Lansoprazole, Amoxicillin, and Clarithromycin (amoxicillin 500 mg) Dailymed
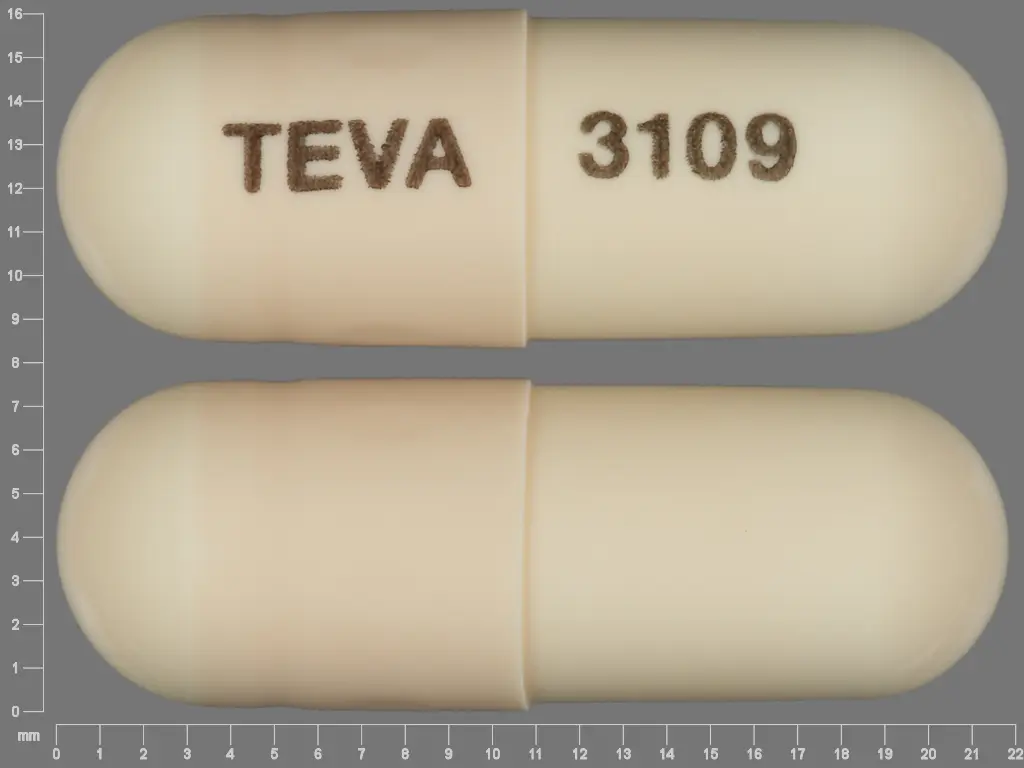
IMPRINT: TEVA 3109
SHAPE: capsule
COLOR: brown
All Imprints
lansoprazole 30 mg - 93 7351 93 7351 capsule
clarithromycin 500 mg oral tablet - 93 7158 oval yellow
amoxicillin 500 mg - teva 3109 capsule brown
Go PRO for all pill images
To reduce the development of drug-resistant bacteria and maintain the effectiveness of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets and other antibacterial drugs, lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
THESE PRODUCTS ARE INTENDED ONLY FOR USE AS DESCRIBED. The individual products contained in this package should not be used alone or in combination for other purposes. The information described in this labeling concerns only the use of these products as indicated in this daily administration pack. For information on use of the individual components when dispensed as individual medications outside this combined use for treating Helicobacter pylori (H. pylori), please see the package inserts for each individual product.
Description
Lansoprazole delayed-release capsules USP, amoxicillin capsules USP, and clarithromycin tablets USP consist of a daily administration card containing two 30 mg lansoprazole delayed-release capsules USP, four 500 mg amoxicillin capsules USP, and two 500 mg clarithromycin tablets USP, for oral administration.
Lansoprazole Delayed-Release Capsules USP
The active ingredient in lansoprazole delayed-release capsules USP is lansoprazole, a substituted benzimidazole, 2-[[[3-methyl-4-(2,2,2-trifluoroethoxy)-2-pyridyl]methyl]sulfinyl] benzimidazole, a compound that inhibits gastric acid secretion. Lansoprazole has the following structure:
![]()
C16H14F3N3O2S M.W. 369.36
Lansoprazole is a white to brownish-white odorless crystalline powder which melts with decomposition at approximately 166¬įC. Lansoprazole is freely soluble in dimethylformamide; soluble in methanol; sparingly soluble in ethanol; slightly soluble in ethyl acetate, dichloromethane and acetonitrile; very slightly soluble in ether; and practically insoluble in hexane and water.
Each delayed-release capsule contains enteric-coated granules consisting of 30 mg of lansoprazole (active ingredient) and the following inactive ingredients: black iron oxide, gelatin, hypromellose, magnesium carbonate, methacrylic acid copolymer dispersion, propylene glycol, red iron oxide, shellac, sugar spheres (which contain sucrose and corn starch), talc, titanium dioxide, and triethyl citrate. Imprinting ink may contain potassium hydroxide.
Amoxicillin Capsules USP
Amoxicillin is a semisynthetic antibiotic, an analogue of ampicillin, with a broad spectrum of bactericidal activity against many gram-positive and gram-negative microorganisms. Chemically it is (2S,5R,6R)-6-[(R)-(-)-2-amino-2-(p-hydroxyphenyl)acetamido]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid trihydrate. Amoxicillin has the following structure:
![]()
C16H19N3O5S ‚ÄĘ 3H2O M.W. 419.45
Amoxicillin capsules USP are intended for oral administration. The buff-colored capsules contain amoxicillin trihydrate equivalent to 500 mg of amoxicillin.
Inactive ingredients: CAPSULES-DRUG PRODUCT: magnesium stearate. CAPSULE SHELL AND PRINT CONSTITUENTS: black iron oxide, D&C Yellow #10, D&C Yellow #10 Aluminum Lake, FD&C Blue #1 Aluminum Lake, FD&C Blue #2 Aluminum Lake, FD&C Red #40, FD&C Red #40 Aluminum Lake, gelatin, propylene glycol, shellac, and titanium dioxide and may also contain methylparaben, potassium hydroxide, propylparaben, silicon dioxide and sodium lauryl sulfate.
Clarithromycin Tablets USP
Clarithromycin is a semi-synthetic macrolide antibiotic. Chemically, it is 6-O-methylerythromycin. Clarithromycin has the following structure:
![]()
C38H69NO13 M.W. 747.96
Clarithromycin is a white to off-white crystalline powder. It is soluble in acetone, slightly soluble in methanol, ethanol, and acetonitrile, and practically insoluble in water. Each light-yellow oval-shaped film-coated immediate-release tablet contains 500 mg of clarithromycin and the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, FD&C blue # 2 indigo carmine lake, FD&C red # 40 allura red AC lake, FD&C yellow # 5 tartrazine lake, hypromellose, magnesium hydroxide, magnesium stearate, microcrystalline cellulose, polyethylene glycol, povidone, sodium starch glycolate, stearic acid, titanium dioxide, and vanillin.
Clinical Pharmacology
Pharmacokinetics
Coadministration of all three components of the lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets for pharmacokinetics have not been studied. Studies have shown no clinically significant interactions of lansoprazole and amoxicillin or lansoprazole and clarithromycin when administered together. There is no information about the gastric mucosal concentrations of lansoprazole, amoxicillin and clarithromycin after administration of these agents concomitantly. The systemic pharmacokinetic information presented below is based on studies in which each product was administered alone.
Lansoprazole
Absorption: Lansoprazole delayed-release capsules contain an enteric-coated granule formulation of lansoprazole. Absorption of lansoprazole begins only after the granules leave the stomach. The absorption of lansoprazole is rapid, with the mean Cmax occurring approximately 1.7 hours after oral dosing, and the absolute bioavailability is over 80%. Both the Cmax and AUC are diminished by about 50 to 70% if lansoprazole is given 30 minutes after food, compared to the fasting condition. There is no significant food effect if lansoprazole is given before meals.
Distribution: Lansoprazole is 97% bound to plasma proteins. Plasma protein binding is constant over the concentration range of 0.05 to 5.0 mcg/mL.
Metabolism: Lansoprazole is extensively metabolized in the liver. Two metabolites have been identified in measurable quantities in plasma (the hydroxylated sulfinyl and sulfone derivatives of lansoprazole). These metabolites have very little or no antisecretory activity. Lansoprazole is thought to be transformed into two active species which inhibit acid secretion by blocking the proton pump [(H+,K+)-ATPase enzyme system] at the secretory surface of the gastric parietal cell. The two active species are not present in the systemic circulation. Therefore, the plasma elimination half-life of lansoprazole does not reflect its duration of suppression of gastric acid secretion.
Elimination: Following single-dose oral administration of lansoprazole, virtually no unchanged lansoprazole was excreted in the urine. In one study, after a single oral dose of 14C-lansoprazole, approximately one-third of the administered radiation was excreted in the urine and two-thirds was recovered in the feces. This implies a significant biliary excretion of the lansoprazole metabolites.
Amoxicillin
Absorption: Amoxicillin is stable in the presence of gastric acid and may be given without regard to meals. It is rapidly absorbed after oral administration. Orally administered doses of 500 mg amoxicillin capsules result in average peak blood levels one to two hours after administration in the range of 5.5 mcg/mL to 7.5 mcg/mL.
Distribution: Amoxicillin diffuses readily into most body tissues and fluids, with the exception of brain and spinal fluid, except when meninges are inflamed. In blood serum, amoxicillin is approximately 20% protein-bound.
Metabolism/Elimination: The elimination half-life of amoxicillin is 61.3 minutes. Detectable serum levels are observed up to eight hours after an orally administered dose of amoxicillin. Approximately 60% of the orally administered dose of amoxicillin is excreted unchanged in the urine within six to eight hours post-dose; its excretion can be delayed by concurrent administration of probenecid.
Clarithromycin
Absorption: Clarithromycin is rapidly absorbed from the gastrointestinal tract after oral administration. The absolute bioavailability of 250 mg clarithromycin tablets was approximately 50%. For a single 500 mg dose of clarithromycin, food slightly delays the onset of clarithromycin absorption, increasing the peak time from approximately two to 2.5 hours. Food also increases the clarithromycin peak plasma concentration by about 24%, but does not affect the extent of clarithromycin bioavailability. Food does not affect the onset of formation of the antimicrobially active metabolite, 14-OH clarithromycin or its peak plasma concentration but does slightly decrease the extent of metabolite formation, indicated by an 11% decrease in area under the plasma concentration-time curve (AUC). Therefore, clarithromycin tablets may be given without regard to food.
In nonfasting, healthy human subjects (males and females), peak plasma concentrations were attained within two to three hours after oral dosing. Steady-state peak plasma clarithromycin concentrations were attained within three days and were approximately 3 to 4 mcg/mL with a 500 mg dose administered every eight to 12 hours.
Metabolism/Elimination: The elimination half-life of clarithromycin was five to seven hours with 500 mg administered every eight to 12 hours. The nonlinearity of clarithromycin pharmacokinetics is slight at the recommended dose of 500 mg administered every eight to 12 hours. With a 500 mg every eight to 12 hours dosing, the peak steady-state concentration of 14-OH clarithromycin is up to 1 mcg/mL, and its elimination half-life is about seven to nine hours. The steady-state concentration of this metabolite is generally attained within three to four days.
After a 500 mg tablet every 12 hours, the urinary excretion of clarithromycin is approximately 30%. The renal clearance of clarithromycin approximates the normal glomerular filtration rate. The major metabolite found in urine is 14-OH clarithromycin, which accounts for an additional 10% to 15% of the dose with a 500 mg tablet administered every 12 hours.
Steady-state concentrations of clarithromycin and 14-OH clarithromycin observed following administration of 500 mg doses of clarithromycin every 12 hours to adult patients with HIV were similar to those observed in healthy volunteers. In adult HIV-infected patients taking 500 mg doses of clarithromycin every 12 hours, steady-state clarithromycin Cmax values ranged from 2 to 4 mcg/mL.
The steady-state concentrations of clarithromycin in subjects with impaired hepatic function did not differ from those in normal subjects; however, the 14-OH clarithromycin concentrations were lower in the hepatically impaired subjects. The decreased formation of 14-OH clarithromycin was at least partially offset by an increase in renal clearance of clarithromycin in the subjects with impaired hepatic function when compared to healthy subjects.
The pharmacokinetics of clarithromycin was also altered in subjects with impaired renal function (see PRECAUTIONS and DOSAGE AND ADMINISTRATION).
Clarithromycin and the 14-OH clarithromycin metabolite distribute readily into body tissues and fluids. There are no data available on cerebrospinal fluid penetration. Because of high intercellular concentrations, tissue concentrations are higher than serum concentrations.
Special Populations
Geriatric Use: The clearance of lansoprazole is decreased in the elderly, with elimination half-life increased approximately 50% to 100%. Because the mean half-life in the elderly remains between 1.9 to 2.9 hours, repeated once daily dosing does not result in accumulation of lansoprazole. Peak plasma levels were not increased in the elderly.
Renal Impairment: In patients with severe renal impairment, plasma protein binding decreased by 1.0% to 1.5% after administration of 60 mg of lansoprazole. Patients with renal impairment had a shortened elimination half-life and decreased total AUC (free and bound). The AUC for free lansoprazole in plasma, however, was not related to the degree of renal impairment; and the Cmax and Tmax (time to reach the maximum concentration) were not different than the Cmax and Tmax from subjects with normal renal function (see DOSAGE AND ADMINISTRATION).
Hepatic Impairment: In patients with various degrees of chronic hepatic impairment, the mean plasma half-life of lansoprazole was prolonged from 1.5 hours to 3.2 to 7.2 hours. An increase in the mean AUC of up to 500% was observed at steady state in hepatically-impaired patients compared to healthy subjects. Consider reduction of lansoprazole dosage in patients with severe hepatic impairment.
Gender: In a study comparing 12 male and six female human subjects who received lansoprazole, no gender differences were found in pharmacokinetics and intragastric pH results.
Race: The pooled pharmacokinetic parameters of lansoprazole from twelve U.S. Phase I studies (N = 513) were compared to the mean pharmacokinetic parameters from two Asian studies (N = 20). The mean AUCs of lansoprazole in Asian subjects were approximately twice those seen in pooled U.S. data; however, the inter-individual variability was high. The Cmax values were comparable.
Pharmacodynamics
Microbiology
Lansoprazole, clarithromycin and/or amoxicillin have been shown to be active against most strains of Helicobacter pyloriin vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Helicobacter pylori Pretreatment Resistance
Clarithromycin pretreatment resistance rates were 9.5% (91/960) by E-test and 11.3% (12/106) by agar dilution in the dual and triple therapy clinical trials (M93-125, M93-130, M93-131, M95-392, and M95-399).
Amoxicillin pretreatment susceptible isolates (‚ȧ 0.25 mcg /mL) occurred in 97.8% (936/957) and 98.0% (98/100) of the patients in the dual and triple therapy clinical trials by E-test and agar dilution, respectively. Twenty-one of 957 patients (2.2%) by E-test, and two of 100 patients (2.0%) by agar dilution, had amoxicillin pretreatment MICs of greater than 0.25 mcg/mL. One patient on the 14-day triple therapy regimen had an unconfirmed pretreatment amoxicillin minimum inhibitory concentration (MIC) of greater than 256 mcg/mL by E-test and the patient was eradicated of H. pylori.
Table 1: Clarithromycin Susceptibility Test Results and Clinical/Bacteriological Outcomes Includes only patients with pretreatment clarithromycin susceptibility test results
Clarithromycin Pretreatment Results
Clarithromycin Post-treatment Results
H. pylori negative - eradicated
H. pylori positive - not eradicated
Post-treatment susceptibility results
SBreakpoints for antimicrobial susceptibility testing at the time of the studies were: Susceptible (S) MIC ‚ȧ 0.25 mcg/mL, Intermediate (I) MIC 0.5 to 1.0 mcg/mL, Resistant (R) MIC ‚Č• 2 mcg/mL. For current performance standards for antimicrobial susceptibility testing, see section below title, Susceptibility Test for Helicobacter pylori.
I
R
No MIC
Triple Therapy 14-Day (lansoprazole 30 mg twice daily/amoxicillin 1 g twice daily/clarithromycin 500 mg twice daily) (M95-399, M93-131, M95-392)
Susceptible
112
105
7
Intermediate
3
3
Resistant
17
6
7
4
Triple Therapy 10-Day (lansoprazole 30 mg twice daily/amoxicillin 1 g twice daily/clarithromycin 500 mg twice daily) (M95-399)
Susceptible
42
40
1
1
Intermediate
Resistant
4
1
3
Patients not eradicated of H. pylori following lansoprazole/amoxicillin/clarithromycin triple therapy will likely have clarithromycin resistant H. pylori isolates. Therefore, for those patients who fail therapy, clarithromycin susceptibility testing should be done if possible. Patients with clarithromycin resistant H. pylori should not be treated with lansoprazole/amoxicillin/clarithromycin triple therapy or other regimens which include clarithromycin as the sole antimicrobial agent.
Amoxicillin Susceptibility Test Results and Clinical/Bacteriological Outcomes
In the dual and triple therapy clinical trials, 82.6% (195/236) of the patients that had pretreatment amoxicillin susceptible MICs (‚ȧ 0.25 mcg/mL) were eradicated of H. pylori. Of those with pretreatment amoxicillin MICs of greater than 0.25 mcg/mL, three of six had the H. pylori eradicated. A total of 30% (21/70) of the patients failed lansoprazole 30 mg three times daily per amoxicillin 1 g three times daily dual therapy and a total of 12.8% (22/172) of the patients failed the 10-and 14-day triple therapy regimens. Post-treatment susceptibility results were not obtained on 11 of the patients who failed therapy. Nine of the 11 patients with amoxicillin post-treatment MICs that failed the triple therapy regimen also had clarithromycin resistant H. pylori isolates.
Susceptibility Test for Helicobacter pylori
The reference methodology for susceptibility testing of H. pylori is agar dilution MICs1. One to three microliters of an inoculum equivalent to a No. 2 McFarland standard (1 x 107-1 x 108 CFU/mL for H. pylori) are inoculated directly onto freshly prepared antimicrobial containing Mueller-Hinton agar plates with 5% aged defibrinated sheep blood (greater than 2 weeks old). The agar dilution plates are incubated at 35¬įC in a microaerobic environment produced by a gas generating system suitable for Campylobacter species. After three days of incubation, the MICs are recorded as the lowest concentration of antimicrobial agent required to inhibit growth of the organism. The clarithromycin and amoxicillin MIC values should be interpreted according to the following criteria:
Susceptibility Test Interpretive Criteria for H. pylori
Clarithromycin MIC (mcg/mL)These are tentative breakpoints for the agar dilution methodology and they should not be used to interpret results obtained using alternative methods.
Interpretation
‚ȧ 0.25
Susceptible (S)
0.5
Intermediate (I)
‚Č• 1.0
Resistant (R)
Susceptibility Test Interpretive Criteria for H. pylori
Amoxicillin MIC (mcg/mL), There were not enough organisms with MICs greater than 0.25 mcg/mL to determine a resistance breakpoint.
Interpretation
< 0.25
Susceptible (S)
Standardized susceptibility test procedures require the use of laboratory control bacteria to monitor and ensure the accuracy and precision of supplies and reagents in the assay, and the techniques of the individual performing the test. Standard clarithromycin or amoxicillin powder should provide the following MIC ranges.
Acceptable Quality Control Ranges
Antimicrobial Agent
MIC (mcg/mL)These are quality control ranges for the agar dilution methodology and they should not be used to control test results obtained using alternative methods.
H. pylori ATCC 43504
Clarithromycin
0.015 to 0.12
H. pylori ATCC 43504
Amoxicillin
0.015 to 0.12
Antisecretory activity
After oral administration, lansoprazole was shown to significantly decrease the basal acid output and significantly increase the mean gastric pH and percent of time the gastric pH was greater than three and greater than four. Lansoprazole also significantly reduced meal-stimulated gastric acid output and secretion volume, as well as pentagastrin-stimulated acid output. In patients with hypersecretion of acid, lansoprazole significantly reduced basal and pentagastrin-stimulated gastric acid secretion. Lansoprazole inhibited the normal increases in secretion volume, acidity and acid output induced by insulin.
The intragastric pH results of a five-day, pharmacodynamic, crossover study of 15 mg and 30 mg of once daily lansoprazole are presented in Table 2.
Table 2: Mean Antisecretory Effects After Single and Multiple Daily Lansoprazole Dosing
Lansoprazole
Parameter
Baseline Value
15 mg
30 mg
Day 1
Day 5
Day 1
Day 5
Mean 24 Hour pH
2.1
2.7(p < 0.05) versus baseline only.
4.0
3.6(p < 0.05) versus baseline and lansoprazole 15 mg.
4.9
Mean Nighttime Hour pH
1.9
2.4
3.0
2.6
3.8
% Time Gastric pH > 3
18
33
59
51
72
% Time Gastric pH > 4
12
22
49
41
66
NOTE: An intragastric pH of greater than 4 reflects a reduction in gastric acid by 99%.
After the initial dose in this study, increased gastric pH was seen within one to two hours with 30 mg of lansoprazole and two to three hours with 15 mg of lansoprazole. After multiple daily dosing, increased gastric pH was seen within the first hour post-dosing with 30 mg of lansoprazole and within one to two hours post-dosing with 15 mg of lansoprazole.
Acid suppression may enhance the effect of antimicrobials in eradicating Helicobacter pylori (H. pylori). The percentage of time gastric pH was elevated above five and six was evaluated in a crossover study of lansoprazole given daily, twice daily and three times daily.
Table 3: Mean Antisecretory Effects After 5 Days of Twice Daily and Three Times Daily Dosing
Lansoprazole
Parameter
30 mg daily
15 mg twice daily
30 mg twice daily
30 mg three times daily
% Time Gastric pH > 5
43
47
59(p < 0.05) versus lansoprazole 30 mg daily
77(p < 0.05) versus lansoprazole 30 mg daily, 15 mg twice daily and 30 mg twice daily
% Time Gastric pH > 6
20
23
28
45
The inhibition of gastric acid secretion as measured by intragastric pH gradually returned to normal over two to four days after multiple doses. There was no indication of rebound gastric acidity.
Clinical Studies
Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
Randomized, double-blind clinical studies performed in the U.S. in patients with H. pylori and duodenal ulcer disease (defined as an active ulcer or history of an ulcer within one year) evaluated the efficacy of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets as triple 14 day therapy for the eradication of H. pylori. The triple therapy regimen (lansoprazole 30 mg twice daily/amoxicillin 1 g twice daily/clarithromycin 500 mg twice daily) produced statistically significantly higher eradication rates than lansoprazole plus amoxicillin, lansoprazole plus clarithromycin, and amoxicillin plus clarithromycin dual therapies.
H. pylori eradication was defined as two negative tests (culture and histology) at four to six weeks following the end of treatment.
Triple therapy was shown to be more effective than all possible dual therapy combinations. The combination of lansoprazole plus amoxicillin and clarithromycin as triple therapy was effective in eradicating H. pylori. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence.
A randomized, double-blind clinical study performed in the U.S. in patients with H. pylori and duodenal ulcer disease (defined as an active ulcer or history of an ulcer within one year) compared the efficacy of lansoprazole triple therapy for ten and 14 days. This study established that the 10-day triple therapy was equivalent to the 14-day triple therapy in eradicating H. pylori.
Table 4: H. pylori Eradication Rates ‚Äď Triple Therapy of Lansoprazole Delayed-Release Capsules/Amoxicillin Capsules/Clarithromycin Tablets Percent of Patients Cured [95% Confidence Interval] (Number of Patients)
Study
Duration
Triple Therapy Evaluable AnalysisBased on evaluable patients with confirmed duodenal ulcer (active or within one year) and H. pylori infection at baseline defined as at least two of three positive endoscopic tests from CLOtest¬ģ, histology and/or culture. Patients were included in the analysis if they completed the study. Additionally, if patients dropped out of the study due to an adverse event related to the study drug, they were included in the evaluable analysis as failures of therapy.
Triple Therapy Intent-to-Treat AnalysisPatients were included in the analysis if they had documented H. pylori infection at baseline as defined above and had a confirmed duodenal ulcer (active or within one year). All dropouts were included as failures of therapy.
M93-131
14 days
92(p < 0.05) versus lansoprazole/amoxicillin and lansoprazole/clarithromycin dual therapy [80.0 to 97.7] (N = 48)
86[73.3 to 93.5] (N = 55)
M95-392
14 days
86(p < 0.05) versus clarithromycin/amoxicillin dual therapy [75.7 to 93.6] (N = 66)
83[72.0 to 90.8] (N = 70)
M95-399The 95% confidence interval for the difference in eradication rates, 10 day minus 14 day is (-10.5, 8.1) in the evaluable analysis and (-9.7, 9.1) in the intent-to-treat analysis.
14 days
85 [77.0 to 91.0] (N = 113)
82 [73.9 to 88.1] (N = 126)
10 days
84 [76.0 to 89.8] (N = 123)
81 [73.9 to 87.6] (N = 135)
Indications And Usage
Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
The components in lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets are indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or one-year history of a duodenal ulcer) to eradicate H. pylori. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence (see CLINICAL STUDIES and DOSAGE AND ADMINISTRATION).
To reduce the development of drug-resistant bacteria and maintain the effectiveness of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets and other antibacterial drugs, lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Contraindications
Lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets are contraindicated in patients with known severe hypersensitivity to any component of the formulation of lansoprazole. Hypersensitivity reactions may include anaphylaxis, anaphylactic shock, angioedema, bronchospasm, acute interstitial nephritis, and urticaria (see ADVERSE REACTIONS).
A history of severe hypersensitivity reactions (e.g., anaphylaxis or Stevens-Johnson syndrome) to amoxicillin or other beta-lactam antibiotics (e.g., penicillins and cephalosporins) is a contraindication.
Clarithromycin is contraindicated in patients with a known hypersensitivity to clarithromycin, erythromycin, or any of the macrolide antibiotics.
Clarithromycin is contraindicated in patients with a history of cholestatic jaundice/hepatic dysfunction associated with prior use of clarithromycin.
Clarithromycin should not be given to patients with history of QT prolongation or ventricular cardiac arrhythmia, including torsades de pointes.
Concomitant administration of clarithromycin, a component of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets, and any of the following drugs is contraindicated: cisapride, pimozide, astemizole, terfenadine, ergotamine or dihydroergotamine (see PRECAUTIONS, Drug Interactions). There have been post-marketing reports of drug interactions when clarithromycin and/or erythromycin are coadministered with cisapride, pimozide, astemizole, or terfenadine resulting in cardiac arrhythmias (QT prolongation, ventricular tachycardia, ventricular fibrillation, and torsades de pointes) most likely due to inhibition of metabolism of these drugs by erythromycin and clarithromycin. Fatalities have been reported.
Concomitant administration of clarithromycin and colchicine is contraindicated in patients with renal or hepatic impairment.
Clarithromycin should not be used concomitantly with HMG-CoA reductase inhibitors (statins) that are extensively metabolized by CYP3A4 (lovastatin or simvastatin), due to the increase risk of myopathy, including rhabdomyolysis (see WARNINGS).
Warnings
Acute Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients on penicillin therapy, including amoxicillin. Although anaphylaxis is more frequent following parenteral therapy, it has occurred in patients on oral penicillins. These reactions are more likely to occur in individuals with a history of penicillin hypersensitivity and/or a history of sensitivity to multiple allergens. There have been reports of individuals with a history of penicillin hypersensitivity who have experienced severe reactions when treated with cephalosporins. Before initiating therapy with lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets careful inquiry should be made regarding previous hypersensitivity reactions to penicillins, cephalosporins, or other allergens. In the event of severe acute hypersensitivity reactions, such as anaphylaxis, Stevens-Johnson Syndrome, toxic epidermal necrolysis, drug rash with eosinophilia and systemic symptoms (DRESS), and Henoch-Schonlein purpura lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets should be discontinued immediately and appropriate treatment should be urgently initiated.
Use in Pregnancy
CLARITHROMYCIN SHOULD NOT BE USED IN PREGNANT WOMEN EXCEPT IN CLINICAL CIRCUMSTANCES WHERE NO ALTERNATIVE THERAPY IS APPROPRIATE. IF PREGNANCY OCCURS WHILE TAKING CLARITHROMYCIN, THE PATIENT SHOULD BE INFORMED OF THE POTENTIAL HAZARD TO THE FETUS. CLARITHROMYCIN HAS DEMONSTRATED ADVERSE EFFECTS OF PREGNANCY OUTCOME AND/OR EMBRYO- FETAL DEVELOPMENT IN MONKEYS, RATS, MICE, AND RABBITS AT DOSES THAT PRODUCED PLASMA LEVELS TWO TO 17 TIMES THE SERUM LEVELS ACHIEVED IN HUMANS TREATED AT THE MAXIMUM RECOMMENDED HUMAN DOSES (see PRECAUTIONS, Pregnancy).
Hepatotoxicity
Hepatic dysfunction, including increased liver enzymes, and hepatocellular and/or cholestatic hepatitis, with or without jaundice, has been reported with clarithromycin. This hepatic dysfunction may be severe and is usually reversible. In some instances, hepatic failure with fatal outcome has been reported and generally has been associated with serious underlying diseases and/or concomitant medications. Discontinue clarithromycin immediately if signs and symptoms of hepatitis occur.
QT Prolongation
Clarithromycin has been associated with prolongation of the QT interval and infrequent cases of arrhythmia. Cases of torsades de pointes have been spontaneously reported during postmarketing surveillance in patients receiving clarithromycin. Fatalities have been reported. Clarithromycin should be avoided in patients with ongoing proarrhythmic conditions such as uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia (see CONTRAINDICATIONS) and in patients receiving Class IA (quinidine, procainamide) or Class III (dofetilide, amiodarone, sotalol) antiarrhythmic agents. Elderly patients may be more susceptible to drug-associated effects on the QT interval.
Gastric Malignancy
Symptomatic response to therapy with lansoprazole does not preclude the presence of gastric malignancy.
Acute Interstitial Nephritis
Acute interstitial nephritis (AIN) has been observed in patients taking proton pump inhibitors (PPIs) including lansoprazole. Acute interstitial nephritis may occur at any point during PPI therapy and is generally attributed to an idiopathic hypersensitivity reaction. Discontinue lansoprazole if AIN develops (see CONTRAINDICATIONS).
Drug Interactions
Serious adverse reactions have been reported in patients taking clarithromycin concomitantly with CYP3A4 substrates. These include colchicine toxicity with colchicine; rhabdomyolysis with simvastatin, lovastatin, and atorvastatin; and hypotension with calcium channel blockers metabolized by CYP3A4 (e.g., verapamil, amlodipine, diltiazem) (see CONTRAINDICATIONS and PRECAUTIONS, Drug Interactions).
Life-threatening and fatal drug interactions have been reported in patients treated with clarithromycin and colchicine. Clarithromycin is a strong CYP3A4 inhibitor and this interaction may occur while using both drugs at their recommended doses. If coadministration of clarithromycin and colchicine is necessary in patients with normal renal and hepatic function, the dose of colchicine should be reduced. Patients should be monitored for clinical symptoms of colchicine toxicity. Concomitant administration of clarithromycin and colchicine is contraindicated in patients with renal or hepatic impairment (see CONTRAINDICATIONS and PRECAUTIONS, Drug Interactions).
Oral Hypoglycemic Agents/Insulin
The concomitant use of clarithromycin and oral hypoglycemic agents and/or insulin can result in significant hypoglycemia. With certain hypoglycemic drugs such as nateglinide, pioglitazone, repaglinide and rosiglitazone, inhibition of CYP3A enzyme by clarithromycin may be involved and could cause hypoglycemia when used concomitantly. Careful monitoring of glucose is recommended.
Oral Anticoagulants
There is a risk of serious hemorrhage and significant elevations in INR and prothrombin time when clarithromycin is coadministered with warfarin. INR and prothrombin times should be frequently monitored while patients are receiving clarithromycin and oral anticoagulants concurrently.
HMG-CoA Reductase Inhibitors (statins)
Concomitant use of clarithromycin with lovastatin or simvastatin is contraindicated (see CONTRAINDICATIONS) as these statins are extensively metabolized by CYP3A4, and concomitant treatment with clarithromycin increases their plasma concentration, which increases the risk of myopathy, including rhabdomyolysis. Cases of rhabdomyolysis have been reported in patients taking clarithromycin concomitantly with these statins. If treatment with clarithromycin cannot be avoided, therapy with lovastatin or simvastatin must be suspended during the course of treatment.
Caution should be exercised when prescribing clarithromycin with statins. In situations where the concomitant use of clarithromycin with atorvastatin or pravastatin cannot be avoided, atorvastatin dose should not exceed 20 mg daily and pravastatin dose should not exceed 40 mg daily. Use of a statin that is not dependent on CYP3A metabolism (e.g., fluvastatin) can be considered. It is recommended to prescribe the lowest registered dose if concomitant use cannot be avoided.
Concomitant Use of Lansoprazole delayed-release capsules, Amoxicillin capsules, and Clarithromycin tablets with Methotrexate
Literature suggests that concomitant use of proton pump inhibitors (PPI) with methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets may be considered in some patients (see PRECAUTIONS, Drug Interactions).
Clostridium Difficile-Associated Diarrhea
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including clarithromycin and/or amoxicillin, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
In addition, published observational studies suggest that PPI therapy, may be associated with an increased risk of CDAD, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve.
Precautions
Clarithromycin tablets contain FD&C Yellow No. 5 (tartrazine) which may cause allergic-type reactions (including bronchial asthma) in certain susceptible persons. Although the overall incidence of FD&C Yellow No. 5 (tartrazine) sensitivity in the general population is low, it is frequently seen in patients who also have aspirin hypersensitivity.
General
The possibility of superinfections with mycotic or bacterial pathogens should be kept in mind during therapy. If superinfections occur, lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets should be discontinued and appropriate therapy instituted.
Prescribing lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Clarithromycin is principally excreted via the liver and kidney. Clarithromycin may be administered without dosage adjustment to patients with hepatic impairment and normal renal function. However, in the presence of severe renal impairment with or without coexisting hepatic impairment, decreased dosage or prolonged dosing intervals may be appropriate.
Exacerbation of symptoms of myasthenia gravis and new onset of symptoms of myasthenic syndrome has been reported in patients receiving clarithromycin therapy.
Information for Patients
Each dose of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets contains four pills: one capsule with a light-gray opaque cap and flesh-colored opaque body, filled with off-white to beige pellets (lansoprazole), two buff-colored capsules (amoxicillin) and one light-yellow tablet (clarithromycin). Each dose should be taken twice per day before eating. Patients should be instructed to swallow each pill whole.
Lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets may interact with some drugs; therefore patients should be advised to report to their doctor the use of any other medications.
Patients should be counseled that antibacterial drugs including lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets are prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Patients should be advised to immediately report and seek care for diarrhea that does not improve. This may be a sign of Clostridium difficile associated diarrhea (see WARNINGS).
Patients should be advised to immediately report and seek care for any cardiovascular or neurological symptoms including palpitations, dizziness, seizures, and tetany as these may be signs of hypomagnesemia (see WARNINGS).
Laboratory Tests
Periodic assessment of renal, hepatic, and hematopoietic function should be made during prolonged therapy.
Drug Interactions
No drug interaction studies have been conducted specifically with lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets. The following drug interactions are for the individual drug components: lansoprazole, amoxicillin, and clarithromycin. Therefore, the decision to adjust dosage should depend on the clinician's assessment of among other things, the cumulative or net effect of the drug components of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets.
Drugs with pH-Dependent Absorption Kinetics: Due to its effects on gastric acid secretion, lansoprazole can reduce the absorption of drugs where gastric pH is an important determinant of their bioavailability. As with other drugs that decrease the intragastric acidity, the absorption of drugs such as ampicillin esters, ketoconazole, atazanavir, iron salts, erlotinib, and mycophenolate mofetil can decrease, while the absorption of drugs such as digoxin can increase during treatment with lansoprazole. Atazanavir: Lansoprazole substantially decreases the systemic concentrations of the HIV protease inhibitor atazanavir, which is dependent upon the presence of gastric acid for absorption, and may result in a loss of therapeutic effect of atazanavir and the development of HIV resistance. Therefore, lansoprazole should not be coadministered with atazanavir.
Mycophenolate: Coadministration of PPIs in healthy volunteers and in transplant patients receiving mycophenolate mofetil has been reported to reduce the exposure to the active metabolite, mycophenolic acid (MPA), possibly due to a decrease in mycophenolate mofetil solubility at an increased gastric pH. The clinical relevance of reduced MPA exposure on organ rejection has not been established in transplant patients receiving PPIs and mycophenolate mofetil. Use PPIs with caution in transplant patients receiving mycophenolate mofetil.
Drugs Metabolized by P450 Enzymes: Lansoprazole is metabolized through the cytochrome P450 system (CYP450), specifically by CYP3A and CYP2C19 isozymes. Studies in healthy subjects have shown that lansoprazole does not have clinically significant interactions with other drugs metabolized by CYP450, particularly warfarin, antipyrine, indomethacin, ibuprofen, phenytoin, propranolol, prednisone, diazepam, or clarithromycin. These compounds are metabolized through various CYP450 enzymes including CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A. However, other studies or post-marketing reports have shown that the interaction of lansoprazole with other drugs metabolized by these CYP450 enzymes may be clinically significant.
Theophylline: When lansoprazole was administered concomitantly with theophylline (CYP1A2, CYP3A), a minor increase (10%) in the clearance of theophylline was seen. Because of the small magnitude and the direction of the effect on theophylline clearance, this interaction is unlikely to be of clinical concern. Nonetheless, individual patients may require additional titration of their theophylline dosage when lansoprazole is started or stopped to ensure clinically effective blood levels.
Tacrolimus: Concomitant administration of lansoprazole and tacrolimus may increase whole blood levels of tacrolimus, especially in transplant patients who are intermediate or poor metabolizers of CYP2C19.
Warfarin: In a study of healthy subjects, neither the pharmacokinetics of warfarin enantiomers nor prothrombin time were affected following single or multiple 60 mg doses of lansoprazole. However, there have been reports of increased International Normalized Ratio (INR) and prothrombin time in patients receiving proton pump inhibitors, including lansoprazole, and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.
Sucralfate: In a single-dose crossover study examining lansoprazole 30 mg and omeprazole 20 mg each administered alone and concomitantly with sucralfate 1 gram, absorption of the proton pump inhibitors was delayed and their bioavailability was reduced by 17% and 16%, respectively, when administered concomitantly with sucralfate. Therefore, proton pump inhibitors should be taken at least 30 minutes prior to sucralfate. In clinical trials, antacids were administered concomitantly with lansoprazole and there was no evidence of a change in the efficacy of lansoprazole.
Clopidogrel: Concomitant administration of lansoprazole and clopidogrel in healthy subjects had no clinically important effect on exposure to the active metabolite of clopidogrel or clopidogrel-induced platelet inhibition. No dose adjustment of clopidogrel is necessary when administered with an approved dose of lansoprazole.
Methotrexate: Case reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of high dose methotrexate with PPIs have been conducted.
In a study of rheumatoid arthritis patients receiving low-dose methotrexate, lansoprazole and naproxen, no effect on pharmacokinetics of methotrexate was observed.
Amoxicillin
Probenecid: Probenecid decreases the renal tubular secretion of amoxicillin. Concurrent use of amoxicillin and probenecid may result in increased and prolonged blood levels of amoxicillin.
Antibiotics: Chloramphenicol, macrolides, sulfonamides, and tetracyclines may interfere with bactericidal effects of penicillin. This has been demonstrated in vitro; however, the clinical significance of this interaction is not well documented.
In common with other antibiotics, amoxicillin may affect the gut flora, leading to lower estrogen reabsorption and reduced efficacy of combined oral estrogen/progesterone contraceptives.
Clarithromycin
Theophylline: Clarithromycin use in patients who are receiving theophylline may be associated with an increase of serum theophylline concentrations. Monitoring of serum theophylline concentrations should be considered for patients receiving high doses of theophylline or with baseline concentrations in the upper therapeutic range. In two studies in which theophylline was administered with clarithromycin (a theophylline sustained-release formulation was dosed at either 6.5 mg/kg or 12 mg/kg together with 250 or 500 mg every12 hours clarithromycin), the steady-state levels of Cmax, Cmin, and the area under the serum concentration time curve (AUC) of theophylline increased about 20%.
Verapamil: Hypotension, bradyarrhythmias, and lactic acidosis have been observed in patients receiving concurrent verapamil, belonging to the calcium channel blockers drug class.
Carbamazepine: Concomitant administration of single doses of clarithromycin and carbamazepine has been shown to result in increased plasma concentrations of carbamazepine. Blood level monitoring of carbamazepine may be considered.
Terfenadine: When clarithromycin and terfenadine were coadministered, plasma concentrations of the active acid metabolite of terfenadine were threefold higher, on average, than the values observed when terfenadine was administered alone. The pharmacokinetics of clarithromycin and the 14-OH-clarithromycin were not significantly affected by coadministration of terfenadine once clarithromycin reached steady-state conditions. Concomitant administration of clarithromycin with terfenadine is contraindicated (see CONTRAINDICATIONS).
Zidovudine: Simultaneous oral administration of clarithromycin tablets and zidovudine to HIV-infected adult patients may result in decreased steady-state zidovudine concentrations. Following administration of clarithromycin 500 mg tablets twice daily with zidovudine 100 mg every four hours, the steady-state zidovudine AUC decreased 12% compared to administration of zidovudine alone (n = 4). Individual values ranged from a decrease of 34% to an increase of 14%. When clarithromycin tablets were administered two to four hours prior to zidovudine, the steady-state zidovudine Cmax increased by 100%, whereas the AUC was unaffected (n = 24). Administration of clarithromycin and zidovudine should be separated by at least two hours. The impact of coadministration of clarithromycin extended-release tablets and zidovudine has not been evaluated.
Didanosine: Simultaneous administration of clarithromycin tablets and didanosine to 12 HIV-infected adult patients resulted in no statistically significant change in didanosine pharmacokinetics.
Fluconazole: Following administration of fluconazole 200 mg daily and clarithromycin 500 mg twice daily to 21 healthy volunteers, the steady-state clarithromycin Cmin and AUC increased 33% and 18%, respectively. Steady-state concentrations of 14-OH clarithromycin were not significantly affected by concomitant administration of fluconazole. No dosage adjustment of clarithromycin is necessary when coadministered with fluconazole.
Ritonavir: Concomitant administration of clarithromycin and ritonavir (n = 22) resulted in a 77% increase in clarithromycin AUC and a 100% decrease in the AUC of 14-OH clarithromycin. Clarithromycin may be administered without dosage adjustment to patients with normal renal function taking ritonavir. Since concentrations of 14-OH clarithromycin are significantly reduced when clarithromycin is coadministered with ritonavir, alternative antibacterial therapy should be considered for indications other than infections due to Mycobacterium avium complex. Doses of clarithromycin greater than 1000 mg/day should not be coadministered with protease inhibitors.
Oral Anticoagulants: Spontaneous reports in the postmarketing period suggest that concomitant administration of clarithromycin and oral anticoagulants may potentiate the effects of the oral anticoagulants. Prothrombin times should be carefully monitored while patients are receiving clarithromycin and oral anticoagulants simultaneously.
Digoxin: Digoxin is a substrate for P-glycoprotein (Pgp) and clarithromycin is known to inhibit Pgp. When clarithromycin and digoxin are coadministered, inhibition of Pgp by clarithromycin may lead to increased exposure of digoxin. Elevated digoxin serum concentrations in patients receiving clarithromycin and digoxin concomitantly have been reported in postmarketing surveillance. Some patients have shown clinical signs consistent with digoxin toxicity, including potentially fatal arrhythmias. Monitoring of serum digoxin concentrations should be considered, especially for patients with digoxin concentrations in the upper therapeutic range.
CYP3A enzyme substrates: Coadministration of clarithromycin, known to inhibit CYP3A, and a drug primarily metabolized by CYP3A may be associated with elevations in drug concentrations that could increase or prolong both therapeutic and adverse effects of the concomitant drug.
Clarithromycin should be used with caution in patients receiving treatment with other drugs known to be CYP3A enzyme substrates, especially if the CYP3A substrate has a narrow safety margin (e.g., carbamazepine) and/or the substrate is extensively metabolized by this enzyme. Dosage adjustments may be considered, and when possible, serum concentrations of drugs primarily metabolized by CYP3A should be monitored closely in patients concurrently receiving clarithromycin.
The following are examples of some clinically significant CYP3A based drug interactions. Interactions with other drugs metabolized by the CYP3A isoform are also possible.
Carbamazepine and Terfenadine: Increased serum concentrations of carbamazepine and the active acid metabolite of terfenadine were observed in clinical trials with clarithromycin.
Colchicine: Colchicine is a substrate for both CYP3A and the efflux transporter, P-glycoprotein (Pgp). Clarithromycin and other macrolides are known to inhibit CYP3A and Pgp. When a single dose of colchicine 0.6 mg was administered with clarithromycin 250 mg twice daily for seven days, the colchicine Cmax increased 197% and the AUC0-‚ąě increased 239% compared to administration of colchicine alone. The dose of colchicine should be reduced when coadministered with clarithromycin in patients with normal renal and hepatic function. Concomitant use of clarithromycin and colchicine is contraindicated in patients with renal or hepatic impairment (see WARNINGS).
Efavirenz, Nevirapine, Rifampicin, Rifabutin, and Rifapentine: Inducers of CYP3A enzymes, such as efavirenz, nevirapine, rifampicin, rifabutin, and rifapentine will increase the metabolism of clarithromycin, thus decreasing plasma concentrations of clarithromycin, while increasing those of 14-OH clarithromycin. Since the microbiological activities of clarithromycin and 14-OH clarithromycin are different for different bacteria, the intended therapeutic effect could be impaired during concomitant administration of clarithromycin and enzyme inducers. Alternative antibacterial treatment should be considered when treating patients receiving inducers of CYP3A.
Sildenafil, Tadalafil, and Vardenafil: Each of these phosphodiesterase inhibitors is primarily metabolized by CYP3A, and CYP3A will be inhibited by concomitant administration of clarithromycin. Coadministration of clarithromycin with sildenafil, tadalafil, or vardenafil will result in increased exposure of these phosphodiesterase inhibitors. Coadministration of these phosphodiesterase inhibitors with clarithromycin is not recommended.
Tolterodine: The primary route of metabolism for tolterodine is via CYP2D6. However, in a subset of the population devoid of CYP2D6, the identified pathway of metabolism is via CYP3A. In this population subset, inhibition of CYP3A results in significantly higher serum concentrations of tolterodine. Tolterodine 1 mg twice daily is recommended in patients deficient in CYP2D6 activity (poor metabolizers) when coadministered with clarithromycin.
Triazolobenzodiazepines (e.g., alprazolam, midazolam, triazolam): When a single dose of midazolam was coadministered with clarithromycin tablets (500 mg twice daily for seven days), midazolam AUC increased 174% after intravenous administration of midazolam and 600% after oral administration. When oral midazolam is coadministered with clarithromycin, dose adjustments may be necessary and possible prolongation and intensity of effect should be anticipated. Caution and appropriate dose adjustments should be considered when triazolam or alprazolam is coadministered with clarithromycin. For benzodiazepines which are not metabolized by CYP3A (e.g., temazepam, nitrazepam, lorazepam), a clinically important interaction with clarithromycin is unlikely.
There have been postmarketing reports of drug interactions and central nervous system (CNS) effects (e.g., somnolence and confusion) with the concomitant use of clarithromycin and triazolam. Monitoring the patient for increased CNS pharmacological effects is suggested.
Atazanavir: Both clarithromycin and atazanavir are substrates and inhibitors of CYP3A, and there is evidence of a bi-directional drug interaction. Following administration of clarithromycin (500 mg twice daily) with atazanavir (400 mg once daily), the clarithromycin AUC increased 94%, the 14-OH clarithromycin AUC decreased 70% and the atazanavir AUC increased 28%. When clarithromycin is coadministered with atazanavir, the dose of clarithromycin should be decreased by 50%. Since concentrations of 14-OH clarithromycin are significantly reduced when clarithromycin is coadministered with atazanavir, alternative antibacterial therapy should be considered for indications other than infections due to Mycobacterium avium complex. Doses of clarithromycin greater than 1000 mg/day should not be coadministered with protease inhibitors.
Itraconazole: Both clarithromycin and itraconazole are substrates and inhibitors of CYP3A, potentially leading to a bi-directional drug interaction when administered concomitantly. Clarithromycin may increase the plasma concentrations of itraconazole, while itraconazole may increase the plasma concentrations of clarithromycin. Patients taking itraconazole and clarithromycin concomitantly should be monitored closely for signs or symptoms of increased or prolonged adverse reactions.
Saquinavir: Both clarithromycin and saquinavir are substrates and inhibitors of CYP3A and there is evidence of a bi-directional drug interaction. Following administration of clarithromycin (500 mg twice daily) and saquinavir (soft gelatin capsules, 1200 mg three times daily) to 12 healthy volunteers, the steady-state saquinavir AUC and Cmax increased 177% and 187% respectively compared to administration of saquinavir alone. Clarithromycin AUC and Cmax increased 45% and 39% respectively, whereas the 14-OH clarithromycin AUC and Cmax decreased 24% and 34% respectively, compared to administration with clarithromycin alone. No dose adjustment of clarithromycin is necessary when clarithromycin is coadministered with saquinavir in patients with normal renal function. When saquinavir is coadministered with ritonavir, consideration should be given to the potential effects of ritonavir on clarithromycin (refer to interaction between clarithromycin and ritonavir) (see PRECAUTIONS, Drug Interactions).
The following CYP3A based drug interactions have been observed with erythromycin products and/or with clarithromycin in postmarketing experience:
Antiarrhythmics: There have been postmarketing reports of torsades de pointes occurring with concurrent use of clarithromycin and quinidine or disopyramide. Electrocardiograms should be monitored for QTc prolongation during coadministration of clarithromycin with these drugs. Serum concentrations of these medications should also be monitored.
Ergotamine/Dihydroergotamine: Postmarketing reports indicate that coadministration of clarithromycin with ergotamine or dihydroergotamine has been associated with acute ergot toxicity characterized by vasospasm and ischemia of the extremities and other tissues including the central nervous system. Concomitant administration of clarithromycin with ergotamine or dihydroergotamine is contraindicated (see CONTRAINDICATIONS).
Triazolobenziodidiazepines (such as triazolam and alprazolam) and Related Benzodiazepines (such as midazolam): Erythromycin has been reported to decrease the clearance of triazolam and midazolam, and thus, may increase the pharmacologic effect of these benzodiazepines. There have been postmarketing reports of drug interactions and CNS effects (e.g., somnolence and confusion) with the concomitant use of clarithromycin and triazolam.
Sildenafil (Viagra): Erythromycin has been reported to increase the systemic exposure (AUC) of sildenafil. A similar interaction may occur with clarithromycin; reduction of sildenafil dosage should be considered (see Viagra package insert).
There have been spontaneous or published reports of CYP3A based interactions of erythromycin and/or clarithromycin with cyclosporine, carbamazepine, tacrolimus, alfentanil, disopyramide, rifabutin, quinidine, methylprednisolone, cilostazol, bromocriptine and vinblastine.
Concomitant administration of clarithromycin with cisapride, pimozide, astemizole, or terfenadine is contraindicated (see CONTRAINDICATIONS).
In addition, there have been reports of interactions of erythromycin or clarithromycin with drugs not thought to be metabolized by CYP3A, including hexobarbital, phenytoin, and valproate.
Drug/Laboratory Test Interactions
High urine concentrations of ampicillin may result in false-positive reactions when testing for the presence of glucose in urine using CLINITEST, Benedict’s Solution or Fehling’s Solution. Since this effect may also occur with amoxicillin, it is recommended that glucose tests based on enzymatic glucose oxidase reactions (such as CLINISTIX) be used.
Following administration of ampicillin to pregnant women, a transient decrease in plasma concentration of total conjugated estriol, estriol-glucuronide, conjugated estrone, and estradiol has been noted. This effect may also occur with amoxicillin.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Lansoprazole
In two 24-month carcinogenicity studies, Sprague-Dawley rats were treated with oral lansoprazole at doses of 5 to 150 mg/kg/day, about 0.5 to 20 times the recommended human dose of 60 mg/day, based on body surface area (BSA). Lansoprazole produced dose-related gastric enterochromaffin-like (ECL) cell hyperplasia and ECL cell carcinoids in both male and female rats. The incidences of intestinal metaplasia of the gastric epithelium were also increased in both sexes. In male rats, lansoprazole produced a dose-related increase in the incidence of testicular interstitial cell adenomas at doses two to 20 times the recommended human dose of 60 mg/day based on BSA.
In a 24-month carcinogenicity study, CD-1 mice were treated with oral lansoprazole at doses of 15 to 600 mg/kg/day (one to 40 times the recommended human dose of 60 mg/day based on BSA comparisons). Lansoprazole produced a dose-related increased incidence of gastric ECL cell hyperplasia. The incidence of liver tumors (hepatocellular adenoma plus carcinoma) was increased in male mice (at doses 20 to 40 times the recommended human dose of 60 mg/day based on BSA) and in female mice (treated at doses ten to 40 times the recommended human dose based on BSA). Lansoprazole treatment produced adenoma of rete testis in male mice receiving doses five to 40 times the recommended human dose of 60 mg/day based on BSA.
A 26 week p53 (+/-) transgenic mouse carcinogenicity study was not positive.
Lansoprazole was positive in the Ames test and the in vitro human lymphocyte chromosomal aberration assay. Lansoprazole was not genotoxic in the ex vivo rat hepatocyte unscheduled DNA synthesis (UDS) test, the in vivo mouse micronucleus test, or the rat bone marrow cell chromosomal aberration test.
Lansoprazole at oral doses up to 150 mg/kg/day (20 times the recommended human dose of 60 mg/day based on BSA) was found to have no effect on fertility and reproductive performance of male and female rats.
Amoxicillin
Long-term studies in animals have not been performed to evaluate the mutagenic or carcinogenic potential of amoxicillin alone. A 4:1 mixture of amoxicillin and potassium clavulanate was non-mutagenic in the Ames bacterial mutation assay, and the yeast gene conversion assay. The amoxicillin/potassium clavulanate mixture was also negative in the mouse micronucleus test, and in the dominant lethal assay in mice, but was weakly positive in the mouse lymphoma assay. In a multi-generation reproduction study in rats, no impairment of fertility or other adverse reproductive effects were seen at doses up to 500 mg/kg, approximately three times the human dose based on BSA comparisons.
Clarithromycin
The following in vitro mutagenicity tests have been conducted with clarithromycin:
  Salmonella/Mammalian Microsomes Test  Bacterial Induced Mutation Frequency Test  In Vitro Chromosome Aberration Test  Rat Hepatocyte DNA Synthesis Assay  Mouse Lymphoma Assay  Mouse Dominant Lethal Study  Mouse Micronucleus Test
All tests had negative results except the In Vitro Chromosome Aberration Test which was weakly positive in one test and negative in another.
In addition, a Bacterial Reverse-Mutation Test (Ames Test) has been performed on clarithromycin metabolites with negative results.
Fertility and reproduction studies have shown that daily doses of up to 160 mg/kg/day
(1.3 times the recommended maximum human dose based on mg/m2) to male and female rats caused no adverse effects on the estrous cycle, fertility, parturition, or number and viability of offspring. Plasma levels in rats after 150 mg/kg/day were two times the human serum levels.
In the 150 mg/kg/day monkey studies, plasma levels were three times the human serum levels. When given orally at 150 mg/kg/day (2.4 times the recommended maximum human dose based on mg/m2), clarithromycin was shown to produce embryonic loss in monkeys. This effect has been attributed to marked maternal toxicity of the drug at this high dose.
In rabbits, in utero fetal loss occurred at an intravenous dose of 33 mg/m2, which is 17 times less than the maximum proposed human oral daily dose of 618 mg/m2.
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of clarithromycin.
Pregnancy
Teratogenic Effects
Pregnancy Category C
Category C is based on the pregnancy category for clarithromycin.
There are no adequate and well-controlled studies of lansoprazole, clarithromycin or amoxicillin (used separately or together) in pregnant women. Lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus and there is no appropriate alternative therapy (see WARNINGS).
Reproduction studies have been performed in pregnant rats at oral lansoprazole doses up to 20 times the recommended human dose (60 mg/day based on BSA) and in pregnant rabbits at oral doses up to eight times the recommended human dose (60 mg/day based on BSA) and have revealed no evidence of impaired fertility or harm to the fetus due to lansoprazole.
Reproduction studies with amoxicillin have been performed in mice and rats at doses up to ten times the human dose and revealed no evidence of impaired fertility or harm to the fetus.
Four teratogenicity studies in rats with clarithromycin (three with oral doses and one with intravenous doses up to 160 mg/kg/day administered during the period of major organogenesis) and two in rabbits at oral doses up to 125 mg/kg/day (approximately two times the recommended maximum human dose based on mg/m2) or intravenous doses of 30 mg/kg/day administered during gestation days six to 18 failed to demonstrate any teratogenicity from clarithromycin. Two additional oral studies in a different rat strain at similar doses and similar conditions demonstrated a low incidence of cardiovascular anomalies at doses of 150 mg/kg/day administered during gestation days six to 15. Plasma levels after 150 mg/kg/day were two times the human serum levels. Four studies in mice revealed a variable incidence of cleft palate following oral doses of 1000 mg/kg/day (two and four times the recommended maximum human dose based on mg/m2, respectively) during gestation days six to 15. Cleft palate was also seen at 500 mg/kg/day. The 1000 mg/kg/day exposure resulted in plasma levels 17 times the human serum levels. In monkeys, an oral dose of 70 mg/kg/day (an approximate equidose of the recommended maximum human dose based on mg/m2) produced fetal growth retardation at plasma levels that were two times the human serum levels.
Labor and Delivery
Oral ampicillin-class antibiotics are poorly absorbed during labor. Studies in guinea pigs showed that intravenous administration of ampicillin slightly decreased the uterine tone and frequency of contractions, but moderately increased the height and duration of contractions. However, it is not known whether use of these drugs in humans during labor or delivery has immediate or delayed adverse effects on the fetus, prolongs the duration of labor, or increases the likelihood that forceps delivery or other obstetrical intervention or resuscitation of the newborn will be necessary.
Nursing Mothers
Lansoprazole and its metabolites are excreted in the milk of rats. It is not known whether lansoprazole is excreted in human milk. Because of the potential for serious adverse reactions in nursing infants from lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets, and the potential for tumorigenicity shown for lansoprazole in rat carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets, taking into account the importance of the therapy to the mother.
Penicillins have been shown to be excreted in human milk. Amoxicillin use by nursing mothers may lead to sensitization of infants. Caution should be exercised when amoxicillin is administered to a nursing woman.
It is not known whether clarithromycin is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when clarithromycin is administered to a nursing woman. It is known that clarithromycin is excreted in the milk of lactating animals and that other drugs of this class are excreted in human milk. Preweaned rats, exposed indirectly via consumption of milk from dams treated with 150 mg/kg/day for three weeks, were not adversely affected, despite data indicating higher drug levels in milk than in plasma.
Pediatric Use
The safety and effectiveness of lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets in pediatric patients infected with H. pylori have not been established (see CONTRAINDICATIONS and WARNINGS).
Geriatric Use
Elderly patients may suffer from asymptomatic renal and hepatic dysfunction. Care should be taken when administering lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets to this patient population.
An analysis of clinical studies of amoxicillin was conducted to determine whether subjects aged 65 and over respond differently from younger subjects. Of the 1,811 subjects treated with capsules of amoxicillin, 85% were less than 60 years old, 15% were ‚Č• 61 years old and 7% were ‚Č• 71 years old. This analysis and other reported clinical experience have not identified differences in responses between the elderly and younger patients, but a greater sensitivity of some older individuals cannot be ruled out.
Amoxicillin is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
In a steady-state study in which healthy elderly subjects (age 65 to 81 years old) were given 500 mg of clarithromycin every 12 hours, the maximum serum concentrations and area under the curves of clarithromycin and 14-OH clarithromycin were increased compared to those achieved in healthy young adults. These changes in pharmacokinetics parallel known age-related decreases in renal function. In clinical trials of clarithromycin, elderly patients did not have an increased incidence of adverse events when compared to younger patients. Dosage adjustment should be considered in elderly patients with severe renal impairment. Elderly patients may be more susceptible to development of torsades de pointes arrhythmias than younger patients (see WARNINGS and PRECAUTIONS).
Adverse Reactions
Lansoprazole delayed-release capsules, amoxicillin capsules, and clarithromycin tablets
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The most common adverse reactions (‚Č• 3%) reported in clinical trials when all three components of this therapy were given concomitantly for 14 days are uled in Table 5.
Table 5: Adverse Reactions Most Frequently Reported in Clinical Trials (‚Č• 3%)
Triple Therapy
n = 138
Adverse Reaction
(%)
Diarrhea
7.0
Headache
6.0
Taste Perversion
5.0
The additional adverse reactions which were reported as possibly or probably related to treatment (less than 3%) in clinical trials when all three components of this therapy were given concomitantly are uled below and divided by body system:
Body as a Whole - abdominal pain
Digestive System - dark stools, dry mouth/thirst, glossitis, rectal itching, nausea, oral moniliasis, stomatitis, tongue discoloration, tongue disorder, vomiting
Musculoskeletal System - myalgia
Nervous System - confusion, dizziness
Respiratory System - respiratory disorders
Skin and Appendages - skin reactions
Urogenital System - vaginitis, vaginal moniliasis.
There were no statistically significant differences in the frequency of reported adverse events between the 10- and 14-day triple therapy regimens.
Lansoprazole
The following adverse reactions from the labeling for lansoprazole are provided for information:
Worldwide, over 10,000 patients have been treated with lansoprazole in Phase 2 or Phase 3 clinical trials involving various dosages and durations of treatment. In general, lansoprazole treatment has been well-tolerated in both short-term and long-term trials.
Incidence in Clinical Trials
The following adverse events were reported by the treating physician to have a possible or probable relationship to drug in 1% or more of lansoprazole-treated patients and occurred at a greater rate in lansoprazole-treated patients than placebo-treated patients:
Table 6: Incidence of Possibly or Probably Treatment-Related Adverse Reactions in Short-Term, Placebo-Controlled Lansoprazole Studies
Lansoprazole
Placebo
(N = 2768)
(N = 1023)
Body System/Adverse Event
%
%
Body as a Whole
Abdominal Pain
2.1
1.2
Digestive System
Constipation
1.0
0.4
Diarrhea
3.8
2.3
Nausea
1.3
1.2
Headache was also seen at greater than 1% incidence but was more common on placebo. The incidence of diarrhea was similar between patients who received placebo and patients who received 30 mg of lansoprazole, but higher in the patients who received 60 mg of lansoprazole (2.9%, 4.2%, and 7.4%, respectively).
The most commonly reported possibly or probably treatment-related adverse event during maintenance therapy was diarrhea.
Additional adverse experiences occurring in less than 1% of patients or subjects who received lansoprazole in domestic trials are shown below:
Body as a Whole - abdomen enlarged, allergic reaction, asthenia, back pain, candidiasis, carcinoma, chest pain (not otherwise specified), chills, edema, fever, flu syndrome, halitosis, infection (not otherwise specified), malaise, neck pain, neck rigidity, pain, pelvic pain
Cardiovascular System - angina, arrhythmia, bradycardia, cerebrovascular accident/cerebral infarction, hypertension/hypotension, migraine, myocardial infarction, palpitations, shock (circulatory failure), syncope, tachycardia, vasodilation
Digestive System - abnormal stools, anorexia, bezoar, cardiospasm, cholelithiasis, colitis, dry mouth, dyspepsia, dysphagia, enteritis, eructation, esophageal stenosis, esophageal ulcer, esophagitis, fecal discoloration, flatulence, gastric nodules/fundic gland polyps, gastritis, gastroenteritis, gastrointestinal anomaly, gastrointestinal disorder, gastrointestinal hemorrhage, glossitis, gum hemorrhage, hematemesis, increased appetite, increased salivation, melena, mouth ulceration, nausea and vomiting, nausea and vomiting and diarrhea, gastrointestinal moniliasis, rectal disorder, rectal hemorrhage, stomatitis, tenesmus, thirst, tongue disorder, ulcerative colitis, ulcerative stomatitis
Endocrine System - diabetes mellitus, goiter, hypothyroidism
Hemic and Lymphatic System - anemia, hemolysis, lymphadenopathy
Metabolism and Nutritional Disorders - avitaminosis, gout, dehydration, hyperglycemia/hypoglycemia, peripheral edema, weight gain/loss
Musculoskeletal System - arthralgia, arthritis, bone disorder, joint disorder, leg cramps, musculoskeletal pain, myalgia, myasthenia, ptosis, synovitis
Nervous System - abnormal dreams, agitation, amnesia, anxiety, apathy, confusion, convulsion, dementia, depersonalization, depression, diplopia, dizziness, emotional lability, hallucinations, hemiplegia, hostility aggravated, hyperkinesia, hypertonia, hypesthesia, insomnia, libido decreased/increased, nervousness, neurosis, paresthesia, sleep disorder, somnolence, thinking abnormality, tremor, vertigo
Respiratory System - asthma, bronchitis, cough increased, dyspnea, epistaxis, hemoptysis, hiccup, laryngeal neoplasia, lung fibrosis, pharyngitis, pleural disorder, pneumonia, respiratory disorder, upper respiratory inflammation/infection, rhinitis, sinusitis, stridor
Skin and Appendages - acne, alopecia, contact dermatitis, dry skin, fixed eruption, hair disorder, maculopapular rash, nail disorder, pruritus, rash, skin carcinoma, skin disorder, sweating, urticaria
Special Senses - abnormal vision, amblyopia, blepharitis, blurred vision, cataract, conjunctivitis, deafness, dry eyes, ear/eye disorder, eye pain, glaucoma, otitis media, parosmia, photophobia, retinal degeneration/disorder, taste loss, taste perversion, tinnitus, visual field defect
Urogenital System - abnormal menses, breast enlargement, breast pain, breast tenderness, dysmenorrhea, dysuria, gynecomastia, impotence, kidney calculus, kidney pain, leukorrhea, menorrhagia, menstrual disorder, penis disorder, polyuria, testis disorder, urethral pain, urinary frequency, urinary retention, urinary tract infection, urinary urgency, urination impaired, vaginitis.
Postmarketing
Additional adverse experiences have been reported since lansoprazole has been marketed. The majority of these cases are foreign-sourced and a relationship to lansoprazole has not been established. Because these events were reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events are uled below by COSTART body system:
Body as a Whole - anaphylactic/anaphylactoid reactions
Digestive System - hepatotoxicity, pancreatitis, vomiting
Hemic and Lymphatic System - agranulocytosis, aplastic anemia, hemolytic anemia, leukopenia, neutropenia, pancytopenia, thrombocytopenia, and thrombotic thrombocytopenic purpura
Infections and infestations ‚Äď Clostridium difficile associated diarrhea
Metabolism and Nutritional Disorders ‚Äď hypomagnesemia
Musculoskeletal System - bone fracture, myositis
Skin and Appendages - severe dermatologic reactions including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, (some fatal)
Special Senses - speech disorder
Urogenital System - interstitial nephritis, urinary retention
Amoxicillin
The following adverse reactions from the labeling for amoxicillin are provided for information:
As with other penicillins, it may be expected that untoward reactions will be essentially limited to sensitivity phenomena. They are more likely to occur in individuals who have previously demonstrated hypersensitivity to penicillins and in those with a history of allergy, asthma, hay fever, or urticaria. The following adverse reactions have been reported as associated with the use of penicillins:
Infections and Infestations ‚Äď Mucocutaneous candidiasis
Gastrointestinal - Nausea, vomiting, diarrhea, black hairy tongue, and hemorrhagic/pseudomembranous colitis.
Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see WARNINGS).
Hypersensitivity Reactions ‚Äď Anaphylaxis (see WARNINGS), serum sickness-like reactions, erythematous maculopapular rashes, erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, toxic epidermal necrolysis, acute generalized exanthematous pustulosis, hypersensitivity vasculitis and urticaria have been reported.
Liver ‚Äď A moderate rise in AST (SGOT) and/or ALT (SGPT) has been noted, but the significance of this finding is unknown. Hepatic dysfunction including cholestatic jaundice, hepatic cholestasis and acute cytolytic hepatitis have been reported.
Renal ‚Äď Crystalluria has also been reported (see OVERDOSAGE).
Hemic and Lymphatic Systems ‚Äď Anemia, including hemolytic anemia, thrombocytopenia, thrombocytopenic purpura, eosinophilia, leukopenia and agranulocytosis have been reported during therapy with penicillins. These reactions are usually reversible on discontinuation of therapy and are believed to be hypersensitivity phenomena.
Central Nervous System ‚Äď Reversible hyperactivity, agitation, anxiety, insomnia, confusion, behavioral changes, and/or dizziness have been reported rarely.
Miscellaneous ‚Äď Tooth discoloration (brown, yellow, or gray staining) has been rarely reported. Most reports occurred in pediatric patients. Discoloration was reduced or eliminated with brushing or dental cleaning in most cases.
Clarithromycin
The following adverse reactions from the labeling for clarithromycin are provided for information:
The majority of adverse reactions observed in clinical trials were of a mild and transient nature. Fewer than 3% of adult patients without mycobacterial infections discontinued therapy because of drug-related side effects.
The most frequently reported events in adults were diarrhea (3%), nausea (3%), abnormal taste (3%), dyspepsia (2%), abdominal pain/discomfort (2%), and headache (2%). Most of these events were described as mild or moderate in severity. Of the reported adverse events, only 1% was described as severe.
The following postmarketing adverse reactions from the labeling for clarithromycin are provided for information:
Allergic reactions ranging from urticaria and mild skin eruptions to cases of anaphylaxis, Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms (DRESS), Henoch-Schonlein Purpura and toxic epidermal necrolysis have occurred. Other spontaneously reported adverse reactions include glossitis, stomatitis, oral moniliasis, anorexia, vomiting, pancreatitis, tongue discoloration, thrombocytopenia, leukopenia, neutropenia, dizziness, myalgia and hemorrhage. There have been reports of tooth discoloration in patients treated with clarithromycin. Tooth discoloration is usually reversible with professional dental cleaning. There have been isolated reports of hearing loss, which is usually reversible, occurring chiefly in elderly women. Reports of alterations of the sense of smell including smell loss, usually in conjunction with taste perversion or taste loss have also been reported.
Transient CNS events including anxiety, behavioral changes, confusional states, convulsions, depersonalization, disorientation, hallucinations, insomnia, depression, manic behavior, nightmares, psychosis, tinnitus, tremor, and vertigo have been reported during postmarketing surveillance. Events usually resolve with discontinuation of the drug.
Adverse reactions related to hepatic dysfunction have been reported in postmarketing experience with clarithromycin (see WARNINGS, Hepatotoxicity).
There have been rare reports of hypoglycemia, some of which have occurred in patients taking oral hypoglycemic agents or insulin.
As with other macrolides, clarithromycin has been associated with QT prolongation and ventricular arrhythmias, including ventricular tachycardia and torsades de pointes.
There have been reports of interstitial nephritis coincident with clarithromycin use.
There have been postmarketing reports of colchicine toxicity with concomitant use of clarithromycin and colchicine, especially in the elderly, some of which occurred in patients with renal insufficiency. Deaths have been reported in some such patients (see WARNINGS and PRECAUTIONS).
There have been cases of rhabdomyolysis reported with clarithromycin use. In some cases, clarithromycin was administered concomitantly with other drugs known to be associated with rhabdomyolysis (such as statins, fibrates, colchicine or allopurinol).
Laboratory Values
Lansoprazole
The following changes in laboratory parameters in patients who received lansoprazole were reported as adverse reactions:
Abnormal liver function tests, increased SGOT (AST), increased SGPT (ALT), increased creatinine, increased alkaline phosphatase, increased globulins, increased GGTP, increased/decreased/abnormal WBC, abnormal AG ratio, abnormal RBC, bilirubinemia, blood potassium increased, blood urea increased, crystal urine present, eosinophilia, hemoglobin decreased, hyperlipemia, increased/decreased electrolytes, increased/decreased cholesterol, increased glucocorticoids, increased LDH, increased/decreased/abnormal platelets, increased gastrin levels and positive fecal occult blood. Urine abnormalities such as albuminuria, glycosuria, and hematuria were also reported.
In the placebo-controlled studies, when SGOT (AST) and SGPT (ALT) were evaluated, 0.4% (4/978) and 0.4% (11/2677) patients, who received placebo and lansoprazole, respectively, had enzyme elevations greater than three times the upper limit of normal range at the final treatment visit. None of these patients who received lansoprazole reported jaundice at any time during the study.
Clarithromycin
Changes in laboratory values due to clarithromycin with possible clinical significance were as follows:
Hepatic ‚Äď elevated SGPT (ALT) < 1%, SGOT (AST) < 1%, GGT < 1%, alkaline phosphatase < 1%, LDH < 1%, total bilirubin < 1%
Hematologic ‚Äď decreased WBC < 1%, elevated prothrombin time 1%
Renal ‚Äď elevated BUN 4%, elevated serum creatinine < 1%
GGT, alkaline phosphatase, and prothrombin time data are from adult studies only.
Overdosage
In case of an overdose, patients should contact a physician, poison control center, or emergency room. There is neither a pharmacologic basis nor data suggesting an increased toxicity of the combination compared to individual components.
Amoxicillin
In case of amoxicillin overdosage, discontinue medication, treat symptomatically and institute supportive measures as needed. If the overdosage is very recent and there is no contraindication, an attempt at emesis or other means of removal of drug from the stomach may be performed. A prospective study of 51 pediatric patients at a poison-control center suggested that overdosages of less than 250 mg/kg of amoxicillin are not associated with significant clinical symptoms and do not require gastric emptying.2
Interstitial nephritis resulting in oliguric renal failure has been reported in a small number of patients after overdosage with amoxicillin.
Crystalluria, in some cases leading to renal failure, has also been reported after amoxicillin overdosage in adult and pediatric patients. In case of overdosage, adequate fluid intake and diuresis should be maintained to reduce the risk of amoxicillin crystalluria. Renal impairment appears to be reversible with cessation of drug administration. High blood levels may occur more readily in patients with impaired renal function because of decreased renal clearance of amoxicillin. Amoxicillin can be removed from circulation by hemodialysis.
Clarithromycin
Overdosage of clarithromycin can cause gastrointestinal symptoms such as abdominal pain, vomiting, nausea, and diarrhea.
Adverse reactions accompanying overdosage should be treated by the prompt elimination of unabsorbed drug and supportive measures. As with other macrolides, clarithromycin serum concentrations are not expected to be appreciably affected by hemodialysis or peritoneal dialysis.
Lansoprazole
Lansoprazole is not removed from the circulation by hemodialysis. In one reported overdose, a patient consumed 600 mg of lansoprazole with no adverse reaction. Oral lansoprazole doses up to 5000 mg/kg in rats (approximately 650 times the recommended human dose of 60 mg/day based on BSA) and in mice (about 338 times the recommended human dose of 60 mg/day based on BSA) did not produce deaths or any clinical signs.
Dosage And Administration
Eradication to Reduce the Risk of Duodenal Ulcer Recurrence
The recommended adult oral dose is 30 mg lansoprazole, 1 g amoxicillin, and 500 mg clarithromycin administered together twice daily (morning and evening) for 10 or 14 days (see INDICATIONS AND USAGE).
Lansoprazole delayed-release capsules USP, 30 mg, amoxicillin capsules USP, 500 mg, and clarithromycin tablets USP, 500 mg are not recommended in patients with creatinine clearance less than 30 mL/min.
How Supplied
Lansoprazole Delayed-Release Capsules USP, 30 mg, Amoxicillin Capsules USP, 500 mg, and Clarithromycin Tablets USP, 500 mg are supplied in boxes of 14 daily administration cards, each card containing:
Lansoprazole Delayed-Release Capsules, USP
Two hard gelatin 30 mg-capsules, with a light-gray opaque cap and flesh-colored opaque body, filled with off-white to beige pellets, imprinted with ‚Äú93‚ÄĚ and ‚Äú7351‚ÄĚ.
Amoxicillin Capsules, USP
Four buff-colored 500 mg-capsules, imprinted ‚ÄúTEVA‚ÄĚ on the cap and ‚Äú3109‚ÄĚ on the body.
Clarithromycin Tablets, USP
Two light-yellow, oval-shaped, film-coated 500 mg-tablets, debossed with ‚Äú93‚ÄĚ on one side and ‚Äú7158‚ÄĚ on the other side.
NDC 0093-8055-14 Carton containing 14 daily administration cards
NDC 0093-8055-78 Daily administration card
Store at 20¬į to 25¬įC (68¬į to 77¬įF) [See USP Controlled Room Temperature]. Protect from light and moisture.
Reference
1. CLSI. Methods for Antimicrobial Dilution and Disk Diffusion Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria ‚Äď 2nd edition. CLSI document M45-A2, 2010.2. Swanson Biearman B, Dean BS, Lopez G, Krenzelok EP. The effects of penicillin and cephalosporin ingestions in children less than six years of age. Vet Hum Toxicol. 1988; 30:66-67.
All brand names uled are the registered trademarks of their respective owners and are not trademarks of Teva Pharmaceuticals USA, Inc.
Lansoprazole Delayed-Release Capsules USP and Clarithromycin Tablets USP Are Manufactured In Israel By:
TEVA PHARMACEUTICAL IND . LTD .
Jerusalem, 91010, Israel
Amoxicillin Capsules USP Are Manufactured In Canada By:
TEVA CANADA LIMITED
Toronto, Canada M1B 2K9
Manufactured For:
TEVA PHARMACEUTICALS USA
Sellersville, PA 18960
Rev. E 1/2015
Package/label Display Panel, Part 1 Of 2
Package/label Display Panel, Part 2 0f 2
![]()
Triple Therapy Lansoprazole Delayed-Release Capsules USP, 30 mg, Amoxicillin Capsules USP, 500 mg, and Clarithromycin Tablets USP, 500 mg; 14s Carton Text
NDC 0093-8055-14
triple therapy LANSOPRAZOLE Delayed-Release Capsules USP, 30 mg, AMOXICILLIN Capsules USP, 500 mg, and CLARITHROMYCIN Tablets USP, 500 mg
14 DAILY PATIENT CARDS
EACH DAILY PATIENT CARD CONTAINS:
2 LANSOPRAZOLE Delayed-Release Capsules USP, 30 mg;
4 AMOXICILLIN Capsules USP, 500 mg; and
2 CLARITHROMYCIN Tablets USP, 500 mg
Clarithromycin tablets USP contain FD&C Yellow No. 5 (tartrazine) as a color additive.
Rx only
14 DAILY PATIENT CARDS
TEVA
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site