Triazolam (triazolam 0.25 mg) Dailymed
Generic: triazolam is used for the treatment of Sleep Initiation and Maintenance Disorders Pregnancy
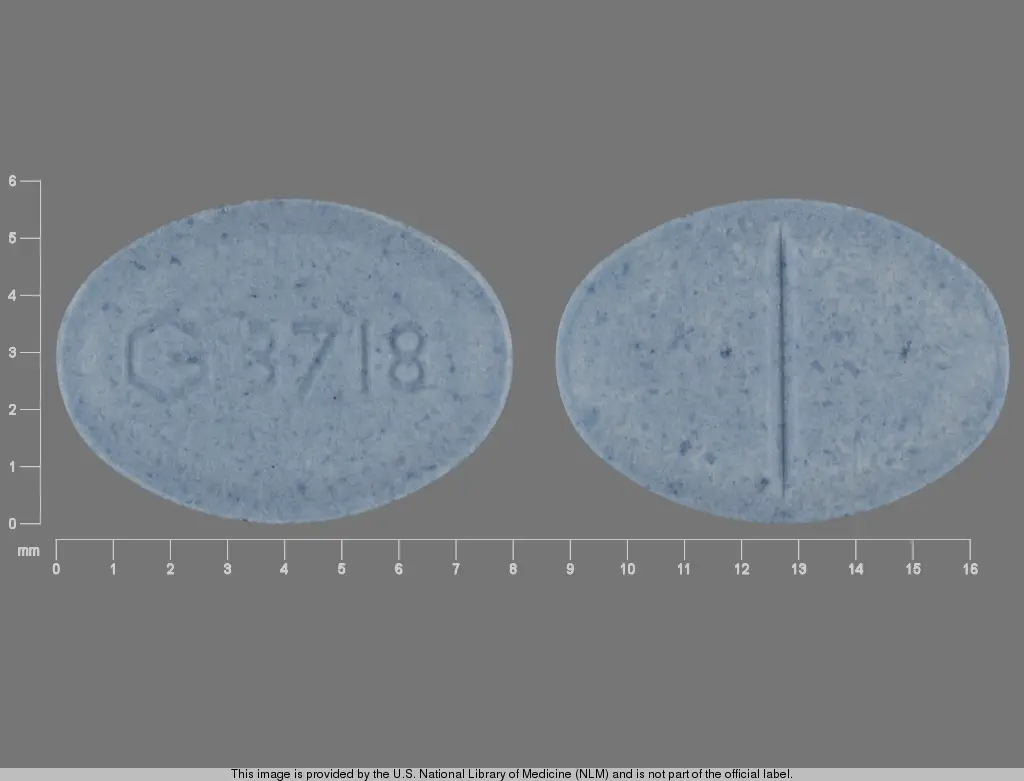
IMPRINT: G3718
SHAPE: oval
COLOR: blue SCORE: 2
All Imprints
triazolam 0.25 mg - g3718 oval blue
triazolam 0.125 mg - g3717 oval white
Boxed Warning
Warning: Risks From Concomitant Use With Opioids
- Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
- Limit dosages and durations to the minimum required.Follow patients for signs and symptoms of respiratory depression and sedation.
Go PRO for all pill images
Warning: Risks From Concomitant Use With Opioids
Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death [see Warnings, Drug Interactions].
- Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
- Limit dosages and durations to the minimum required.Follow patients for signs and symptoms of respiratory depression and sedation.
Description
Triazolam is a triazolobenzodiazepine hypnotic agent.
Triazolam is a white crystalline powder, soluble in alcohol and poorly soluble in water. It has a molecular weight of 343.21.
The chemical name for triazolam is 8-chloro-6-(o-chlorophenyl)-1-methyl-4H-s-triazolo-[4,3-α] [1,4] benzodiazepine.
The structural formula is represented below:

Each triazolam tablet, for oral administration, contains 0.125 mg or 0.25 mg of triazolam. Inactive ingredients: 0.125 mg—cellulose, corn starch, docusate sodium, lactose, magnesium stearate, silicon dioxide, sodium benzoate; 0.25 mg—cellulose, corn starch, docusate sodium, FD&C Blue No. 2, lactose, magnesium stearate, silicon dioxide, sodium benzoate.
Clinical Pharmacology
Triazolam is a hypnotic with a short mean plasma half-life reported to be in the range of 1.5 to 5.5 hours. In normal subjects treated for 7 days with four times the recommended dosage, there was no evidence of altered systemic bioavailability, rate of elimination, or accumulation. Peak plasma levels are reached within 2 hours following oral administration. Following recommended doses of triazolam tablets, triazolam peak plasma levels in the range of 1 to 6 ng/mL are seen. The plasma levels achieved are proportional to the dose given.
Triazolam and its metabolites, principally as conjugated glucuronides, which are presumably inactive, are excreted primarily in the urine. Only small amounts of unmetabolized triazolam appear in the urine. The two primary metabolites accounted for 79.9% of urinary excretion. Urinary excretion appeared to be biphasic in its time course.
Triazolam tablets 0.5 mg, in two separate studies, did not affect the prothrombin times or plasma warfarin levels in male volunteers administered sodium warfarin orally.
Extremely high concentrations of triazolam do not displace bilirubin bound to human serum albumin in vitro.
Triazolam 14C was administered orally to pregnant mice. Drug-related material appeared uniformly distributed in the fetus with 14C concentrations approximately the same as in the brain of the mother.
In sleep laboratory studies, triazolam tablets significantly decreased sleep latency, increased the duration of sleep, and decreased the number of nocturnal awakenings. After 2 weeks of consecutive nightly administration, the drug's effect on total wake time is decreased, and the values recorded in the last third of the night approach baseline levels. On the first and/or second night after drug discontinuance (first or second post-drug night), total time asleep, percentage of time spent sleeping, and rapidity of falling asleep frequently were significantly less than on baseline (predrug) nights. This effect is often called "rebound" insomnia.
The type and duration of hypnotic effects and the profile of unwanted effects during administration of benzodiazepine drugs may be influenced by the biologic half-life of administered drug and any active metabolites formed. When half-lives are long, the drug or metabolites may accumulate during periods of nightly administration and be associated with impairments of cognitive and motor performance during waking hours; the possibility of interaction with other psychoactive drugs or alcohol will be enhanced. In contrast, if half-lives are short, the drug and metabolites will be cleared before the next dose is ingested, and carry-over effects related to excessive sedation or CNS depression should be minimal or absent. However, during nightly use for an extended period pharmacodynamic tolerance or adaptation to some effects of benzodiazepine hypnotics may develop. If the drug has a short half-life of elimination, it is possible that a relative deficiency of the drug or its active metabolites (ie, in relationship to the receptor site) may occur at some point in the interval between each night's use. This sequence of events may account for two clinical findings reported to occur after several weeks of nightly use of rapidly eliminated benzodiazepine hypnotics: 1) increased wakefulness during the last third of the night and 2) the appearance of increased daytime anxiety after 10 days of continuous treatment.
In a study of elderly (62–83 years old) versus younger subjects (21–41 years old) who received triazolam at the same dose levels (0.125 mg and 0.25 mg), the elderly experienced both greater sedation and impairment of psychomotor performance. These effects resulted largely from higher plasma concentrations of triazolam in the elderly.
Indications And Usage
Triazolam is indicated for the short-term treatment of insomnia (generally 7–10 days). Use for more than 2–3 weeks requires complete reevaluation of the patient (see WARNINGS).
Prescriptions for triazolam should be written for short-term use (7–10 days) and it should not be prescribed in quantities exceeding a 1-month supply.
Contraindications
Triazolam tablets are contraindicated in patients with known hypersensitivity to this drug or other benzodiazepines.
Benzodiazepines may cause fetal damage when administered during pregnancy. An increased risk of congenital malformations associated with the use of diazepam and chlordiazepoxide during the first trimester of pregnancy has been suggested in several studies. Transplacental distribution has resulted in neonatal CNS depression following the ingestion of therapeutic doses of a benzodiazepine hypnotic during the last weeks of pregnancy.
Triazolam is contraindicated in pregnant women. If there is a likelihood of the patient becoming pregnant while receiving triazolam, she should be warned of the potential risk to the fetus. Patients should be instructed to discontinue the drug prior to becoming pregnant. The possibility that a woman of childbearing potential may be pregnant at the time of institution of therapy should be considered.
Triazolam is contraindicated with medications that significantly impair the oxidative metabolism mediated by cytochrome P450 3A (CYP 3A) including ketoconazole, itraconazole, nefazodone, and several HIV protease inhibitors, (see WARNINGS and PRECAUTIONS–Drug Interactions).
Warnings
Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including triazolam, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe triazolam concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. In patients already receiving an opioid analgesic, prescribe a lower initial dose of triazolam than indicated in the absence of an opioid and titrate based on clinical response. If an opioid is initiated in a patient already taking triazolam, prescribe a lower initial dose of the opioid and titrate based upon clinical response.
Advise both patients and caregivers about the risks of respiratory depression and sedation when triazolam is used with opioids. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined [see Drug Interactions].
Persistent or Worsening Insomnia
Because sleep disturbances may be the presenting manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after a careful evaluation of the patient. The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Worsening of insomnia or the emergence of new thinking or behavior abnormalities may be the consequence of an unrecognized psychiatric or physical disorder. Such findings have emerged during the course of treatment with sedative-hypnotic drugs. Because some of the important adverse effects of sedative-hypnotics appear to be dose related (see Precautions and Dosage and Administration), it is important to use the smallest possible effective dose, especially in the elderly.
"Sleep-driving" and Other Complex Behaviors
Complex behaviors such as "sleep-driving" (i.e., driving while not fully awake after ingestion of a sedative-hypnotic, with amnesia for the event) have been reported. These events can occur in sedative-hypnotic-naĂŻve as well as in sedative-hypnotic-experienced persons. Although behaviors such as sleep-driving may occur with sedative-hypnotics alone at therapeutic doses, the use of alcohol and other CNS depressants with sedative-hypnotics appears to increase the risk of such behaviors, as does the use of sedative-hypnotics at doses exceeding the maximum recommended dose. Due to the risk to the patient and the community, discontinuation of sedative-hypnotics should be strongly considered for patients who report a "sleep-driving" episode.
Other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex) have been reported in patients who are not fully awake after taking a sedative-hypnotic. As with sleep-driving, patients usually do not remember these events.
Severe anaphylactic and anaphylactoid reactions
Rare cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or subsequent doses of sedative-hypnotics, including triazolam. Some patients have had additional symptoms such as dyspnea, throat closing, or nausea and vomiting that suggest anaphylaxis. Some patients have required medical therapy in the emergency department. If angioedema involves the tongue, glottis or larynx, airway obstruction may occur and be fatal. Patients who develop angioedema after treatment with triazolam should not be rechallenged with the drug.
Central nervous system manifestations
An increase in daytime anxiety has been reported for triazolam after as few as 10 days of continuous use. In some patients this may be a manifestation of interdose withdrawal (see CLINICAL PHARMACOLOGY). If increased daytime anxiety is observed during treatment, discontinuation of treatment may be advisable.
A variety of abnormal thinking and behavior changes have been reported to occur in association with the use of benzodiazepine hypnotics including triazolam. Some of these changes may be characterized by decreased inhibition, eg, aggressiveness and extroversion that seem excessive, similar to that seen with alcohol and other CNS depressants (eg, sedative/hypnotics). Other kinds of behavioral changes have also been reported, for example, bizarre behavior, agitation, hallucinations, depersonalization. In primarily depressed patients, the worsening of depression, including suicidal thinking, has been reported in association with the use of benzodiazepines.
It can rarely be determined with certainty whether a particular instance of the abnormal behaviors uled above is drug induced, spontaneous in origin, or a result of an underlying psychiatric or physical disorder. Nonetheless, the emergence of any new behavioral sign or symptom of concern requires careful and immediate evaluation.
Because of its depressant CNS effects, patients receiving triazolam should be cautioned against engaging in hazardous occupations requiring complete mental alertness such as operating machinery or driving a motor vehicle. For the same reason, patients should be cautioned about the concomitant ingestion of alcohol and other CNS depressant drugs during treatment with triazolam tablets.
As with some, but not all benzodiazepines, anterograde amnesia of varying severity and paradoxical reactions have been reported following therapeutic doses of triazolam. Data from several sources suggest that anterograde amnesia may occur at a higher rate with triazolam than with other benzodiazepine hypnotics.
Triazolam interaction with drugs that inhibit metabolism via cytochrome P450 3A
The initial step in triazolam metabolism is hydroxylation catalyzed by cytochrome P450 3A (CYP 3A). Drugs that inhibit this metabolic pathway may have a profound effect on the clearance of triazolam. Consequently, triazolam should be avoided in patients receiving very potent inhibitors of CYP 3A. With drugs inhibiting CYP 3A to a lesser but still significant degree, triazolam should be used only with caution and consideration of appropriate dosage reduction. For some drugs, an interaction with triazolam has been quantified with clinical data; for other drugs, interactions are predicted from in vitro data and/or experience with similar drugs in the same pharmacologic class.
The following are examples of drugs known to inhibit the metabolism of triazolam and/or related benzodiazepines, presumably through inhibition of CYP 3A.
Potent CYP 3A inhibitors
Potent inhibitors of CYP 3A that should not be used concomitantly with triazolam include ketoconazole, itraconazole, nefazodone and several HIV protease inhibitors including ritonavir, indinavir, nelfinavir, saquinavir and lopinavir. Although data concerning the effects of azole-type antifungal agents other than ketoconazole and itraconazole on triazolam metabolism are not available, they should be considered potent CYP 3A inhibitors, and their coadministration with triazolam is not recommended (see CONTRAINDICATIONS).
Drugs demonstrated to be CYP 3A inhibitors on the basis of clinical studies involving triazolam (caution and consideration of dose reduction are recommended during coadministration with triazolam)
Macrolide Antibiotics
Coadministration of erythromycin increased the maximum plasma concentration of triazolam by 46%, decreased clearance by 53%, and increased half-life by 35%; caution and consideration of appropriate triazolam dose reduction are recommended. Similar caution should be observed during coadministration with clarithromycin and other macrolide antibiotics.
Cimetidine
Coadministration of cimetidine increased the maximum plasma concentration of triazolam by 51%, decreased clearance by 55%, and increased half-life by 68%; caution and consideration of appropriate triazolam dose reduction are recommended.
Other drugs possibly affecting triazolam metabolism
Other drugs possibly affecting triazolam metabolism by inhibition of CYP 3A are discussed in the PRECAUTIONS section (see PRECAUTIONS–Drug Interactions).
Precautions
General
In elderly and/or debilitated patients it is recommended that treatment with triazolam tablets be initiated at 0.125 mg to decrease the possibility of development of oversedation, dizziness, or impaired coordination.
Some side effects reported in association with the use of triazolam appear to be dose related. These include drowsiness, dizziness, light-headedness, and amnesia.
The relationship between dose and what may be more serious behavioral phenomena is less certain. Specifically, some evidence, based on spontaneous marketing reports, suggests that confusion, bizarre or abnormal behavior, agitation, and hallucinations may also be dose related, but this evidence is inconclusive. In accordance with good medical practice it is recommended that therapy be initiated at the lowest effective dose (see DOSAGE AND ADMINISTRATION).
Cases of "traveler's amnesia" have been reported by individuals who have taken triazolam to induce sleep while traveling, such as during an airplane flight. In some of these cases, insufficient time was allowed for the sleep period prior to awakening and before beginning activity. Also, the concomitant use of alcohol may have been a factor in some cases.
Caution should be exercised if triazolam is prescribed to patients with signs or symptoms of depression that could be intensified by hypnotic drugs. Suicidal tendencies may be present in such patients and protective measures may be required. Intentional over-dosage is more common in these patients, and the least amount of drug that is feasible should be available to the patient at any one time.
The usual precautions should be observed in patients with impaired renal or hepatic function, chronic pulmonary insufficiency, and sleep apnea. In patients with compromised respiratory function, respiratory depression and apnea have been reported infrequently.
Information for patients
The text of a Medication Guide for patients is included at the end of this insert. To assure safe and effective use of triazolam, the information and instructions provided in this Medication Guide should be discussed with patients.
Risks from Concomitant Use with Opioids
Advise both patients and caregivers about the risks of potentially fatal respiratory depression and sedation when triazolam is used with opioids and not to use such drugs concomitantly unless supervised by a healthcare provider. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined [see Drug Interactions].
"Sleep-driving" and other complex behaviors
There have been reports of people getting out of bed after taking a sedative-hypnotic and driving their cars while not fully awake, often with no memory of the event. If a patient experiences such an episode, it should be reported to his or her doctor immediately, since "sleep-driving" can be dangerous. This behavior is more likely to occur when sedative-hypnotics are taken with alcohol or other central nervous system depressants (see WARNINGS). Other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex) have been reported in patients who are not fully awake after taking a sedative hypnotic. As with sleep-driving, patients usually do not remember these events.
Laboratory tests
Laboratory tests are not ordinarily required in otherwise healthy patients.
Drug interactions
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAA sites and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and monitor patients closely for respiratory depression and sedation.
Both pharmacodynamic and pharmacokinetic interactions have been reported with benzodiazepines. In particular, triazolam produces additive CNS depressant effects when coadministered with other psychotropic medications, anticonvulsants, antihistamines, ethanol, and other drugs which themselves produce CNS depression.
Drugs that inhibit triazolam metabolism via cytochrome P450 3A
The initial step in triazolam metabolism is hydroxylation catalyzed by cytochrome P450 3A (CYP 3A). Drugs which inhibit this metabolic pathway may have a profound effect on the clearance of triazolam (see CONTRAINDICATIONS and WARNINGS for additional drugs of this type). Triazolam is contraindicated with ketoconzaole, itraconazole, nefazodone, and several HIV protease inhibitors.
Drugs and other substances demonstrated to be CYP 3A inhibitors of possible clinical significance on the basis of clinical studies involving triazolam (caution is recommended during coadministration with triazolam)
Isoniazid
Coadministration of isoniazid increased the maximum plasma concentration of triazolam by 20%, decreased clearance by 42%, and increased half-life by 31%.
Oral contraceptives
Coadministration of oral contraceptives increased maximum plasma concentration by 6%, decreased clearance by 32%, and increased half-life by 16%.
Grapefruit juice
Coadministration of grapefruit juice increased the maximum plasma concentration of triazolam by 25%, increased the area under the concentration curve by 48%, and increased half-life by 18%.
Drugs demonstrated to be CYP 3A inhibitors on the basis of clinical studies involving benzodiazepines metabolized similarly to triazolam or on the basis of in vitro studies with triazolam or other benzodiazepines (caution is recommended during coadministration with triazolam)
Available data from clinical studies of benzodiazepines other than triazolam suggest a possible drug interaction with triazolam for the following: fluvoxamine, diltiazem, and verapamil. Data from in vitro studies of triazolam suggest a possible drug interaction with triazolam for the following: sertraline and paroxetine. Data from in vitro studies of benzodiazepines other than triazolam suggest a possible drug interaction with triazolam for the following: ergotamine, cyclosporine, amiodarone, nicardipine, and nifedipine. Caution is recommended during coadministration of any of these drugs with triazolam (see WARNINGS).
Drugs that affect triazolam pharmacokinetics by other mechanisms
Ranitidine
Coadministration of ranitidine increased the maximum plasma concentration of triazolam by 30%, increased the area under the concentration curve by 27%, and increased half-life by 3.3%. Caution is recommended during coadministration with triazolam.
Carcinogenesis, mutagenesis, impairment of fertility
No evidence of carcinogenic potential was observed in mice during a 24-month study with triazolam in doses up to 4,000 times the human dose.
Pregnancy
1. Teratogenic effects
Pregnancy category X (see CONTRAINDICATIONS).
2. Non-teratogenic effects
It is to be considered that the child born of a mother who is on benzodiazepines may be at some risk for withdrawal symptoms from the drug, during the postnatal period. Also, neonatal flaccidity has been reported in an infant born of a mother who had been receiving benzodiazepines.
Nursing mothers
Human studies have not been performed; however, studies in rats have indicated that triazolam and its metabolites are secreted in milk. Therefore, administration of triazolam to nursing mothers is not recommended.
Pediatric use
Safety and effectiveness of triazolam in individuals below 18 years of age have not been established.
Geriatric use
The elderly are especially susceptible to the dose related adverse effects of triazolam. They exhibit higher plasma triazolam concentrations due to reduced clearance of the drug as compared with younger subjects at the same dose. To minimize the possibility of development of oversedation, the smallest effective dose should be used (see CLINICAL PHARMACOLOGY, WARNINGS, PRECAUTIONS, and DOSAGE AND ADMINISTRATION).
Tolerance/Withdrawal Phenomena
Some loss of effectiveness or adaptation to the sleep inducing effects of these medications may develop after nightly use for more than a few weeks and there may be a degree of dependence that develops. For the benzodiazepine sleeping pills that are eliminated quickly from the body, a relative deficiency of the drug may occur at some point in the interval between each night's use. This can lead to (1) increased wakefulness during the last third of the night, and (2) the appearance of increased signs of daytime anxiety or nervousness. These two events have been reported in particular for triazolam.
There can be more severe 'withdrawal' effects when a benzodiazepine sleeping pill is stopped. Such effects can occur after discontinuing these drugs following use for only a week or two, but may be more common and more severe after longer periods of continuous use. One type of withdrawal phenomenon is the occurrence of what is known as 'rebound insomnia'. That is, on the first few nights after the drug is stopped, insomnia is actually worse than before the sleeping pill was given. Other withdrawal phenomena following abrupt stopping of benzodiazepine sleeping pills range from mild unpleasant feelings to a major withdrawal syndrome which may include abdominal and muscle cramps, vomiting, sweating, tremor, and rarely, convulsions.
Adverse Reactions
During placebo-controlled clinical studies in which 1,003 patients received triazolam tablets, the most troublesome side effects were extensions of the pharmacologic activity of triazolam, eg, drowsiness, dizziness, or light-headedness.
The figures cited below are estimates of untoward clinical event incidence among subjects who participated in the relatively short duration (i.e., 1 to 42 days) placebo-controlled clinical trials of triazolam. The figures cannot be used to predict precisely the incidence of untoward events in the course of usual medical practice where patient characteristics and other factors often differ from those in clinical trials. These figures cannot be compared with those obtained from other clinical studies involving related drug products and placebo, as each group of drug trials is conducted under a different set of conditions.
Comparison of the cited figures, however, can provide the prescriber with some basis for estimating the relative contributions of drug and nondrug factors to the untoward event incidence rate in the population studied. Even this use must be approached cautiously, as a drug may relieve a symptom in one patient while inducing it in others. (For example, an anticholinergic, anxiolytic drug may relieve dry mouth [a sign of anxiety] in some subjects but induce it [an untoward event] in others.)
Triazolam PLACEBO Number of Patients 1003 997 % Patients Reporting: Central Nervous System Drowsiness 14.0 6.4 Headache 9.7 8.4 Dizziness 7.8 3.1 Nervousness 5.2 4.5 Light-headedness 4.9 0.9 Coordination disorders/ataxia 4.6 0.8 Gastrointestinal Nausea/vomiting 4.6 3.7
In addition to the relatively common (i.e., 1% or greater) untoward events enumerated above, the following adverse events have been reported less frequently (i.e., 0.9% to0.5%): euphoria, tachycardia, tiredness, confusional states/memory impairment, cramps/pain, depression, visual disturbances.
Rare (i.e., less than 0.5%) adverse reactions included constipation, taste alterations, diarrhea, dry mouth, dermatitis/allergy, dreaming/nightmares, insomnia, paresthesia, tinnitus, dysesthesia, weakness, congestion, death from hepatic failure in a patient also receiving diuretic drugs.
In addition to these untoward events for which estimates of incidence are available, the following adverse events have been reported in association with the use of triazolam and other benzodiazepines: amnestic symptoms (anterograde amnesia with appropriate or inappropriate behavior), confusional states (disorientation, derealization, depersonalization, and/or clouding of consciousness), dystonia, anorexia, fatigue, sedation, slurred speech, jaundice, pruritus, dysarthria, changes in libido, menstrual irregularities, incontinence, and urinary retention. Other factors may contribute to some of these reactions, eg, concomitant intake of alcohol or other drugs, sleep deprivation, an abnormal premorbid state, etc.
Other events reported include: paradoxical reactions such as stimulation, mania, an agitational state (restlessness, irritability, and excitation), increased muscle spasticity, sleep disturbances, hallucinations, delusions, aggressiveness, falling, somnambulism, syncope, inappropriate behavior and other adverse behavioral effects. Should these occur, use of the drug should be discontinued.
The following events have also been reported: chest pain, burning tongue/glossitis/stomatitis.
Laboratory analyses were performed on all patients participating in the clinical program for triazolam. The following incidences of abnormalities were observed in patients receiving triazolam and the corresponding placebo group. None of these changes were considered to be of physiological significance.
Triazolam PLACEBO Number of Patients 380 361 % of Patients Reporting: Low High Low High Hematology Hematocrit Less than 1% Hemoglobin Total WBC count 1.7 2.1 1.3 Neutrophil count 1.5 1.5 3.3 1.0 Lymphocyte count 2.3 4.0 3.1 3.8 Monocyte count 3.6 4.4 1.5 Eosinophil count 10.2 3.2 9.8 3.4 Basophil count 1.7 2.1 1.8 Urinalysis Albumin — 1.1 — Sugar — — RBC/HPF — 2.9 — 2.9 WBC/HPF — 11.7 — 7.9 Blood chemistry Creatinine 2.4 1.9 3.6 1.5 Bilirubin 1.5 1.0 SGOT 5.3 4.5 Alkaline phosphatase 2.2 2.6
When treatment with triazolam is protracted, periodic blood counts, urinalysis, and blood chemistry analyses are advisable.
Minor changes in EEG patterns, usually low-voltage fast activity, have been observed in patients during therapy with triazolam and are of no known significance.
Drug Abuse And Dependence
Abuse and addiction are separate and distinct from physical dependence and tolerance. Abuse is characterized by misuse of the drug for non-medical purposes, often in combination with other psychoactive substances. Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug and/or administration of an antagonist. Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug's effects over time. Tolerance may occur to both the desired and undesired effects of drugs and may develop at different rates for different effects.
Addiction is a primary, chronic, neurobiological disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. Drug addiction is a treatable disease, utilizing a multidisciplinary approach, but relapse is common.
Controlled Substance
Triazolam is a controlled substance under the Controlled Substance Act, and triazolam tablets have been assigned to Schedule IV.
Abuse, Dependence and Withdrawal
Withdrawal symptoms, similar in character to those noted with barbiturates and alcohol (convulsions, tremor, abdominal and muscle cramps, vomiting, sweating, dysphoria, perceptual disturbances and insomnia), have occurred following abrupt discontinuance of benzodiazepines, including triazolam. The more severe symptoms are usually associated with higher dosages and longer usage, although patients at therapeutic dosages given for as few as 1–2 weeks can also have withdrawal symptoms and in some patients there may be withdrawal symptoms (daytime anxiety, agitation) between nightly doses (see CLINICAL PHARMACOLOGY). Consequently, abrupt discontinuation should be avoided and a gradual dosage tapering schedule is recommended in any patient taking more than the lowest dose for more than a few weeks. The recommendation for tapering is particularly important in any patient with a history of seizure.
The risk of dependence is increased in patients with a history of alcoholism, drug abuse, or in patients with marked personality disorders. Such dependence-prone individuals should be under careful surveillance when receiving triazolam. As with all hypnotics, repeat prescriptions should be limited to those who are under medical supervision.
Overdosage
Because of the potency of triazolam, some manifestations of overdosage may occur at 2 mg, four times the maximum recommended therapeutic dose (0.5 mg).
Manifestations of overdosage with triazolam tablets include somnolence, confusion, impaired coordination, slurred speech, and ultimately, coma. Respiratory depression and apnea have been reported with overdosages of triazolam. Seizures have occasionally been reported after overdosages.
Death has been reported in association with overdoses of triazolam by itself, as it has with other benzodiazepines. In addition, fatalities have been reported in patients who have overdosed with a combination of a single benzodiazepine, including triazolam, and alcohol; benzodiazepine and alcohol levels seen in some of these cases have been lower than those usually associated with reports of fatality with either substance alone.
As in all cases of drug overdosage, respiration, pulse, and blood pressure should be monitored and supported by general measures when necessary. Immediate gastric lavage should be performed. An adequate airway should be maintained. Intravenous fluids may be administered.
Flumazenil, a specific benzodiazepine receptor antagonist, is indicated for the complete or partial reversal of the sedative effects of benzodiazepines and may be used in situations when an overdose with a benzodiazepine is known or suspected. Prior to the administration of flumazenil, necessary measures should be instituted to secure airway, ventilation and intravenous access. Flumazenil is intended as an adjunct to, not as a substitute for, proper management of benzodiazepine overdose. Patients treated with flumazenil should be monitored for resedation, respiratory depression, and other residual benzodiazepine effects for an appropriate period after treatment. The prescriber should be aware of a risk of seizure in association with flumazenil treatment, particularly in long-term benzodiazepine users and in cyclic antidepressant overdose. The complete flumazenil package insert including CONTRAINDICATIONS, WARNINGS and PRECAUTIONS should be consulted prior to use.
Experiments in animals have indicated that cardiopulmonary collapse can occur with massive intravenous doses of triazolam. This could be reversed with positive mechanical respiration and the intravenous infusion of norepinephrine bitartrate or metaraminol bitartrate. Hemodialysis and forced diuresis are probably of little value. As with the management of intentional overdosage with any drug, the physician should bear in mind that multiple agents may have been ingested by the patient.
The oral LD50 in mice is greater than 1,000 mg/kg and in rats is greater than 5,000 mg/kg.
Dosage And Administration
It is important to individualize the dosage of triazolam tablets for maximum beneficial effect and to help avoid significant adverse effects.
The recommended dose for most adults is 0.25 mg before retiring. A dose of 0.125 mg may be found to be sufficient for some patients (e.g., low body weight). A dose of 0.5 mg should be used only for exceptional patients who do not respond adequately to a trial of a lower dose since the risk of several adverse reactions increases with the size of the dose administered. A dose of 0.5 mg should not be exceeded.
In geriatric and/or debilitated patients the recommended dosage range is 0.125 mg to 0.25 mg. Therapy should be initiated at 0.125 mg in these groups and the 0.25 mg dose should be used only for exceptional patients who do not respond to a trial of the lower dose. A dose of 0.25 mg should not be exceeded in these patients.
As with all medications, the lowest effective dose should be used.
How Supplied
Triazolam tablets are available in the following strengths and package sizes:
0.125 mg (white, imprinted G3717): Â Â Bottles of 10 NDC 59762-3717-4 Â Â Bottles of 100 NDC 59762-3717-9 0.25 mg (powder blue, scored, imprinted G3718): Â Â Bottles of 10 NDC 59762-3718-4 Â Â Bottles of 100 NDC 59762-3718-9 Â Â Bottles of 500 NDC 59762-3718-3 STORAGE AND HANDLING SECTION
Store at controlled room temperature 20° to 25°C (68° to 77°F) [see USP].

LAB-0689-5.0January 2017
Spl Medguide Section
MEDICATION GUIDETRIAZOLAM Tablets, C-IV Rx only What is the most important information I should know about triazolam?
- Triazolam is a benzodiazepine medicine. Taking benzodiazepines with opioid medicines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, breathing problems (respiratory depression), coma and death.
- After taking triazolam, you may get up out of bed while not being fully awake and do an activity that you do not know you are doing. The next morning, you may not remember that you did anything during the night. You have a higher chance for doing these activities if you drink alcohol or take other medicines that make you sleepy with triazolam. Reported activities include:
Call your healthcare provider right away if you find out that you have done any of the above activities after taking triazolam.
- driving a car ("sleep-driving")
- making and eating food
- talking on the phone
- having sex
- sleep-walking
- Do not take triazolam unless you are able to stay in bed a full night (7 to 8 hours) before you must be active again.
- Do not take more triazolam than prescribed.
What is triazolam?
- Triazolam is a prescription medicine used to treat certain types of insomnia including difficulty falling asleep, waking up often during the night, or waking up early in the morning.
- Triazolam is a federal controlled substance (C-IV) because it can be abused or lead to dependence. Keep triazolam in a safe place to prevent misuse and abuse. Selling or giving away triazolam may harm others, and is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs.
- It is not known if triazolam is safe and effective in children.
- Elderly patients are especially susceptible to dose related adverse effects when taking triazolam.
- It is not known if triazolam is safe and effective for use longer than 2 to 3 weeks.
Do not take triazolam if you:
- are allergic to triazolam, other benzodiazepines, or any of the ingredients in triazolam. See the end of this Medication Guide for a complete ul of ingredients in triazolam.
- take antifungal medicines including ketoconazole and itraconazole
- take a medicine to treat depression called nefazodone
- take medicines to treat HIV infection called protease inhibitors, including ritonavir, indinavir, nelfinavir, saquinavir or lopinavir
Before you take triazolam, tell your healthcare provider about all of your medical conditions, including if you: Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Do not take triazolam with other medicines that can make you sleepy. Taking triazolam with certain other medicines can cause side effects or affect how well triazolam or the other medicines work. Do not start or stop other medicines without talking to your healthcare provider.
- have a history of depression, mental illness or, suicidal thoughts
- have a history of drug or alcohol abuse or addiction
- have kidney or liver disease
- have lung disease, breathing problems, or sleep apnea
- are pregnant or plan to become pregnant. Triazolam may harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if triazolam can pass through your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take triazolam.
How should I take triazolam?
- See "What is the most important information I should know about triazolam?"
- Take triazolam exactly as your healthcare provider tells you to take it.
- Take triazolam right before you get into bed. Or you can take triazolam after you have been in bed and have trouble falling asleep.
- Do not take triazolam with or right after a meal.
- Do not take triazolam unless you are able to get a full night's sleep before you must be active again.
- If you take too much triazolam, get emergency treatment right away
What should I avoid while taking triazolam?
- Do not drive, operate machinery, do other dangerous activities or do anything that needs you to be alert until you know how triazolam affects you.
- You should not drink alcohol while you are taking triazolam.
What are the possible side effects of triazolam?Triazolam may cause serious side effects, including:
- See "What is the most important information I should know about triazolam?"
- Other conditions. Call your healthcare provider if your insomnia worsens or is not better within 7 to 10 days. This may mean that there is another condition causing your sleep problem.
- Abnormal thoughts and behavior. Symptoms include more outgoing or aggressive behavior than normal, confusion, agitation, hallucinations, worsening of depression, and suicidal thoughts or actions.
- Withdrawal symptoms. You may have withdrawal symptoms for 1 to 2 days when you stop taking triazolam suddenly. Withdrawal symptoms include trouble sleeping, unpleasant feelings, stomach and muscle cramps, vomiting, sweating, shakiness, and seizures. Talk to your healthcare provider about slowly stopping triazolam to avoid withdrawal symptoms.
- Abuse and dependence. Taking triazolam can cause physical and psychological dependence. Physical and psychological dependence is not the same as drug addiction. Your healthcare provider can tell you more about the differences between physical and psychological dependence and drug addiction.
- Memory loss, including "traveler's amnesia"
- Anxiety
- Severe allergic reactions. Symptoms include swelling of the tongue or throat, trouble breathing, nausea and vomiting. Get emergency medical help if you have these symptoms after taking triazolam.
The most common side effects of triazolam include:
- drowsiness
- dizziness
- "pins and needles" feeling on your skin
- headache
- lightheadedness
- difficulty with coordination
You may still feel drowsy the next day after taking triazolam. Do not drive or do other dangerous activities (including operating machinery) after taking triazolam until you feel fully awake. These are not all the possible side effects of triazolam. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store triazolam?
- Store at room temperature between 68°F to 77° F (20°C to 25°C).
- Protect from light.
- Keep triazolam and all medicines out of the reach of children
- Do not use triazolam after the expiration date on the bottle.
General information about the safe and effective use of triazolam.
- Medicines are sometimes prescribed for purposes other than those uled in a Medication Guide.
- Do not use triazolam for a condition for which it was not prescribed.
- Do not give triazolam to other people, even if they have the same symptoms that you have. It may harm them.
- You can ask your healthcare provider or pharmacist for information about triazolam that is written for healthcare professionals.
What are the ingredients in triazolam? Active Ingredient: triazolam Inactive Ingredients: 0.125 mg tablet: cellulose, corn starch, docusate sodium, lactose, magnesium stearate, silicon dioxide, sodium benzoate, 0.25 mg tablet: cellulose, corn starch, docusate sodium, FD&C Blue No. 2, lactose, magnesium stearate, silicon dioxide, sodium benzoate.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
This product's label may have been updated. For current full prescribing information, please visit www.greenstonellc.com.

LAB-0260-10.0January 2017
Repackaging Information
Please reference theHow Supplied section uled above for a description of individual tablets. This drug product has been received by Aphena Pharma - TN in a manufacturer or distributor packaged configuration and repackaged in full compliance with all applicable cGMP regulations. The package configurations available from Aphena are uled below:
Count 0.25 mg 30 43353-451-30 60 43353-451-53
Store between 20°-25°C (68°-77°F). See USP Controlled Room Temperature. Dispense in a tight light-resistant container as defined by USP. Keep this and all drugs out of the reach of children.
Repackaged by:Cookeville, TN 38506 20171116JH
Principal Display Panel - 0.25 Mg
NDC 43353-451 - Triazolam 0.25 mg - Rx Only
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site