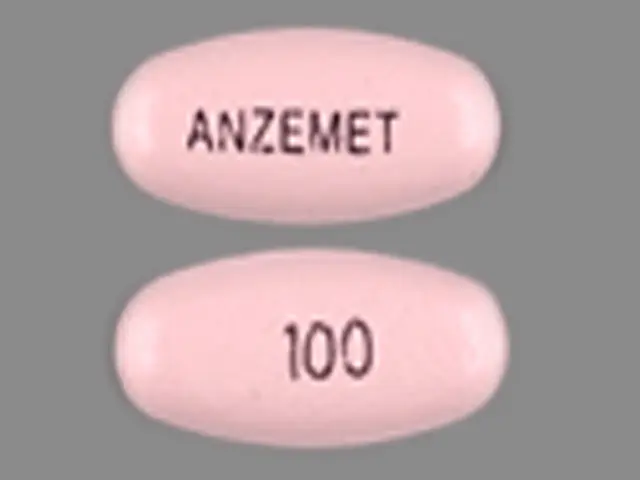
Anzemet (dolasetron mesylate 100 mg) Dailymed
Generic: dolasetron mesylate
IMPRINT: 100 ANZEMET
SHAPE: oval
COLOR: pink
All Imprints
dolasetron mesylate 50 mg - a 50 round pink
dolasetron mesylate 100 mg - 100 anzemet oval pink
Go PRO for all pill images
Description
ANZEMET (dolasetron mesylate) is an antinauseant and antiemetic agent. Chemically, dolasetron mesylate is (2α,6α,8α,9aβ)-octahydro-3-oxo-2,6-methano-2H-quinolizin-8-yl-1H-indole-3-carboxylate monomethanesulfonate, monohydrate. It is a highly specific and selective serotonin subtype 3 (5-HT3) receptor antagonist both in vitro and in vivo. Dolasetron mesylate has the following structural formula:
![]()
The empirical formula is C19H20N2O3 • CH3SO3H • H2O, with a molecular weight of 438.50. Approximately 74% of dolasetron mesylate monohydrate is dolasetron base.
Dolasetron mesylate monohydrate is a white to off-white powder that is freely soluble in water and propylene glycol, slightly soluble in ethanol, and slightly soluble in normal saline.
Each ANZEMET Tablet for oral administration contains dolasetron mesylate (as the monohydrate) and also contains the inactive ingredients: carnauba wax, croscarmellose sodium, hypromellose, lactose, magnesium stearate, polyethylene glycol, polysorbate 80, pregelatinized starch, synthetic red iron oxide, titanium dioxide, and white wax. The tablets are printed with black ink, which contains lecithin, pharmaceutical glaze, propylene glycol, and synthetic black iron oxide.
Clinical Pharmacology
Dolasetron mesylate and its active metabolite, hydrodolasetron (MDL 74,156), are selective serotonin 5-HT3 receptor antagonists not shown to have activity at other known serotonin receptors and with low affinity for dopamine receptors. The serotonin 5-HT3 receptors are located on the nerve terminals of the vagus in the periphery and centrally in the chemoreceptor trigger zone of the area postrema. It is thought that chemotherapeutic agents produce nausea and vomiting by releasing serotonin from the enterochromaffin cells of the small intestine, and that the released serotonin then activates 5-HT3 receptors located on vagal efferents to initiate the vomiting reflex.
In healthy volunteers (N=64), dolasetron mesylate in single intravenous doses up to 5 mg/kg produced no effect on pupil size or meaningful changes in EEG tracings. Results from neuropsychiatric tests revealed that dolasetron mesylate did not alter mood or concentration. Multiple daily doses of dolasetron have had no effect on colonic transit in humans. Dolasetron has no effect on plasma prolactin concentrations.
Effects on Electrocardiogram
QTcF interval was evaluated in a randomized, placebo and active (moxifloxacin 400 mg once-daily) controlled crossover study in 80 healthy adults, with 14 measurements over 24 hours on Day 4. The maximum mean (95% upper confidence bound) differences in QTcF from placebo after baseline-correction were 14.1 (16.1) and 36.6 (38.6) ms for 100 mg and supratherapeutic 300 mg ANZEMET, administered intravenously, respectively. ANZEMET 300 mg once daily resulted in approximately 3-fold higher mean Cmax values of dolasetron mesylate and its active metabolite hydrodolasetron on Day 4 compared to those observed with the therapeutic 100 mg ANZEMET dose.
Based on exposure-response analysis in healthy volunteers, QTc interval prolongations appear to be associated with concentrations of hydrodolasetron. Using the established exposure-response relationship, the mean predicted increase (95% upper prediction interval) in QTcF intervals were 16.0 (17.1) and 17.9 (19.1) ms for renally impaired and elderly subjects following an oral dose of 100 mg.
In the thorough QT study, exposure dependent prolongation of the PR and QRS interval was also noted in healthy subjects receiving ANZEMET. The maximum mean (95% upper confidence bound) difference in PR from placebo after baseline-correction was 9.8 (11.6) ms and 33.1 (34.9) ms for 100 mg and supratherapeutic 300 mg ANZEMET, respectively. The maximum mean (95% upper confidence bound) difference in QRS from placebo after baseline-correction was 3.5 (4.5) ms and 13 (14.5) ms for 100 mg and supratherapeutic 300 mg ANZEMET, respectively. Over one-fourth of the subjects treated with the 300 mg dose had an absolute PR over 200 ms and absolute QRS of over 110 ms post-treatment. A change from baseline ≥ 25% was noted in several of these subjects. (seeWARNINGS)
Pharmacokinetics in Humans
Oral dolasetron is well absorbed, although parent drug is rarely detected in plasma due to rapid and complete metabolism to the most clinically relevant species, hydrodolasetron.
The reduction of dolasetron to hydrodolasetron is mediated by a ubiquitous enzyme, carbonyl reductase. Cytochrome P-450 (CYP)2D6 is primarily responsible for the subsequent hydroxylation of hydrodolasetron and both CYP3A and flavin monooxygenase are responsible for the N-oxidation of hydrodolasetron.
Hydrodolasetron is excreted in the urine unchanged (61.0% of administered oral dose). Other urinary metabolites include hydroxylated glucuronides and N-oxide.
Hydrodolasetron appears rapidly in plasma, with a maximum concentration occurring approximately 1 hour after dosing, and is eliminated with a mean half-life of 8.1 hours (%CV=18%) and an apparent clearance of 13.4 mL/min/kg (%CV=29%) in 30 adults. The apparent absolute bioavailability of oral dolasetron, determined by the major active metabolite hydrodolasetron, is approximately 75%. Orally administered dolasetron intravenous solution and tablets are bioequivalent. Food does not affect the bioavailability of dolasetron taken by mouth.
Hydrodolasetron is eliminated by multiple routes, including renal excretion and, after metabolism, mainly, glucuronidation and hydroxylation. Two thirds of the administered dose is recovered in the urine and one third in the feces. Hydrodolasetron is widely distributed in the body with a mean apparent volume of distribution of 5.8 L/kg (%CV=25%, N=24) in adults.
Sixty-nine to 77% of hydrodolasetron is bound to plasma protein. In a study with 14C labeled dolasetron, the distribution of radioactivity to blood cells was not extensive. Approximately 50% of hydrodolasetron is bound to α1-acid glycoprotein. The pharmacokinetics of hydrodolasetron are linear and similar in men and women.
The pharmacokinetics of hydrodolasetron, in special and targeted patient populations following oral administration of dolasetron, are summarized in Table 1. The pharmacokinetics of hydrodolasetron are similar in adult (young and elderly) healthy volunteers and in adult cancer patients receiving chemotherapeutic agents. The apparent clearance following oral administration of hydrodolasetron is approximately 1.6- to 3.4-fold higher in children and adolescents than in adults. The clearance following oral administration of hydrodolasetron is not affected by age in adult cancer patients. The apparent oral clearance of hydrodolasetron decreases 42% with severe hepatic impairment and 44% with severe renal impairment. No dose adjustment is necessary for renally impaired or elderly patients, however ECG monitoring is recommended (seeWARNINGSandPRECAUTIONS, Geriatric Use). No dose adjustment is recommended for patients with hepatic impairment.
The pharmacokinetics of ANZEMET Tablets have not been studied in the pediatric population. However, the following pharmacokinetic data are available on intravenous ANZEMET Injection administered orally to children.
Thirty-two pediatric cancer patients ages 3 to 11 years (N=19) and 12 to 17 years (N=13), received 0.6, 1.2, or 1.8 mg/kg ANZEMET Injection diluted with either apple or apple-grape juice and administered orally. In this study, the mean apparent clearances of hydrodolasetron were 3 times greater in the younger pediatric group and 1.8 times greater in the older pediatric group than those observed in healthy adult volunteers. Across this spectrum of pediatric patients, maximum plasma concentrations were 0.6 to 0.7 times those observed in healthy adults receiving similar doses.
For 12 pediatric patients, ages 2 to 12 years receiving 1.2 mg/kg ANZEMET Injection diluted in apple or apple-grape juice and administered orally, the mean apparent clearance was 34% greater and half-life was 21% shorter than in healthy adults receiving the same dose.
The table below summarizes the pharmacokinetic data from multiple populations. Please note that the doses studied may have exceeded the maximum recommended dose.
Table 1. Pharmacokinetic Values for Plasma Hydrodolasetron Following Oral Administration of ANZEMET : mean values Age(years) Dose CLapp (mL/min/kg) t1/2 (h) Cmax (ng/mL) CLapp: apparent clearance t1/2: terminal elimination half-life ( ): coefficient of variation in % Young Healthy Volunteers (N=30) 19–45 200 mg 13.4 (29%) 8.1 (18%) 556 (28%) Elderly Healthy Volunteers (N=15) 65–75 2.4 mg/kg 9.5 (36%) 7.2 (32%) 662 (28%) Cancer Patients   Adults (N=61) : analyzed by nonlinear mixed effect modeling with data pooled across dose strengths 24–84 25–200 mg 12.9 (49%) 7.9 (43%) -- : sampling times did not allow calculation   Adolescents (N=13) 12–17 0.6–1.8 mg/kg 26.5 (67%) 6.4 (30%) 374 : results from adolescents (dose=1.8 mg/kg, N=3) the maximum dose exceeded 100 mg. When data from patients who received greater than 47 mg (N=9) are combined and normalized to the 1.8 mg/kg dose with a cap of 100 mg, the mean Cmax was 229 ng/mL (51%). (32%)  Children (N=19) 3–11 0.6–1.8 mg/kg 44.2 (49%) 5.5 (39%) 217 : results from children (dose=1.8 mg/kg, N=7) (67%)Patients with Severe Renal Impairment (N=12)(Creatinine clearance ≤10 mL/min) 28–74 200 mg 7.2 (48%) 10.7 (29%) 701 (21%) Patients with Severe Hepatic Impairment (N=3) 42–52 150 mg 8.8 (57%) 11.0 (36%) 410 (12%) Clinical Studies
Oral ANZEMET at a dose of 100 mg prevents nausea and vomiting associated with moderately emetogenic cancer therapy as shown by 24 hour efficacy data from two double-blind studies. Efficacy was based on complete response (i.e., no vomiting, no rescue medication).
The first randomized, double-blind trial compared single oral ANZEMET doses of 25, 50, 100 and 200 mg in 60 men and 259 women cancer patients receiving cyclophosphamide and/or doxorubicin. There was no statistically significant difference in complete response between the 100 mg and 200 mg dose. Results are summarized in Table 2.
Table 2. Prevention of Chemotherapy-Induced Nausea and Vomiting from Moderately Emetogenic Chemotherapy Response Over 24 Hours ANZEMET Tablets 25 mg(N=78) 50 mg(N=83) 100 mg : The recommended dose (N=80)200 mg(N=78) p-value for Linear Trend Complete Response : No emetic episodes and no rescue medication. 24 (31%) 34 (41%) 49 (61%) 46 (59%) P<.0001 Nausea Score : Median 24-h change from baseline nausea score using visual analog scale (VAS): Score range 0="none" to 100="nausea as bad as it could be." 49 10 11 7 P=.0006
Another trial also compared single oral ANZEMET doses of 25, 50, 100, and 200 mg in 307 patients receiving moderately emetogenic chemotherapy. In this study, the 100 mg ANZEMET dose gave a 73% complete response rate.
Indications And Usage
ANZEMET Tablets are indicated for the prevention of nausea and vomiting associated with moderately emetogenic cancer chemotherapy, including initial and repeat courses in adults and children 2 years and older.
Contraindications
ANZEMET Tablets are contraindicated in patients known to have hypersensitivity to the drug.
Warnings
QT Interval Prolongation
ANZEMET prolongs the QT interval in a dose dependent fashion. Torsade de Pointes has been reported during post-marketing experience. Avoid ANZEMET in patients with congenital long QT syndrome, hypomagnesemia, or hypokalemia. Hypokalemia and hypomagnesemia must be corrected prior to ANZEMET administration. Monitor these electrolytes after administration as clinically indicated. Use ECG monitoring in patients with congestive heart failure, bradycardia, renal impairment, and elderly patients (seeCLINICAL PHARMACOLOGY).
PR and QRS Interval Prolongation
ANZEMET has been shown to cause dose dependent prolongation of the PR and QRS interval and reports of second or third degree atrioventricular block, cardiac arrest and serious ventricular arrhythmias including fatalities in both adult and pediatric patients. At particular risk are patients with underlying structural heart disease and preexisting conduction system abnormalities, elderly, patients with sick sinus syndrome, patients with atrial fibrillation with slow ventricular response, patients with myocardial ischemia or patients receiving drugs known to prolong the PR interval (such as verapamil) and QRS interval (e.g., flecainide or quinidine). ANZEMET should be used with caution and with ECG monitoring in these patients. ANZEMET should be avoided in patients with complete heart block or at risk for complete heart block, unless they have an implanted pacemaker (seeCLINICAL PHARMACOLOGY).
Serotonin Syndrome
The development of serotonin syndrome has been reported with 5-HT3 receptor antagonists. Most reports have been associated with concomitant use of serotonergic drugs (e.g., selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors, mirtazapine, fentanyl, lithium, tramadol, and intravenous methylene blue). Some of the reported cases were fatal. Serotonin syndrome occurring with overdose of another 5-HT3 receptor antagonist alone has also been reported. The majority of reports of serotonin syndrome related to 5-HT3 receptor antagonist use occurred in a post-anesthesia care unit or an infusion center.
Symptoms associated with serotonin syndrome may include the following combination of signs and symptoms: mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome, especially with concomitant use of Anzemet and other serotonergic drugs. If symptoms of serotonin syndrome occur, discontinue Anzemet and initiate supportive treatment. Patients should be informed of the increased risk of serotonin syndrome, especially if Anzemet is used concomitantly with other serotonergic drugs (see DRUG INTERACTIONS, Patient Counseling Information).
Precautions
General
Dolasetron should be administered with caution in patients who have or may develop prolongation of cardiac conduction intervals, particularly QTc. These include patients with hypokalemia or hypomagnesemia, patients taking diuretics with potential for inducing electrolyte abnormalities, patients with congenital QT syndrome, patients taking anti-arrhythmic drugs or other drugs which lead to QT prolongation, and cumulative high dose anthracycline therapy.
Cross hypersensitivity reactions have been reported in patients who received other selective 5-HT3 receptor antagonists. These reactions have not been seen with dolasetron mesylate.
Drug Interactions
The potential for clinically significant drug-drug interactions posed by dolasetron and hydrodolasetron appears to be low for drugs commonly used in chemotherapy because hydrodolasetron is eliminated by multiple routes. SeePRECAUTIONS, Generalfor information about potential interaction with other drugs that prolong the QTc interval.
When oral dolasetron (200 mg once daily) was coadministered with cimetidine (300 mg four times daily) for 7 days, the systemic exposure (i.e., AUC) of hydrodolasetron increased by 24% and the maximum plasma concentration of hydrodolasetron increased by 15%. When oral dolasetron (200 mg once daily) was coadministered with rifampin (600 mg once daily) for 7 days, the systemic exposure of hydrodolasetron decreased by 28% and the maximum plasma concentration of hydrodolasetron decreased by 17%.
Caution should be exercised when ANZEMET is coadministered with drugs, including those used in chemotherapy, that prolong ECG intervals and/or cause hypokalemia or hypomagnesemia. (seeWARNINGS).
In patients taking furosemide, nifedipine, diltiazem, ACE inhibitors, verapamil, glyburide, propranolol, and various chemotherapy agents, no effect was shown on the clearance of hydrodolasetron. Clearance of hydrodolasetron decreased by about 27% when dolasetron mesylate was administered intravenously concomitantly with atenolol. Dolasetron mesylate did not inhibit the antitumor activity of four chemotherapeutic agents (cisplatin, 5-fluorouracil, doxorubicin, cyclophosphamide) in four murine models.
Serotonin syndrome (including altered mental status, autonomic instability, and neuromuscular abnormalities) has been described following the concomitant use of 5-HT3 receptor antagonists and other serotonergic drugs, including selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs).
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 24-month carcinogenicity study, there was a statistically significant (P<0.001) increase in the incidence of combined hepatocellular adenomas and carcinomas in male mice treated with 150 mg/kg/day and above. In this study, mice (CD-1) were treated orally with dolasetron mesylate 75, 150, or 300 mg/kg/day (225, 450 or 900 mg/m2/day). For a 50 kg person of average height (1.46 m2 body surface area), these doses represent 3, 6, and 12 times the recommended clinical dose (74 mg/m2) on a body surface area basis. No increase in liver tumors was observed at a dose of 75 mg/kg/day in male mice and at doses up to 300 mg/kg/day in female mice.
In a 24-month rat (Sprague-Dawley) carcinogenicity study, oral dolasetron mesylate was not tumorigenic at doses up to 150 mg/kg/day (900 mg/m2/day, 12 times the recommended human dose based on body surface area) in male rats and 300 mg/kg/day (1800 mg/m2/day, 24 times the recommended human dose based on body surface area) in female rats.
Dolasetron mesylate was not genotoxic in the Ames test, the rat lymphocyte chromosomal aberration test, the Chinese hamster ovary (CHO) cell (HGPRT) forward mutation test, the rat hepatocyte unscheduled DNA synthesis (UDS) test or the mouse micronucleus test.
Dolasetron mesylate was found to have no effect on fertility and reproductive performance at oral doses up to 100 mg/kg/day (600 mg/m2/day, 8 times the recommended human dose based on body surface area) in female rats and up to 400 mg/kg/day (2400 mg/m2/day, 32 times the recommended human dose based on body surface area) in male rats.
Pregnancy
Teratogenic Effects
Pregnancy Category B
Teratology studies have not revealed evidence of impaired fertility or harm to the fetus due to dolasetron mesylate. These studies have been performed in pregnant rats at oral doses up to 100 mg/kg/day (8 times the recommended human dose based on body surface area) and pregnant rabbits at oral doses up to 100 mg/kg/day (16 times the recommended human dose based on body surface area). There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
It is not known whether dolasetron mesylate is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ANZEMET Tablets are administered to a nursing woman.
Pediatric Use
(SeePRECAUTIONS, General)
Safety and effectiveness in pediatric patients (2 years and older) is based on pharmacokinetic studies and efficacy data in adults. Safety and effectiveness in pediatric patients under 2 years of age have not been established.
ANZEMET Tablets are expected to be as safe and effective as when ANZEMET Injection is given orally to pediatric patients. ANZEMET Tablets are recommended for children old enough to swallow tablets (seeCLINICAL PHARMACOLOGY, Pharmacokinetics in Humans).
Geriatric Use
Elderly patients are at particular risk for prolongation of the PR, QRS, and QT interval; therefore, caution should be exercised and ECG monitoring should be performed when using ANZEMET in this population (seeWARNINGS).
In controlled clinical trials in the prevention of chemotherapy-induced nausea and vomiting, 301 (29%) of 1026 patients were 65 years of age or older. Of the 301 geriatric patients in the trial, 282 received oral ANZEMET Tablets. No overall differences in safety or effectiveness were observed between geriatric and younger patients, and other reported clinical experience has not identified differences in responses between geriatric and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
The pharmacokinetics, including clearance of oral ANZEMET Tablets, in elderly and younger patients are similar (seeCLINICAL PHARMACOLOGY, Pharmacokinetics in Humans). Dosage adjustment is not needed in patients over the age of 65.
Adverse Reactions
In controlled clinical trials, 943 adult cancer patients received ANZEMET Tablets. These patients were receiving concurrent chemotherapy, predominantly cyclophosphamide and doxorubicin regimens. The following adverse events were reported in ≥2% of patients receiving either ANZEMET 25 mg or ANZEMET 100 mg tablets for prevention of cancer chemotherapy induced nausea and vomiting in controlled clinical trials (Table 3).
Table 3. Adverse Events ≥2% from Chemotherapy-Induced Nausea and Vomiting Studies Event ANZEMET 25 mg(N=235) 100 mg(N=227) Headache 42 (17.9%) 52 (22.9%) Fatigue 6 (2.6%) 13 (5.7%) Diarrhea 5 (2.1%) 12 (5.3%) Bradycardia 12 (5.1%) 9 (4.0%) Dizziness 3 (1.3%) 7 (3.1%) Pain 0 7 (3.1%) Tachycardia 7 (3.0%) 6 (2.6%) Dyspepsia 7 (3.0%) 5 (2.2%) Chills/Shivering 3 (1.3%) 5 (2.2%)
In clinical trials, the following reported adverse events, assessed by investigators as treatment-related or causality unknown, occurred following oral or intravenous administration of ANZEMET in < 2% of adult patients receiving concomitant cancer chemotherapy:
Cardiovascular: Hypotension; edema, peripheral edema. The following events also occurred and with a similar frequency as placebo and/or active comparator: Mobitz I AV block, chest pain, orthostatic hypotension, myocardial ischemia, syncope, severe bradycardia, and palpitations. SeePRECAUTIONSsection for information on potential effects on ECG.
In addition, the following asymptomatic treatment-emergent ECG changes were seen at rates less than or equal to those for active or placebo controls: bradycardia, T wave change, ST-T wave change, sinus arrhythmia, extrasystole (APCs or VPCs), poor R-wave progression, bundle branch block (left and right), nodal arrhythmia, U wave change, atrial flutter/fibrillation.
Furthermore, severe hypotension, bradycardia and syncope have been reported immediately or closely following IV administration.
Dermatologic: Rash, increased sweating.
Gastrointestinal System: Constipation, dyspepsia, abdominal pain, anorexia; pancreatitis.
Hearing, Taste and Vision: Taste perversion, abnormal vision, tinnitus, photophobia.
Hematologic: Hematuria, epistaxis, prothrombin time prolonged, PTT increased, anemia, purpura/hematoma, thrombocytopenia.
Hypersensitivity: Anaphylactic reaction, facial edema, urticaria.
Liver and Biliary System: Transient increases in AST (SGOT) and/or ALT (SGPT) values have been reported as adverse events in less than 1% of adult patients receiving ANZEMET in clinical trials. The increases did not appear to be related to dose or duration of therapy and were not associated with symptomatic hepatic disease. Similar increases were seen with patients receiving active comparator. Hyperbilirubinemia, increased GGT.
Metabolic and Nutritional: Alkaline phosphatase increased.
Musculoskeletal: Myalgia, arthralgia.
Nervous System: Flushing, vertigo, paresthesia, tremor; ataxia, twitching.
Psychiatric: Agitation, sleep disorder, depersonalization; confusion, anxiety, abnormal dreaming.
Respiratory System: Dyspnea, bronchospasm.
Urinary System: Dysuria, polyuria, acute renal failure.
Vascular (Extracardiac): Local pain or burning on IV administration; peripheral ischemia, thrombophlebitis/phlebitis.
Postmarketing Experience There are reports of wide complex tachycardia or ventricular tachycardia and of ventricular fibrillation cardiac arrest following intravenous administration.
Overdosage
There is no known specific antidote for dolasetron mesylate, and patients with suspected overdose should be managed with supportive therapy. Individual doses as large as 5 mg/kg intravenously or 400 mg orally have been safely given to healthy volunteers or cancer patients.
Following a suspected overdose of ANZEMET Injection, a patient found to have second-degree or higher AV conduction block with ECG should undergo cardiac telemetry monitoring.
It is not known if dolasetron mesylate is removed by hemodialysis or peritoneal dialysis.
Single intravenous doses of dolasetron mesylate at 160 mg/kg in male mice and 140 mg/kg in female mice and rats of both sexes (6.3 to 12.6 times the recommended human dose based on body surface area) were lethal. Symptoms of acute toxicity were tremors, depression and convulsions.
A 59-year-old man with metastatic melanoma and no known pre-existing cardiac conditions developed severe hypotension and dizziness 40 minutes after receiving a 15 minute intravenous infusion of 1000 mg (13 mg/kg) of dolasetron mesylate. Treatment for the overdose consisted of infusion of 500 mL of a plasma expander, dopamine, and atropine. The patient had normal sinus rhythm and prolongation of PR, QRS and QTc intervals on an ECG recorded 2 hours after the infusion. The patient's blood pressure was normal 3 hours after the event and the ECG intervals returned to baseline on follow-up. The patient was released from the hospital 6 hours after the event.
Dosage And Administration
The recommended doses of ANZEMET Tablets should not be exceeded.
Adults
The recommended oral dosage of ANZEMET (dolasetron mesylate) is 100 mg given within one hour before chemotherapy.
Pediatric Patients
The recommended oral dosage in pediatric patients 2 to 16 years of age is 1.8 mg/kg given within one hour before chemotherapy, up to a maximum of 100 mg. Safety and effectiveness in pediatric patients under 2 years of age have not been established.
In children for whom the 100 mg tablet is not appropriate based on their weight or ability to swallow tablets, the ANZEMET Injection solution may be mixed into apple or apple-grape juice for oral dosing in pediatric patients. The diluted product may be kept up to 2 hours at room temperature before use. However, ANZEMET Injection solution when administered intravenously is contraindicated in adult and pediatric patients for the prevention of nausea and vomiting associated with initial and repeat courses of emetogenic cancer chemotherapy due to dose dependent QT prolongation.
Use in the Elderly, Renal Failure Patients, or Hepatically Impaired Patients
No dosage adjustment is recommended, however; ECG monitoring is recommended for elderly and renally impaired patients (seeWARNINGSandCLINICAL PHARMACOLOGY, Pharmacokinetics in Humans).
How Supplied
ANZEMET® Tablets (dolasetron mesylate) Strength Quantity NDC Number Description 50 mg 5 ct Bottle10 ct Unit Dose Pack 0088-1202-050088-1202-43 Light pink, film coated, round tablet imprinted with "A" on one side and "50"on the other. 100 mg 5 ct Bottle10 ct Unit Dose 5 ct Buler Pack 0088-1203-050088-1203-430088-1203-29 Pink, film coated, elongated oval tablet imprinted with "100" on one side and "ANZEMET" on the other. STORAGE AND HANDLING SECTION
Store at controlled room temperature 20–25°C (68–77°F). Protect from light.
Patient Counseling Information
Patients should be informed that ANZEMET may cause serious cardiac arrhythmias such as QT prolongation or heart block. Patients should be instructed to tell their health care provider right away if they perceive a change in their heart rate, if they feel lightheaded, or if they have a syncopal episode.
Patients should be informed that the chances of developing serious cardiac arrhythmias such as QT prolongation and Torsade de Pointes or heart block are higher in the following people:
- Patients with a personal or family history of abnormal heart rhythms, such as congenital long QT syndrome
- Patients with a personal history of sick sinus syndrome, atrial fibrillation with slow ventricular response or myocardial ischemia
- Patients who take medications that may prolong the PR interval, such as certain antihypertensives or medications that may prolong the QRS interval, such as antiarrythmic medications
- Patients who take medications, such as diuretics, which may cause electrolyte abnormalities
- Patients with hypokalemia or hypomagnesemia. Some types of chemotherapy cause hypokalemia and hypomagnesemia
- Elderly patients and renally impaired patients
ANZEMET should be avoided in these patients, since they may be more at risk for cardiac arrhythmias such as QT prolongation and Torsade de Pointes.
Advise patients of the possibility of serotonin syndrome with concomitant use of Anzemet and another serotonergic agent such as medications to treat depression and migraines. Advise patients to seek immediate medical attention if the following symptoms occur: changes in mental status, autonomic instability, neuromuscular symptoms with or without gastrointestinal symptoms.
Prescribing Information as of September 2014
Manufactured by: Patheon Pharmaceuticals Inc.Cincinnati, OH 45237
Manufactured for: sanofi-aventis U.S. LLCBridgewater, NJ 08807A SANOFI COMPANY
©2014 sanofi-aventis U.S. LLC
Principal Display Panel - 50mg Tablet Carton
NDC 0088-1202-43
Anzemet® Tablets
dolasetron mesylate
50mg
10 Tablets
sanofi aventis
![]()
Principal Display Panel - 100 Mg Tablet Carton
NDC 0088-1203-43
Anzemet® Tablets
dolasetron mesylate
100mg
10 Tablets
sanofi aventis
![]()
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site