CEFTIN (cefuroxime axetil 500 mg) Dailymed
Generic: cefuroxime axetil
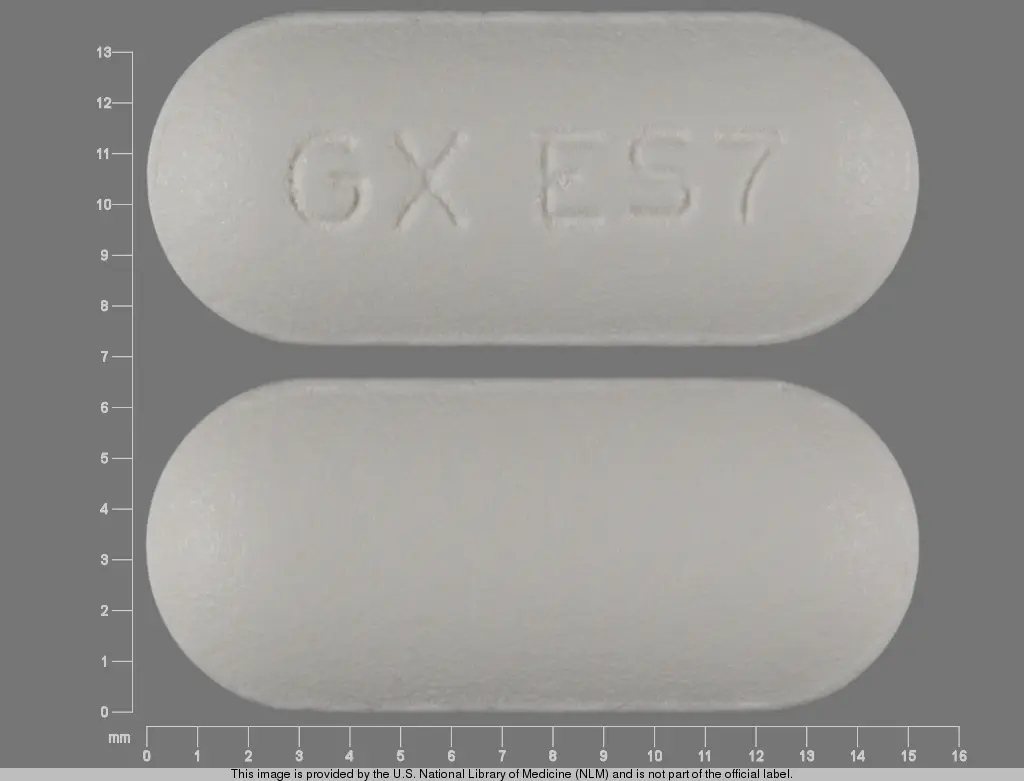
IMPRINT: GX ES7
SHAPE: oval
COLOR: white
All Imprints
cefuroxime axetil 250 mg - gx es7 oval white
cefuroxime axetil 500 mg - gx eg2 oval white
Go PRO for all pill images
1 Indications And Usage
CEFTIN is a cephalosporin antibacterial drug indicated for the treatment of the following infections due to susceptible bacteria: (1 )
- •Pharyngitis/tonsillitis (adults and pediatric patients) (
1.1 )- •Acute bacterial otitis media (pediatric patients) (
1.2 )- •Acute bacterial maxillary sinusitis (adults and pediatric patients) (
1.3 )- •Acute bacterial exacerbations of chronic bronchitis (adults and pediatric patients 13 years and older) (
1.4 )- •Uncomplicated skin and skin-structure infections (adults and pediatric patients 13 years and older) (
1.5 )- •Uncomplicated urinary tract infections (adults and pediatric patients 13 years and older) (
1.6 )- •Uncomplicated gonorrhea (adults and pediatric patients 13 years and older) (
1.7 )- •Early Lyme disease (adults and pediatric patients 13 years and older) (
1.8 )- •Impetigo (pediatric patients) (
1.9 )
To reduce the development of drug-resistant bacteria and maintain the effectiveness of CEFTIN and other antibacterial drugs, CEFTIN should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
1.1Pharyngitis/Tonsillitis
CEFTIN tablets are indicated for the treatment of adult patients and pediatric patients (13 years and older) with mild-to-moderate pharyngitis/tonsillitis caused by susceptible strains of Streptococcus pyogenes.
CEFTIN for oral suspension is indicated for the treatment of pediatric patients aged 3 months to 12 years with mild-to-moderate pharyngitis/tonsillitis caused by susceptible strains of Streptococcus pyogenes.
Limitations of Use
- •The efficacy of CEFTIN in the prevention of rheumatic fever was not established in clinical trials.
- •The efficacy of CEFTIN in the treatment of penicillin‑resistant strains of Streptococcus pyogenes has not been demonstrated in clinical trials.
1.2Acute Bacterial Otitis Media
CEFTIN tablets are indicated for the treatment of pediatric patients (who can swallow tablets whole) with acute bacterial otitis media caused by susceptible strains of Streptococcus pneumoniae, Haemophilus influenzae (including β-lactamase–producing strains), Moraxella catarrhalis (including β-lactamase–producing strains), or Streptococcus pyogenes.
CEFTIN for oral suspension is indicated for the treatment of pediatric patients aged 3 months to 12 years with acute bacterial otitis media caused by susceptible strains of Streptococcus pneumoniae, Haemophilus influenzae (including β-lactamase–producing strains), Moraxella catarrhalis (including β-lactamase–producing strains), or Streptococcus pyogenes.
1.3Acute Bacterial Maxillary Sinusitis
CEFTIN tablets are indicated for the treatment of adult and pediatric patients (13 years and older) with mild-to-moderate acute bacterial maxillary sinusitis caused by susceptible strains of Streptococcus pneumoniae or Haemophilus influenzae (non-β‑lactamase–producing strains only).
CEFTIN for oral suspension is indicated for the treatment of pediatric patients aged 3 months to 12 years with mild-to-moderate acute bacterial maxillary sinusitis caused by susceptible strains of Streptococcus pneumoniae or Haemophilus influenzae (non-β‑lactamase–producing strains only).
Limitations of Use
The effectiveness of CEFTIN for sinus infections caused by β-lactamase–producing Haemophilus influenzae or Moraxella catarrhalis in patients with acute bacterial maxillary sinusitis was not established due to insufficient numbers of these isolates in the clinical trials [see Clinical Studies (14.1)].
1.4Acute Bacterial Exacerbations of Chronic Bronchitis
CEFTIN tablets are indicated for the treatment of adult patients and pediatric patients (aged 13 and older) with mild-to-moderate acute bacterial exacerbations of chronic bronchitis caused by susceptible strains of Streptococcus pneumoniae, Haemophilus influenzae (β‑lactamase–negative strains), or Haemophilus parainfluenzae (β‑lactamase–negative strains).
1.5Uncomplicated Skin and Skin Structure Infections
CEFTIN tablets are indicated for the treatment of adult patients and pediatric patients (aged 13 and older) with uncomplicated skin and skin-structure infections caused by susceptible strains of Staphylococcus aureus (including β-lactamase–producing strains) or Streptococcus pyogenes.
1.6Uncomplicated Urinary Tract Infections
CEFTIN tablets are indicated for the treatment of adult patients and pediatric patients (aged 13 and older) with uncomplicated urinary tract infections caused by susceptible strains of Escherichia coli or Klebsiella pneumoniae.
1.7Uncomplicated Gonorrhea
CEFTIN tablets are indicated for the treatment of adult patients and pediatric patients (aged 13 and older) with uncomplicated gonorrhea, urethral and endocervical, caused by penicillinase-producing and non‑penicillinase–producing susceptible strains of Neisseria gonorrhoeae and uncomplicated gonorrhea, rectal, in females, caused by non‑penicillinase–producing susceptible strains of Neisseria gonorrhoeae.
1.8Early Lyme Disease (erythema migrans)
CEFTIN tablets are indicated for the treatment of adult patients and pediatric patients (aged 13 and older) with early Lyme disease (erythema migrans) caused by susceptible strains of Borrelia burgdorferi.
1.9Impetigo
CEFTIN for oral suspension is indicated for the treatment of pediatric patients aged 3 months to 12 years with impetigo caused by susceptible strains of Staphylococcus aureus (including β-lactamase–producing strains) or Streptococcus pyogenes.
1.10Usage
To reduce the development of drug‑resistant bacteria and maintain the effectiveness of CEFTIN and other antibacterial drugs, CEFTIN should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
2 Dosage And Administration
- •Tablets and oral suspension are not bioequivalent and are therefore not substitutable on a milligram-per-milligram basis. (
2.1 )- •Administer tablets with or without food. (
2.2 )- •Administer oral suspension with food. (
2.3 )- •Administer CEFTIN tablets or CEFTIN for oral suspension as described in the dosage guidelines. (
2.2 ,2.3 ,2.4 )- •Dosage adjustment is required for patients with impaired renal function. (
2.5 )
Adult Patients and Pediatric Patients Dosage Guidelines for CEFTIN Tablets
Infection
Dosage
Duration
(Days)
Adults and Adolescents (13 years and older)
Pharyngitis/tonsillitis (mild to moderate)
250 mg
every 12 hours
10
Acute bacterial maxillary sinusitis (mild to moderate)
250 mg
every 12 hours
10
Acute bacterial exacerbations of chronic bronchitis (mild to moderate)
250 or 500 mg
every 12 hours
10
Uncomplicated skin and skin-structure infections
250 or 500 mg
every 12 hours
10
Uncomplicated urinary tract infections
250 mg every 12 hours
7 to 10
Uncomplicated gonorrhea
1,000 mg
single dose
Early Lyme disease
500 mg
every 12 hours
20
Pediatric Patients younger than 13 years (who can swallow tablets whole)
Acute bacterial otitis media
250 mg
every 12 hours
10
Acute bacterial maxillary sinusitis
250 mg
every 12 hours
10
a Total daily dose given twice daily divided in equal doses.
Pediatric Patients (3 Months to 12 Years) Dosage Guidelines for CEFTIN for Oral Suspension
Infection
Recommended
Daily
Dosea
Maximum
Daily
Dose
Duration
(Days)
Pharyngitis/tonsillitis
20 mg/kg
500 mg
10
Acute bacterial otitis media
30 mg/kg
1,000 mg
10
Acute bacterial maxillary sinusitis (mild to moderate)
30 mg/kg
1,000 mg
10
Impetigo
30 mg/kg
1,000 mg
10
2.1Important Administration Instructions
- •CEFTIN tablets and CEFTIN for oral suspension are not bioequivalent and are therefore not substitutable on a milligram-per-milligram basis [see Clinical Pharmacology (12.3)].
- •Administer CEFTIN tablets or oral suspension as described in the appropriate dosage guidelines [see Dosage and Administration (2.2, 2.3, 2.4)].
- •Administer CEFTIN tablets with or without food.
- •Administer CEFTIN for oral suspension with food.
- •Pediatric patients (aged 13 years and older) who cannot swallow the CEFTIN tablets whole should receive CEFTIN for oral suspension because the tablet has a strong, persistent bitter taste when crushed [see Dosage and Administration (2.2)].
2.2Dosage for CEFTIN Tablets
Administer CEFTIN tablets as described in the dosage guidelines table below with or without food.
Table 1. Adult Patients and Pediatric Patients Dosage Guidelines for CEFTIN Tablets a The safety and effectiveness of CEFTIN administered for less than 10 days in patients with acute exacerbations of chronic bronchitis have not been established. b When crushed, the tablet has a strong, persistent bitter taste. Therefore, patients who cannot swallow the tablet whole should receive the oral suspension.
Infection
Dosage
Duration
(Days)
Adults and Adolescents (13 years and older)
Pharyngitis/tonsillitis (mild to moderate)
250 mg every 12 hours
10
Acute bacterial maxillary sinusitis (mild to moderate)
250 mg every 12 hours
10
Acute bacterial exacerbations of chronic bronchitis (mild to moderate)
250 or 500 mg every 12 hours
10a
Uncomplicated skin and skin-structure infections
250 or 500 mg every 12 hours
10
Uncomplicated urinary tract infections
250 mg every 12 hours
7 to 10
Uncomplicated gonorrhea
1,000 mg
single dose
Early Lyme disease
500 mg every 12 hours
20
Pediatric Patients younger than 13 years (who can swallow tablets whole)b
Acute bacterial otitis media
250 mg every 12 hours
10
Acute bacterial maxillary sinusitis
250 mg every 12 hours
10
2.3Dosage for CEFTIN for Oral Suspension
Administer CEFTIN for oral suspension as described in the dosage guidelines table below with food.
Table 2. Pediatric Patients (3 Months to 12 Years) Dosage Guidelines for CEFTIN for Oral Suspension a Recommended daily dose given twice daily divided in equal doses.
Infection
Recommended
Daily Dosea
Maximum Daily Dose
Duration (Days)
Pharyngitis/tonsillitis
20 mg/kg
500 mg
10
Acute bacterial otitis media
30 mg/kg
1,000 mg
10
Acute bacterial maxillary sinusitis
30 mg/kg
1,000 mg
10
Impetigo
30 mg/kg
1,000 mg
10
2.4Preparation and Administration of CEFTIN for Oral Suspension
Prepare a suspension at the time of dispensing as follows:
- 1.Shake the bottle to loosen the powder.
- 2.Remove the cap.
- 3.Add the total amount of cold water for reconstitution (Table 3) and replace the cap.
- 4.Invert the bottle and vigorously rock the bottle from side to side so that water rises through the powder.
- 5.Once the sound of the powder against the bottle disappears, turn the bottle upright and vigorously shake it in a diagonal direction for at least one minute.
- 6.After reconstitution, wait one hour before administering suspension to a patient.
Table 3. Amount of Water Required for Reconstitution of Labeled Volumes of CEFTIN for Oral Suspension
Oral Suspension
Amount of Water Required for Reconstitution
Labeled Volume after Reconstitution
125 mg/5 mL
37 mL
100 mL
250 mg/5 mL
19 mL
50 mL
35 mL
100 mL
- •Shake the oral suspension well before each use.
- •Replace cap securely after each opening.
- •Store the reconstituted suspension refrigerated between 2° and 8°C (36° and 46°F).
- •Discard the reconstituted suspension after 10 days.
2.5Dosage in Patients with Impaired Renal Function
A dosage interval adjustment is required for patients whose creatinine clearance is less than 30 mL/min, as uled in Table 4 below, because cefuroxime is eliminated primarily by the kidney [see Clinical Pharmacology (12.3)].
Table 4. Dosing in Adults with Renal Impairment
Creatinine Clearance (mL/min)
Recommended Dosage
≥30
No dosage adjustment
10 to ˂30
Standard individual dose given every 24 hours
˂10 (without hemodialysis)
Standard individual dose given every 48 hours
Hemodialysis
A single additional standard dose should be given at the end of each dialysis
3 Dosage Forms And Strengths
CEFTIN tablets are white, capsule‑shaped, film‑coated tablets available in the following strengths:
- •250 mg of cefuroxime (as cefuroxime axetil) with "GX ES7" engraved on one side and blank on the other side.
- •500 mg of cefuroxime (as cefuroxime axetil) with "GX EG2" engraved on one side and blank on the other side.
CEFTIN for oral suspension is provided as dry, white to off‑white, tutti‑frutti–flavored powder. When reconstituted as directed, the suspension provides the equivalent of 125 mg or 250 mg of cefuroxime (as cefuroxime axetil) per 5 mL.
- •Tablets: 250 mg and 500 mg (
3 )- •For oral suspension: 125 mg/5 mL and 250 mg/5 mL (
3 )
4 Contraindications
CEFTIN is contraindicated in patients with a known hypersensitivity (e.g., anaphylaxis) to CEFTIN or to other β-lactam antibacterial drugs (e.g., penicillins and cephalosporins).
Known hypersensitivity (e.g., anaphylaxis) to CEFTIN or to other β‑lactams (e.g., penicillins and cephalosporins). (4 )
5 Warnings And Precautions
- •Serious hypersensitivity (anaphylactic) reactions: In the event of a serious reaction, discontinue CEFTIN and institute appropriate therapy. (
5.1 )- • Clostridioides difficile-associated diarrhea (CDAD): If diarrhea occurs, evaluate patients for CDAD. (
5.2 )5.1Anaphylactic Reactions
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients on β-lactam antibacterials, including CEFTIN [see Adverse Reactions (6.2)]. These reactions are more likely to occur in individuals with a history of β-lactam hypersensitivity and/or a history of sensitivity to multiple allergens. There have been reports of individuals with a history of penicillin hypersensitivity who have experienced severe reactions when treated with cephalosporins. CEFTIN is contraindicated in patients with a known hypersensitivity to CEFTIN or other β-lactam antibacterial drugs [see Contraindications (4)]. Before initiating therapy with CEFTIN, inquire about previous hypersensitivity reactions to penicillins, cephalosporins, or other allergens. If an allergic reaction occurs, discontinue CEFTIN and institute appropriate therapy.
5.2-Associated Diarrhea
Clostridioides difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including CEFTIN, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over 2 months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.3Potential for Microbial Overgrowth
The possibility of superinfections with fungal or bacterial pathogens should be considered during therapy.
5.4Development of Drug-Resistant Bacteria
Prescribing CEFTIN either in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug‑resistant bacteria.
5.5Phenylketonuria
CEFTIN for oral suspension 125 mg/5 mL contains phenylalanine 11.8 mg per 5 mL (1 teaspoonful) of reconstituted suspension. CEFTIN for oral suspension 250 mg/5 mL contains phenylalanine 25.2 mg per 5 mL (1 teaspoonful) of reconstituted suspension.
5.6Interference with Glucose Tests
A false-positive result for glucose in the urine may occur with copper reduction tests, and a false-negative result for blood/plasma glucose may occur with ferricyanide tests in subjects receiving CEFTIN [see Drug Interactions (7.3)].
6 Adverse Reactions
The following serious and otherwise important adverse reaction is described in greater detail in the Warnings and Precautions section of the label:
Anaphylactic Reactions [see Warnings and Precautions (5.1)].
The most common adverse reactions (≥3%) for CEFTIN tablets are diarrhea, nausea/vomiting, Jarisch‑Herxheimer reaction, and vaginitis (early Lyme disease). (6.1 )
The most common adverse reactions (≥2%) for CEFTIN for oral suspension are diarrhea, dislike of taste, diaper rash, and nausea/vomiting. (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch.
6.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Tablets
Multiple‑Dose Dosing Regimens with 7 to 10 Days’ Duration: In multiple-dose clinical trials, 912 subjects were treated with CEFTIN (125 to 500 mg twice daily). It is noted that 125 mg twice daily is not an approved dosage. Twenty (2.2%) subjects discontinued medication due to adverse reactions. Seventeen (85%) of the 20 subjects who discontinued therapy did so because of gastrointestinal disturbances, including diarrhea, nausea, vomiting, and abdominal pain. The percentage of subjects treated with CEFTIN who discontinued study drug because of adverse reactions was similar at daily doses of 1,000, 500, and 250 mg (2.3%, 2.1%, and 2.2%, respectively). However, the incidence of gastrointestinal adverse reactions increased with the higher recommended doses.
The adverse reactions in Table 5 are for subjects (n = 912) treated with CEFTIN in multiple‑dose clinical trials.
Table 5. Adverse Reactions (≥1%) after Multiple-Dose Regimens with CEFTIN Tablets
Adverse Reaction
CEFTIN
(n = 912)
Blood and lymphatic system disorders
Eosinophilia
1%
Gastrointestinal disorders
Diarrhea
4%
Nausea/Vomiting
3%
Investigations
Transient elevation in AST
2%
Transient elevation in ALT
2%
Transient elevation in LDH
1%
The following adverse reactions occurred in less than 1% but greater than 0.1% of subjects (n = 912) treated with CEFTIN in multiple-dose clinical trials.
- Immune System Disorders: Hives, swollen tongue.
- Metabolism and Nutrition Disorders: Anorexia.
- Nervous System Disorders: Headache.
- Cardiac Disorders: Chest pain.
- Respiratory Disorders: Shortness of breath.
- Gastrointestinal Disorders: Abdominal pain, abdominal cramps, flatulence, indigestion, mouth ulcers.
- Skin and Subcutaneous Tissue Disorders: Rash, itch.
- Renal and Urinary Disorders: Dysuria.
- Reproductive System and Breast Disorders: Vaginitis, vulvar itch.
- General Disorders and Administration Site Conditions: Chills, sleepiness, thirst.
- Investigations: Positive Coombs’ test.
Early Lyme Disease with 20-Day Regimen: Two multicenter trials assessed CEFTIN 500 mg twice daily for 20 days. The most common drug‑related adverse experiences were diarrhea (10.6%), Jarisch‑Herxheimer reaction (5.6%), and vaginitis (5.4%). Other adverse experiences occurred with frequencies comparable to those reported with 7 to 10 days’ dosing.
Single‑Dose Regimen for Uncomplicated Gonorrhea: In clinical trials using a single 1,000-mg dose of CEFTIN, 1,061 subjects were treated for uncomplicated gonorrhea.
The adverse reactions in Table 6 were for subjects treated with a single dose of 1,000 mg CEFTIN in U.S. clinical trials.
Table 6. Adverse Reactions (≥1%) after Single-Dose Regimen with 1,000-mg CEFTIN Tablets for Uncomplicated Gonorrhea
Adverse Reaction
CEFTIN
(n = 1,061)
Gastrointestinal disorders
Nausea/Vomiting
7%
Diarrhea
4%
The following adverse reactions occurred in less than 1% but greater than 0.1% of subjects (n = 1,061) treated with a single dose of CEFTIN 1,000 mg for uncomplicated gonorrhea in U.S. clinical trials.
- Infections and Infestations: Vaginal candidiasis.
- Nervous System Disorders: Headache, dizziness, somnolence.
- Cardiac Disorders: Tightness/pain in chest, tachycardia.
- Gastrointestinal Disorders: Abdominal pain, dyspepsia.
- Skin and Subcutaneous Tissue Disorders: Erythema, rash, pruritus.
- Musculoskeletal and Connective Tissue Disorders: Muscle cramps, muscle stiffness, muscle spasm of neck, lockjaw-type reaction.
- Renal and Urinary Disorders: Bleeding/pain in urethra, kidney pain.
- Reproductive System and Breast Disorders: Vaginal itch, vaginal discharge.
Oral Suspension
In clinical trials using multiple doses of CEFTIN, pediatric subjects (96.7% were younger than 12 years) were treated with CEFTIN (20 to 30 mg/kg/day divided twice daily up to a maximum dose of 500 or 1,000 mg/day, respectively). Eleven (1.2%) U.S. subjects discontinued medication due to adverse reactions. The discontinuations were primarily for gastrointestinal disturbances, usually diarrhea or vomiting. Thirteen (1.4%) U.S. pediatric subjects discontinued therapy due to the taste and/or problems with drug administration.
The adverse reactions in Table 7 are for U.S. subjects (n = 931) treated with CEFTIN in multiple‑dose clinical trials.
Table 7. Adverse Reactions (≥1%) after Multiple-Dose Regimens with CEFTIN for Oral Suspension
Adverse Reaction
CEFTIN
(n = 931)
Gastrointestinal disorders
Diarrhea
9%
Dislike of taste
5%
Nausea/vomiting
3%
Skin and subcutaneous tissue disorders
Diaper rash
3%
The following adverse reactions occurred in less than 1% but greater than 0.1% of U.S. subjects (n = 931) treated with CEFTIN for oral suspension in multiple‑dose clinical trials.
Infections and Infestations: Gastrointestinal infection, candidiasis, viral illness, upper respiratory infection, sinusitis, urinary tract infection.
Blood and Lymphatic System Disorders: Eosinophilia.
Psychiatric Disorders: Hyperactivity, irritable behavior.
Gastrointestinal Disorders: Abdominal pain, flatulence, ptyalism.
Skin and Subcutaneous Tissue Disorders: Rash.
Musculoskeletal and Connective Tissue Disorders: Joint swelling, arthralgia.
Reproductive System and Breast Disorders: Vaginal irritation.
General Disorders and Administration Site Conditions: Cough, fever.
Investigations: Elevated liver enzymes, positive Coombs’ test.
6.2Postmarketing Experience
The following adverse reactions have been identified during post-approval use of CEFTIN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System Disorders
Hemolytic anemia, leukopenia, pancytopenia, thrombocytopenia.
Gastrointestinal Disorders
Pseudomembranous colitis [see Warnings and Precautions (5.2)].
Hepatobiliary Disorders
Hepatic impairment including hepatitis and cholestasis, jaundice.
Immune System Disorders
Anaphylaxis, serum sickness‑like reaction, acute myocardial ischemia with or without myocardial infarction may occur as part of an allergic reaction.
Investigations
Increased prothrombin time.
Nervous System Disorders
Seizure, encephalopathy.
Renal and Urinary Disorders
Renal dysfunction.
Skin and Subcutaneous Tissue Disorders
Angioedema, erythema multiforme, Stevens‑Johnson syndrome, toxic epidermal necrolysis, urticaria.
7 Drug Interactions
- •Drugs that reduce gastric acidity may lower the bioavailability of CEFTIN. (
7.1 )- •Coadministration with probenecid increases systemic exposure to CEFTIN and is therefore not recommended. (
7.2 )7.1Drugs that Reduce Gastric Acidity
Drugs that reduce gastric acidity may result in a lower bioavailability of CEFTIN compared with administration in the fasting state. Administration of drugs that reduce gastric acidity may negate the food effect of increased absorption of CEFTIN when administered in the postprandial state. Administer CEFTIN at least 1 hour before or 2 hours after administration of short-acting antacids. Histamine-2 (H2) antagonists and proton pump inhibitors should be avoided.
7.2Probenecid
Concomitant administration of probenecid with cefuroxime axetil tablets increases serum concentrations of cefuroxime [see Clinical Pharmacology (12.3)]. Coadministration of probenecid with cefuroxime axetil is not recommended.
7.3Drug/Laboratory Test Interactions
A false‑positive reaction for glucose in the urine may occur with copper reduction tests (e.g., Benedict's or Fehling's solution), but not with enzyme‑based tests for glycosuria. As a false‑negative result may occur in the ferricyanide test, it is recommended that either the glucose oxidase or hexokinase method be used to determine blood/plasma glucose levels in patients receiving cefuroxime axetil. The presence of cefuroxime does not interfere with the assay of serum and urine creatinine by the alkaline picrate method.
8 Use In Specific Populations
8.1Pregnancy
Risk Summary
Available data from published epidemiologic studies, case series, and case reports over several decades with cephalosporin use, including CEFTIN, in pregnant women have not established drug-associated risks of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data).
In studies in pregnant mice and rats administered oral cefuroxime axetil during organogenesis at 14 and 9 times the maximum recommended human dose (MRHD) based on body surface area, respectively, there were no adverse developmental outcomes (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated populations are unknown. All pregnancies have a background risk of birth defects, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk: Maternal gonorrhea may be associated with preterm birth, low neonatal birth weight, chorioamnionitis, intrauterine growth restriction, small for gestational age, and premature rupture of membranes. Perinatal transmission of gonorrhea to the offspring can result in infant blindness, joint infections, and bloodstream infections.
Data
Human Data: While available studies cannot definitively establish the absence of risk, published data from epidemiologic studies, case series, and case reports over several decades have not identified an association with cephalosporin use (including CEFTIN) during pregnancy and major birth defects, miscarriage, or other adverse maternal or fetal outcomes. Available studies have methodologic limitations, including small sample size, retrospective data collection, and inconsistent comparator groups.
Animal Data: Studies performed with oral cefuroxime axetil administered to pregnant mice during organogenesis (Gestation Days 7 through 16) at doses up to 3,200 mg/kg/day (14 times the MRHD based on body surface area); and in rats dosed during organogenesis and lactation (Gestation Days 7 through 16 and Gestation Days 17 through Lactation Day 21, respectively) at doses up to 1,000 mg/kg/day (9 times the MRHD based on body surface area) have revealed no adverse developmental outcomes.
8.2 Lactation
Risk Summary
Based on several published case reports describing multiple lactating women who received cefuroxime via intravenous, intramuscular, and oral routes, cefuroxime is present in human milk. The highest maternal milk concentration described occurred in lactating women 8 hours after an intramuscular administration of cefuroxime 750 mg. Allowing for an infant milk consumption of 150 mL/kg/day, the estimated breastfed infant dose would be less than 1% of the adult dose. No data are available on the effects of the drug on the breastfed infant or the effects of the drug on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for cefuroxime and any potential adverse effects on the breastfed infant from cefuroxime or from the underlying maternal condition.
8.4Pediatric Use
The safety and effectiveness of CEFTIN have been established for pediatric patients aged 3 months to 12 years for acute bacterial maxillary sinusitis based upon its approval in adults. Use of CEFTIN in pediatric patients is supported by pharmacokinetic and safety data in adults and pediatric patients, and by clinical and microbiological data from adequate and well‑controlled trials of the treatment of acute bacterial maxillary sinusitis in adults and of acute otitis media with effusion in pediatric patients. It is also supported by postmarketing adverse events surveillance. [See Indications and Usage (1), Dosage and Administration (2), Adverse Reactions (6), Clinical Pharmacology (12.3).]
8.5Geriatric Use
Of the total number of subjects who received CEFTIN in 20 clinical trials, 375 were aged 65 and older while 151 were aged 75 and older. No overall differences in safety or effectiveness were observed between these subjects and younger adult subjects. Reported clinical experience has not identified differences in responses between the elderly and younger adult patients, but greater sensitivity of some older individuals cannot be ruled out.
Cefuroxime is substantially excreted by the kidney, and the risk of adverse reactions may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6Renal Impairment
Reducing the dosage of CEFTIN is recommended for adult patients with severe renal impairment (creatinine clearance <30 mL/min) [see Dosage and Administration (2.5), Clinical Pharmacology (12.3)].
10 Overdosage
Overdosage of cephalosporins can cause cerebral irritation leading to convulsions or encephalopathy. Serum levels of cefuroxime can be reduced by hemodialysis and peritoneal dialysis.
11 Description
CEFTIN tablets and CEFTIN for oral suspension contain cefuroxime as cefuroxime axetil. CEFTIN is a semisynthetic, cephalosporin antibacterial drug for oral administration.
The chemical name of cefuroxime axetil (1‑(acetyloxy) ethyl ester of cefuroxime) is (RS)-1-hydroxyethyl (6R,7R)-7-[2-(2-furyl)glyoxyl-amido]-3-(hydroxymethyl)-8-oxo-5-thia-1-azabicyclo[4.2.0]-oct-2-ene-2-carboxylate, 72-(Z)-(O-methyl-oxime), 1-acetate 3-carbamate. Its molecular formula is C20H22N4O10S, and it has a molecular weight of 510.48.
Cefuroxime axetil is in the amorphous form and has the following structural formula:
![]()
Tablets are film‑coated and contain the equivalent of 250 or 500 mg of cefuroxime as cefuroxime axetil. Tablets contain the inactive ingredients colloidal silicon dioxide, croscarmellose sodium, hydrogenated vegetable oil, hypromellose, methylparaben, microcrystalline cellulose, propylene glycol, propylparaben, sodium benzoate, sodium lauryl sulfate, and titanium dioxide.
Oral suspension, when reconstituted with water, provides the equivalent of 125 mg or 250 mg of cefuroxime (as cefuroxime axetil) per 5 mL. Oral suspension contains the inactive ingredients acesulfame potassium, aspartame, povidone K30, stearic acid, sucrose, tutti‑frutti flavoring, and xanthan gum.
12 Clinical Pharmacology
12.1Mechanism of Action
CEFTIN is an antibacterial drug [see Microbiology (12.4)].
12.3Pharmacokinetics
Absorption
After oral administration, cefuroxime axetil is absorbed from the gastrointestinal tract and rapidly hydrolyzed by nonspecific esterases in the intestinal mucosa and blood to cefuroxime. Serum pharmacokinetic parameters for cefuroxime following administration of CEFTIN tablets to adults are shown in Table 8.
Table 8. Pharmacokinetics of Cefuroxime Administered in the Postprandial State as CEFTIN Tablets to Adultsa a Mean values of 12 healthy adult volunteers. b Drug administered immediately after a meal.
Doseb
(Cefuroxime
Equivalent)
Peak Plasma Concentration
(mcg/mL)
Time of Peak Plasma Concentration
(h)
Mean
Elimination
Half‑life (h)
AUC
(mcg•h/mL)
125 mg
2.1
2.2
1.2
6.7
250 mg
4.1
2.5
1.2
12.9
500 mg
7.0
3.0
1.2
27.4
1,000 mg
13.6
2.5
1.3
50.0
Effect of Food: Absorption of the tablet is greater when taken after food (absolute bioavailability increases from 37% to 52%). Despite this difference in absorption, the clinical and bacteriologic responses of subjects were independent of food intake at the time of tablet administration in 2 trials where this was assessed.
All pharmacokinetic and clinical effectiveness and safety trials in pediatric subjects using the suspension formulation were conducted in the fed state. No data are available on the absorption kinetics of the suspension formulation when administered to fasted pediatric subjects.
Lack of Bioequivalence: Oral suspension was not bioequivalent to tablets when tested in healthy adults. The tablet and oral suspension formulations are NOT substitutable on a milligram-per-milligram basis. The area under the curve for the suspension averaged 91% of that for the tablet, and the peak plasma concentration for the suspension averaged 71% of the peak plasma concentration of the tablets. Therefore, the safety and effectiveness of both the tablet and oral suspension formulations were established in separate clinical trials.
Distribution
Cefuroxime is distributed throughout the extracellular fluids. Approximately 50% of serum cefuroxime is bound to protein.
Metabolism
The axetil moiety is metabolized to acetaldehyde and acetic acid.
Excretion
Cefuroxime is excreted unchanged in the urine; in adults, approximately 50% of the administered dose is recovered in the urine within 12 hours. The pharmacokinetics of cefuroxime in pediatric subjects have not been studied. Until further data are available, the renal elimination of cefuroxime axetil established in adults should not be extrapolated to pediatric subjects.
Specific Populations
Patients with Renal Impairment: In a trial of 28 adults with normal renal function or severe renal impairment (creatinine clearance <30 mL/min), the elimination half-life was prolonged in relation to severity of renal impairment. Prolongation of the dosage interval is recommended in adult patients with creatinine clearance <30 mL/min [see Dosage and Administration (2.5)].
Pediatric Patients: Serum pharmacokinetic parameters for cefuroxime in pediatric subjects administered CEFTIN for oral suspension are shown in Table 9.
Table 9. Pharmacokinetics of Cefuroxime Administered in the Postprandial State as CEFTIN for Oral Suspension to Pediatric Subjectsa a Mean age = 23 months. b Drug administered with milk or milk products.
Doseb
(Cefuroxime Equivalent)
n
Peak Plasma
Concentration
(mcg/mL)
Time of Peak
Plasma
Concentration (h)
Mean
Elimination
Half‑life
(h)
AUC
(mcg•h/mL)
10 mg/kg
8
3.3
3.6
1.4
12.4
15 mg/kg
12
5.1
2.7
1.9
22.5
20 mg/kg
8
7.0
3.1
1.9
32.8
Geriatric Patients: In a trial of 20 elderly subjects (mean age = 83.9 years) having a mean creatinine clearance of 34.9 mL/min, the mean serum elimination half‑life was prolonged to 3.5 hours; however, despite the lower elimination of cefuroxime in geriatric patients, dosage adjustment based on age is not necessary [see Use in Specific Populations (8.5)].
Drug Interaction Studies
Concomitant administration of probenecid with cefuroxime axetil tablets increases the cefuroxime area under the serum concentration versus time curve and maximum serum concentration by 50% and 21%, respectively [see Drug Interactions (7.2)].
12.4Microbiology
Mechanism of Action
Cefuroxime axetil is a bactericidal agent that acts by inhibition of bacterial cell wall synthesis. Cefuroxime axetil has activity in the presence of some β-lactamases, both penicillinases and cephalosporinases, of gram-negative and gram-positive bacteria.
Resistance
Resistance to cefuroxime axetil is primarily through hydrolysis by β-lactamase, alteration of penicillin-binding proteins (PBPs), decreased permeability, and the presence of bacterial efflux pumps.
Susceptibility to cefuroxime axetil will vary with geography and time; local susceptibility data should be consulted, if available. Beta-lactamase‑negative, ampicillin-resistant (BLNAR) isolates of H. influenzae should be considered resistant to cefuroxime axetil.
Antimicrobial Activity
Cefuroxime axetil has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections [see Indications and Usage (1)]:
Aerobic Bacteria:
Gram‑positive bacteria
- • Staphylococcus aureus (methicillin-susceptible isolates only)
- • Streptococcus pneumoniae
- • Streptococcus pyogenes
Gram‑negative bacteria
- • Escherichia coli a
- • Klebsiella pneumoniae a
- • Haemophilus influenzae
- • Haemophilus parainfluenzae
- • Moraxella catarrhalis
- • Neisseria gonorrhoeae
a Most extended spectrum β-lactamase (ESBL)‑producing and carbapenemase-producing isolates are resistant to cefuroxime axetil.
Spirochetes
- • Borrelia burgdorferi
The following in vitro data are available, but their clinical significance is unknown. At least 90 percent of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for cefuroxime against isolates of similar genus or organism group. However, the efficacy of cefuroxime axetil in treating clinical infections caused by these bacteria has not been established in adequate and well-controlled clinical trials.
Aerobic Bacteria:
Gram-positive bacteria
- • Staphylococcus epidermidis (methicillin-susceptible isolates only)
- • Staphylococcus saprophyticus (methicillin-susceptible isolates only)
- • Streptococcus agalactiae
Gram-negative bacteria
- • Morganella morganii
- • Proteus inconstans
- • Proteus mirabilis
- • Providencia rettgeri
Anaerobic Bacteria:
Gram-positive bacteria
- • Peptococcus niger
Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
13 Nonclinical Toxicology
13.1Carcinogenesis, Mutagenesis, Impairment of Fertility
Although lifetime studies in animals have not been performed to evaluate carcinogenic potential, no mutagenic activity was found for cefuroxime axetil in a battery of bacterial mutation tests. Positive results were obtained in an in vitro chromosome aberration assay; however, negative results were found in an in vivo micronucleus test at doses up to 1.5 g/kg. Fertility studies in rats (males dosed for 70 days prior to and through mating; females dosed 21 days prior to mating through lactation) at doses up to 1,000 mg/kg/day (9 times the MRHD based on body surface area) have revealed no adverse effects on fertility.
14 Clinical Studies
14.1Acute Bacterial Maxillary Sinusitis
One adequate and well‑controlled trial was performed in subjects with acute bacterial maxillary sinusitis. In this trial, each subject had a maxillary sinus aspirate collected by sinus puncture before treatment was initiated for presumptive acute bacterial sinusitis. All subjects had radiographic and clinical evidence of acute maxillary sinusitis. In the trial, the clinical effectiveness of CEFTIN in treating acute maxillary sinusitis was comparable to an oral antimicrobial agent containing a specific β‑lactamase inhibitor. However, microbiology data demonstrated CEFTIN to be effective in treating acute bacterial maxillary sinusitis due only to Streptococcus pneumoniae or non-β‑lactamase–producing Haemophilus influenzae. Insufficient numbers of β-lactamase–producing Haemophilus influenzae and Moraxella catarrhalis isolates were obtained in this trial to adequately evaluate the effectiveness of CEFTIN in treating acute bacterial maxillary sinusitis due to these 2 organisms.
This trial randomized 317 adult subjects, 132 subjects in the U. S. and 185 subjects in South America. Table 10 shows the results of the intent‑to‑treat analysis.
Table 10. Clinical Effectiveness of CEFTIN Tablets in the Treatment of Acute Bacterial Maxillary Sinusitis a 95% confidence interval around the success difference [‑0.08, +0.32]. b 95% confidence interval around the success difference [‑0.10, +0.16]. c Control was an antibacterial drug containing a β-lactamase inhibitor.
U.S. Subjectsa
South American Subjectsb
CEFTIN
250 mg Twice Daily
(n = 49)
Controlc
(n = 43)
CEFTIN
250 mg Twice Daily
(n = 49)
Controlc
(n = 43)
Clinical success
(cure + improvement)
65%
53%
77%
74%
Clinical cure
53%
44%
72%
64%
Clinical improvement
12%
9%
5%
10%
In this trial and in a supporting maxillary puncture trial, 15 evaluable subjects had non-β‑lactamase–producing Haemophilus influenzae as the identified pathogen. Of these, 67% (10/15) had this pathogen eradicated. Eighteen (18) evaluable subjects had Streptococcus pneumoniae as the identified pathogen. Of these, 83% (15/18) had this pathogen eradicated.
14.2Early Lyme Disease
Two adequate and well‑controlled trials were performed in subjects with early Lyme disease. All subjects presented with physician-documented erythema migrans, with or without systemic manifestations of infection. Subjects were assessed at 1 month posttreatment for success in treating early Lyme disease (Part I) and at 1 year posttreatment for success in preventing the progression to the sequelae of late Lyme disease (Part II).
A total of 355 adult subjects (181 treated with cefuroxime axetil and 174 treated with doxycycline) were randomized in the 2 trials, with diagnosis of early Lyme disease confirmed in 79% (281/355). The clinical diagnosis of early Lyme disease in these subjects was validated by 1) blinded expert reading of photographs, when available, of the pretreatment erythema migrans skin lesion, and 2) serologic confirmation (using enzyme-linked immunosorbent assay [ELISA] and immunoblot assay [“Western” blot]) of the presence of antibodies specific to Borrelia burgdorferi, the etiologic agent of Lyme disease. The efficacy data in Table 11 are specific to this “validated” patient subset, while the safety data below reflect the entire patient population for the 2 trials. Clinical data for evaluable subjects in the “validated” patient subset are shown in Table 11.
Table 11. Clinical Effectiveness of CEFTIN Tablets Compared with Doxycycline in the Treatment of Early Lyme Disease a 95% confidence interval around the satisfactory difference for Part I (-0.08, +0.05). b 95% confidence interval around the satisfactory difference for Part II (-0.13, +0.07). c n’s include subjects assessed as unsatisfactory clinical outcomes (failure + recurrence) in Part I (CEFTIN ‑ 11 [5 failure, 6 recurrence]; doxycycline - 8 [6 failure, 2 recurrence]). d Satisfactory clinical outcome includes cure + improvement (Part I) and success + improvement (Part II).
Part I
(1 Month after 20 Days of Treatment)a
Part II
(1 Year after 20 Days of Treatment)b
CEFTIN
500 mg Twice Daily
(n = 125)
Doxycycline
100 mg 3 Times Daily
(n = 108)
CEFTIN
500 mg Twice Daily
(n = 105c)
Doxycycline
100 mg 3 Times Daily
(n = 83c)
Satisfactory clinical outcomed
91%
93%
84%
87%
Clinical cure/success
72%
73%
73%
73%
Clinical improvement
19%
19%
10%
13%
CEFTIN and doxycycline were effective in prevention of the development of sequelae of late Lyme disease.
While the incidence of drug-related gastrointestinal adverse reactions was similar in the 2 treatment groups (cefuroxime axetil - 13%; doxycycline - 11%), the incidence of drug-related diarrhea was higher in the cefuroxime axetil arm versus the doxycycline arm (11% versus 3%, respectively).
16 How Supplied/storage And Handling
CEFTIN tablets, 250 mg of cefuroxime (as cefuroxime axetil), are white, capsule‑shaped, film‑coated tablets engraved with "GX ES7" on one side and blank on the other side as follows:
20 Tablets/Bottle NDC 0173-0387-00
CEFTIN tablets, 500 mg of cefuroxime (as cefuroxime axetil), are white, capsule‑shaped, film‑coated tablets engraved with "GX EG2" on one side and blank on the other side as follows:
20 Tablets/Bottle NDC 0173-0394-00
Store the tablets between 15° and 30°C (59° and 86°F). Replace cap securely after each opening.
CEFTIN for oral suspension is provided as dry, white to off‑white, tutti‑frutti–flavored powder. When reconstituted as directed, the suspension provides the equivalent of 125 mg or 250 mg of cefuroxime (as cefuroxime axetil) per 5 mL. It is supplied in amber glass bottles as follows:
125 mg/5 mL:
100‑mL Suspension NDC 0173-0740-00
250 mg/5 mL:
50‑mL Suspension NDC 0173-0741-10
100‑mL Suspension NDC 0173-0741-00
Before reconstitution, store dry powder between 2° and 30°C (36° and 86°F).
After reconstitution, immediately store suspension refrigerated between 2° and 8°C (36° and 46°F). DISCARD AFTER 10 DAYS.
17 Patient Counseling Information
Allergic Reactions
Inform patients that CEFTIN is a cephalosporin that can cause allergic reactions in some individuals [see Warnings and Precautions (5.1)].
Clostridioides difficile-Associated Diarrhea
Inform patients that diarrhea is a common problem caused by antibacterials, and it usually ends when the antibacterial is discontinued. Sometimes after starting treatment with antibacterials, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as 2 or more months after having taken their last dose of the antibacterial. If this occurs, advise patients to contact their physician as soon as possible.
Phenylketonuria
Inform patients and caregivers that CEFTIN for oral suspension contains phenylalanine (a component of aspartame) [see Warnings and Precautions (5.5)].
Crushing Tablets
Instruct patients to swallow the tablet whole, without crushing the tablet. Patients who cannot swallow the tablet whole should receive the oral suspension.
Oral Suspension
Instruct patients to shake the oral suspension well before each use, store in the refrigerator, and discard after 10 days. The oral suspension should be taken with food.
Drug Resistance
Inform patients that antibacterial drugs, including CEFTIN, should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When CEFTIN is prescribed to treat a bacterial infection, inform patients that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may: (1) decrease the effectiveness of the immediate treatment, and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by CEFTIN or other antibacterial drugs in the future.
Trademark is owned by or licensed to the GSK group of companies.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2021 GSK group of companies or its licensor.
CFT:9PI
Package Label.principal Display Panel
PRINCIPAL DISPLAY PANEL
NDC 0173-0387-00
Ceftin® Tablets
(cefuroxime axetil tablets)
250 mg
20 tablets
Rx only
Replace cap securely after each opening.
Each tablet contains cefuroxime axetil equivalent to 250 mg of cefuroxime.
See package insert for Dosage and Administration.
Store between 15º and 30ºC (59º and 86ºF).
GlaxoSmithKline
RTP, NC 27709
Made in England
- 10000000136237 Rev. 9/15
![]()
Package Label.principal Display Panel
PRINCIPAL DISPLAY PANEL
NDC 0173-0740-00
Ceftin® for Oral Suspension
(cefuroxime axetil for oral suspension)
For Oral Use Only
125 mg per 5 mL
100 mL (when reconstituted)
Rx only
Contains 3.0 g of cefuroxime axetil equivalent to 2.5 g of cefuroxime.
Phenylketonurics: Contains Phenylalanine 11.8 mg per 5 mL (1 teaspoonful) constituted suspension.
See package insert for Dosage and Administration.
Directions for Mixing Oral Suspension: Prepare the suspension at time of dispensing. Shake the bottle to loosen the powder. Remove the cap. Add 37 mL of water for reconstitution and replace the cap. Invert bottle and vigorously rock it from side to side so that water rises through the powder. Once the sound of powder against the bottle disappears, turn thebottle upright and vigorously shake it in a diagonal direction.
Before reconstitution, store dry powder between 2º and 30ºC (36º and 86ºF).
After reconstitution, store suspension between 2º and 8ºC (36º and 46ºF), in a refrigerator. SHAKE WELL BEFORE EACH USE. Replace cap securely after each opening. Discard after 10 days.
GlaxoSmithKline
Research Triangle Park, NC 27709
Made in England
- 10000000136641 Rev. 8/15
![]()
Package Label.principal Display Panel
PRINCIPAL DISPLAY PANEL
NDC 0173-0741-10
Ceftin® for Oral Suspension
(cefuroxime axetil for oral suspension)
For Oral Use Only
250 mg per 5 mL
50 mL (when reconstituted)
Rx only
Contains 3.6 g of cefuroxime axetil equivalent to 3 g of cefuroxime.
Phenylketonurics: Contains Phenylalanine 25.2 mg per 5 mL (1 teaspoonful) constituted suspension.
See package insert for Dosage and Administration.
Directions for Mixing Oral Suspension: Prepare the suspension at time of dispensing. Shake the bottle to loosen the powder. Remove the cap. Add 19 mL of water for reconstitution and replace the cap. Invert bottle and vigorously rock it from side to side so that water rises through the powder. Once the sound of powder against the bottle disappears, turn the bottle upright and vigorously shake it in a diagonal direction.
Before reconstitution, store dry powder between 2º and 30ºC (36º and 86ºF).
After reconstitution, store suspension between 2º and 8ºC (36º and 46ºF), in a refrigerator. SHAKE WELL BEFORE EACH USE. Replace cap securely after each opening. Discard after 10 days.
GlaxoSmithKline
RTP, NC 27709
Made in England
- 10000000136681 Rev. 8/15
![]()
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site