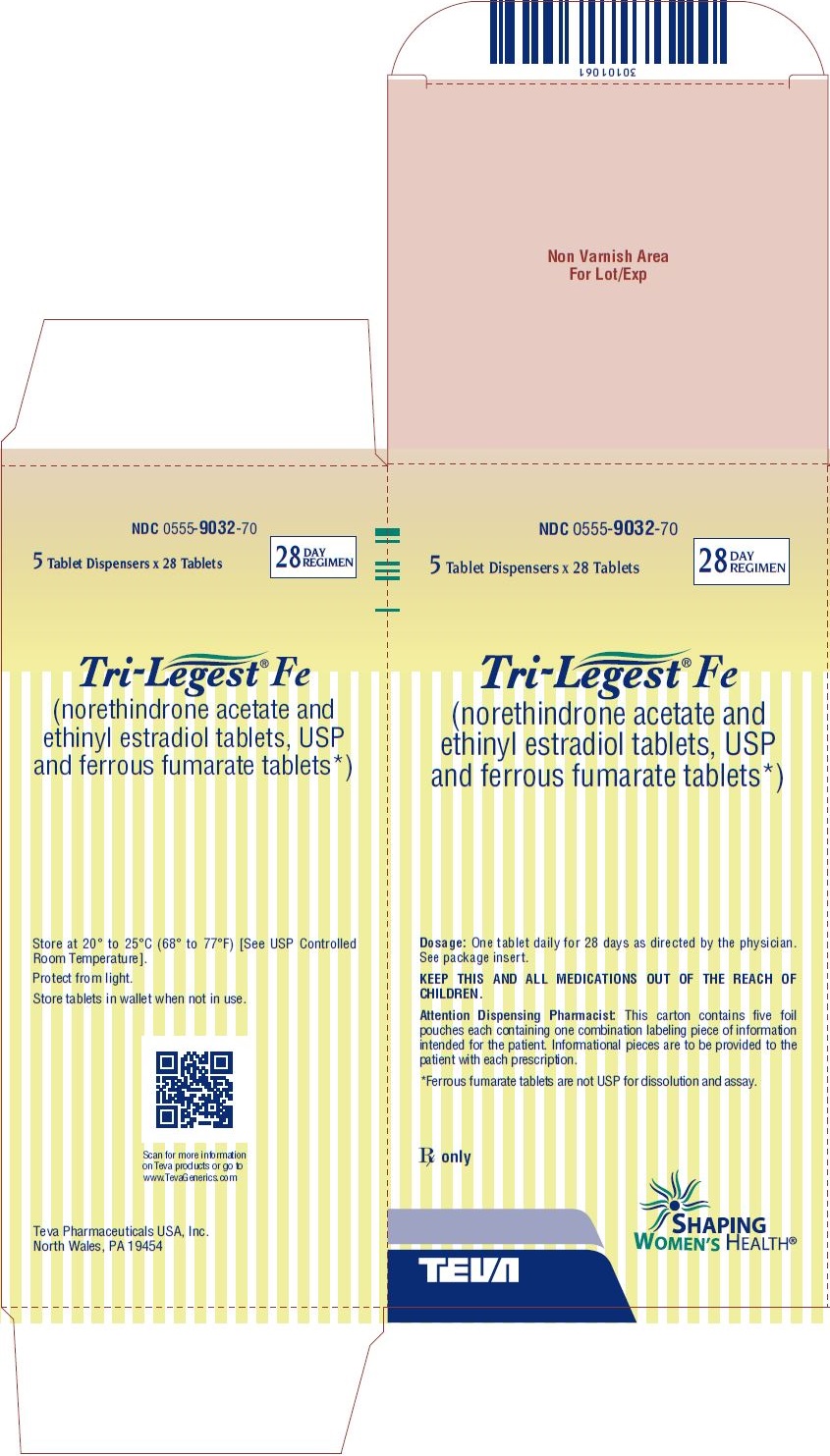
Tri-Legest® Fe
(Each light pink tablet contains 1 mg norethindrone acetate and 20 mcg ethinyl estradiol; each light yellow tablet contains 1 mg norethindrone acetate and 30 mcg ethinyl estradiol; each light blue tablet contains 1 mg norethindrone acetate and 35 mcg ethinyl estradiol; each brown tablet contains 75 mg ferrous fumarate.)
Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Description
Tri-Legest® Fe (norethindrone acetate and ethinyl estradiol tablets, USP and ferrous fumarate tablets [not USP]) is a graduated estrophasic combined oral contraceptive providing estrogen in a graduated sequence over a 21-day period with a constant dose of progestogen.
Tri-Legest® Fe provides for a continuous dosage regimen consisting of 21 oral contraceptive tablets and seven ferrous fumarate tablets. The ferrous fumarate tablets are present to facilitate ease of drug administration via a 28-day regimen, are non-hormonal, and do not serve any therapeutic purpose.
Each light pink tablet contains 1 mg norethindrone acetate [(17α)-17-(acetyloxy)-19-norpregna-4-en-20-yn-3-one] and 20 mcg ethinyl estradiol [(17α)-19-norpregna-1,3,5(10)-trien-20-yne-3,17-diol] Each light pink tablet contains the following inactive ingredients: calcium stearate, FD&C red no. 40 aluminum lake, lactose monohydrate, microcrystalline cellulose, pregelatinized corn starch, and sodium starch glycolate.
Each light yellow tablet contains 1 mg norethindrone acetate and 30 mcg ethinyl estradiol. Each light yellow tablet contains the following inactive ingredients: calcium stearate, D&C yellow no.10 aluminum lake, lactose monohydrate, microcrystalline cellulose, pregelatinized corn starch, and sodium starch glycolate.
Each light blue tablet contains 1 mg norethindrone acetate and 35 mcg ethinyl estradiol. Each light blue tablet contains the following inactive ingredients: calcium stearate, FD&C blue no. 2 aluminum lake, lactose monohydrate, microcrystalline cellulose, pregelatinized corn starch, and sodium starch glycolate.
Each brown tablet contains crospovidone, ferrous fumarate, hydrogenated vegetable oil, and microcrystalline cellulose.
The structural formulas are as follows:

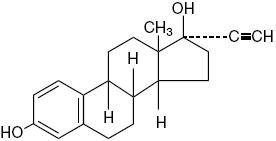
Norethindrone Acetate                          Ethinyl Estradiol
C22H28O3 Â Molecular Weight: 340.46Â Â Â Â Â Â Â Â Â Â C20H24O2Â Â Molecular Weight: 296.40Â
Each Tri-Legest® Fe tablet dispenser contains five light pink tablets, seven light yellow tablets, nine light blue tablets, and seven brown tablets. These tablets are to be taken in the following order: one light pink tablet each day for five days, then one light yellow tablet each day for seven days, followed by one light blue tablet each day for nine days, and then one brown tablet each day for seven days.
Clinical Pharmacology
ORAL CONTRACEPTION
Combined oral contraceptives act by suppression of gonadotropins. Although the primary mechanism of this action is inhibition of ovulation, other alterations include changes in the cervical mucus (which increase the difficulty of sperm entry into the uterus) and the endometrium (which reduce the likelihood of implantation).
In vitro and animal studies have shown that norethindrone combines high progestational activity with low intrinsic androgenicity. In humans, norethindrone acetate in combination with ethinyl estradiol does not counteract estrogen-induced increases in sex hormone binding globulin (SHBG). Following multiple-dose administration of norethindrone acetate and ethinyl estradiol, serum SHBG concentrations increase two- to three-fold and free testosterone concentrations decrease by 47% to 64%, indicating minimal androgenic activity.
ACNE
Acne is a skin condition with a multifactorial etiology, including androgen stimulation of sebum production. While the combination of norethindrone acetate and ethinyl estradiol increases sex hormone binding globulin (SHBG) and decreases free testosterone, the relationship between these changes and a decrease in the severity of facial acne in otherwise healthy women with this skin condition has not been established.
Pharmacokinetics
Norethindrone acetate appears to be completely and rapidly deacetylated to norethindrone after oral administration, since the disposition of norethindrone acetate is indistinguishable from that of orally administered norethindrone. Norethindrone acetate and ethinyl estradiol are rapidly absorbed, with maximum plasma concentrations of norethindrone and ethinyl estradiol occurring 1 to 2 hours post-dose. Both are subject to first-pass metabolism after oral dosing, resulting in an absolute bioavailability of approximately 64% for norethindrone and 43% for ethinyl estradiol.
Administration of norethindrone acetate/ethinyl estradiol with a high fat meal decreases rate, but not extent, of ethinyl estradiol absorption. The extent of norethindrone absorption is increased by 27% following administration with food.
Plasma concentrations of norethindrone and ethinyl estradiol following chronic administration of norethindrone acetate and ethinyl estradiol to 17 women are shown below (Figure 1). Mean steady-state concentrations of norethindrone for the 1/20, 1/30, and 1/35 tablet strengths increased as ethinyl estradiol dose increased over the 21-day dose regimen, due to dose-dependent effects of ethinyl estradiol on serum SHBG concentrations (Table 1). Mean steady-state plasma concentrations of ethinyl estradiol for the 1/20, 1/30, and 1/35 tablet strengths were proportional to ethinyl estradiol dose (Table 1).
Figure 1. Mean Steady-State Plasma Ethinyl Estradiol and Norethindrone Concentrations Following Chronic Administration of Norethindrone Acetate and Ethinyl Estradiol
Table 1. Mean (SD) Steady-State Pharmacokinetic Parameters Following Chronic Administration of Norethindrone Acetate and Ethinyl Estradiol*
Norethindrone Acetate/
Ethinyl Estradiol Dose
Cycle
Day
Cmax
AUC
CL/F
SHBG â€
Norethindrone
mg/µg
ng/mL
ngâ–Şhr/mL
mL/min
nmol/L
1/20
5
10.8
81.1
220
120
(3.9)
(28.5)
(137)
(33)
1/30
12
12.7
102
166
139
(4.1)
(32)
(85)
(42)
1/35
21
12.7
109
152
163
(4.1)
(32)
(73)
(40)
Ethinyl Estradiol
mg/µg
pg/mL
pgâ–Şhr/mL
mL/min
nmol/L
1/20
5
61.0
661
549
(16.8)
(190)
(171)
1/30
12
92.4
973
546
(26.9)
(293)
(199)
1/35
21
113
1149
568
(44)
(372)
(219)
* Cmax = Maximum plasma concentration; AUC (0 to 24) = Area under the plasma concentration-time curve over the dosing interval; CL/F = Apparent oral clearance †Mean (SD) baseline value = 55 (29) nmol/LÂ
No age-related differences were seen in plasma concentrations of ethinyl estradiol and norethindrone following administration of norethindrone acetate and ethinyl estradiol to 119 postmenarchal women ages 15 to 48 years.
Volume of distribution of norethindrone and ethinyl estradiol ranges from 2 to 4 L/kg. Plasma protein binding of both steroids is extensive (>95%); norethindrone binds to both albumin and sex hormone binding globulin, whereas ethinyl estradiol binds only to albumin. Although ethinyl estradiol does not bind to SHBG, it induces SHBG synthesis. Norethindrone acetate and ethinyl estradiol increases serum SHBG concentrations two- to three-fold (Table 1).
Norethindrone undergoes extensive biotransformation, primarily via reduction, followed by sulfate and glucuronide conjugation. The majority of metabolites in the circulation are sulfates, with glucuronides accounting for most of the urinary metabolites. A small amount of norethindrone acetate is metabolically converted to ethinyl estradiol. Ethinyl estradiol is also extensively metabolized, both by oxidation and by conjugation with sulfate and glucuronide. Sulfates are the major circulating conjugates of ethinyl estradiol and glucuronides predominate in urine. The primary oxidative metabolite is 2-hydroxy ethinyl estradiol, formed by the CYP3A4 isoform of cytochrome P450. Part of the first-pass metabolism of ethinyl estradiol is believed to occur in gastrointestinal mucosa. Ethinyl estradiol may undergo enterohepatic circulation.
Norethindrone and ethinyl estradiol are excreted in both urine and feces, primarily as metabolites. Plasma clearance values for norethindrone and ethinyl estradiol are similar (approximately 0.4 L/hr/kg). Steady-state elimination half-lives of norethindrone and ethinyl estradiol following administration of norethindrone acetate and ethinyl estradiol are approximately 13 hours and 19 hours, respectively.
Special Population
The effect of race on the disposition of norethindrone acetate and ethinyl estradiol has not been evaluated.
The effect of renal disease on the disposition of norethindrone acetate and ethinyl estradiol has not been evaluated. In premenopausal women with chronic renal failure undergoing peritoneal dialysis who received multiple doses of a combined oral contraceptive containing ethinyl estradiol and norethindrone, plasma ethinyl estradiol concentrations were higher and norethindrone concentrations were unchanged compared to concentrations in premenopausal women with normal renal function.
The effect of hepatic disease on the disposition of norethindrone acetate and ethinyl estradiol has not been evaluated. However, ethinyl estradiol and norethindrone may be poorly metabolized in patients with impaired liver function.
Drug-Drug Interactions
Numerous drug-drug interactions have been reported for combined oral contraceptives. A summary of these is found under PRECAUTIONS, Drug Interactions .
Indications And Usage
Tri-Legest® Fe (norethindrone acetate and ethinyl estradiol tablets, USP and ferrous fumarate tablets [not USP]) is indicated for the prevention of pregnancy in women who elect to use combined oral contraceptives as a method of contraception.
Tri-Legest® Fe is indicated for the treatment of moderate acne vulgaris in females, ≥15 years of age, who have no known contraindications to combined oral contraceptive therapy, desire oral contraception, have achieved menarche, and are unresponsive to topical anti-acne medications. Tri-Legest® Fe should be used for the treatment of acne only if the patient desires a combined oral contraceptive for birth control and plans to stay on it for at least 6 months.
Combined oral contraceptives are highly effective for pregnancy prevention. Table 2 uls the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.
Table 2. Percentage of Women Experiencing an Unintended Pregnancy During the First Year of Typical Use and the First Year of Perfect Use of Contraception and the Percentage Continuing Use at the End of the First Year. United States.
% of Women Experiencing an Unintended Pregnancy within the First Year of Use
% of Women Continuing Use at One Year‡
Method
Typical Use*
Perfect Useâ€
(1)
(2)
(3)
(4)
Chance§
85
85
Spermicides¶
26
6
40
Periodic Abstinence
25
63
Calendar
9
Ovulation Method
3
Symptothermal#Ăž
2
Post-ovulation
1
CapĂź
Parous Women
40
26
42
Nulliparous Women
20
9
56
Sponge
Parous Women
40
20
42
Nulliparous Women
20
9
56
DiaphragmĂź
20
6
56
Withdrawal
19
4
CondomĂ
Female (Reality)
21
5
56
Male
14
3
61
Pill
5
71
Progestin only
0.5
Combined
0.1
IUD
Progesterone T
2.0
1.5
81
Copper T380A
0.8
0.6
78
LNG 20
0.1
0.1
81
Depo-Provera®
0.3
0.3
70
Norplant® and Norplant-2®
0.05
0.05
88
Female Sterilization
0.5
0.5
100
Male Sterilization
0.15
0.10
100
Emergency Contraceptives Pills: Treatment initiated within 72 hours after unprotected intercourse reduces the risk of pregnancy by at least 75%è.
Lactational Amenorrhea Method: LAM is a highly effective, temporary method of contraception.Ă°
Source: Trussell J, The Essentials of Contraception. In Hatcher RA, Trussell J, Stewart F, Cates W, Stewart GK, Kowel D, Guest F, Contraceptive Technology: Seventeenth Revised Edition. New York NY: Irvington Publishers, 1998.
‡ Among couples attempting to avoid pregnancy, the percentage who continue to use a method for 1 year.
* Among typical couples who initiate use of a method (not necessarily for the first time), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason.
†Among couples who initiate use of a method (not necessarily for the first time) and who use it perfectly (both consistently and correctly), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason.
§ The percentages becoming pregnant in columns (2) and (3) are based on data from populations where contraception is not used and from women who cease using contraception in order to become pregnant. Among such populations, about 89% become pregnant within one year. This estimate was lowered slightly (to 85%) to represent the percent who would become pregnant within one year among women now relying on reversible methods of contraception if they abandoned contraception altogether.
¶ Foams, creams, gels, vaginal suppositories, and vaginal film.
#Ăž Cervical mucus (ovulation) method supplemented by calendar in the pre-ovulatory and basal body temperature in the post-ovulatory phases.
Ăź With spermicidal cream or jelly.
Ă Without spermicides.
è The treatment schedule is one dose within 72 hours after unprotected intercourse, and a second dose 12 hours after the first dose. The Food and Drug Administration has declared the following brands of combined oral contraceptives to be safe and effective for emergency contraception: Ovral® (1 dose is 2 white pills), Alesse® (1 dose is 5 pink pills), Nordette® or Levlen® (1 dose is 4 light-orange pills), Lo/Ovral® (1 dose is 4 white pills), Triphasil® or Tri-Levlen® (1 dose is 4 yellow pills).
Ă° However, to maintain effective protection against pregnancy, another method of contraception must be used as soon as menstruation resumes, the frequency or duration of breastfeeds is reduced, bottle feeds are introduced, or the baby reaches 6 months of age.
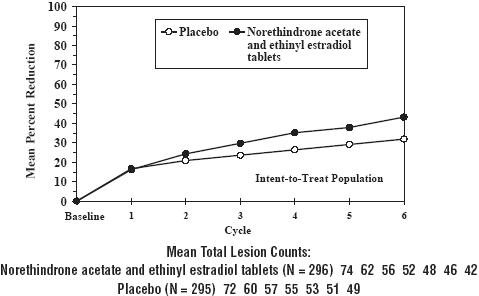
Norethindrone acetate and ethinyl estradiol tablets were evaluated for the treatment of acne vulgaris in two randomized, double-blind, placebo-controlled, multicenter, Phase 3, six (28-day) cycle studies. A total of 296 patients received norethindrone acetate and ethinyl estradiol tablets and 295 received placebo. Mean age at enrollment for both groups was 24 years. At six months each study demonstrated a statistically significant difference between norethindrone acetate and ethinyl estradiol tablets and placebo for mean change from baseline in lesion counts (see Table 3 and Figure 2). Each study also demonstrated overall treatment success in the investigator’s global evaluation. Patients with severe androgen excess were not studied.
Table 3. Acne Vulgaris Indication Pooled Data 376 to 403 and 376 to 404 Observed Means at Six Months and at Baseline* Intent To Treat Population
Norethindrone Acetate and Ethinyl
Estradiol Tablets
N = 296
Placebo N = 295
Difference in Counts Between Norethindrone
Acetate and Ethinyl
Estradiol Tablets and Placebo at Six Months (95% CI) â€
Number of Lesions
Counts
% reduction
Counts
% reduction
INFLAMMATORY LESIONS
Baseline Mean
29
29
Six Month Mean
14
52%
17
41%
3 (±2)
NON-INFLAMMATORY LESIONS
Baseline Mean
44
43
Six Month Mean
27
38%
32
25%
5 (±3.5)
TOTAL LESIONS
Baseline Mean
74
72
Six Month Mean
42
43%
49
32%
7 (±5)
*Numbers rounded to nearest integer
†Limits for 95% Confidence Interval; not adjusted for baseline differences
Norethindrone acetate and ethinyl estradiol tablets users who started with about 74 acne lesions had about 42 lesions after 6 months of treatment. Placebo users who started with about 72 acne lesions had about 49 lesions after the same duration of treatment.
Figure 2. Mean Percent Reduction in Total Lesion Counts From Baseline to Each 28-Day Cycle and Mean Total Lesion Counts at Each Cycle Following Administration of Norethindrone acetate and ethinyl estradiol tablets and Placebo (Statistically significant differences were not found in both studies individually until cycle 6)
Contraindications
Combined oral contraceptives should not be used in women who currently have the following:
- A high risk of arterial or venous thrombotic diseases. Examples include women who are known to:
- Smoke, if over age 35
- Have cerebrovascular disease
- Have coronary artery disease
- Have current or history of deep vein thrombosis or pulmonary embolism
- Have thrombogenic valvular or thrombogenic rhythm diseases of the heart
- Have inherited or acquired hypercoagulopathies
- Have uncontrolled hypertension or hypertension with vascular disease
- Have headaches with focal neurological symptoms, migraine headaches with aura, or over age 35 with any migraine headaches
- Have diabetes mellitus and are over age 35, diabetes mellitus with hypertension or with vascular disease or end-organ damage, or diabetes mellitus of > 20 years duration
- Current diagnosis of, or history of, breast cancer, which may be hormone-sensitive
- Undiagnosed abnormal genital bleeding
- Cholestatic jaundice of pregnancy or jaundice with prior pill use
- Hepatic adenomas or carcinomas
- Known or suspected pregnancy
- Are receiving Hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to the potential for ALT elevations (see WARNINGS , RISK OF LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENT ).
Warnings
The use of combined oral contraceptives is associated with increased risks of several serious conditions including myocardial infarction, thromboembolism, stroke, hepatic neoplasia, and gallbladder disease, although the risk of serious morbidity or mortality is very small in healthy women without underlying risk factors. The risk of morbidity and mortality increases significantly in the presence of other underlying risk factors such as hypertension, hyperlipidemias, obesity, and diabetes.
Practitioners prescribing combined oral contraceptives should be familiar with the following information relating to these risks.
The information contained in this package insert is principally based on studies carried out in patients who used combined oral contraceptives with higher formulations of estrogens and progestogens than those in common use today. The effect of long-term use of the combined oral contraceptives with lower formulations of both estrogens and progestogens remains to be determined.
Throughout this labeling, epidemiological studies reported are of two types: retrospective or case control studies and prospective or cohort studies. Case control studies provide a measure of the relative risk of a disease, namely, a ratio of the incidence of a disease among combined oral contraceptive users to that among nonusers. The relative risk does not provide information on the actual clinical occurrence of a disease. Cohort studies provide a measure of attributable risk, which is the difference in the incidence of disease between combined oral contraceptive users and nonusers. The attributable risk does provide information about the actual occurrence of a disease in the population (adapted from References 8 and 9 with the author’s permission). For further information, the reader is referred to a text on epidemiological methods.
1. Thromboembolic Disorders and Other Vascular Problems
An increased risk of myocardial infarction has been attributed to combined oral contraceptive use. This risk is primarily in smokers or women with other underlying risk factors for coronary artery disease such as hypertension, hypercholesterolemia, morbid obesity, and diabetes. The relative risk of heart attack for current combined oral contraceptive users has been estimated to be two to six. The risk is very low under the age of 30.
Smoking in combination with combined oral contraceptive use has been shown to contribute substantially to the incidence of myocardial infarctions in women in their mid-thirties or older with smoking accounting for the majority of excess cases. Mortality rates associated with circulatory disease have been shown to increase substantially in smokers over the age of 35 and non-smokers over the age of 40 (Figure 3) among women who use combined oral contraceptives.
Figure 3. Circulatory Disease Mortality Rates per 100,000 Woman Years by Age, Smoking Status and Combined Oral Contraceptive Use
Combined oral contraceptives may compound the effects of well-known risk factors, such as hypertension, diabetes, hyperlipidemias, age and obesity. In particular, some progestogens are known to decrease HDL cholesterol and cause glucose intolerance, while estrogens may create a state of hyperinsulinism. Combined oral contraceptives have been shown to increase blood pressure among users (see Section 10 in WARNINGS ). Similar effects on risk factors have been associated with an increased risk of heart disease. Combined oral contraceptives must be used with caution in women with cardiovascular disease risk factors.
An increased risk of thromboembolic and thrombotic disease associated with the use of combined oral contraceptives is well established. Case control studies have found the relative risk of users compared to nonusers to be 3 for the first episode of superficial venous thrombosis, 4 to 11 for deep vein thrombosis or pulmonary embolism, and 1.5 to 6 for women with predisposing conditions for venous thromboembolic disease. Cohort studies have shown the relative risk to be somewhat lower, about 3 for new cases and about 4.5 for new cases requiring hospitalization. The risk of thromboembolic disease due to combined oral contraceptives is not related to length of use and disappears after combined oral contraceptive pill use is stopped.
A two- to four-fold increase in relative risk of postoperative thromboembolic complications has been reported with the use of combined oral contraceptives. The relative risk of venous thrombosis in women who have predisposing conditions is twice that of women without such medical conditions. If feasible, combined oral contraceptives should be discontinued at least 4 weeks prior to and for 2 weeks after elective surgery of a type associated with an increase in risk of thromboembolism and during and following prolonged immobilization. Since the immediate postpartum period is also associated with an increased risk of thromboembolism, combined oral contraceptives should be started no earlier than 4 to 6 weeks after delivery in women who elect not to breastfeed.
Combined oral contraceptives have been shown to increase both the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes), although, in general, the risk is greatest among older (>35 years), hypertensive women who also smoke. Hypertension was found to be a risk factor for both users and nonusers, for both types of strokes, while smoking interacted to increase the risk for hemorrhagic strokes.
In a large study, the relative risk of thrombotic strokes has been shown to range from 3 for normotensive users to 14 for users with severe hypertension. The relative risk of hemorrhagic stroke is reported to be 1.2 for non-smokers who used combined oral contraceptives, 2.6 for smokers who did not use combined oral contraceptives, 7.6 for smokers who used oral contraceptives, 1.8 for normotensive users, and 25.7 for users with severe hypertension. The attributable risk is also greater in older women.
A positive association has been observed between the amount of estrogen and progestogen in combined oral contraceptives and the risk of vascular disease. A decline in serum high-density lipoproteins (HDL) has been reported with many progestational agents. A decline in serum high-density lipoproteins has been associated with an increased incidence of ischemic heart disease. Because estrogens increase HDL cholesterol, the net effect of a combined oral contraceptive depends on a balance achieved between doses of estrogen and progestin and the nature of the progestin used in the contraceptives. The amount and activity of both hormones should be considered in the choice of a combined oral contraceptive.
Minimizing exposure to estrogen and progestogen is in keeping with good principles of therapeutics. For any particular combined oral contraceptive, the dosage regimen prescribed should be one which contains the least amount of estrogen and progestogen that is compatible with the needs of the individual patient. New acceptors of combined oral contraceptive agents should be started on preparations containing the lowest dose of estrogen which produces satisfactory results for the patient.
There are two studies which have shown persistence of risk of vascular disease for ever-users of combined oral contraceptives. In a study in the United States, the risk of developing myocardial infarction after discontinuing combined oral contraceptives persists for at least 9 years for women 40 to 49 years who had used combined oral contraceptives for 5 or more years, but this increased risk was not demonstrated in other age groups. In another study in Great Britain, the risk of developing cerebrovascular disease persisted for at least 6 years after discontinuation of combined oral contraceptives, although excess risk was very small. However, both studies were performed with combined oral contraceptive formulations containing 50 mcg or higher of estrogens.
2. Estimates of Mortality from Combined OralContraceptive Use
One study gathered data from a variety of sources which have estimated the mortality rate associated with different methods of contraception at different ages (Table 4). These estimates include the combined risk of death associated with contraceptive methods plus the risk attributable to pregnancy in the event of method failure. Each method of contraception has its specific benefits and risks. The study concluded that with the exception of combined oral contraceptive users 35 and older who smoke and 40 and older who do not smoke, mortality associated with all methods of birth control is low and below that associated with childbirth. The observation of a possible increase in risk of mortality with age for combined oral contraceptive users is based on data gathered in the 1970’s but not reported until 1983. However, current clinical practice involves the use of lower estrogen dose formulations combined with careful restriction of combined oral contraceptive use to women who do not have the various risk factors uled in this labeling.
Because of these changes in practice and, also, because of some limited new data which suggest that the risk of cardiovascular disease with the use of combined oral contraceptives may now be less than previously observed (Porter JB, Hunter J, Jick H, et al. Oral contraceptives and nonfatal vascular disease. Obstet Gynecol 1985;66:1 to 4; and Porter JB, Hershel J, Walker AM. Mortality among oral contraceptive users. Obstet Gynecol 1987;70:29 to 32), the Fertility and Maternal Health Drugs Advisory Committee was asked to review the topic in 1989. The Committee concluded that although cardiovascular disease risks may be increased with combined oral contraceptive use after age 40 in healthy nonsmoking women (even with the newer low-dose formulations), there are greater potential health risks associated with pregnancy in older women and with the alternative surgical and medical procedures which may be necessary if such women do not have access to effective and acceptable means of contraception.
Therefore, the Committee recommended that the benefits of combined oral contraceptive use by healthy non-smoking women over 40 may outweigh the possible risks. Of course, older women, as all women who take combined oral contraceptives, should take the lowest possible dose formulation that is effective.
Table 4. Annual Number of Birth-Related or Method-Related Deaths Associated with Control of Fertility Per 100,000 Nonsterile Women by Fertility Control Method According to Age
Method of control and outcome
15 to 19
20 to 24
25 to 29
30 to 34
35 to 39
40 to 44
No fertility control methods*
7.0
7.4
9.1
14.8
25.7
28.2
Oral contraceptives non-smoker**
0.3
0.5
0.9
1.9
13.8
31.6
Oral contraceptives smoker**
2.2
3.4
6.6
13.5
51.1
117.2
IUD**
0.8
0.8
1.0
1.0
1.4
1.4
Condom*
1.1
1.6
0.7
0.2
0.3
0.4
Diaphragm/spermicide*
1.9
1.2
1.2
1.3
2.2
2.8
Periodic abstinence*
2.5
1.6
1.6
1.7
2.9
3.6
*Deaths are birth-related.
**Deaths are method-related.
Adapted from H.W. Ory
3.Malignant Neoplasms
Breast Cancer Tri-Legest® Fe is contraindicated in females who currently have or have had breast cancer because breast cancer may be hormonally sensitive (see CONTRAINDICATIONS ).Â
Epidemiology studies have not found a consistent association between use of combined oral contraceptives (COCs) and breast cancer risk. Studies do not show an association between ever (current or past) use of COCs and risk of breast cancer. However, some studies report a small increase in the risk of breast cancer among current or recent users (<6 months since last use) and current users with longer duration of COC use (see ADVERSE REACTIONS ).
Cervical Cancer Some studies suggest that combined oral contraceptive use has been associated with an increase in the risk of cervical intraepithelial neoplasia in some populations of women. However, there continues to be controversy about the extent to which such findings may be due to differences in sexual behavior and other factors.
4. Hepatic Neoplasia
Benign hepatic adenomas are associated with combined oral contraceptive use, although the incidence of benign tumors is rare in the United States. Indirect calculations have estimated the attributable risk to be in the range of 3.3 cases/100,000 for users, a risk that increases after 4 or more years of use. Rupture of rare, benign, hepatic adenomas may cause death through intra-abdominal hemorrhage.
Studies from Britain have shown an increased risk of developing hepatocellular carcinoma in long-term (>8 years) combined oral contraceptive users. However, these cancers are extremely rare in the U.S., and the attributable risk (the excess incidence) of liver cancers in combined oral contraceptive users approaches less than one per million users.
5. Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Treatment
During clinical trials with the Hepatitis C combination drug regimen that contains ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN), including some cases greater than 20 times the ULN, were significantly more frequent in women using ethinyl estradiol-containing medications such as COCs. Discontinue Tri-Legest® Fe prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir (see CONTRAINDICATIONS ).
Tri-Legest® Fe can be restarted approximately 2 weeks following completion of treatment with the combination drug regimen.
6. Ocular Lesions
There have been clinical case reports of retinal thrombosis associated with the use of combined oral contraceptives. Combined oral contraceptives should be discontinued if there is unexplained partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or retinal vascular lesions. Appropriate diagnostic and therapeutic measures should be undertaken immediately.
7. Oral Contraceptive Use Before and During Early Pregnancy
Extensive epidemiological studies have revealed no increased risk of birth defects in women who have used combined oral contraceptives prior to pregnancy. Studies also do not suggest a teratogenic effect, particularly insofar as cardiac anomalies and limb reduction defects are concerned, when taken inadvertently during early pregnancy.
The administration of combined oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Combined oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion.
It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out before continuing oral contraceptive use. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period. Combined oral contraceptive use should be discontinued if pregnancy is confirmed.
8. Gallbladder Disease
Earlier studies have reported an increased lifetime relative risk of gallbladder surgery in users of combined oral contraceptives and estrogens. More recent studies, however, have shown that the relative risk of developing gallbladder disease among oral contraceptive users may be minimal. The recent findings of minimal risk may be related to the use of combined oral contraceptive formulations containing lower hormonal doses of estrogens and progestogens.
9. Carbohydrate and Lipid Metabolic Effects
Combined oral contraceptives have been shown to cause glucose intolerance in a significant percentage of users. Combined oral contraceptives containing greater than 75 mcg of estrogens cause hyperinsulinism, while lower doses of estrogen cause less glucose intolerance. Progestogens increase insulin secretion and create insulin resistance, this effect varying with different progestational agents. However, in the non-diabetic woman, combined oral contraceptives appear to have no effect on fasting blood glucose. Because of these demonstrated effects, prediabetic and diabetic women should be carefully observed while taking combined oral contraceptives.
A small proportion of women will have persistent hypertriglyceridemia while on the pill. As discussed earlier (see WARNINGS Â 1a. and 1d.), changes in serum triglycerides and lipoprotein levels have been reported in combined oral contraceptive users.
10. Elevated Blood Pressure
An increase in blood pressure has been reported in women taking combined oral contraceptives and this increase is more likely in older combined oral contraceptive users and with continued use. Data from the Royal College of General Practitioners and subsequent randomized trials have shown that the incidence of hypertension increases with increasing concentrations of progestogens.
Women with a history of hypertension or hypertension-related diseases or renal disease should be encouraged to use another method of contraception. If women elect to use combined oral contraceptives, they should be monitored closely, and if significant elevation of blood pressure occurs, combined oral contraceptives should be discontinued. For most women, elevated blood pressure will return to normal after stopping combined oral contraceptives, and there is no difference in the occurrence of hypertension among ever and never users.
11. Headache
The onset or exacerbation of migraine or development of headache with a new pattern which is recurrent, persistent, or severe requires discontinuation of combined oral contraceptives and evaluation of the cause.
12. Bleeding Irregularities
Breakthrough bleeding and spotting are sometimes encountered in patients on combined oral contraceptives, especially during the first three months of use. Non-hormonal causes should be considered, and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of prolonged breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If pathology has been excluded, time or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out.
Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was preexistent.
13. Hereditary Angioedema
In women with hereditary angioedema, exogenous estrogens may induce or exacerbate symptoms of angioedema.
14. Chloasma
Chloasma may occur with norethindrone acetate and ethinyl estradiol tablets, especially in women with a history of chloasma gravidarum. Advise women with a history of chloasma to avoid exposure to the sun or ultraviolet radiation while taking norethindrone acetate and ethinyl estradiol tablets.
Precautions
1. Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
2. Physical Examination and Follow-Up
It is good medical practice for all women to have annual history and physical examinations, including women using combined oral contraceptives. The physical examination, however, may be deferred until after initiation of combined oral contraceptives if requested by the woman and judged appropriate by the clinician. The physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology, and relevant laboratory tests. In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate measures should be conducted to rule out malignancy. Women with a strong family history of breast cancer or who have breast nodules should be monitored with particular care.
3. Lipid Disorders
Women who are being treated for hyperlipidemia should be followed closely if they elect to use combined oral contraceptives. Some progestogens may elevate LDL levels and may render the control of hyperlipidemias more difficult.
4. Liver Function
If jaundice develops in any woman receiving such drugs, the medication should be discontinued. Steroid hormones may be poorly metabolized in patients with impaired liver function.
5. Fluid Retention
Combined oral contraceptives may cause some degree of fluid retention. They should be prescribed with caution, and only with careful monitoring, in patients with conditions which might be aggravated by fluid retention.
6. Emotional Disorders
Women with a history of depression should be carefully observed and the drug discontinued if depression recurs to a serious degree.
7. Contact Lenses
Contact lens wearers who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.
8. Drug Interactions
Rifampin: Metabolism of both norethindrone and ethinyl estradiol is increased by rifampin. A reduction in contraceptive effectiveness and increased incidence of breakthrough bleeding and menstrual irregularities have been associated with concomitant use of rifampin.
Anticonvulsants: Anticonvulsants such as phenobarbital, phenytoin, and carbamazepine, have been shown to increase the metabolism of ethinyl estradiol and/or norethindrone, which could result in a reduction in contraceptive effectiveness.
Antibiotics: Pregnancy while taking combined oral contraceptives has been reported when the combined oral contraceptives were administered with antimicrobials such as ampicillin, tetracycline, and griseofulvin. However, clinical pharmacokinetic studies have not demonstrated any consistent effect of antibiotics (other than rifampin) on plasma concentrations of synthetic steroids.
Atorvastatin: Coadministration of atorvastatin and an combined oral contraceptive increased AUC values for norethindrone and ethinyl estradiol by approximately 30% and 20%, respectively.
St. John’s Wort: Herbal products containing St. John’s Wort (hypericum perforatum) may induce hepatic enzymes (cytochrome P450) and p-glycoprotein transporter and may reduce the effectiveness of combined oral contraceptives. This may also result in breakthrough bleeding.
Human immunodeficiency virus (HIV)/Hepatitis C virus (HCV) protease inhibitors and non-nucleoside reverse transcriptase inhibitors
Significant changes (increase or decrease) in the plasma concentrations of estrogen and progestin have been noted in some cases of co-administration with HIV/HCV protease inhibitors (decrease [e.g., nelfinavir, ritonavir, darunavir/ritonavir, (fos)amprenavir/ritonavir, lopinavir/ritonavir, and tipranavir/ritonavir] or increase [e.g., indinavir and atazanavir/ritonavir])/HCV protease inhibitors (decrease [e.g., boceprevir and telaprevir]) or with non-nucleoside reverse transcriptase inhibitors (decrease [e.g., nevirapine] or increase [e.g., etravirine]).
Concomitant Use with HCV Combination Therapy – Liver Enzyme Elevation: Do not co-administer Tri-Legest® Fe with HCV drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to potential for ALT elevations (see WARNINGS , RISK OF LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENT ).
Other: Ascorbic acid and acetaminophen may increase plasma ethinyl estradiol concentrations, possibly by inhibition of conjugation. A reduction in contraceptive effectiveness and increased incidence of breakthrough bleeding has been suggested with phenylbutazone.
COCs containing ethinyl estradiol may inhibit the metabolism of other compounds (e.g., cyclosporine, prednisolone, theophylline, tizanidine, and voriconazole) and increase their plasma concentrations. COCs have been shown to decrease plasma concentrations of acetaminophen, clofibric acid, morphine, salicylic acid, temazepam and lamotrigine. Significant decrease in plasma concentration of lamotrigine has been shown, likely due to induction of lamotrigine glucuronidation. This may reduce seizure control; therefore, dosage adjustments of lamotrigine may be necessary.
Women on thyroid hormone replacement therapy may need increased doses of thyroid hormone because the serum concentration of thyroid-binding globulin increase with use of COCs.
9. Interactions with Laboratory Tests
Certain endocrine and liver function tests and blood components may be affected by combined oral contraceptives:
a. Increased prothrombin and factors VII, VIII, IX, and X; decreased antithrombin 3; increased norepinephrine-induced platelet aggregability.
b. Increased thyroid binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 by column or by radioimmunoassay. Free T3 resin uptake is decreased, reflecting the elevated TBG; free T4 concentration is unaltered.
c. Other binding proteins may be elevated in serum.
d. Sex-binding globulins are increased and result in elevated levels of total circulating sex steroids and corticoids; however, free or biologically active levels remain unchanged.
e. Triglycerides may be increased.
f. Glucose tolerance may be decreased.
g. Serum folate levels may be depressed by combined oral contraceptive therapy. This may be of clinical significance if a woman becomes pregnant shortly after discontinuing combined oral contraceptives.
10. Carcinogenesis
See WARNINGS section.
11. Pregnancy
See CONTRAINDICATIONSÂ and WARNINGS Â sections.
12. Nursing Mothers
Small amounts of oral contraceptive steroids have been identified in the milk of nursing mothers, and a few adverse effects on the child have been reported, including jaundice and breast enlargement. In addition, combined oral contraceptives given in the postpartum period may interfere with lactation by decreasing the quantity and quality of breast milk. If possible, the nursing mother should be advised not to use combined oral contraceptives but to use other forms of contraception until she has completely weaned her child.
13. Pediatric Use
Safety and efficacy of norethindrone acetate and ethinyl estradiol tablets have been established in women of reproductive age. Safety and efficacy are expected to be the same for postpubertal adolescents under the age of 16 and for users 16 years and older. Use of this product before menarche is not indicated.
14. Geriatric Use
This product has not been studied in women over 65 years of age and is not indicated in this population.
Information For The Patient
See patient labeling printed below.
Adverse Reactions
Post Marketing Experience
Five studies that compared breast cancer risk between ever-users (current or past use) of COCs and never-users of COCs reported no association between ever use of COCs and breast cancer risk, with effect estimates ranging from 0.90 to 1.12 (Figure 4).
Three studies compared breast cancer risk between current or recent COC users (<6 months since last use) and never users of COCs (Figure 4). One of these studies reported no association between breast cancer risk and COC use. The other two studies found an increased relative risk of 1.19 to 1.33 with current or recent use. Both of these studies found an increased risk of breast cancer with current use of longer duration, with relative risks ranging from 1.03 with less than one year of COC use to approximately 1.4 with more than 8 to 10 years of COC use.
Figure 4: Relevant Studies of Risk of Breast Cancer with Combined Oral Contraceptives
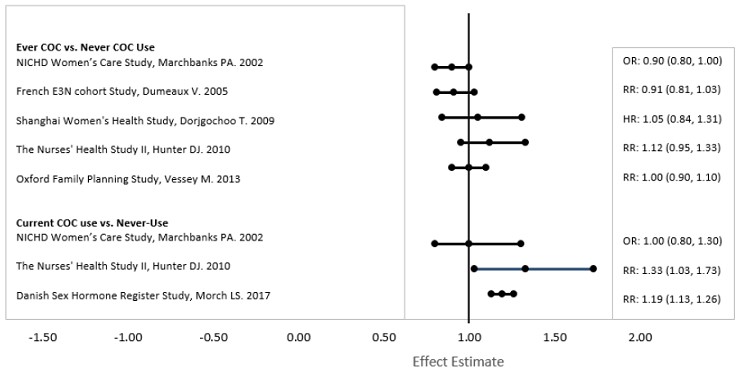
RR = relative risk; OR = odds ratio; HR = hazard ratio. “ever COC” are females with current or past COC use; “never COC use” are females that never used COCs.
An increased risk of the following serious adverse reactions has been associated with the use of combined oral contraceptives (see WARNINGS section):
- Thrombophlebitis
- Arterial thromboembolism
- Pulmonary embolism
- Myocardial infarction
- Cerebral hemorrhage
- Cerebral thrombosis
- Hypertension
- Gallbladder disease
- Hepatic adenomas or benign liver tumors
There is evidence of an association between the following conditions and the use of combined oral contraceptives, although additional confirmatory studies are needed:
- Mesenteric thrombosis
- Retinal thrombosis
The following adverse reactions have been reported in patients receiving combined oral contraceptives and are believed to be drug-related:
- Nausea
- Vomiting
- Gastrointestinal symptoms (such as abdominal cramps and bloating)
- Breakthrough bleeding
- Spotting
- Change in menstrual flow
- Amenorrhea
- Temporary infertility after discontinuation of treatment
- Edema
- Melasma which may persist
- Breast changes: tenderness, enlargement, secretion
- Change in weight (increase or decrease)
- Change in cervical erosion and secretion
- Diminution in lactation when given immediately postpartum
- Cholestatic jaundice
- Migraine
- Rash (allergic)
- Mental depression
- Mood swings
- Reduced tolerance to carbohydrates
- Vaginal candidiasis
- Change in corneal curvature (steepening)
- Intolerance to contact lenses
The following adverse reactions have been reported in users of combined oral contraceptives and the association has been neither confirmed nor refuted:
- Pre-menstrual syndrome
- Cataracts
- Changes in appetite
- Cystitis-like syndrome
- Headache
- Nervousness
- Dizziness
- Hirsutism
- Loss of scalp hair
- Erythema multiforme
- Erythema nodosum
- Hemorrhagic eruption
- Vaginitis
- Porphyria
- Impaired renal function
- Hemolytic uremic syndrome
- Budd-Chiari syndrome
- Acne
- Changes in libido
- Colitis
To report SUSPECTED ADVERSE EVENTS, contact Teva at 1-888-838-2872 or FDA at 1-800-FDA-1088 or http://www.fda.gov/medwatch for voluntary reporting of adverse reactions.
Overdosage
Serious ill effects have not been reported following acute ingestion of large doses of combined oral contraceptives by young children. Overdosage may cause nausea, and withdrawal bleeding may occur in females.
Non-contraceptive Health Benefits
The following non-contraceptive health benefits related to the use of combined oral contraceptives are supported by epidemiological studies which largely utilized combined oral contraceptive formulations containing estrogen doses exceeding 0.035 mg of ethinyl estradiol or 0.05 mg of mestranol.
Effects on menses:
- Increased menstrual cycle regularity
- Decreased blood loss and decreased incidence of iron deficiency anemia
- Decreased incidence of dysmenorrhea
Effects related to inhibition of ovulation:
- Decreased incidence of functional ovarian cysts
- Decreased incidence of ectopic pregnancies
Effects from long-term use:
- Decreased incidence of fibroadenomas and fibrocystic disease of the breast
- Decreased incidence of acute pelvic inflammatory disease
- Decreased incidence of endometrial cancer
- Decreased incidence of ovarian cancer
Dosage And Administration
The tablet dispenser has been designed to make Tri-Legest® Fe (norethindrone acetate and ethinyl estradiol tablets, USP and ferrous fumarate tablets [not USP]) dosing as easy and as convenient as possible. The tablets are arranged in four rows of seven tablets each, with the days of the week appearing on the tablet dispenser above the first row of tablets.
Note: Each tablet dispenser has been preprinted with the days of the week, starting with Sunday, to facilitate a Sunday-Start regimen. Six different days of the week stickers have been provided with the Detailed Patient & Brief Summary Patient Package Insert in order to accommodate a Day-1 Start regimen. If the patient is using the Day-1 Start regimen, she should place the self-adhesive days of the week sticker that corresponds to her starting day over the preprinted days.
Important: The patient should be instructed to use an additional method of protection until after the first week of administration in the initial cycle when utilizing the Sunday-Start regimen.
The possibility of ovulation and conception prior to initiation of use should be considered.
Dosage and Administration for 28-Day Dosage Regimen
To achieve maximum contraceptive effectiveness, Tri-Legest® Fe (norethindrone acetate and ethinyl estradiol tablets, USP and ferrous fumarate tablets [not USP]) should be taken exactly as directed and at intervals not exceeding 24 hours.
Tri-Legest® Fe (norethindrone acetate and ethinyl estradiol tablets, USP and ferrous fumarate tablets [not USP]) provides a continuous administration regimen consisting of 21 light pink, light yellow, and light blue tablets of norethindrone acetate and ethinyl estradiol and seven brown non-hormone containing tablets of ferrous fumarate. The ferrous fumarate tablets are present to facilitate ease of drug administration via a 28-day regimen and do not serve any therapeutic purpose. There is no need for the patient to count days between cycles because there are no “off-tablet days”.
A. Sunday-Start Regimen: The patient begins taking the first light pink tablet from the top row of the tablet dispenser (labeled Sunday) on the first Sunday after menstrual flow begins. When menstrual flow begins on Sunday, the first light pink tablet is taken on the same day. The patient takes one tablet daily for 21 days. The last light blue tablet in the dispenser will be taken on a Saturday. Upon completion of all 21 tablets, and without interruption, the patient takes one brown tablet daily for 7 days. Upon completion of this first course of tablets, the patient begins a second course of 28-day tablets, without interruption, the next day (Sunday), starting with the Sunday light pink tablet in the top row. Adhering to this regimen of one tablet daily for 21 days, followed without interruption by one brown tablet daily for 7 days, the patient will start all subsequent cycles on a Sunday.
B. Day-1 Start Regimen: The first day of menstrual flow is Day 1. The patient places the self-adhesive days of the week sticker that corresponds to her starting day over the preprinted days on the tablet dispenser. She starts taking one light pink tablet daily, beginning with the first light pink tablet in the top row. After the last light blue tablet (at the end of the third row) has been taken, the patient will then take the brown tablets for a week (7 days). For all subsequent cycles, the patient begins a new 28 tablet regimen on the eighth day after taking her last light blue tablet, again starting with the first tablet in the top row after placing the appropriate days of the week sticker over the preprinted days on the tablet dispenser. Following this regimen of 21 light pink, light yellow, and light blue tablets and 7 brown tablets, the patient will start all subsequent cycles on the same day of the week as the first course.
Tablets should be taken regularly at the same time each day and can be taken without regard to meals. It should be stressed that efficacy of medication depends on strict adherence to the dosage schedule.
Special Notes on Administration
Menstruation usually begins two or three days, but may begin as late as the fourth or fifth day, after the brown tablets have been started. In any event, the next course of tablets should be started without interruption. If spotting occurs while the patient is taking light pink, light yellow, or light blue tablets, continue medication without interruption.
If the patient forgets to take one or more light pink, light yellow or light blue tablets, the following is suggested:
One tablet is missed
- take tablet as soon as remembered
- take next tablet at the regular time
Two consecutive tablets are missed (Week 1 or Week 2)
- take two tablets as soon as remembered
- take two tablets the next day
- use another birth control method for seven days following the missed tablets
Two consecutive tablets are missed (Week 3)
Sunday-Start Regimen:
- take one tablet daily until Sunday
- discard remaining tablets
- start new pack of tablets immediately (Sunday)
- use another birth control method for seven days following the missed tablets
Day-1 Start Regimen:
- discard remaining tablets
- start new pack of tablets that same day
- use another birth control method for seven days following the missed tablets
Three (or more) consecutive tablets are missed
Sunday-Start Regimen:
- take one tablet daily until Sunday
- discard remaining tablets
- start new pack of tablets immediately (Sunday)
- use another birth control method for seven days following the missed tablets
Day-1 Start Regimen:
- discard remaining tablets
- start new pack of tablets that same day
- use another birth control method for seven days following the missed tablets
The possibility of ovulation occurring increases with each successive day that scheduled light pink, light yellow and light blue tablets are missed. While there is little likelihood of ovulation occurring if only one tablet is missed, the possibility of spotting or bleeding is increased. This is particularly likely to occur if two or more consecutive light pink, light yellow, and light blue tablets are missed.
If the patient forgets to take any of the seven brown tablets in week four, those brown tablets that were missed are discarded and one brown tablet is taken each day until the pack is empty. A back-up birth control method is not required during this time. A new pack of tablets should be started no later than the eighth day after the last light blue tablet was taken.
In the rare case of bleeding which resembles menstruation, the patient should be advised to discontinue medication and then begin taking tablets from a new tablet dispenser on the next Sunday or the first day (Day 1) depending on her regimen. Persistent bleeding which is not controlled by this method indicates the need for reexamination of the patient, at which time nonfunctional causes should be considered.
Use of Combined Oral Contraceptives in the Event of a Missed Menstrual Period
1. If the patient has not adhered to the prescribed dosage regimen, the possibility of pregnancy should be considered after the first missed period and combined oral contraceptives should be withheld until pregnancy has been ruled out.
2. If the patient has adhered to the prescribed regimen and misses two consecutive periods, pregnancy should be ruled out before continuing the contraceptive regimen.
After several months on treatment, bleeding may be reduced to a point of virtual absence. This reduced flow may occur as a result of medication, in which event it is not indicative of pregnancy.
Acne
The timing of initiation of dosing with Tri-Legest® Fe for acne should follow the guidelines for use of Tri-Legest® Fe as a combined oral contraceptive. Consult the DOSAGE AND ADMINISTRATION section for Tri-Legest® Fe oral contraceptives.
How Supplied
Tri-Legest® Fe (norethindrone acetate and ethinyl estradiol tablets, USP and ferrous fumarate tablets [not USP]) is packaged in cartons of five tablet dispensers of 28 tablets each. Each tablet dispenser contains five light pink, round, flat-faced, beveled-edge, unscored tablets debossed with stylized b on one side and 711 on the other side each containing 1 mg of norethindrone acetate and 20 mcg of ethinyl estradiol; seven light yellow, round, flat-faced, beveled-edge, unscored tablets debossed with stylized b on one side and 712 on the other side each containing 1 mg of norethindrone acetate and 30 mcg of ethinyl estradiol; nine light blue, round, flat-faced, beveled-edge, unscored tablets debossed with stylized b on one side and 713 on the other side each containing 1 mg of norethindrone acetate and 35 mcg of ethinyl estradiol; and seven brown, round, flat-faced, beveled-edge, unscored tablets debossed with stylized b on one side and 247 on the other side each containing 75 mg ferrous fumarate. The ferrous fumarate tablets are present to facilitate ease of drug administration via a 28-day regimen, are non-hormonal, and do not serve any therapeutic purpose.
NDC 0555-9032-70 Carton of 5 Tablet Dispensers
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Protect from light.
Store tablets inside pouch when not in use.
REFERENCES AVAILABLE UPON REQUEST.
Teva Pharmaceuticals USA, Inc. North Wales, PA 19454
Rev. G 3/2023
Brief Summary Patient Package Insert
Do not use Tri-Legest® Fe if you smoke cigarettes and are over 35 years old. Smoking increases your risk of serious cardiovascular side effects (heart and blood vessel problems) from birth control pills, including death from heart attack, blood clots or stroke. This risk increases with age and the number of cigarettes you smoke
Tri-Legest® Fe (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted diseases.
Combined oral contraceptives, also known as “birth control pills” or “the pill”, are taken to prevent pregnancy and, when taken correctly, have a failure rate of about 1% per year when used without missing any pills. The typical failure rate of large numbers of pill users is less than 3% per year when women who miss pills are included. For most women combined oral contraceptives are also free of serious or unpleasant side effects. However, forgetting to take pills considerably increases the chances of pregnancy.
Tri-Legest® Fe may also be taken to treat moderate acne in females who are at least 15 years of age, have started having menstrual periods, are able to use the pill and want the pill for birth control, plan to stay on the pill for at least 6 months, and have not improved with acne medicines that are put on the skin.
For the majority of women, combined oral contraceptives can be taken safely. But there are some women who are at high risk of developing certain serious diseases that can be life-threatening or may cause temporary or permanent disability. The risks associated with taking oral contraceptives increase significantly if you:
Smoke
- Have high blood pressure, diabetes, high cholesterol, migraine headaches
- Have or have had blood clots in your arms, legs, lungs, or eyes, clotting disorders, heart attack, heart problems, stroke, angina pectoris, cancer of the breast, jaundice, or malignant or benign liver tumors.
- Are receiving Hepatitis C medication
You should not take the pill if you suspect you are pregnant or have unexplained vaginal bleeding.
Most side effects of the pill are not serious. The most common side effects are nausea, vomiting, bleeding between menstrual periods, weight gain, breast tenderness, and difficulty wearing contact lenses. These side effects, especially nausea, vomiting, and breakthrough bleeding, may subside within the first three months of use.
The serious side effects of the pill occur very infrequently, especially if you are in good health and are young. However, you should know that the following medical conditions have been associated with or made worse by the pill:
- Blood clots in the legs (thrombophlebitis), lungs (pulmonary embolism), stoppage or rupture of a blood vessel in the brain (stroke), blockage of blood vessels in the heart (heart attack or angina pectoris), or other organs of the body. As mentioned above, smoking increases the risk of heart attacks and strokes and subsequent serious medical consequences.
- Liver tumors, which may rupture and cause severe bleeding. A possible but not definite association has been found with the pill and liver cancer. However, liver cancers are extremely rare. The chance of developing liver cancer from using the pill is thus even rarer.
- High blood pressure, although blood pressure usually returns to normal when the pill is stopped.
The symptoms associated with these serious side effects are discussed in the detailed leaflet given to you with your supply of pills. Notify your doctor or healthcare provider if you notice any unusual physical disturbances while taking the pill. In addition, drugs such as rifampin, as well as some anticonvulsants and some antibiotics, may decrease combined oral contraceptive effectiveness.
Do not take the pill if you take any Hepatitis C drug combination containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir. This may increase levels of the liver enzyme “alanine aminotransferase” (ALT) in the blood.
Do birth control pills cause cancer?
There may be slight increases in the risk of breast cancer among current users of hormonal birth control pills with longer duration of use of 8 years or more. Some studies have found an increase in the incidence of precancerous lesions of the cervix in women who use combined oral contraceptives. However, this finding may be related to factors other than the use of combined oral contraceptives.
Taking the pill provides some important non-contraceptive benefits. These include less painful menstruation, less menstrual blood loss and anemia, fewer pelvic infections, and fewer cancers of the ovary and the lining of the uterus.
Be sure to discuss any medical condition you may have with your healthcare provider. Your healthcare provider will take a medical and family history and examine you before prescribing oral contraceptives. The physical examination may be delayed to another time if you request it and your healthcare provider believes that it is a good medical practice to postpone it. You should be reexamined at least once a year while taking oral contraceptives. The Detailed Patient Information leaflet gives you further information which you should read and discuss with your healthcare provider.
Instructions To Patient
TABLET DISPENSER
The Tri-Legest® Fe tablet dispenser has been designed to make combined oral contraceptive dosing as easy and as convenient as possible. The tablets are arranged in four rows of seven tablets each, with the days of the week appearing above the first row of tablets.
Each light pink tablet contains 1 mg norethindrone acetate and 20 mcg ethinyl estradiol.
Each light yellow tablet contains 1 mg norethindrone acetate and 30 mcg ethinyl estradiol.
Each light blue tablet contains 1 mg norethindrone acetate and 35 mcg ethinyl estradiol.
Each brown tablet contains 75 mg ferrous fumarate and is intended to help you remember to take the tablets correctly. These brown tablets are not intended to have any health benefit.
DIRECTIONS
To remove a tablet, press down on it with your thumb or finger. The tablet will drop through the back of the tablet dispenser. Do not press with your thumbnail, fingernail, or any other sharp object.Â
HOW TO TAKE THE PILL
IMPORTANT POINTS TO REMEMBER
BEFORE YOU START TAKING YOUR PILLS:
1. BE SURE TO READ THESE DIRECTIONS:
Before you start taking your pills.
Anytime you are not sure what to do.
2. THE RIGHT WAY TO TAKE THE PILL IS TO TAKE ONE PILL EVERY DAY AT THE SAME TIME. If you miss pills you could get pregnant. This includes starting the pack late. The more pills you miss, the more likely you are to get pregnant.
3. MANY WOMEN HAVE SPOTTING OR LIGHT BLEEDING, OR MAY FEEL SICK TO THEIR STOMACH, DURING THE FIRST 1 to 3 PACKS OF PILLS. If you do have spotting or light bleeding or feel sick to your stomach, do not stop taking the pill. The problem will usually go away. If it doesn’t go away, check with your doctor or clinic.
4. MISSING PILLS CAN ALSO CAUSE SPOTTING OR LIGHT BLEEDING, even when you make up these missed pills. On the days you take 2 pills to make up for missed pills, you could also feel a little sick to your stomach.
5. IF YOU HAVE VOMITING OR DIARRHEA, for any reason, or IF YOU TAKE SOME MEDICINES, including some antibiotics, your birth control pills may not work as well. Use a back-up birth control method (such as condoms or spermicide) until you check with your doctor or clinic.
6. IF YOU HAVE TROUBLE REMEMBERING TO TAKE THE PILL, talk to your doctor or clinic about how to make pill-taking easier or about using another method of birth control.
7. IF YOU HAVE ANY QUESTIONS OR ARE UNSURE ABOUT THE INFORMATION IN THIS LEAFLET, call your doctor or clinic.
BEFORE YOU START TAKING YOUR PILLS
1. DECIDE WHAT TIME OF DAY YOU WANT TO TAKE YOUR PILL. It is important to take it at about the same time every day.
2. LOOK AT YOUR PILL PACK. The pill pack has 21 “active” pills (5 light pink, 7 light yellow, and 9 light blue tablets - with hormones) to take for 3 weeks, followed by 1 week of reminder brown pills (without hormones).
3. ALSO FIND:     1) where on the pack to start taking pills,     2) in what order to take the pills (follow the arrows), and     3) the week numbers are shown in the following pictures:
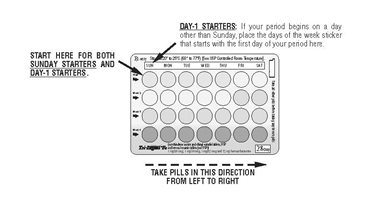
Each Tri-Legest® Fe tablet dispenser contains 5 light pink, 7 light yellow, and 9 light blue pills for Weeks 1, 2, and 3. Week 4 will contain BROWN PILLS ONLY. These tablets are to be taken in the following order: one light pink tablet each day for five days, one light yellow tablet each day for seven days, and then one light blue tablet each day for nine days, followed by one brown tablet each day for seven days.
4. BE SURE YOU HAVE READY AT ALL TIMES: ANOTHER KIND OF BIRTH CONTROL (such as condoms or spermicide) to use as a back-up in case you miss pills.
An EXTRA, FULL PILL PACK.
WHEN TO START THE FIRST PACK OF PILLS
You have a choice of which day to start taking your first pack of pills. Decide with your doctor or clinic which is the best day for you. Pick a time of day which will be easy to remember.
DAY-1 START:
- Pick the days of the week sticker that starts with the first day of your period. (This is the day you start bleeding or spotting, even if it is almost midnight when the bleeding begins.)
- Place the days of the week sticker on the tablet dispenser over the area that has the days of the week (starting with Sunday) printed on the card.
- Take the first “active” light pink pill of the first pack during the first 24 hours of your period.
- You will not need to use a back-up method of birth control, since you are starting the pill at the beginning of your period.
SUNDAY START:
- Take the first “active” light pink pill of the first pack on the Sunday after your period starts, even if you are still bleeding. If your period begins on Sunday, start the pack that same day.
- Use another method of birth control as a back-up method if you have sex anytime from the Sunday you start your first pack until the next Sunday (7 days). Condoms or spermicide are good back-up methods of birth control.
WHAT TO DO DURING THE MONTH
1. TAKE ONE PILL AT THE SAME TIME EVERY DAY UNTIL THE PACK IS EMPTY.
Do not skip pills even if you are spotting or bleeding between monthly periods or feel sick to your stomach (nausea).
Do not skip pills even if you do not have sex very often.
2. WHEN YOU FINISH A PACK OR SWITCH YOUR BRAND OF PILLS:
21 pills: Wait 7 days to start the next pack. You will probably have your period during that week. Be sure that no more than 7 days pass between 21-day packs.
28 pills: Start the next pack on the day after your last “reminder” pill. Do not wait any days between packs.
WHAT TO DO IF YOU MISS PILLS
If you MISS 1 light pink, light yellow, or light blue “active” pill:
1. Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
2. You do not need to use a back-up birth control method if you have sex.
If you MISS 2 “light pink or light yellow active” pills in a row in Week 1 OR Week 2 of your pack:
1. Take 2 pills on the day you remember and 2 pills the next day.
2. Then take 1 pill a day until you finish the pack.
3. You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or spermicide) as a back-up method of birth control until you have taken an “active” pill every day for 7 days.
If you MISS 2 “active” light blue pills in a row in THE 3rd WEEK:
1. If you are a Day-1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
3. You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or spermicide) as a back-up method of birth control until you have taken an “active” pill every day for 7 days.
If you MISS 3 OR MORE “active” light pink, light yellow, or light blue pills in a row (during the first 3 weeks):
1. If you are a Day-1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
3. You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or spermicide) as a back-up method of birth control until you have taken an “active” pill every day for 7 days.
REMINDER:
IF YOU FORGET ANY OF THE 7 BROWN “REMINDER” PILLS IN WEEK 4:
THROW AWAY THE PILLS YOU MISSED.
KEEP TAKING 1 PILL EACH DAY UNTIL THE PACK IS EMPTY.
YOU DO NOT NEED A BACK-UP METHOD.
FINALLY, IF YOU ARE STILL NOT SURE WHAT TO DO ABOUT THE PILLS YOU HAVE MISSED:
Use a BACK-UP METHOD anytime you have sex.
KEEP TAKING ONE “ACTIVE” PILL EACH DAY until you can reach your doctor or clinic.
Based on his or her assessment of your medical needs, your doctor or healthcare provider has prescribed this drug for you. Do not give this drug to anyone else.
Keep this and all medications out of the reach of children.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Protect from light.
Store tablets inside pouch when not in use.
Detailed Patient Package Insert
What is the most important information I should know about Tri-Legest® Fe?
Do not use Tri-Legest ® Fe if you smoke cigarettes and are over 35 years old. Smoking increases your risk of serious cardiovascular side effects (heart and blood vessel problems) from birth control pills, including death from heart attack, blood clots or stroke. This risk increases with age and the number of cigarettes you smoke.
Tri-Legest® Fe (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted diseases.
What You Should Know About Combined Oral Contraceptives
Any woman who considers using oral contraceptives (the “birth control pill” or “the pill”) should understand the benefits and risks of using this form of birth control. This leaflet will give you much of the information you will need to make this decision and will also help you determine if you are at risk of developing any of the serious side effects of the pill. It will tell you how to use the pill properly so that it will be as effective as possible. However, this leaflet is not a replacement for a careful discussion between you and your healthcare provider. You should discuss the information provided in this leaflet with him or her, both when you first start taking the pill and during your revisits. You should also follow your healthcare provider’s advice with regard to regular check-ups while you are on the pill.
EFFECTIVENESS OF COMBINEDÂ ORAL CONTRACEPTIVES
Oral contraceptives or “birth control pills” or “the pill” are used to prevent pregnancy and are more effective than other nonsurgical methods of birth control. When they are taken correctly, the chance of becoming pregnant is less than 1% (1 pregnancy per 100 women per year of use) when used perfectly, without missing any pills. Typical failure rates are actually 5% per year. The chance of becoming pregnant increases with each missed pill during a menstrual cycle.
In comparison, typical failure rates for other methods of birth control during the first year of use are as follows:
Implant: <1%
Injection: <1%
IUD: <1 to 2%
Diaphragm with spermicides: 20%
Spermicides alone: 26%
Vaginal Sponge: 20 to 40%
Female sterilization: <1%
Male sterilization: <1%
Cervical Cap: 20 to 40%
Condom alone (male): 14%
Condom alone (female): 21%
Periodic abstinence: 25%
Withdrawal: 19%
No method: 85%
Tri-Legest® Fe may also be taken to treat moderate acne if all of the following are true:
- Your doctor says it is safe for you to use the pill
- You are at least 15 years old
- You have started having menstrual periods
- You want to use the pill for birth control
- You plan to stay on the pill for at least 6 months
- Your acne has not improved with acne medicines that you put on your skin.
Norethindrone acetate and ethinyl estradiol users who started with about 74 acne pimples had about 42 pimples after 6 months of treatment. Placebo users who started with about 72 acne pimples had about 49 pimples after six months of treatment. Use Tri-Legest® Fe to treat acne only if you want the pill for birth control and plan to stay on it for at least 6 months.
WHO SHOULD NOT TAKE COMBINEDORAL CONTRACEPTIVES?
Do not take Tri-Legest® Fe if you have:
- Smoke and are over age 35 years old
- History of heart attack or stroke
- History or current blood clots in your arms, legs, lungs, or eyes
- Chest pain (angina pectoris)
- Certain heart valve problems or heart rhythm abnormalities that can cause blood clots to form in the heart
- Problem with your blood that makes it clot more than normal
- High blood pressure that medicine cannot control
- Diabetes with kidney, eye, nerve or blood vessel damage
- Certain kinds of severe migraine headaches with aura, numbness, weakness or changes in vision, or have any migraine headache if you are over age 35
- Known or suspected breast cancer
- Unexplained vaginal bleeding
- Yellowing of the whites of the eyes or of the skin (jaundice) during pregnancy or during previous use of the pill
- Liver problems, including liver tumors
- Known or suspected pregnancy
- Are receiving Hepatitis C drug combination containing ombitasvir/paritaprevir/ ritonavir, with or without dasabuvir. This may increase levels of the liver enzyme “alanine aminotransferase” (ALT) in the blood.
If any of these conditions happen while you are taking Tri-Legest® Fe, stop taking Tri-Legest® Fe right away and talk with your healthcare provider. Your healthcare provider can recommend a safer method of birth control.
Before you use Tri-Legest® Fe, tell your healthcare provider if you:
- Are pregnant or think you are pregnant
- Have any medical conditions, including conditions uled above
- Elevated cholesterol or triglycerides
- Are depressed now or have been depressed in the past
- Are breastfeeding or plan to breastfeed
- Gallbladder disease
- History of scanty or irregular menstrual periods
RISKS OF TAKING COMBINEDÂ ORAL CONTRACEPTIVES
1. Risk of Developing Blood Clots
Blood clots and blockage of blood vessels are the most serious side effects of taking oral contraceptives; in particular, a clot in the leg can cause thrombophlebitis, and a clot that travels to the lungs can cause a sudden blocking of the vessel carrying blood to the lungs. Rarely, clots occur in the blood vessels of the eye and may cause blindness, double vision, or impaired vision.
If you take oral contraceptives and need elective surgery, need to stay in bed for a prolonged illness, or have recently delivered a baby, you may be at risk of developing blood clots. You should consult your doctor about stopping oral contraceptives three to four weeks before surgery and not taking oral contraceptives for two weeks after surgery or during bed rest. You should also not take oral contraceptives soon after delivery of a baby. It is advisable to wait for at least four weeks after delivery if you are not breastfeeding. If you are breastfeeding, you should wait until you have weaned your child before using the pill. (See also the section on Breastfeeding in GENERAL PRECAUTIONS .)
2. Heart Attacks and Strokes
Oral contraceptives may increase the tendency to develop strokes (stoppage or rupture of blood vessels in the brain) and angina pectoris and heart attacks (blockage of blood vessels in the heart). Any of these conditions can cause death or disability.
Smoking greatly increases the possibility of suffering heart attacks and strokes. Furthermore, smoking and the use of oral contraceptives greatly increase the chances of developing and dying of heart disease.
3. Gallbladder Disease
Oral contraceptive users probably have a greater risk than nonusers of having gallbladder disease, although this risk may be related to pills containing high doses of estrogens.
4. Liver Tumors
In rare cases, oral contraceptives can cause benign but dangerous liver tumors. These benign liver tumors can rupture and cause fatal internal bleeding. In addition, a possible but not definite association has been found with the pill and liver cancers in two studies, in which a few women who developed these very rare cancers were found to have used oral contraceptives for long periods. However, liver cancers are extremely rare. The chance of developing liver cancer from using the pill is thus even rarer.
5. Risk of Cancer
It is not known if hormonal birth control pills cause breast cancer. Some studies, but not all, suggest that there could be a slight increase in the risk of breast cancer among current users with longer duration of use.
If you have breast cancer now, or have had it in the past, do not use hormonal birth control because some breast cancers are sensitive to hormones.
Some studies have found an increase in the incidence of precancerous lesions of the cervix in women who use oral contraceptives. However, this finding may be related to factors other than the use of oral contraceptives.
ESTIMATED RISK OF DEATH FROM A BIRTH CONTROL METHOD OR PREGNANCY
All methods of birth control and pregnancy are associated with a risk of developing certain diseases which may lead to disability or death. An estimate of the number of deaths associated with different methods of birth control and pregnancy has been calculated and is shown in the following table.
Annual Number of Birth-Related or Method-Related Deaths Associated with Control of Fertility Per 100,000 Nonsterile Women by Fertility Control Method According to Age
Method of control and outcome
15 to 19
20 to 24
25 to 29
30 to 34
35 to 39
40 to 44
No fertility control methods*
7.0
7.4
9.1
14.8
25.7
28.2
Oral contraceptives non-smoker**
0.3
0.5
0.9
1.9
13.8
31.6
Oral contraceptives smoker**
2.2
3.4
6.6
13.5
51.1
117.2
IUD**
0.8
0.8
1.0
1.0
1.4
1.4
Condom*
1.1
1.6
0.7
0.2
0.3
0.4
Diaphragm/spermicide*
1.9
1.2
1.2
1.3
2.2
2.8
Periodic abstinence*
2.5
1.6
1.6
1.7
2.9
3.6
 *Deaths are birth-related
**Deaths are method-related
 In the above table, the risk of death from any birth control method is less than the risk of childbirth, except for oral contraceptive users over the age of 35 who smoke and pill users over the age of 40 even if they do not smoke. It can be seen in the table that for women aged 15 to 39, the risk of death was highest with pregnancy (7 to 26 deaths per 100,000 women, depending on age). Among pill users who do not smoke, the risk of death was always lower than that associated with pregnancy for any age group, although over the age of 40, the risk increases to 32 deaths per 100,000 women, compared to 28 associated with pregnancy at that age. However, for pill users who smoke and are over the age of 35, the estimated number of deaths exceeds those for other methods of birth control. If a woman is over the age of 40 and smokes, her estimated risk of death is four times higher (117/100,000 women) than the estimated risk associated with pregnancy (28/100,000 women) in that age group.
The suggestion that women over 40 who don’t smoke should not take oral contraceptives is based on information from older higher dose pills and on less selective use of pills than is practiced today. An Advisory Committee of the FDA discussed this issue in 1989 and recommended that the benefits of oral contraceptive use by healthy, non-smoking women over 40 years of age may outweigh the possible risks. However, all women, especially older women, are cautioned to use the lowest dose pill that is effective.
WARNING SIGNALS
If any of these adverse effects occur while you are taking oral contraceptives, call your doctor immediately:
- Sharp chest pain, coughing of blood, or sudden shortness of breath (indicating a possible clot in the lung)
- Pain in the calf (indicating a possible clot in the leg)
- Crushing chest pain or heaviness in the chest (indicating a possible heart attack)
- Sudden severe headache or vomiting, dizziness or fainting, disturbances of vision or speech, weakness, or numbness in an arm or leg (indicating a possible stroke)
- Sudden partial or complete loss of vision (indicating a possible clot in the eye)
- Breast lumps (indicating possible breast cancer or fibrocystic disease of the breast; ask your doctor or healthcare provider to show you how to examine your breasts)
- Severe pain or tenderness in the stomach area (indicating a possible ruptured liver tumor)
- Difficulty in sleeping, weakness, lack of energy, fatigue, or change in mood (possibly indicating severe depression)
- Jaundice or a yellowing of the skin or eyeballs, accompanied frequently by fever, fatigue, loss of appetite, dark colored urine, or light-colored bowel movements (indicating possible liver problems)
SIDE EFFECTS OF COMBINEDÂ ORAL CONTRACEPTIVES
1. Vaginal Bleeding
Irregular vaginal bleeding or spotting may occur while you are taking the pills. Irregular bleeding may vary from slight staining between menstrual periods to breakthrough bleeding which is a flow much like a regular period. Irregular bleeding occurs most often during the first few months of oral contraceptive use, but may also occur after you have been taking the pill for some time. Such bleeding may be temporary and usually does not indicate serious problems. It is important to continue taking your pills on schedule. If the bleeding occurs in more than one cycle or lasts for more than a few days, talk to your doctor or healthcare provider.
2. Contact Lenses
If you wear contact lenses and notice a change in vision or an inability to wear your lenses, contact your doctor or healthcare provider.
3. Fluid Retention
Oral contraceptives may cause edema (fluid retention) with swelling of the fingers or ankles and may raise your blood pressure. If you experience fluid retention, contact your doctor or healthcare provider.
4. Chloasma
A spotty darkening of the skin is possible, particularly of the face.
5. Other Side Effects
Other side effects may include change in appetite, headache, nervousness, depression, dizziness, loss of scalp hair, rash, and vaginal infections. If any of these side effects bother you, call your doctor or healthcare provider.
GENERAL PRECAUTIONS
1. Missed Periods and Use of Combined Oral Contraceptives Before or During Early Pregnancy
There may be times when you may not menstruate regularly after you have completed taking a cycle of pills. If you have taken your pills regularly and miss one menstrual period, continue taking your pills for the next cycle but be sure to inform your healthcare provider before doing so. If you have not taken the pills daily as instructed and missed a menstrual period, or if you missed two consecutive menstrual periods, you may be pregnant. Check with your healthcare provider immediately to determine whether you are pregnant. Do not continue to take oral contraceptives until you are sure you are not pregnant, but continue to use another method of contraception.
There is no conclusive evidence that oral contraceptive use is associated with an increase in birth defects, when taken inadvertently during early pregnancy. Previously, a few studies had reported that oral contraceptives might be associated with birth defects, but these studies have not been confirmed. Nevertheless, oral contraceptives or any other drugs should not be used during pregnancy unless clearly necessary and prescribed by your doctor. You should check with your doctor about risks to your unborn child of any medication taken during pregnancy.
2. While Breastfeeding
If you are breastfeeding, consult your doctor before starting oral contraceptives. Some of the drug will be passed on to the child in the milk. A few adverse effects on the child have been reported, including yellowing of the skin (jaundice) and breast enlargement. In addition, oral contraceptives may decrease the amount and quality of your milk. If possible, do not use oral contraceptives while breastfeeding. You should use another method of contraception since breastfeeding provides only partial protection from becoming pregnant, and this partial protection decreases significantly as you breastfeed for longer periods of time. You should consider starting oral contraceptives only after you have weaned your child completely.
3. Laboratory Tests
If you are scheduled for any laboratory tests, tell your doctor you are taking birth control pills. Certain blood tests may be affected by birth control pills.
4. Drug Interactions
Certain drugs may interact with birth control pills to make them less effective in preventing pregnancy or cause an increase in breakthrough bleeding. Such drugs include rifampin; drugs used for epilepsy such as barbiturates (for example, phenobarbital), carbamazepine, and phenytoin (Dilantin® is one brand of this drug); phenylbutazone; and possibly St. John’s Wort and certain antibiotics. You may need to use additional contraception when you take drugs which can make oral contraceptives less effective.
Birth control pills may interact with lamotrigine, an anticonvulsant used for epilepsy. This may increase the risk of seizures, so your healthcare provider may need to adjust the dose of lamotrigine. Birth control pills interact with certain drugs. These drugs include acetaminophen, clofibric acid, cyclosporine, morphine, prednisolone, salicylic acid, temazepam, and theophylline. You should tell your doctor if you are taking any of these medications.
5. Sexually Transmitted Diseases
Tri-Legest® Fe (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted diseases such as Chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
INSTRUCTIONS TO PATIENT
TABLET DISPENSER
The Tri-Legest® Fe tablet dispenser has been designed to make oral contraceptive dosing as easy and as convenient as possible. The tablets are arranged in four rows of seven tablets each, with the days of the week appearing above the first row of tablets.
Each light pink tablet contains 1 mg norethindrone acetate and 20 mcg ethinyl estradiol.
Each light yellow tablet contains 1 mg norethindrone acetate and 30 mcg ethinyl estradiol.
Each light blue tablet contains 1 mg norethindrone acetate and 35 mcg ethinyl estradiol.
Each brown tablet contains 75 mg ferrous fumarate and is intended to help you remember to take the tablets correctly. These brown tablets are not intended to have any health benefit.
DIRECTIONS
To remove a tablet, press down on it with your thumb or finger. The tablet will drop through the back of the tablet dispenser. Do not press with your thumbnail, fingernail, or any other sharp object.Â
HOW TO TAKE THE PILL
IMPORTANT POINTS TO REMEMBER
BEFORE YOU START TAKING YOUR PILLS:
1. BE SURE TO READ THESE DIRECTIONS:
Before you start taking your pills.
Anytime you are not sure what to do.
2. THE RIGHT WAY TO TAKE THE PILL IS TO TAKE ONE PILL EVERY DAY AT THE SAME TIME. If you miss pills you could get pregnant. This includes starting the pack late. The more pills you miss, the more likely you are to get pregnant.
3. MANY WOMEN HAVE SPOTTING OR LIGHT BLEEDING, OR MAY FEEL SICK TO THEIR STOMACH, DURING THE FIRST 1 to 3 PACKS OF PILLS. If you do have spotting or light bleeding or feel sick to your stomach, do not stop taking the pill. The problem will usually go away. If it doesn’t go away, check with your doctor or clinic.
4. MISSING PILLS CAN ALSO CAUSE SPOTTING OR LIGHT BLEEDING, even when you make up these missed pills. On the days you take 2 pills to make up for missed pills, you could also feel a little sick to your stomach.
5. IF YOU HAVE VOMITING OR DIARRHEA, for any reason, or IF YOU TAKE SOME MEDICINES, including some antibiotics, your birth control pills may not work as well. Use a back-up birth control method (such as condoms or spermicide) until you check with your doctor or clinic.
6. IF YOU HAVE TROUBLE REMEMBERING TO TAKE THE PILL, talk to your doctor or clinic about how to make pill-taking easier or about using another method of birth control.
7. IF YOU HAVE ANY QUESTIONS OR ARE UNSURE ABOUT THE INFORMATION IN THIS LEAFLET, call your doctor or clinic.
BEFORE YOU START TAKING YOUR PILLS
1. DECIDE WHAT TIME OF DAY YOU WANT TO TAKE YOUR PILL. It is important to take it at about the same time every day.
2. LOOK AT YOUR PILL PACK. The pill pack has 21 “active” pills (5 light pink, 7 light yellow, and 9 light blue tablets - with hormones) to take for 3 weeks, followed by 1 week of "reminder" brown pills (without hormones).
3. ALSO FIND:     1) where on the pack to start taking pills,     2) in what order to take the pills (follow the arrows), and     3) the week numbers are shown in the following pictures:
Each Tri-Legest® Fe tablet dispenser contains 5 light pink, 7 light yellow, and 9 light blue pills for Weeks 1, 2, and 3. Week 4 will contain BROWN PILLS ONLY. These tablets are to be taken in the following order: one light pink tablet each day for five days, one light yellow tablet each day for seven days, and then one light blue tablet each day for nine days, followed by one brown tablet each day for seven days.
4. BE SURE YOU HAVE READY AT ALL TIMES: ANOTHER KIND OF BIRTH CONTROL (such as condoms or spermicide) to use as a back-up in case you miss pills.
An EXTRA, FULL PILL PACK.
WHEN TO START THE FIRST PACK OF PILLS
You have a choice of which day to start taking your first pack of pills. Decide with your doctor or clinic which is the best day for you. Pick a time of day which will be easy to remember.
DAY-1 START:
- Pick the days of the week sticker that starts with the first day of your period. (This is the day you start bleeding or spotting, even if it is almost midnight when the bleeding begins.)
- Place the days of the week sticker on the tablet dispenser over the area that has the days of the week (starting with Sunday) printed on the card.
- Take the first “active” light pink pill of the first pack during the first 24 hours of your period.
- You will not need to use a back-up method of birth control, since you are starting the pill at the beginning of your period.
SUNDAY START:
- Take the first “active” light pink pill of the first pack on the Sunday after your period starts, even if you are still bleeding. If your period begins on Sunday, start the pack that same day.
- Use another method of birth control as a back-up method if you have sex anytime from the Sunday you start your first pack until the next Sunday (7 days). Condoms or spermicide are good back-up methods of birth control.
WHAT TO DO DURING THE MONTH
1. TAKE ONE PILL AT THE SAME TIME EVERY DAY UNTIL THE PACK IS EMPTY.
Do not skip pills even if you are spotting or bleeding between monthly periods or feel sick to your stomach (nausea).
Do not skip pills even if you do not have sex very often.
2. WHEN YOU FINISH A PACK OR SWITCH YOUR BRAND OF PILLS:
21 pills: Wait 7 days to start the next pack. You will probably have your period during that week. Be sure that no more than 7 days pass between 21-day packs.
28 pills: Start the next pack on the day after your last “reminder” pill. Do not wait any days between packs.
WHAT TO DO IF YOU MISS PILLS
If you MISS 1 light pink, light yellow, or light blue “active” pill:
1. Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
2. You do not need to use a back-up birth control method if you have sex.
If you MISS 2 “active” light pink or light yellow pills in a row in Week 1 OR Week 2 of your pack:
1. Take 2 pills on the day you remember and 2 pills the next day.
2. Then take 1 pill a day until you finish the pack.
3. You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or spermicide) as a back-up method of birth control until you have taken an “active” pill every day for 7 days.
If you MISS 2 “active” light blue pills in a row in THE 3rd WEEK:
1. If you are a Day-1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
3. You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or spermicide) as a back-up method of birth control until you have taken an “active” pill every day for 7 days.
If you MISS 3 OR MORE “active” light pink, light yellow, or light blue pills in a row (during the first 3 weeks):
1. If you are a Day-1 Starter:
THROW OUT the rest of the pill pack and start a new pack that same day.
If you are a Sunday Starter:
Keep taking 1 pill every day until Sunday.
On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day.
2. You may not have your period this month, but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
3. You COULD GET PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms or spermicide) as a back-up method of birth control until you have taken an “active” pill every day for 7 days.
REMINDER:
IF YOU FORGET ANY OF THE 7 BROWN “REMINDER” PILLS IN WEEK 4:
THROW AWAY THE PILLS YOU MISSED.
KEEP TAKING 1 PILL EACH DAY UNTIL THE PACK IS EMPTY.
YOU DO NOT NEED A BACK-UP METHOD.
FINALLY, IF YOU ARE STILL NOT SURE WHAT TO DO ABOUT THE PILLS YOU HAVE MISSED:
Use a BACK-UP METHOD anytime you have sex.
KEEP TAKING ONE “ACTIVE” PILL EACH DAY until you can reach your doctor or clinic.
PREGNANCY DUE TO PILL FAILURE
The incidence of pill failure resulting in pregnancy is approximately 1% (i.e., one pregnancy per 100 women per year) if taken every day as directed, but more typical failure rates are about 5%. If failure does occur, the risk to the fetus is minimal.
PREGNANCY AFTER STOPPING THE PILL
There may be some delay in becoming pregnant after you stop using oral contraceptives, especially if you had irregular menstrual cycles before you used oral contraceptives. It may be advisable to postpone conception until you begin menstruating regularly once you have stopped taking the pill and desire pregnancy.
There does not appear to be any increase in birth defects in newborn babies when pregnancy occurs soon after stopping the pill.
OVERDOSAGE
Serious ill effects have not been reported following ingestion of large doses of oral contraceptives by young children. Overdosage may cause nausea and withdrawal bleeding in females. In case of overdosage, contact your healthcare provider or pharmacist.
OTHER INFORMATION
Your healthcare provider will take a medical and family history and examine you before prescribing oral contraceptives. The physical examination may be delayed to another time if you request it and your healthcare provider believes that it is a good medical practice to postpone it. You should be reexamined at least once a year. Be sure to inform your healthcare provider if there is a family history of any of the conditions uled previously in this leaflet. Be sure to keep all appointments with your healthcare provider, because this is a time to determine if there are early signs of side effects of oral contraceptive use.
Do not use the drug for any condition other than the one for which it was prescribed. This drug has been prescribed specifically for you; do not give it to others who may want birth control pills.
HEALTH BENEFITS FROMÂ COMBINEDÂ ORAL CONTRACEPTIVES
In addition to preventing pregnancy, use of oral contraceptives may provide certain benefits. They are:
- Menstrual cycles may become more regular.
- Blood flow during menstruation may be lighter and less iron may be lost. Therefore, anemia due to iron deficiency is less likely to occur.
- Pain or other symptoms during menstruation may be encountered less frequently.
- Ectopic (tubal) pregnancy may occur less frequently.
- Noncancerous cysts or lumps in the breast may occur less frequently.
- Acute pelvic inflammatory disease may occur less frequently.
- Oral contraceptive use may provide some protection against developing two forms of cancer: cancer of the ovaries and cancer of the lining of the uterus.
If you want more information about birth control pills, ask your doctor or pharmacist. They have a more technical leaflet called the “Physician Insert”, which you may wish to read.
Remembering to take tablets according to schedule is stressed because of its importance in providing you the greatest degree of protection.
MISSED MENSTRUAL PERIODS
At times there may be no menstrual period after a cycle of pills. Therefore, if you miss one menstrual period but have taken the pills exactly as you were supposed to, continue as usual into the next cycle. If you have not taken the pills correctly and miss a menstrual period, you may be pregnant and should stop taking oral contraceptives until your doctor or healthcare provider determines whether or not you are pregnant. Until you can get to your doctor or healthcare provider, use another form of contraception. If two consecutive menstrual periods are missed, you should stop taking pills until it is determined whether or not you are pregnant. Although there does not appear to be any increase in birth defects in newborn babies, if you become pregnant while using oral contraceptives, you should discuss the situation with your doctor or healthcare provider.
Periodic Examination
Your doctor or healthcare provider will take a complete medical and family history before prescribing oral contraceptives. At that time and about once a year thereafter, he or she will generally examine your blood pressure, breasts, abdomen, and pelvic organs (including a Papanicolaou smear, i.e., test for cancer).
Keep this and all medications out of the reach of children.
Store 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Protect from light.
Store tablets inside pouch when not in use.
Teva Pharmaceuticals USA, Inc. North Wales, PA 19454
Rev. E 3/2023
Package/label Display Panel, Part 1 Of 2
NDCÂ 0555-9032-70
5 Tablet Dispensers x 28 Tablets 28 DAY REGIMEN
Tri-Legest® Fe
(norethindrone acetate and
ethinyl estradiol tablets, USP
and ferrous fumarate tablets*)
Each cycle pack contains the following:
Each light pink tablet (5) contains 1 mg norethindrone acetate
and 20 mcg ethinyl estradiol.
Each light yellow tablet (7) contains 1 mg norethindrone acetate
and 30 mcg ethinyl estradiol.
Each light blue tablet (9) contains 1 mg norethindrone acetate
and 35 mcg ethinyl estradiol.
Each brown tablet (7) contains ferrous fumarate 75 mg.
*Ferrous fumarate tablets are not USP for dissolution and assay.
Rx only
SHAPINGWOMEN'S HEALTH®
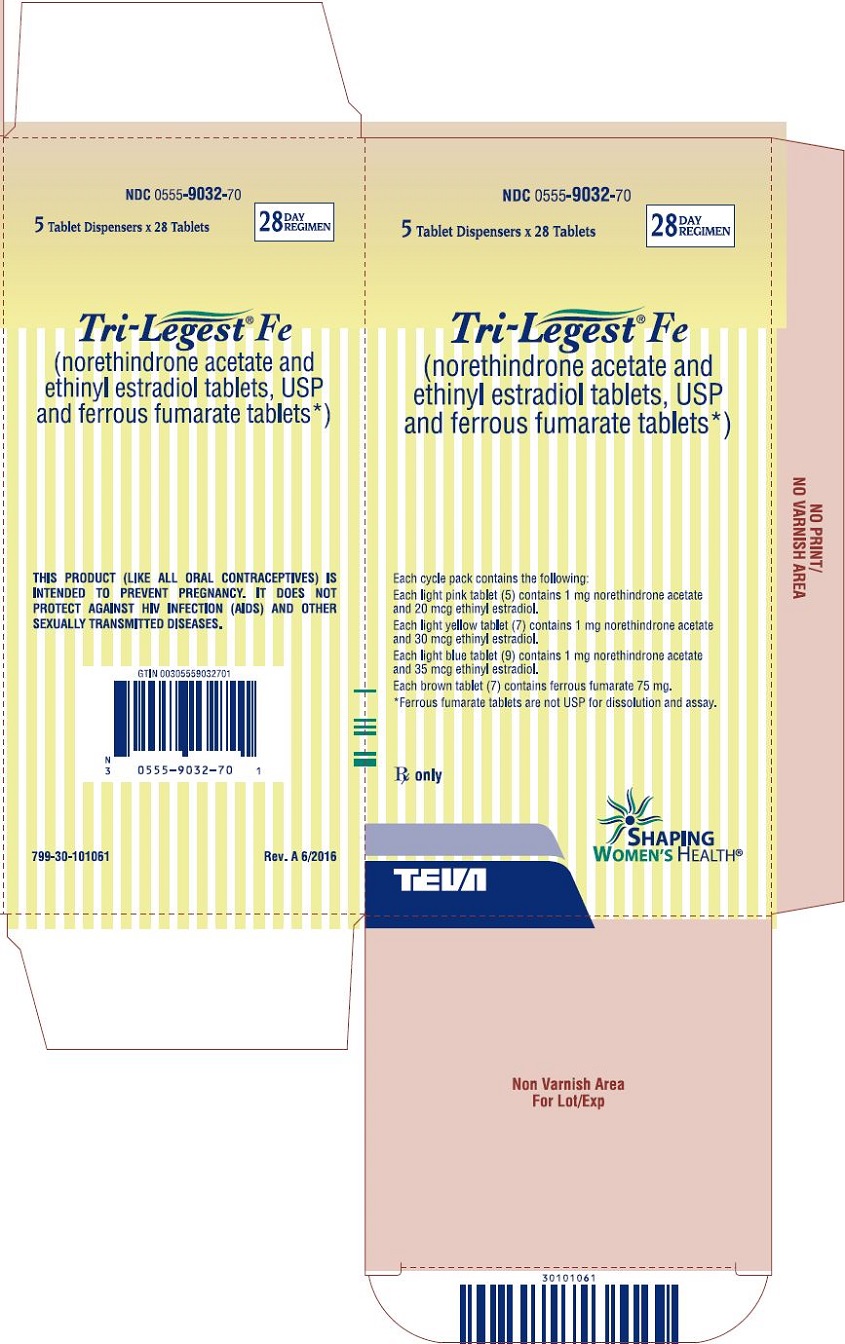
Package/label Display Panel, Part 2 Of 2
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site