Prednisone (prednisone 1 mg) Dailymed
Generic: prednisone is used for the treatment of Adrenal Insufficiency Anemia, Hemolytic, Autoimmune Arthritis, Rheumatoid Asthma Berylliosis Bursitis Chickenpox Colitis, Ulcerative Collagen Diseases Conjunctivitis, Allergic Dermatitis Herpetiformis Dermatitis, Atopic Dermatitis, Contact Dermatomyositis Erythema Multiforme Graft vs Host Disease Hypercalcemia Infections Inflammation Iritis Leukemia Lupus Erythematosus, Systemic Lymphoma Multiple Sclerosis Mycoses Nephrotic Syndrome Neuralgia Pemphigus Rheumatic Diseases Sarcoidosis Dermatitis, Seborrheic Serum Sickness Spondylitis, Ankylosing Synovitis Thyroiditis Tuberculosis, Pulmonary Arthritis, Gouty Arthritis, Psoriatic Purpura, Thrombocytopenic, Idiopathic Rhinitis, Allergic
IMPRINT: 50 93 V
SHAPE: round
COLOR: white SCORE: 2
All Imprints
prednisone 20 mg - 50 92 50 92 v round orange
prednisone 10 mg - v 50 93 50 93 v round white
prednisone 10 mg oral tablet - 5093 v round white
prednisone 20 mg oral tablet - 50 92 v round orange
prednisone 10 mg - 50 93 v round white
prednisone 20 mg oral tablet - v 50 92 round orange
prednisone 10 mg - v 50 93 round white
prednisone 5 mg - 5094 v round white
prednisone 20 mg - 5092 v round orange
prednisone 10 mg - 5093 v round white
prednisone 2.5 mg - 5085 v round white
prednisone 1 mg - 5084 v round white
Go PRO for all pill images
Description
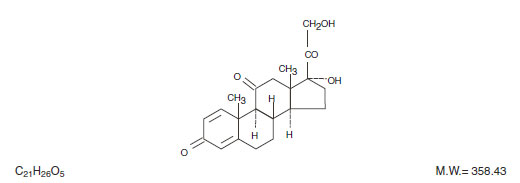
PredniSONE Tablets contain prednisone which is a glucocorticoid. Glucocorticoids are adrenocortical steroids, both naturally occurring and synthetic, which are readily absorbed from the gastrointestinal tract. Prednisone is a white to practically white, odorless, crystalline powder. It is very slightly soluble in water; slightly soluble in alcohol, chloroform, dioxane, and methanol.
The chemical name for prednisone is pregna-1,4-diene-3,11,20-trione monohydrate,17,21-dihydroxy-. The structural formula is represented below:
PredniSONE Tablets are available in 5 strengths: 1 mg, 2.5 mg, 5 mg, 10 mg and 20 mg.
INACTIVE INGREDIENT SECTION
Inactive ingredients: 1 mg — colloidal silicon dioxide, lactose monohydrate, magnesium stearate, pregelatinized starch, sodium starch glycolate; 2.5 mg — colloidal silicon dioxide, lactose monohydrate, magnesium stearate, pregelatinized starch, sodium starch glycolate; 5 mg — colloidal silicon dioxide, lactose monohydrate, magnesium stearate, pregelatinized starch, sodium starch glycolate; 10 mg — colloidal silicon dioxide, lactose monohydrate, magnesium stearate, pregelatinized starch, sodium starch glycolate; 20 mg — FD&C Yellow #6 Lake, lactose monohydrate, magnesium stearate, microcrystalline cellulose, sodium starch glycolate.
Clinical Pharmacology
Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their potent anti-inflammatory effects in disorders of many organ systems.
Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli.
Indications And Usage
PredniSONE Tablets are indicated in the following conditions:
1. Endocrine Disorders
Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation is of particular importance)
Congenital adrenal hyperplasia
Hypercalcemia associated with cancer
Nonsuppurative thyroiditis
2. Rheumatic Disorders
As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in:
Psoriatic arthritis
Rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy)
Ankylosing spondylitis
Acute and subacute bursitis
Acute nonspecific tenosynovitis
Acute gouty arthritis
Post-traumatic osteoarthritis
Synovitis of osteoarthritis
Epicondylitis
3. Collagen Diseases
During an exacerbation or as maintenance therapy in selected cases of:
Systemic lupus erythematosus
Systemic dermatomyositis (polymyositis)
Acute rheumatic carditis
4. Dermatologic Diseases
Pemphigus
Bullous dermatitis herpetiformis
Severe erythema multiforme (Stevens-Johnson syndrome)
Exfoliative dermatitis
Mycosis fungoides
Severe psoriasis
Severe seborrheic dermatitis
5. Allergic States
Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional
treatment:
Seasonal or perennial allergic rhinitis
Bronchial asthma
Contact dermatitis
Atopic dermatitis
Serum sickness
Drug hypersensitivity reactions
6. Ophthalmic Diseases
Severe acute and chronic allergic and inflammatory processes involving the eye and its adnexa such as:
Allergic corneal marginal ulcers
Herpes zoster ophthalmicus
Anterior segment inflammation
Diffuse posterior uveitis and choroiditis
Sympathetic ophthalmia
Allergic conjunctivitis
Keratitis
Chorioretinitis
Optic neuritis
Iritis and iridocyclitis
7. Respiratory Diseases
Symptomatic sarcoidosis
Loeffler’s syndrome not manageable by other means
Berylliosis
Fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy
Aspiration pneumonitis
8. Hematologic Disorders
Idiopathic thrombocytopenic purpura in adults
Secondary thrombocytopenia in adults
Acquired (autoimmune) hemolytic anemia
Erythroblastopenia (RBC anemia)
Congenital (erythroid) hypoplastic anemia
9. Neoplastic Diseases
For palliative management of:
Leukemias and lymphomas in adults
Acute leukemia of childhood
10. Edematous States
To induce a diuresis or remission of proteinuria in the nephrotic syndrome, without uremia, of the
idiopathic type or that due to lupus erythematosus
11. Gastrointestinal Diseases
To tide the patient over a critical period of the disease in:
Ulcerative colitis
Regional enteritis
12. Miscellaneous
Tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy.
Trichinosis with neurologic or myocardial involvement
Contraindications
Prednisone tablets are contraindicated in systemic fungal infections and known hypersensitivity to components.
Warnings
General
Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy (see ADVERSE REACTIONS: Allergic Reactions).
Increased dosage of rapidly acting corticosteroids is indicated in patients on corticosteroid therapy subjected to any unusual stress before, during and after the stressful situation.
Cardio-Renal
Average and large doses of hydrocortisone or cortisone can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion. Literature reports suggest an apparent association between use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
Endocrine
Corticosteroids can produce reversible hypothalamic-pituitary adrenal (HPA) axis suppression with the potential for corticosteroid insufficiency after withdrawal of treatment. Adrenocortical insufficiency may result from too rapid withdrawal of corticosteroids and may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for up to 12 months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted. If the patient is receiving steroids already, dosage may have to be increased.
Metabolic clearance of corticosteroids is decreased in hypothyroid patients and increased in hyperthyroid patients. Changes in thyroid status of the patient may necessitate adjustment in dosage.
Immunosuppression and Increased Risk of Infection
Corticosteroids, including prednisone tablets, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
• Reduce resistance to new infections
• Exacerbate existing infections
• Increase the risk of disseminated infections
• Increase the risk of reactivation or exacerbation of latent infections
• Mask some signs of infection
Corticosteroid-associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
Monitor for the development of infection and consider prednisone tablets withdrawal or dosage reduction as needed.
Do not administer prednisone tablets by an intraarticular, intrabursal, intratendinous, or intralesional route in the presence of acute local infection.
Tuberculosis
If prednisone tablets is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of tuberculosis may occur. Closely monitor such patients for reactivation. During prolonged prednisone tablets therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella Zoster and Measles Viral Infections
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including prednisone tablets. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
• If a prednisone tablets-treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin may be indicated. If varicella develops, treatment with antiviral agents may be considered.
• If a prednisone tablets-treated patient is exposed to measles, prophylaxis with immunoglobulin may be indicated.
Hepatitis B Virus Reactivation
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including prednisone tablets. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with prednisone tablets. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Fungal Infections
Corticosteroids, including prednisone tablets, may exacerbate systemic fungal infections; therefore, avoid prednisone tablets use in the presence of such infections unless prednisone tablets is needed to control drug reactions. For patients on chronic prednisone tablets therapy who develop systemic fungal infections, prednisone tablets withdrawal or dosage reduction is recommended.
Amebiasis
Corticosteroids, including prednisone tablets, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating prednisone tablets in patients who have spent time in the tropics or patients with unexplained diarrhea.
Strongyloides Infestation
Corticosteroids, including prednisone tablets, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gramnegative septicemia.
Cerebral Malaria
Avoid corticosteroids, including prednisone tablets, in patients with cerebral malaria.
Vaccination
Administration of live or live, attenuated vaccines is contraindicated in patients receiving immunosuppressive doses of corticosteroids. Killed or inactivated vaccines may be administered. However, the response to such vaccines may be diminished and cannot be predicted. Indicated immunization procedures may be undertaken in patients receiving nonimmunosuppressive doses of corticosteroids as replacement therapy (e.g., for Addison’s disease).
Ophthalmic
Use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi or viruses. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should not be used in active ocular herpes simplex because of possible corneal perforation.
Kaposi’s Sarcoma
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for
chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma.
Precautions
General Precautions
The lowest possible dose of corticosteroids should be used to control the condition under treatment. When reduction in dosage is possible, the reduction should be gradual.
Since complications of treatment with glucocorticoids are dependent on the size of the dose and the duration of treatment, a risk/benefit decision must be made in each individual case as to dose and duration of treatment and as to whether daily or intermittent therapy should be used.
Cardio-Renal
As sodium retention with resultant edema and potassium loss may occur in patients receiving corticosteroids, these agents should be used with caution in patients with congestive heart failure, hypertension, or renal insufficiency.
Endocrine
Drug-induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for up to 12 months after discontinuation of therapy following large doses for prolonged periods; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted. Since mineralocorticoid secretion may be impaired, salt and/or a mineralocorticoid should be administered concurrently.
There is an enhanced effect of corticosteroids on patients with hypothyroidism.
Gastrointestinal
Steroids should be used with caution in active or latent peptic ulcers, diverticulitis, fresh intestinal anastomoses, and nonspecific ulcerative colitis, since they may increase the risk of a perforation.
Signs of peritoneal irritation following gastrointestinal perforation in patients receiving corticosteroids may be minimal or absent.
There is an enhanced effect due to decreased metabolism of corticosteroids in patients with cirrhosis.
Musculoskeletal
Corticosteroids decrease bone formation and increase bone resorption both through their effect on calcium regulation (i.e., decreasing absorption and increasing excretion) and inhibition of osteoblast function. This, together with a decrease in the protein matrix of the bone secondary to an increase in protein catabolism, and reduced sex hormone production, may lead to inhibition of bone growth in pediatric patients and the development of osteoporosis at any age. Growth and development of infants and children on prolonged corticosteroid therapy should be carefully observed. Special consideration should be given to patients at increased risk of osteoporosis (e.g., postmenopausal women) before initiating corticosteroid therapy.
Inclusion of therapy for osteoporosis prevention or treatment should be considered. To minimize the risk of glucocortoicoid-induced bone loss, the smallest possible effective dosage and duration should be used. Lifestyle modification to reduce the risk of osteoporosis (e.g., cigarette smoking cessation, limitation of alcohol consumption, participation in weight-bearing exercise for 30-60 minutes daily) should be encouraged. Calcium and vitamin D supplementation, bisphosphonate (e.g., alendronate, risedronate), and a weight-bearing exercise program that maintains muscle mass are suitable first-line therapies aimed at reducing the risk of adverse bone effects. Current recommendations suggest that all interventions be initiated in any patient in whom glucocorticoid therapy with at least the equivalent of 5 mg of prednisone for at least 3 months is anticipated; in addition, sex hormone replacement therapy (combined estrogen and progestin in women; testosterone in men) should be offered to such patients who are hypogonadal or in whom replacement is otherwise clinically indicated and biphosphonate therapy should be initiated (if not already) if bone mineral density (BMD) of the lumbar spine and/or hip is below normal.
Neuro-Psychiatric
Although controlled clinical trials have shown corticosteroids to be effective in speeding the resolution of acute exacerbations of multiple sclerosis, they do not show that they affect the ultimate outcome or natural history of the disease. The studies do show that relatively high doses of corticosteroids are necessary to demonstrate a significant effect. (See DOSAGE AND ADMINISTRATION: Multiple Sclerosis .)
An acute myopathy has been observed with the use of high doses of corticosteroids, most often occurring in patients with disorders of neuromuscular transmission (e.g., myasthenia gravis), or in patients receiving concomitant therapy with neuromuscular blocking drugs (e.g., pancuronium). This acute myopathy is generalized, may involve ocular and respiratory muscles, and may result in quadriparesis. Elevation of creatinine kinase may occur. Clinical improvement or recovery after stopping corticosteroids may require weeks to years.
Psychiatric derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression, to frank psychotic manifestations. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids.
Ophthalmic
Intraocular pressure may become elevated in some individuals. If steroid therapy is continued for more than 6 weeks, intraocular pressure should be monitored.
Information for Patients
Patients should be warned not to discontinue the use of corticosteroids abruptly or without medical supervision. As prolonged use may cause adrenal insufficiency and make patients dependent on corticosteroids, they should advise any medical attendants that they are taking corticosteroids and they should seek medical advice at once should they develop an acute illness including fever or other signs of infection. Following prolonged therapy, withdrawal of corticosteroids may result in symptoms of the corticosteroid withdrawal syndrome including, myalgia, arthralgia, and malaise.
Persons who are on corticosteroids should be warned to avoid exposure to chickenpox or measles. Patients should also be advised that if they are exposed, medical advice should be sought without delay.
Drug Interactions
Amphotericin B Injection and Potassium-Depleting Agents
When corticosteroids are administered concomitantly with potassium-depleting agents (e.g., amphotericin B, diuretics), patients should be observed closely for development of hypokalemia. In addition, there have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure.
Antibiotics
Macrolide antibiotics have been reported to cause a significant decrease in corticosteroid clearance (see PRECAUTIONS: Drug Interactions: Hepatic Enzyme Inducers, Inhibitors and Substrates).
Anticholinesterases
Concomitant use of anticholinesterase agents (e.g., neostigmine, pyridostigmine) and corticosteroids may produce severe weakness in patients with myasthenia gravis. If possible, anticholinesterase agents should be withdrawn at least 24 hours before initiating corticosteroid therapy. If concomitant therapy must occur, it should take place under close supervision and the need for respiratory support should be anticipated.
Anticoagulants, Oral
Co-administration of corticosteroids and warfarin usually results in inhibition of response to warfarin, although there have been some conflicting reports. Therefore, coagulation indices should be monitored frequently to maintain the desired anticoagulant effect.
Antidiabetics
Because corticosteroids may increase blood glucose concentrations, dosage adjustments of antidiabetic agents may be required.
Antitubercular drugs
Serum concentrations of isoniazid may be decreased.
Bupropion
Since systemic steroids, as well as bupropion, can lower the seizure threshold, concurrent administration should be undertaken only with extreme caution; low initial dosing and small gradual increases should be employed.
Cholestyramine
Cholestyramine may increase the clearance of corticosteroids.
Cyclosporine
Increased activity of both cyclosporine and corticosteroids may occur when the two are used concurrently. Convulsions have been reported with this concurrent use.
Digitalis Glycosides
Patients on digitalis glycosides may be at increased risk of arrhythmias due to hypokalemia.
Estrogens, Including Oral Contraceptives
Estrogens may decrease the hepatic metabolism of certain corticosteroids, thereby increasing their effect.
Fluoroquinolones
Post-marketing surveillance reports indicate that the risk of tendon rupture may be increased in patients receiving concomitant fluoroquinolones (e.g., ciprofloxacin, levofloxacin) and corticosteroids, especially in the elderly. Tendon rupture can occur during or after treatment with quinolones.
Hepatic Enzyme Inducers, Inhibitors and Substrates
Drugs which induce cytochrome P450 3A4 (CYP 3A4) enzyme activity (e.g., barbiturates, phenytoin, carbamazepine, rifampin) may enhance the metabolism of corticosteroids and require that the dosage of the corticosteroid be increased. Drugs which inhibit CYP 3A4 (e.g., ketoconazole, itraconazole, ritonavir, indinavir, macrolide antibiotics such as erythromycin) have the potential to result in increased plasma concentrations of corticosteroids. Glucocorticoids are moderate inducers of CYP 3A4. Co-administration with other drugs that are metabolized by CYP 3A4 (e.g., indinavir, erythromycin) may increase their clearance, resulting in decreased plasma concentration.
Ketoconazole
Ketoconazole has been reported to decrease the metabolism of certain corticosteroids by up to 60%, leading to increased risk of corticosteroid side effects. In addition, ketoconazole alone can inhibit adrenal corticosteroid synthesis and may cause adrenal insufficiency during corticosteroid withdrawal.
Nonsteroidal Anti-Inflammatory Agents (NSAIDS)
Concomitant use of aspirin (or other nonsteroidal anti-inflammatory agents) and corticosteroids increases the risk of gastrointestinal side effects. Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia. The clearance of salicylates may be increased with concurrent use of corticosteroids; this could lead to decreased salicylate serum levels or increase the risk of salicylate toxicity when corticosteroid is withdrawn.
Phenytoin
In post-marketing experience, there have been reports of both increases and decreases in phenytoin levels with dexamethasone co-administration, leading to alterations in seizure control. Phenytoin has been demonstrated to increase the hepatic metabolism of corticosteroids, resulting in a decreased therapeutic effect of the corticosteroid.
Quetiapine
Increased doses of quetiapine may be required to maintain control of symptoms of schizophrenia in patients receiving a glucocorticoid, a hepatic enzyme inducer.
Skin Tests
Corticosteroids may suppress reactions to skin tests.
Thalidomide
Co-administration with thalidomide should be employed cautiously, as toxic epidermal necrolysis has been reported with concomitant use.
Vaccines
Patients on corticosteroid therapy may exhibit a diminished response to toxoids and live or inactivated vaccines due to inhibition of antibody response. Corticosteroids may also potentiate the replication of some organisms contained in live attenuated vaccines. Routine administration of vaccines or toxoids should be deferred until corticosteroid therapy is discontinued if possible (see WARNINGS: Infection: Vaccination).
Carcinogenesis, Mutagenesis, Impairment of Fertility
No adequate studies have been conducted in animals to determine whether corticosteroids have a potential for carcinogenesis or mutagenesis. Steroids may increase or decrease motility and number of spermatozoa in some patients.
Pregnancy
Teratogenic Effects
Corticosteroids have been shown to be teratogenic in many species when given in doses equivalent to the human dose. Animal studies in which corticosteroids have been given to pregnant mice, rats, and rabbits have yielded an increased incidence of cleft palate in the offspring. There are no adequate and well-controlled studies in pregnant women. Corticosteroids should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Infants born to mothers who have received substantial doses of corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Nursing Mothers
Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. Because of the potential for serious adverse reactions in nursing infants from corticosteroids, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The efficacy and safety of corticosteroids in the pediatric population are based on the well-established course of effect of corticosteroids, which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome (patients >2 years of age), and aggressive lymphomas and leukemias (patients >1 month of age). Other indications for pediatric use of corticosteroids, e.g., severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults, on the premises that the course of the diseases and their pathophysiology are considered to be substantially similar in both populations.
The adverse effects of corticosteroids in pediatric patients are similar to those in adults (see ADVERSE REACTIONS ). Like adults, pediatric patients should be carefully observed with frequent measurements of blood pressure, weight, height, intraocular pressure, and clinical evaluation for the presence of infection, psychosocial disturbances, thromboembolism, peptic ulcers, cataracts, and osteoporosis. Pediatric patients who are treated with corticosteroids by any route, including systemically administered corticosteroids, may experience a decrease in their growth velocity. This negative impact of corticosteroids on growth has been observed at low systemic doses and in the absence of laboratory evidence of hypothalamic-pituitary-adrenal (HPA) axis suppression (i.e., cosyntropin stimulation and basal cortisol plasma levels). Growth velocity may therefore be a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA axis function. The linear growth of pediatric patients treated with corticosteroids should be monitored, and the potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of treatment alternatives. In order to minimize the potential growth effects of corticosteroids, pediatric patients should be titrated to the lowest effective dose.
Geriatric Use
Clinical studies did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. In particular, the increased risk of diabetes mellitus, fluid retention and hypertension in elderly patients treated with corticosteroids should be considered.
Adverse Reactions
(uled alphabetically, under each subsection) The following adverse reactions have been reported with prednisone or other corticosteroids:
Allergic Reactions anaphylactoid or hypersensitivity reactions, anaphylaxis, angioedema.
Cardiovascular System bradycardia, cardiac arrest, cardiac arrhythmias, cardiac enlargement, circulatory collapse, congestive heart failure, ECG changes caused by potassium deficiency, edema, fat embolism, hypertension or aggravation of hypertension, hypertrophic cardiomyopathy in premature infants, myocardial rupture following recent myocardial infarction (see WARNINGS: Cardio-Renal ), necrotizing angiitis, pulmonary edema, syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis.
Dermatologic acne, acneiform eruptions, allergic dermatitis, alopecia, angioedema, angioneurotic edema, atrophy and thinning of skin, dry scaly skin, ecchymoses and petechiae (bruising), erythema, facial edema, hirsutism, impaired wound healing, increased sweating, Karposi’s sarcoma (see PRECAUTIONS: General Precautions ), lupus erythematosus-like lesions, perineal irritation, purpura, rash, striae, subcutaneous fat atrophy, suppression of reactions to skin tests, striae, telangiectasis, thin fragile skin, thinning scalp hair, urticaria.
Endocrine Adrenal insufficiency-greatest potential caused by high potency glucocorticoids with long duration of action (associated symptoms include; arthralgias, buffalo hump, dizziness, life-threatening hypotension, nausea, severe tiredness or weakness), amenorrhea, postmenopausal bleeding or other menstrual irregularities, decreased carbohydrate and glucose tolerance, development of cushingoid state, diabetes mellitus (new onset or manifestations of latent), glycosuria, hyperglycemia, hypertrichosis, hyperthyroidism (see WARNINGS: Endocrine ), hypothyroidism, increased requirements for insulin or oral hypoglycemic agents in diabetics, lipids abnormal, moon face, negative nitrogen balance caused by protein catabolism, secondary adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery or illness) (see WARNINGS: Endocrine ), suppression of growth in pediatric patients.
Fluid and Electrolyte Disturbances congestive heart failure in susceptible patients, fluid retention, hypokalemia, hypokalemic alkalosis, metabolic alkalosis, hypotension or shock-like reaction, potassium loss, sodium retention with resulting edema.
Gastrointestinal abdominal distention, abdominal pain, anorexia which may result in weight loss, constipation, diarrhea, elevation in serum liver enzyme levels (usually reversible upon discontinuation), gastric irritation, hepatomegaly, increased appetite and weight gain, nausea, oropharyngeal candidiasis, pancreatitis, peptic ulcer with possible perforation and hemorrhage, perforation of the small and large intestine (particularly in patients with inflammatory bowel disease), ulcerative esophagitis, vomiting.
Hematologic anemia, neutropenia (including febrile neutropenia).
Metabolic negative nitrogen balance due to protein catabolism.
Musculoskeletal arthralgias, aseptic necrosis of femoral and humeral heads, increase risk of fracture, loss of muscle mass, muscle weakness, myalgias, osteopenia, osteoporosis (see PRECAUTIONS: Musculoskeletal ), pathologic fracture of long bones, steroid myopathy, tendon rupture (particularly of the Achilles tendon), vertebral compression fractures.
Neurological/Psychiatric amnesia, anxiety, benign intracranial hypertension, convulsions, delirium, dementia (characterized by deficits in memory retention, attention, concentration, mental speed and efficiency, and occupational performance), depression, dizziness, EEG abnormalities, emotional instability and irritability, euphoria, hallucinations, headache, impaired cognition, incidence of severe psychiatric symptoms, increased intracranial pressure with papilledema (pseudotumor cerebri) usually following discontinuation of treatment, increased motor activity, insomnia, ischemic neuropathy, long-term memory loss, mania, mood swings, neuritis, neuropathy, paresthesia, personality changes, psychiatric disorders including steroid psychoses or aggravation of preexisting psychiatric conditions, restlessness, schizophrenia, verbal memory loss, vertigo, withdrawn behavior.
Ophthalmic blurred vision, cataracts (including posterior subcapsular cataracts), central serous chorioretinopathy, establishment of secondary bacterial, fungal and viral infections, exophthalmos, glaucoma, increased intraocular pressure (see PRECAUTIONS: Ophthalmic ), optic nerve damage, papilledema.
Other abnormal fat deposits, aggravation/masking of infections, decreased resistance to infection (see WARNINGS: Infection ), hiccups, immunosuppression, increased or decreased motility and number of spermatozoa, malaise, insomnia, moon face, pyrexia.
Dosage And Administration
Gastric irritation may be reduced if taken before, during, or immediately after meals or with food or milk.
The maximal activity of the adrenal cortex is between 2 am and 8 am, and it is minimal between 4 pm and midnight. Exogenous corticosteroids suppress adrenocorticoid activity the least when given at the time of maximal activity (am) for single dose administration. Therefore, it is recommended that prednisone be administered in the morning prior to 9 am and when large doses are given, administration of antacids between meals to help prevent peptic ulcers. Multiple dose therapy should be evenly distributed in evenly spaced intervals throughout the day.
Dietary salt restriction may be advisable in patients.
Do not stop taking this medicine without first talking to your doctor. Avoid abrupt withdraw of therapy.
The initial dosage of PredniSONE tablets may vary from 5 mg to 60 mg per day, depending on the specific disease entity being treated. In situations of less severity lower doses will generally suffice, while in selected patients higher initial doses may be required. The initial dosage should be maintained or adjusted until a satisfactory response is noted. If after a reasonable period of time there is a lack of satisfactory clinical response, PredniSONE should be discontinued and the patient transferred to other appropriate therapy.
IT SHOULD BE EMPHASIZED THAT DOSAGE REQUIREMENTS ARE VARIABLE AND MUST BE INDIVIDUALIZED ON THE BASIS OF THE DISEASE UNDER TREATMENT AND THE RESPONSE OF THE PATIENT. After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial drug dosage in small increments at appropriate time intervals until the lowest dosage which will maintain an adequate clinical response is reached. It should be kept in mind that constant monitoring is needed in regard to drug dosage. Included in the situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient's individual drug responsiveness, and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment; in this latter situation, it may be necessary to increase the dosage of PredniSONE for a period of time consistent with the patient's condition. If after long-term therapy the drug is to be stopped, it is recommended that it be withdrawn gradually rather than abruptly.
Multiple Sclerosis
In the treatment of acute exacerbations of multiple sclerosis daily doses of 200 mg of prednisolone for a week followed by 80 mg every other day for 1 month have been shown to be effective. (Dosage range is the same for prednisone and prednisolone.)
Alternate Day Therapy
Alternate day therapy is a corticosteroid dosing regimen in which twice the usual daily dose of corticoid is administered every other morning. The purpose of this mode of therapy is to provide the patient requiring longterm pharmacologic dose treatment with the beneficial effects of corticoids while minimizing certain undesirable effects, including pituitary-adrenal suppression, the Cushingoid state, corticoid withdrawal symptoms, and growth suppression in children.
The rationale for this treatment schedule is based on two major premises: (a) the anti-inflammatory or therapeutic effect of corticoids persists longer than their physical presence and metabolic effects and (b) administration of the corticosteroid every other morning allows for re-establishment of more nearly normal hypothalamic-pituitary-adrenal (HPA) activity on the off-steroid day.
A brief review of the HPA physiology may be helpful in understanding this rationale. Acting primarily through the hypothalamus a fall in free cortisol stimulates the pituitary gland to produce increasing amounts of corticotropin (ACTH) while a rise in free cortisol inhibits ACTH secretion. Normally the HPA system is characterized by diurnal (circadian) rhythm. Serum levels of ACTH rise from a low point about 10 pm to a peak level about 6 am. Increasing levels of ACTH stimulate adrenocortical activity resulting in a rise in plasma cortisol with maximal levels occurring between 2 am and 8 am. This rise in cortisol dampens ACTH production and in turn adrenocortical activity. There is a gradual fall in plasma corticoids during the day with lowest levels occurring about midnight.
The diurnal rhythm of the HPA axis is lost in Cushing's disease, a syndrome of adrenocortical hyperfunction characterized by obesity with centripetal fat distribution, thinning of the skin with easy bruisability, muscle wasting with weakness, hypertension, latent diabetes, osteoporosis, electrolyte imbalance, etc. The same clinical findings of hyperadrenocorticism may be noted during long-term pharmacologic dose corticoid therapy administered in conventional daily divided doses. It would appear, then, that a disturbance in the diurnal cycle with maintenance of elevated corticoid values during the night may play a significant role in the development of undesirable corticoid effects. Escape from these constantly elevated plasma levels for even short periods of time may be instrumental in protecting against undesirable pharmacologic effects.
During conventional pharmacologic dose corticosteroid therapy, ACTH production is inhibited with subsequent suppression of cortisol production by the adrenal cortex. Recovery time for normal HPA activity is variable depending upon the dose and duration of treatment. During this time the patient is vulnerable to any stressful situation. Although it has been shown that there is considerably less adrenal suppression following a single morning dose of prednisolone (10 mg) as opposed to a quarter of that dose administered every 6 hours, there is evidence that some suppressive effect on adrenal activity may be carried over into the following day when pharmacologic doses are used. Further, it has been shown that a single dose of certain corticosteroids will produce adrenocortical suppression for two or more days. Other corticoids, including methylprednisolone, hydrocortisone, prednisone, and prednisolone, are considered to be short acting (producing adrenocortical suppression for 11/4; to 11/2; days following a single dose) and thus are recommended for alternate day therapy.
The following should be kept in mind when considering alternate day therapy:
Basic principles and indications for corticosteroid therapy should apply. The benefits of alternate day therapy should not encourage the indiscriminate use of steroids.
Alternate day therapy is a therapeutic technique primarily designed for patients in whom long-term pharmacologic corticoid therapy is anticipated.
In less severe disease processes in which corticoid therapy is indicated, it may be possible to initiate treatment with alternate day therapy. More severe disease states usually will require daily divided high dose therapy for initial control of the disease process. The initial suppressive dose level should be continued until satisfactory clinical response is obtained, usually four to ten days in the case of many allergic and collagen diseases. It is important to keep the period of initial suppressive dose as brief as possible particularly when subsequent use of alternate day therapy is intended. Once control has been established, two courses are available: (a) change to alternate day therapy and then gradually reduce the amount of corticoid given every other day or (b) following control of the disease process reduce the daily dose of corticoid to the lowest effective level as rapidly as possible and then change over to an alternate day schedule. Theoretically, course (a) may be preferable.
Because of the advantages of alternate day therapy, it may be desirable to try patients on this form of therapy who have been on daily corticoids for long periods of time (e.g., patients with rheumatoid arthritis). Since these patients may already have a suppressed HPA axis, establishing them on alternate day therapy may be difficult and not always successful. However, it is recommended that regular attempts be made to change them over. It may be helpful to triple or even quadruple the daily maintenance dose and administer this every other day rather than just doubling the daily dose if difficulty is encountered. Once the patient is again controlled, an attempt should be made to reduce this dose to a minimum.
As indicated above, certain corticosteroids, because of their prolonged suppressive effect on adrenal activity, are not recommended for alternate day therapy (e.g., dexamethasone and betamethasone).
The maximal activity of the adrenal cortex is between 2 am and 8 am, and it is minimal between 4 pm and midnight. Exogenous corticosteroids suppress adrenocortical activity the least, when given at the time of maximal activity (am).
In using alternate day therapy it is important, as in all therapeutic situations to individualize and tailor the therapy to each patient. Complete control of symptoms will not be possible in all patients. An explanation of the benefits of alternate day therapy will help the patient to understand and tolerate the possible flareup in symptoms which may occur in the latter part of the off-steroid day. Other symptomatic therapy may be added or increased at this time if needed.
In the event of an acute flare-up of the disease process, it may be necessary to return to a full suppressive daily divided corticoid dose for control. Once control is again established alternate day therapy may be re-instituted.
Although many of the undesirable features of corticosteroid therapy can be minimized by alternate day therapy, as in any therapeutic situation, the physician must carefully weigh the benefit-risk ratio for each patient in whom corticoid therapy is being considered.
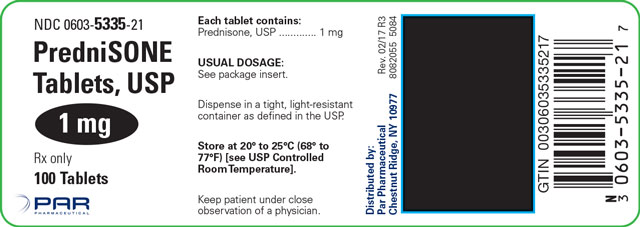
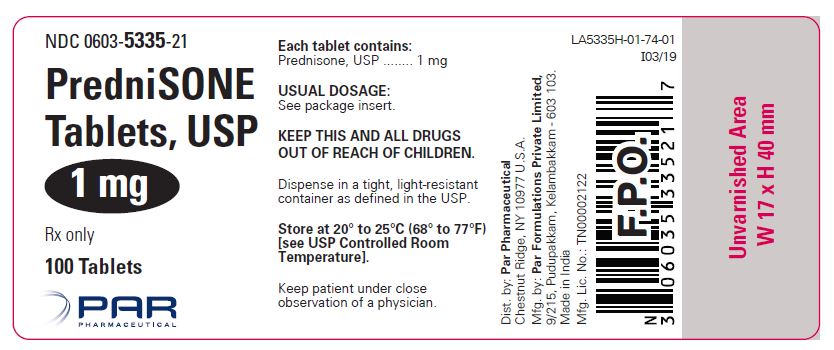
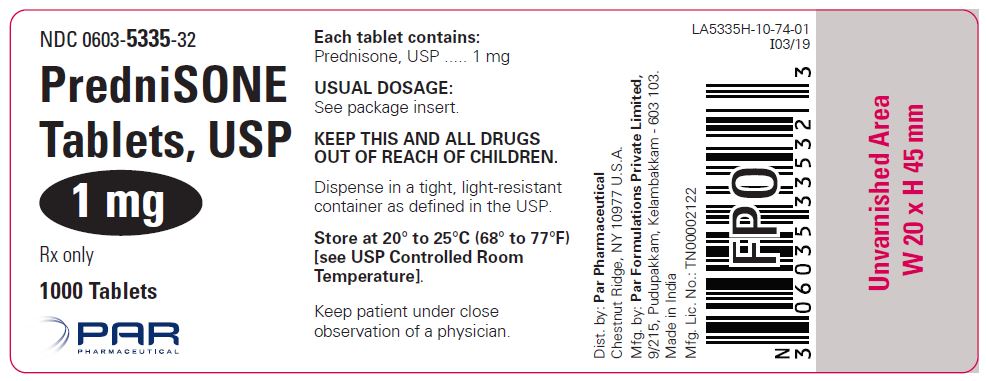
How Supplied
PredniSONE Tablets are available in the following strengths and package sizes:
1 mg (white, round, flat-faced, beveled edge, scored, debossed “5084” on one side and debossed “V” on the reverse side)
- Bottles of 100 NDC 0603-5335-21
- Bottles of 1000 NDC 0603-5335-32
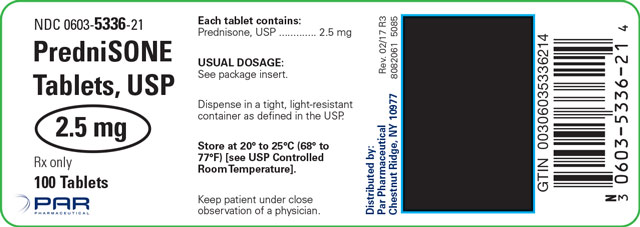
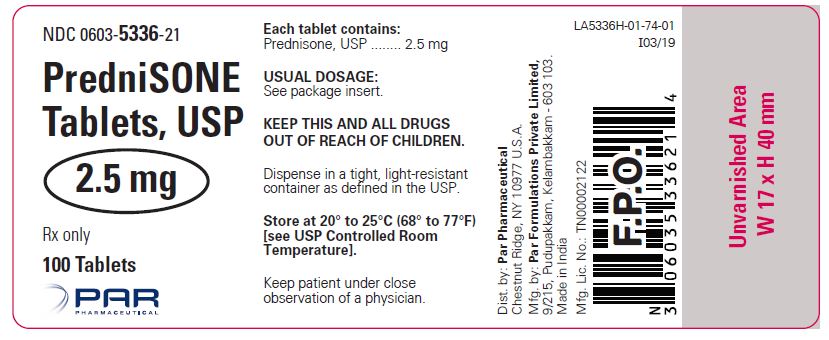
2.5 mg (white, round, flat-faced, beveled edge, scored, debossed “5085” on one side and debossed “V” on the reverse side)
- Bottles of 100 NDC 0603-5336-21
5 mg (white, round, scored, debossed “5094” on one side and debossed “V” on the reverse side)
- Bottles of 100 NDC 0603-5337-21
- Bottles of 1000 NDC 0603-5337-32
- Unit-of-Use (21 Tablets) NDC 0603-5337-15
- Unit-of-Use (48 Tablets) NDC 0603-5337-31
10 mg (white, round, scored, debossed “5093” on one side and debossed “V” on the reverse side)
- Bottles of 100 NDC 0603-5338-21
- Bottles of 500 NDC 0603-5338-28
- Bottles of 1000 NDC 0603-5338-32
- Unit-of-Use (21 Tablets) NDC 0603-5338-15
- Unit-of-Use (48 Tablets) NDC 0603-5338-31
20 mg (peach, round, scored, debossed “5092” on one side and debossed “V” on the reverse side)
- Bottles of 100 NDC 0603-5339-21
- Bottles of 500 NDC 0603-5339-28
- Bottles of 1000 NDC 0603-5339-32
STORAGE AND HANDLING SECTION
Dispense in a tight, light-resistant container as defined in the USP.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
References
- Fekety R. Infections associated with corticosteroids and immunosuppressive therapy. In: Gorbach SL, Bartlett JG, Blacklow NR, eds. Infectious Diseases. Philadelphia: WBSaunders Company 1992:1050-1.
- Stuck AE, Minder CE, Frey FJ. Risk of infectious complications in patients taking glucocorticoids. Rev Infect Dis 1989:11(6):954-63.
Manufactured for:
Endo USA
Malvern, PA 19355 U.S.A.
Made in India
Neutral Code: TN/DRUGS/TN00002122
© 2024 Endo, Inc. or one of its affiliates.
OS5335H-01-74-03
Revised: 08/2024
Principal Display Panel - 1 Mg
Principal Display Panel - 2.5 Mg
Principal Display Panel - 5 Mg
Principal Display Panel - 10 Mg
Principal Display Panel - 20 Mg
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site