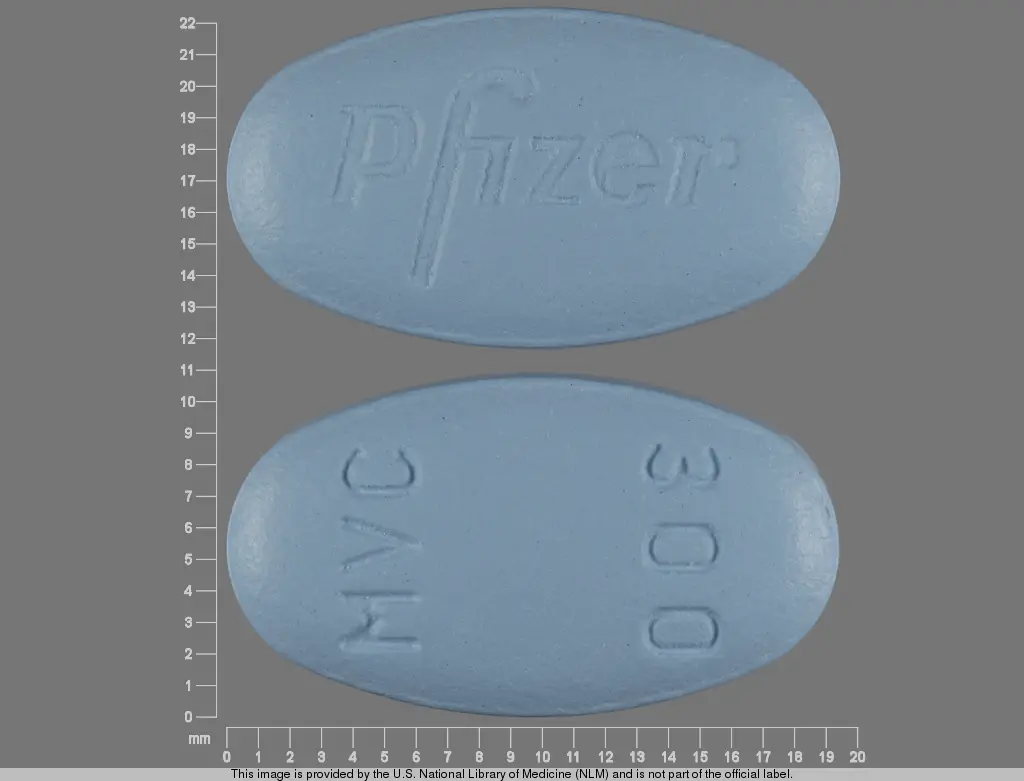
SELZENTRY (maraviroc 300 mg) Dailymed
Generic: maraviroc
IMPRINT: PFIZER MVC300
SHAPE: oval
COLOR: blue
All Imprints
maraviroc 150 mg - pfizer mvc150 oval blue
maraviroc 300 mg - pfizer mvc300 oval blue
Boxed Warning
Boxed Warning Section
- Hepatotoxicity has been reported which may be preceded by evidence of a systemic allergic reaction (e.g., pruritic rash, eosinophilia, or elevated IgE).
- Immediately evaluate patients with signs or symptoms of hepatitis or allergic reaction. (5.1)
Go PRO for all pill images
Recent Major Changes Section
Dosage and Administration (2.2) 05/2010
Contraindications (4) 05/2010
Warnings and Precautions (5.2) 05/2010
Boxed Warning Section
Hepatotoxicity has been reported with use of SELZENTRY. Evidence of a systemic allergic reaction (e.g., pruritic rash, eosinophilia, or elevated IgE) prior to the development of hepatotoxicity may occur. Patients with signs or symptoms of hepatitis or allergic reaction following use of SELZENTRY should be evaluated immediately [see Warnings and Precautions (5.1)].
WARNING: HEPATOTOXICITY
See full prescribing information for complete boxed warning
- Hepatotoxicity has been reported which may be preceded by evidence of a systemic allergic reaction (e.g., pruritic rash, eosinophilia, or elevated IgE).
- Immediately evaluate patients with signs or symptoms of hepatitis or allergic reaction. (5.1)
1 Indications And Usage
SELZENTRY, in combination with other antiretroviral agents, is indicated for adult patients infected with only CCR5-tropic HIV-1.
This indication is based on analyses of plasma HIV-1 RNA levels in 2 controlled studies of SELZENTRY in treatment-experienced subjects and one study in treatment-naive subjects. Both studies in treatment-experienced subjects were conducted in clinically advanced, 3-class antiretroviral-experienced (nucleoside reverse transcriptase inhibitor [NRTI], non-nucleoside reverse transcriptase inhibitor [NNRTI], protease inhibitor [PI], or enfuvirtide) adults with evidence of HIV-1 replication despite ongoing antiretroviral therapy.
The following points should be considered when initiating therapy with SELZENTRY:
- Adult patients infected with only CCR5-tropic HIV-1 should use SELZENTRY.
- Tropism testing must be conducted with a highly sensitive tropism assay that has demonstrated the ability to identify patients appropriate for use of SELZENTRY. Outgrowth of pre-existing low-level CXCR4- or dual/mixed-tropic HIV-1 not detected by tropism testing at screening has been associated with virologic failure on SELZENTRY [see Microbiology (12.4), Clinical Studies (14.3)].
- Use of SELZENTRY is not recommended in subjects with dual/mixed- or CXCR4-tropic HIV-1 as efficacy was not demonstrated in a Phase 2 study of this patient group.
- The safety and efficacy of SELZENTRY have not been established in pediatric patients.
- In treatment-naive subjects, more subjects treated with SELZENTRY experienced virologic failure and developed lamivudine resistance compared with efavirenz [see Microbiology (12.4), Clinical Studies (14.3)].
SELZENTRY is a CCR5 co-receptor antagonist indicated for combination antiretroviral treatment of adults infected with only CCR5-tropic HIV-1.
- In treatment-naive subjects, more subjects treated with SELZENTRY experienced virologic failure and developed lamivudine resistance compared with efavirenz. (12.4,14.3)
- Tropism testing with a highly sensitive tropism assay is required for the appropriate use of SELZENTRY. (1)
2 Dosage And Administration
When given with potent CYP3A inhibitors (with or without potent CYP3A inducers) including PIs (except tipranavir/ritonavir), delavirdine (2, 7.1)
150 mg
twice dailyWith NRTIs, tipranavir/ritonavir, nevirapine, raltegravir, and other drugs that are not potent CYP3A inhibitors or CYP3A inducers (2, 7.1)
300 mg
twice dailyWith potent CYP3A inducers including efavirenz (without a potent CYP3A inhibitor) (2, 7.1)
600 mg
twice daily
A more complete ul of coadministered drugs is uled in Dosage and Administration (2).
Dose adjustment may be necessary in patients with renal impairment. (2.2)
2.1 Dose Recommendations for Patients With Normal Renal Function
The recommended dose of SELZENTRY differs based on concomitant medications due to drug interactions (see Table 1). SELZENTRY can be taken with or without food. SELZENTRY must be given in combination with other antiretroviral medications.
Table 1 gives the recommended dose adjustments [see Drug Interactions (7.1)].
Table 1. Recommended Dosing Regimen Concomitant Medications Dose of SELZENTRY
Potent CYP3A inhibitors (with or without a potent CYP3A inducer) including:
- protease inhibitors (except tipranavir/ritonavir)
- delavirdine
- ketoconazole, itraconazole, clarithromycin
- other potent CYP3A inhibitors (e.g., nefazodone, telithromycin)
150 mg twice daily Other concomitant medications, including tipranavir/ritonavir, nevirapine, raltegravir, all NRTIs, and enfuvirtide 300 mg twice daily
Potent CYP3A inducers (without a potent CYP3A inhibitor) including:
- efavirenz
- rifampin
- etravirine
- carbamazepine, phenobarbital, and phenytoin
600 mg twice daily 2.2 Dose Recommendations for Patients With Renal Impairment
Table 2 provides dosing recommendations for patients based on renal function and concomitant medications.
Table 2. Recommended Dosing Regimens Based on Renal Function Concomitant Medicationsa Dose of SELZENTRY Based on Renal Function
Normal
(CrCl>80 mL/min)
Mild
(CrCl >50 and ‚ȧ80 mL/min)
Moderate
(CrCl ‚Č•30 and ‚ȧ50 mL/min)
Severe
(CrCl <30 mL/min)
End-Stage Renal Disease (ESRD)
On Regular HemodialysisPotent CYP3A inhibitors (with or without a CYP3A inducer)a 150 mg twice daily 150 mg twice daily 150 mg twice daily NR NR Other concomitant medicationsa 300 mg twice daily 300 mg twice daily 300 mg twice daily 300 mg twice dailyb 300 mg twice dailyb Potent CYP3A Inducers (without a potent CYP3A inhibitor)a 600 mg twice daily 600 mg twice daily 600 mg twice daily NR NR
NR = Not recommended.
a See Table 1 for the ul of concomitant medications.
b The dose of SELZENTRY should be reduced to 150 mg twice daily if there are any symptoms of postural hypotension [see Warnings and Precautions (5.2)].
3 Dosage Forms And Strengths
- 150-mg blue, oval, film-coated tablets debossed with ‚ÄúPfizer‚ÄĚ on one side and ‚ÄúMVC 150‚ÄĚ on the other.
- 300-mg blue, oval, film-coated tablets debossed with ‚ÄúPfizer‚ÄĚ on one side and ‚ÄúMVC 300‚ÄĚ on the other.
Tablets: 150 mg and 300 mg (3)
4 Contraindications
SELZENTRY should not be used in patients with severe renal impairment or end-stage renal disease (ESRD) (CrCl <30 mL/min) who are taking potent CYP3A inhibitors or inducers.
- SELZENTRY should not be used in patients with severe renal impairment or end-stage renal disease (ESRD) (CrCl <30 mL/min) who are taking potent CYP3A inhibitors or inducers. (4)
5 Warnings And Precautions
- Use caution when administering SELZENTRY to patients with pre-existing liver dysfunction or who are co-infected with viral hepatitis B or C. (5.1)
- More cardiovascular events including myocardial ischemia and/or infarction were observed in treatment-experienced subjects who received SELZENTRY. Use with caution in patients at increased risk of cardiovascular events. (5.2)
- If patients with severe renal impairment or end-stage renal disease (ESRD) receiving SELZENTRY (without concomitant CYP3A inducers or inhibitors) experience postural hypotension; the dose of SELZENTRY should be reduced from 300 mg twice daily to 150 mg twice daily. (5.2)
5.1 Hepatotoxicity
A case of possible hepatotoxicity with allergic features induced by SELZENTRY has been reported in a study of healthy volunteers. Discontinuation of SELZENTRY should be considered in any patient with signs or symptoms of hepatitis, or with increased liver transaminases combined with rash or other systemic symptoms.
The safety and efficacy of SELZENTRY  have not been specifically studied in patients with significant underlying liver disorders. In studies of treatment-experienced HIV-infected subjects, approximately 6% of subjects were co-infected with hepatitis B and approximately 6% were co-infected with hepatitis C. Due to the small number of co-infected subjects studied, no conclusions can be drawn regarding whether they are at an increased risk for hepatic adverse events with administration of SELZENTRY. However, caution should be used when administering SELZENTRY to patients with pre-existing liver dysfunction or who are co-infected with viral hepatitis B or C.
5.2 Cardiovascular Events
Use with caution in patients at increased risk for cardiovascular events. Eleven subjects (1.3%) who received SELZENTRY had cardiovascular events including myocardial ischemia and/or infarction during the Phase 3 studies in treatment-experienced studies (total exposure 609 patient-years [300 on SELZENTRY once daily + 309 on SELZENTRY twice daily]), while no subjects who received placebo had such events (total exposure 111 patient-years). These subjects generally had cardiac disease or cardiac risk factors prior to use of SELZENTRY, and the relative contribution of SELZENTRY to these events is not known.
In the Phase 2b/3 study in treatment-naive subjects, 3 subjects (0.8%) who received SELZENTRY had events related to ischemic heart diseases and 5 subjects (1.4%) who received efavirenz had such events (total exposure 506 and 508 patient-years for SELZENTRY and efavirenz, respectively).
When SELZENTRY was administered to healthy volunteers at doses higher than the recommended dose, symptomatic postural hypotension was seen at a greater frequency than in placebo. However, when SELZENTRY was given at the recommended dose in HIV subjects in Phase 3 studies, postural hypotension was seen at a rate similar to placebo (approximately 0.5%). Caution should be used when administering SELZENTRY in patients with a history of postural hypotension or on concomitant medication known to lower blood pressure.
Postural Hypotension in Patients With Renal Impairment: Patients with impaired renal function may have cardiovascular co-morbidities and could be at increased risk of cardiovascular adverse events triggered by postural hypotension. An increased risk of postural hypotension may occur in patients with severe renal insufficiency or in those with ESRD due to increased maraviroc exposure in some patients. SELZENTRY should be used in patients with severe renal impairment or ESRD only if they are not receiving a concomitant potent CYP3A inhibitor or inducer. However, the use of SELZENTRY in these patients should only be considered when no alternative treatment options are available. If patients with severe renal impairment or ESRD experience any symptoms of postural hypotension while taking 300 mg twice daily, the dose should be reduced to 150 mg twice daily [see Dosage and Administration (2.2)].
5.3 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including maraviroc. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as infection with Mycobacterium avium, cytomegalovirus, Pneumocystis jirovecii, Mycobacterium tuberculosis, or reactivation of Herpes simplex and Herpes zoster), which may necessitate further evaluation and treatment.
5.4 Potential Risk of Infection
SELZENTRY antagonizes the CCR5 co-receptor located on some immune cells, and therefore could potentially increase the risk of developing infections. The overall incidence and severity of infection, as well as AIDS-defining category C infections, was comparable in the treatment groups during the Phase 3 treatment-experienced studies of SELZENTRY. While there was a higher rate of certain upper respiratory tract infections reported in the arm receiving SELZENTRY compared with placebo (23% versus 13%), there was a lower rate of pneumonia (2% vs 5%) reported in subjects receiving SELZENTRY. A higher incidence of Herpes virus infections (11 per 100 patient-years) was also reported in the arm receiving SELZENTRY when adjusted for exposure compared with placebo (8 per 100 patient-years).
In the Phase 2b/3 study in treatment-naive subjects, the incidence of AIDS-defining Category C events when adjusted for exposure was 1.8 for SELZENTRY compared with 2.4 for efavirenz per 100 patient-years of exposure.
Patients should be monitored closely for evidence of infections while receiving SELZENTRY.
5.5 Potential Risk of Malignancy
While no increase in malignancy has been observed with SELZENTRY, due to this drug’s mechanism of action it could affect immune surveillance and lead to an increased risk of malignancy.
The exposure-adjusted rate for malignancies per 100 patient-years of exposure in treatment-experienced studies was 4.6 for SELZENTRY compared with 9.3 on placebo. In treatment-naive subjects, the rates were 1.0 and 2.4 per 100 patient-years of exposure for SELZENTRY and efavirenz, respectively.
Long-term follow-up is needed to more fully assess this risk.
6 Adverse Reactions
The following adverse reactions are discussed in other sections of the labeling:
- Hepatotoxicity [see Boxed Warning, Warnings and Precautions (5.1)]
- Cardiovascular events [see Warnings and Precautions (5.2)]
The most common adverse events in treatment-experienced subjects (>8% incidence) which occurred at a higher frequency compared with placebo are upper respiratory tract infections, cough, pyrexia, rash, and dizziness. (6)
To report SUSPECTED ADVERSE REACTIONS, contact ViiV Healthcare at 1-877-844-8872 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Studies in Treatment-Experienced Subjects: The safety profile of SELZENTRY  is primarily based on 840 HIV-infected subjects who received at least 1 dose of SELZENTRY during two Phase 3 trials. A total of 426 of these subjects received the indicated twice-daily dosing regimen.
Assessment of treatment-emergent adverse events is based on the pooled data from 2 studies in subjects with CCR5-tropic HIV-1 (A4001027 and A4001028). The median duration of maraviroc therapy for subjects in these studies was 48 weeks, with the total exposure on SELZENTRY twice daily at 309 patient-years versus 111 patient-years on placebo + optimized background therapy (OBT). The population was 89% male and 84% white, with mean age of 46 years (range: 17 to 75 years). Subjects received dose equivalents of 300 mg maraviroc once or twice daily.
The most common adverse events reported with twice-daily therapy with SELZENTRY with frequency rates higher than placebo, regardless of causality, were upper respiratory tract infections, cough, pyrexia, rash, and dizziness. Additional adverse events that occurred with once-daily dosing at a higher rate than both placebo and twice-daily dosing were diarrhea, edema, influenza, esophageal candidiasis, sleep disorders, rhinitis, parasomnias, and urinary abnormalities. In these 2 studies, the rate of discontinuation due to adverse events was 5% for subjects who received SELZENTRY twice daily + OBT as well as those who received placebo + OBT. Most of the adverse events reported were judged to be mild to moderate in severity. The data described below occurred with twice-daily dosing of SELZENTRY.
The total number of subjects reporting infections were 233 (55%) and 84 (40%) in the group receiving SELZENTRY twice daily and the placebo group, respectively. Correcting for the longer duration of exposure on SELZENTRY compared with placebo, the exposure-adjusted frequency (rate per 100 subject-years) of these events was 133 for both SELZENTRY twice daily and placebo.
Dizziness or postural dizziness occurred in 8% of subjects on either SELZENTRY or placebo, with 2 subjects (0.5%) on SELZENTRY permanently discontinuing therapy (1 due to syncope, 1 due to orthostatic hypotension) versus 1 subject on placebo (0.5%) permanently discontinuing therapy due to dizziness.
Treatment-emergent adverse events, regardless of causality, from A4001027 and A4001028 are summarized in Table 3. Selected events occurring at ‚Č•2% of subjects and at a numerically higher rate in subjects treated with SELZENTRY are included; events that occurred at the same or higher rate on placebo are not displayed.
Table 3. Percentage of Subjects With Selected Treatment-Emergent Adverse Events (All Causality)(‚Č•2% on SELZENTRY and at a higher rate compared with placebo) Studies A4001027 and A4001028 (Pooled Analysis, 48 Weeks)
SELZENTRY
Twice DailyaPlacebo
N = 426
(%)
Exposure-adjusted rate
(per 100 pt-yrs)
PYE = 309b
N = 426
(%)
Exposure-adjusted rate
(per 100 pt-yrs)
PYE = 111bEye Disorders Conjunctivitis 2 3 1 3 Ocular infections, inflammations, and associated manifestations 2 3 1 2 Gastrointestinal Disorders Constipation 6 9 3 6 General Disorders and Administration Site Conditions Pyrexia 13 20 9 17 Pain and discomfort 4 5 3 5 Infections and Infestations Upper respiratory tract infection 23 37 13 27 Herpes infection 8 11 4 8 Sinusitis 7 10 3 6 Bronchitis 7 9 5 9 Folliculitis 4 5 2 4 Pneumonia 2 3 5 10 Anogenital warts 2 3 1 3 Influenza 2 3 0.5 1 Otitis media 2 3 0.5 1 Metabolism and Nutrition Disorders Appetite disorders 8 11 7 13 Musculoskeletal and Connective Tissue Disorders Joint-related signs and symptoms 7 10 3 5 Muscle pains 3 4 0.5 1 Neoplasms Benign, Malignant, and Unspecified Skin neoplasms benign 3 4 1 3 Nervous System Disorders Dizziness/postural dizziness 9 13 8 17 Paresthesias and dysesthesias 5 7 3 6 Sensory abnormalities 4 6 1 3 Disturbances in consciousness 4 5 3 6 Peripheral neuropathies 4 5 3 6 Psychiatric Disorders Disturbances in initiating and maintaining sleep 8 11 5 10 Depressive disorders 4 6 3 5 Anxiety symptoms 4 5 3 7 Renal and Urinary Disorders Bladder and urethral symptoms 5 7 1 3 Urinary tract signs and symptoms 3 4 1 3 Respiratory, Thoracic, and Mediastinal Disorders Coughing and associated symptoms 14 21 5 10 Upper respiratory tract signs and symptoms 6 9 3 6 Nasal congestion and inflammations 4 6 3 5 Breathing abnormalities 4 5 2 5 Paranasal sinus disorders 3 4 0.5 1 Skin and Subcutaneous Tissue Disorders Rash 11 16 5 11 Apocrine and eccrine gland disorders 5 7 4 7.5 Pruritus 4 5 2 4 Lipodystrophies 3 5 0.5 1 Erythemas 2 3 1 2 Vascular Disorders Vascular hypertensive disorders 3 4 2 4
a300-mg dose equivalent. 
bPYE = Patient-years of exposure.
Laboratory Abnormalities: Table 4 shows the treatment-emergent Grade 3-4 laboratory abnormalities that occurred in >2% of subjects receiving SELZENTRY.
Table 4. Maximum Shift in Laboratory Test Values (Without Regard to Baseline)
Incidence ‚Č•2% of Grade 3-4 Abnormalities (ACTG Criteria) Studies A4001027 and A4001028 (Pooled Analysis, 48 Weeks)
Laboratory Parameter Preferred Term Limit
SELZENTRY
Twice Daily + OBT
(N = 421)a
%
Placebo + OBT
(N = 207)a
%Aspartate aminotransferase >5.0x ULN 4.8 2.9 Alanine aminotransferase >5.0x ULN 2.6 3.4 Total bilirubin >5.0x ULN 5.5 5.3 Amylase >2.0x ULN 5.7 5.8 Lipase >2.0x ULN 4.9 6.3 Absolute neutrophil count <750/mm3 4.3 2.4
aPercentages based on total subjects evaluated for each laboratory parameter.
Study in Treatment-Naive Subjects: ¬† Treatment-Emergent Adverse Events: Treatment-emergent adverse events, regardless of causality, from Study A4001026, a double-blind, comparative, controlled study in which 721¬†treatment-naive subjects received SELZENTRY 300¬†mg twice daily (N¬†=¬†360) or efavirenz (N¬†=¬†361) in combination with zidovudine/lamivudine for 96¬†weeks, are summarized in Table 5. Selected events occurring at ‚Č•2% of subjects and at a numerically higher rate in subjects treated with SELZENTRY are included; events that occurred at the same or higher rate on efavirenz are not displayed.
Table 5. Percentage of Subjects With Selected Treatment-Emergent Adverse Events (All Causality) (‚Č•2% on SELZENTRY and at a higher rate compared with efavirenz) Study A4001026 (96 Weeks)
SELZENTRY +
Zidovudine/Lamivudine
300 mg Twice Daily
(N = 360)
%
Efavirenz +
Zidovudine/Lamivudine
600 mg Once Daily
(N = 361)
%Blood and Lymphatic System Disorders Anemias NEC 8 5 Neutropenias 4 3 Ear and Labyrinth Disorders Ear disorders NEC 3 2 Gastrointestinal Disorders Flatulence, bloating, and distention 10 7 Gastrointestinal atonic and hypomotility disorders NEC 9 5 Gastrointestinal signs and symptoms NEC 3 2 General Disorders and Administrtion Site Conditions Body temperature perception 3 1 Infections and Infestations Bronchitis 13 9 Herpes infection 7 6 Upper respiratory tract infection 32 30 Bacterial infections NEC 6 3 Herpes zoster/varicella 5 4 Lower respiratory tract and lung infections 3 2 Neisseria infections 3 0 Tinea infections 4 3 Viral infections NEC 3 2 Musculoskeletal and Connective Tissue Disorders Joint-related signs and symptoms 6 5 Nervous System Disorders Memory loss (excluding dementia) 3 1 Paresthesias and dyesthesias 4 3 Renal and Urinary Disorders Bladder and urethral symptoms 4 3 Reproductive System and Breast Disorders Erection and ejaculation conditions and disorders 3 2 Respiratory, Thoracic, and Mediastinal Disorders Upper respiratory tract signs and symptoms 9 5 Skin and Subcutaneous Disorders Acnes 3 2 Alopecias 2 1 Lipodystrophies 4 3 Nail and nail bed conditions (excluding infections and infestations) 6 2
Laboratory Abnormalities:
Table 6. Maximum Shift in Laboratory Test Values (Without Regard to Baseline) Incidence ‚Č•2% of Grade 3-4 Abnormalities (ACTG Criteria) Study A4001026 (96 Weeks) Laboratory Parameter Preferred Term Limit
SELZENTRY
300 mg Twice Daily +
Zidovudine/Lamivudine(N = 353)a
%
Efavirenz
600 mg Once Daily+
Zidovudine/Lamivudine(N = 350)a
%Aspartate aminotransferase >5.0 x ULN 4.0 4.0 Alanine aminotransferase >5.0 x ULN 3.9 4.0 Creatine kinase 3.9 4.8 Amylase >2.0 x ULN 4.3 6.0 Absolute neutrophil count <750/mm3 5.7 4.9 Hemoglobin <7.0 g/dL 2.9 2.3
a N = Total number of subjects evaluable for laboratory abnormalities.
Percentages based on total subjects evaluated for each laboratory parameter. If the same subject in a given treatment group had >1 occurrence of the same abnormality, only the most severe is counted.
Less Common Adverse Events in Clinical Trials: The following adverse events occurred in <2% of subjects treated with SELZENTRY. These events have been included because of their seriousness and either increased frequency on SELZENTRY or are potential risks due to the mechanism of action. Events attributed to the patient’s underlying HIV infection are not uled.
Blood and Lymphatic System: Marrow depression and hypoplastic anemia.
Cardiac Disorders: Unstable angina, acute cardiac failure, coronary artery disease, coronary artery occlusion, myocardial infarction, myocardial ischemia.
Hepatobiliary Disorders: Hepatic cirrhosis, hepatic failure, cholestatic jaundice, portal vein thrombosis, hypertransaminasemia, jaundice.
Infections and Infestations: Endocarditis, infective myositis, viral meningitis, pneumonia, treponema infections, septic shock, Clostridium difficile colitis, meningitis.
Musculoskeletal and Connective Tissue Disorders: Myositis, osteonecrosis, rhabdomyolysis, blood CK increased.
Neoplasms Benign, Malignant, and Unspecified (Including Cysts and Polyps): Abdominal neoplasm, anal cancer, basal cell carcinoma, Bowen’s disease, cholangiocarcinoma, diffuse large B-cell lymphoma, lymphoma, metastases to liver, esophageal carcinoma, nasopharyngeal carcinoma, squamous cell carcinoma, squamous cell carcinoma of skin, tongue neoplasm (malignant stage unspecified), anaplastic large cell lymphomas T- and null-cell types, bile duct neoplasms malignant, endocrine neoplasms malignant and unspecified.
Nervous System Disorders:  Cerebrovascular accident, convulsions and epilepsy, tremor (excluding congenital), facial palsy, hemianopia, loss of consciousness, visual field defect.
6.2 Postmarketing Experience
The following events have been identified during post-approval use of SELZENTRY. Because these reactions are reported voluntarily from a population of unknown size, it is not possible to estimate their frequency or establish a causal relationship to exposure to SELZENTRY.
Skin and Subcutaneous Tissue Disorders: Stevens-Johnson syndrome.
7 Drug Interactions
- Coadministration with CYP3A inhibitors, including protease inhibitors (except tipranavir/ritonavir) and delavirdine, will increase the concentration of SELZENTRY. (7.1)
- Coadministration with CYP3A inducers, including efavirenz, may decrease the concentration of SELZENTRY. (7.1)
7.1 Effect of Concomitant Drugs on the Pharmacokinetics of Maraviroc
Maraviroc is a substrate of CYP3A and Pgp and hence its pharmacokinetics are likely to be modulated by inhibitors and inducers of these enzymes/transporters. Therefore, a dose adjustment may be required when maraviroc is coadministered with those drugs [see Dosage and Administration (2)].
Concomitant use of maraviroc and St. John's wort (hypericum perforatum) or products containing St. John's wort is not recommended. Coadministration of maraviroc with St. John's wort is expected to substantially decrease maraviroc concentrations and may result in suboptimal levels of maraviroc and lead to loss of virologic response and possible resistance to maraviroc.
For additional drug interaction information see Clinical Pharmacology (12.3).
8 Use In Specific Populations
- SELZENTRY should only be used in pregnant women if the potential benefit justifies the potential risk to the fetus. (8.1)
- There are no data available in pediatric patients; therefore, SELZENTRY should not be used in patients aged <16 years. (8.4)
8.1 Pregnancy
Pregnancy Category B: The incidence of fetal variations and malformations was not increased in embryofetal toxicity studies performed with maraviroc in rats at exposures (AUC) approximately 20-fold higher and in rabbits at approximately 5-fold higher than human exposures at the recommended daily dose (up to 1,000 mg/kg/day in rats and 75 mg/kg/day in rabbits). During the pre- and postnatal development studies in the offspring, development of the offspring, including fertility and reproductive performance, was not affected by the maternal administration of maraviroc.
However, there are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, SELZENTRY should be used during pregnancy only if clearly needed.
Antiretroviral Pregnancy Registry: To monitor maternal-fetal outcomes of pregnant women exposed to SELZENTRY and other antiretroviral agents, an Antiretroviral Pregnancy Registry has been established. Physicians are encouraged to register patients by calling 1-800-258-4263.
8.3 Nursing Mothers
The Centers for Disease Control and Prevention recommend that HIV-infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV infection. Studies in lactating rats indicate that maraviroc is extensively secreted into rat milk. It is not known whether maraviroc is secreted into human milk. Because of the potential for both HIV transmission and serious adverse reactions in nursing infants, mothers should be instructed not to breastfeed if they are receiving SELZENTRY.
8.4 Pediatric Use
The pharmacokinetics, safety and efficacy of maraviroc in patients aged <16 years have not been established. Therefore, maraviroc should not be used in this patient population.
8.5 Geriatric Use
  There were insufficient numbers of subjects aged 65 and over in the clinical studies to determine whether they respond differently from younger subjects. In general, caution should be exercised when administering SELZENTRY in elderly patients, also reflecting the greater frequency of decreased hepatic and renal function, of concomitant disease and other drug therapy.
8.6 Renal Impairment
¬† Recommended doses of SELZENTRY for patients with impaired renal function (CrCl¬†‚ȧ80¬†mL/min) are based on the results of a pharmacokinetic study conducted in healthy subjects with various degrees of renal impairment. The pharmacokinetics of maraviroc in subjects with mild and moderate renal impairment was similar to that in subjects with normal renal function [see Clinical Pharmacology (12.3)]. A limited number of subjects with mild and moderate renal impairment in the Phase 3 clinical trials (n¬†=¬†131 and n¬†=¬†12, respectively) received the same dose of SELZENTRY as that administered to subjects with normal renal function. In these subjects there was no apparent difference in the adverse event profile for maraviroc compared with subjects with normal renal function.
If patients with severe renal impairment or ESRD not receiving a concomitant potent CYP3A inhibitor or inducer experience any symptoms of postural hypotension while taking SELZENTRY 300 mg twice daily, the dose should be reduced to 150 mg twice daily. No studies have been performed in subjects with severe renal impairment or ESRD co-treated with potent CYP3A inhibitors or inducers. Hence, no dose of SELZENTRY can be recommended, and SELZENTRY is contraindicated for these patients [see Dosage and Administration (2.2), Contraindications (4), Warnings and Precautions (5.2), Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Maraviroc is principally metabolized by the liver; therefore, caution should be exercised when administering this drug to patients with hepatic impairment, because maraviroc concentrations may be increased. Maraviroc concentrations are higher when SELZENTRY 150 mg is administered with a potent CYP3A inhibitor compared with following administration of 300 mg without a CYP3A inhibitor, so patients with moderate hepatic impairment who receive SELZENTRY 150 mg with a potent CYP3A inhibitor should be monitored closely for maraviroc-associated adverse events. Maraviroc has not been studied in subjects with severe hepatic impairment [see Warnings and Precautions (5.1), Clinical Pharmacology (12.3)].
8.8 Gender
Population pharmacokinetic analysis of pooled Phase 1/2a data indicated gender (female: n = 96, 23.2% of the total population) does not affect maraviroc concentrations. Dosage adjustment based on gender is not necessary.
8.9 Race
Population pharmacokinetic analysis of pooled Phase 1/2a data indicated exposure was 26.5% higher in Asians (N = 95) as compared with non-Asians (n = 318). However, a study designed to evaluate pharmacokinetic differences between Caucasians (n = 12) and Singaporeans (n = 12) showed no difference between these 2 populations. No dose adjustment based on race is needed.
10 Overdosage
The highest dose administered in clinical studies was 1,200 mg. The dose-limiting adverse event was postural hypotension, which was observed at 600 mg. While the recommended dose for SELZENTRY in patients receiving a CYP3A inducer without a CYP3A inhibitor is 600 mg twice daily, this dose is appropriate due to enhanced metabolism.
Prolongation of the QT interval was seen in dogs and monkeys at plasma concentrations 6 and 12 times, respectively, those expected in humans at the intended exposure of 300 mg equivalents twice daily. However, no significant QT prolongation was seen in the studies in treatment-experienced subjects with HIV using the recommended doses of maraviroc or in a specific pharmacokinetic study to evaluate the potential of maraviroc to prolong the QT interval [see Clinical Pharmacology (12.3)].
There is no specific antidote for overdose with maraviroc. Treatment of overdose should consist of general supportive measures including keeping the patient in a supine position, careful assessment of patient vital signs, blood pressure, and ECG.
If indicated, elimination of unabsorbed active maraviroc should be achieved by emesis or gastric lavage. Administration of activated charcoal may also be used to aid in removal of unabsorbed drug. Since maraviroc is moderately protein-bound, dialysis may be beneficial in removal of this medicine.
11 Description
SELZENTRY (maraviroc) is a selective, slowly reversible, small molecule antagonist of the interaction between human CCR5 and HIV-1 gp120. Blocking this interaction prevents CCR5-tropic HIV-1 entry into cells.
SELZENTRY is available as film-coated tablets for oral administration containing either 150 or 300¬†mg of maraviroc and the following inactive ingredients: dibasic calcium phosphate (anhydrous), magnesium stearate, microcrystalline cellulose, and sodium starch glycolate. The film coat [Opadry¬ģ II Blue (85G20583)] contains FD&C blue #2 aluminum lake, soya lecithin, polyethylene glycol (macrogol 3350), polyvinyl alcohol, talc, and titanium dioxide.¬†
Maraviroc is chemically described as 4,4-difluoro-N-{(1S)-3-[exo-3-(3-isopropyl-5-methyl-4H-1,2,4-triazol-4-yl)-8-azabicyclo[3.2.1]oct-8-yl]-1-phenylpropyl}cyclohexanecarboxamide.
The molecular formula is C29H41F2N5O and the structural formula is:
![]()
Maraviroc is a white- to pale-colored powder with a molecular weight of 513.67. It is highly soluble across the physiological pH range (pH 1.0 to 7.5).
12 Clinical Pharmacology
12.1 Mechanism of Action
Maraviroc is an antiviral drug [see Clinical Pharmacology (12.4)].
12.2 Pharmacodynamics
  Exposure-Response Relationship in Treatment-Experienced Subjects: The relationship between maraviroc, modeled plasma trough concentration (Cmin) (1 to 9 samples per patient taken on up to 7 visits), and virologic response was evaluated in 973 treatment-experienced HIV-1-infected subjects with varied optimized background antiretroviral regimens in Studies A4001027 and A4001028. The Cmin, baseline viral load, baseline CD4+ cell count, and overall sensitivity score (OSS) were found to be important predictors of virologic success (defined as viral load <400 copies/mL at 24 weeks). Table 7 illustrates the proportions of subjects with virologic success (%) within each Cmin quartile for 150-mg twice-daily and 300-mg twice-daily groups.
Table 7. Treatment-Experienced Subjects With Virologic Success by Cmin Quartile (Q1-Q4)) 150 mg Twice Daily(With CYP3A Inhibitors) 300 mg Twice Daily(Without CYP3A Inhibitors) n Median Cmin % Subjects With Virologic Success n Median Cmin % Subjects With Virologic Success Placebo 160 - 30.6 35 - 28.6 Q1 78 33 52.6 22 13 50.0 Q2 77 87 63.6 22 29 68.2 Q3 78 166 78.2 22 46 63.6 Q4 78 279 74.4 22 97 68.2
  Exposure-Response Relationship in Treatment-Naive Subjects: The relationship between maraviroc, modeled plasma trough concentration (Cmin) (1 to 12 samples per patient taken on up to 8 visits), and virologic response was evaluated in 294 treatment-naive HIV-1-infected subjects receiving maraviroc 300 mg twice daily in combination with zidovudine/lamivudine in Study A4001026. Table 8 illustrates the proportion (%) of subjects with virologic success <50 copies/mL at 48 weeks within each Cmin quartile for the 300-mg twice-daily dose.
Table 8. Treatment-Naive Subjects With Virologic Success by Cmin Quartile (Q1-Q4) 300 mg Twice Daily n Median Cmin % Subjects With Virologic Success Q1 75 23 57.3 Q2 72 39 72.2 Q3 73 56 74.0 Q4 74 81 83.8
Eighteen of 75 (24%) subjects in Q1 had no measurable maraviroc concentration on at least one occasion vs. 1 of 73 and 1 of 74 in Q3 and Q4, respectively.
¬† Effects on Electrocardiogram: A placebo-controlled, randomized, crossover study to evaluate the effect on the QT interval of healthy male and female volunteers was conducted with 3¬†single oral doses of maraviroc and moxifloxacin. The placebo-adjusted mean maximum (upper 1-sided 95% CI) increases in QTc from baseline after 100, 300, and 900¬†mg of maraviroc were ‚Äď2 (0), -1 (1), and 1 (3) msec, respectively, and 13 (15) msec for moxifloxacin 400¬†mg. No subject in any group had an increase in QTc of ‚Č•60¬†msec from baseline. No subject experienced an interval exceeding the potentially clinically relevant threshold of 500¬†msec.
12.3 Pharmacokinetics
 
Table 9. Mean Maraviroc Pharmacokinetic Parameters Patient Population Maraviroc Dose N AUC12 (ng.hr/mL) Cmax (ng/mL) Cmin (ng/mL) Healthy volunteers (Phase 1) 300 mg twice daily 64 2,908 888 43.1 Asymptomatic HIV subjects (Phase 2a) 300 mg twice daily 8 2,550 618 33.6 Treatment-experienced HIV subjects (Phase 3)a 300 mg twice daily 94 1,513 266 37.2
150 mg twice daily
(+ CYP3A inhibitor)375 2,463 332 101 Treatment-naive HIV subjects (Phase 2b/3)a 300 mg twice daily 344 1,865 287 60
a The estimated exposure is lower compared with other studies possibly due to sparse sampling, food effect, compliance, and concomitant medications.
Absorption: Peak maraviroc plasma concentrations are attained 0.5 to 4 hours following single oral doses of 1 to 1,200 mg administered to uninfected volunteers. The pharmacokinetics of oral maraviroc are not dose proportional over the dose range.
The absolute bioavailability of a 100-mg dose is 23% and is predicted to be 33% at 300 mg. Maraviroc is a substrate for the efflux transporter P-glycoprotein.
Effect of Food on Oral Absorption: Coadministration of a 300-mg tablet with a high-fat breakfast reduced maraviroc Cmax and AUC by 33% in healthy volunteers. There were no food restrictions in the studies that demonstrated the efficacy and safety of maraviroc [see Clinical Studies (14)]. Therefore, maraviroc can be taken with or without food at the recommended dose [see Dosage and Administration (2)].
Distribution: Maraviroc is bound (approximately 76%) to human plasma proteins, and shows moderate affinity for albumin and alpha-1 acid glycoprotein. The volume of distribution of maraviroc is approximately 194 L.
Metabolism: Studies in humans and in vitro studies using human liver microsomes and expressed enzymes have demonstrated that maraviroc is principally metabolized by the cytochrome P450 system to metabolites that are essentially inactive against HIV-1. In vitro studies indicate that CYP3A is the major enzyme responsible for maraviroc metabolism. In vitro studies also indicate that polymorphic enzymes CYP2C9, CYP2D6, and CYP2C19 do not contribute significantly to the metabolism of maraviroc.
Maraviroc is the major circulating component (~42% drug-related radioactivity) following a single oral dose of 300 mg [14C]-maraviroc. The most significant circulating metabolite in humans is a secondary amine (~22% radioactivity) formed by N-dealkylation. This polar metabolite has no significant pharmacological activity. Other metabolites are products of mono-oxidation and are only minor components of plasma drug-related radioactivity.
Excretion: The terminal half-life of maraviroc following oral dosing to steady state in healthy subjects was 14 to 18 hours. A mass balance/excretion study was conducted using a single 300-mg dose of 14C-labeled maraviroc. Approximately 20% of the radiolabel was recovered in the urine and 76% was recovered in the feces over 168 hours. Maraviroc was the major component present in urine (mean of 8% dose) and feces (mean of 25% dose). The remainder was excreted as metabolites.
Hepatic Impairment: Maraviroc is primarily metabolized and eliminated by the liver. A study compared the pharmacokinetics of a single 300-mg dose of SELZENTRY in subjects with mild (Child-Pugh Class A, n = 8), and moderate (Child-Pugh Class B, n = 8) hepatic impairment to pharmacokinetics in healthy subjects (n = 8). The mean Cmax and AUC were 11% and 25% higher, respectively, for subjects with mild hepatic impairment, and 32% and 46% higher, respectively, for subjects with moderate hepatic impairment compared with subjects with normal hepatic function. These changes do not warrant a dose adjustment. Maraviroc concentrations are higher when SELZENTRY 150 mg is administered with a potent CYP3A inhibitor compared with following administration of 300 mg without a CYP3A inhibitor, so patients with moderate hepatic impairment who receive SELZENTRY 150 mg with a potent CYP3A inhibitor should be monitored closely for maraviroc-associated adverse events. The pharmacokinetics of maraviroc have not been studied in subjects with severe hepatic impairment [see Warnings and Precautions (5.1)].
Renal Impairment: A study compared the pharmacokinetics of a single 300-mg dose of SELZENTRY in subjects with severe renal impairment (CLcr <30 mL/min, n= 6) and ESRD (n = 6) to healthy volunteers (n = 6). Geometric mean ratios for maraviroc Cmax and AUCinf were 2.4-fold and 3.2-fold higher, respectively, for subjects with severe renal impairment, and 1.7-fold and 2.0-fold higher, respectively, for subjects with ESRD as compared with subjects with normal renal function in this study. Hemodialysis had a minimal effect on maraviroc clearance and exposure in subjects with ESRD. Exposures observed in subjects with severe renal impairment and ESRD were within the range observed in previous 300-mg single-dose studies of SELZENTRY in healthy volunteers with normal renal function. However, maraviroc exposures in the subjects with normal renal function in this study were 50% lower than that observed in previous studies. Based on the results of this study, no dose adjustment is recommended for patients with renal impairment receiving SELZENTRY without a potent CYP3A inhibitor or inducer. However, if patients with severe renal impairment or ESRD experience any symptoms of postural hypotension while taking SELZENTRY 300 mg twice daily, their dose should be reduced to 150 mg twice daily [see Dosage and Administration (2.2); Warnings and Precautions (5.2)].
In addition, the study compared the pharmacokinetics of multiple-dose SELZENTRY in combination with saquinavir/ritonavir 1,000/100¬†mg twice daily (a potent CYP3A inhibitor combination) for 7¬†days in subjects with mild renal impairment (CLcr >50 and ‚ȧ80¬†mL/min, n¬†=¬†6) and moderate renal impairment (CLcr ‚Č•30 and ‚ȧ50¬†mL/min, n¬†=¬†6) to healthy volunteers with normal renal function (n¬†=¬†6). Subjects received 150¬†mg of SELZENTRY at different dose frequencies (healthy volunteers ‚Äď every 12¬†hours; mild renal impairment ‚Äď every 24¬†hours; moderate renal impairment ‚Äď every 48¬†hours). Compared with healthy volunteers (dosed every 12¬†hours), geometric mean ratios for maraviroc AUCtau, Cmax, and Cmin were 50% higher, 20% higher, and 43% lower, respectively for subjects with mild renal impairment (dosed every 24¬†hours). Geometric mean ratios for maraviroc AUCtau, Cmax, and Cmin were 16% higher, 29% lower, and 85% lower, respectively for subjects with moderate renal impairment (dosed every 48¬†hours) compared with healthy volunteers (dosed every 12¬†hours). Based on the data from this study, no adjustment in dose is recommended for patients with mild or moderate renal impairment [see Dosage and Administration (2.2)].
¬† Effect of Concomitant Drugs on the Pharmacokinetics of Maraviroc: Maraviroc is a substrate of CYP3A and Pgp and hence its pharmacokinetics are likely to be modulated by inhibitors and inducers of these enzymes/transporters. The CYP3A/Pgp inhibitors ketoconazole, lopinavir/ritonavir, ritonavir, darunavir/ritonavir, saquinavir/ritonavir, and atazanavir ¬Ī ritonavir all increased the Cmax and AUC of maraviroc (see Table 10). The CYP3A inducers rifampin, etravirine, and efavirenz decreased the Cmax and AUC of maraviroc (see Table 10).
Tipranavir/ritonavir (net CYP3A inhibitor/Pgp inducer) did not affect the steady-state pharmacokinetics of maraviroc (see Table 10). Cotrimoxazole and tenofovir did not affect the pharmacokinetics of maraviroc.
 
Table 10. Effect of Coadministered Agents on the Pharmacokinetics of Maraviroc
Coadministered Drug
and DoseN Maraviroc Dose
Ratio (90% CI) of Maraviroc Pharmacokinetic Parameters With/Without Coadministered Drug
(No Effect = 1.00)Cmin AUCtau Cmax CYP3A and/or P-gp Inhibitors
Ketoconazole
400 mg q.d.12 100 mg b.i.d.
3.75
(3.01, 4.69)
5.00
(3.98, 6.29)
3.38
(2.38, 4.78)
Ritonavir
100 mg b.i.d.8 100 mg b.i.d.
4.55
(3.37, 6.13)
2.61
(1.92, 3.56)
1.28
(0.79, 2.09)
Saquinavir (soft gel capsules) /ritonavir
1,000 mg/100 mg b.i.d.11 100 mg b.i.d.
11.3
(8.96, 14.1)
9.77
(7.87, 12.14)
4.78
(3.41, 6.71)
Lopinavir/ritonavir
400 mg/100 mg b.i.d.11 300 mg b.i.d.
9.24
(7.98, 10.7)
3.95
(3.43, 4.56)
1.97
(1.66, 2.34)
Atazanavir
400 mg q.d.12 300 mg b.i.d.
4.19
(3.65, 4.80)
3.57
(3.30, 3.87)
2.09
(1.72, 2.55)
Atazanavir/ritonavir
300 mg/100 mg q.d.12 300 mg b.i.d.
6.67
(5.78, 7.70)
4.88
(4.40, 5.41)
2.67
(2.32, 3.08)
Darunavir/ritonavir
600 mg/100 mg b.i.d.12 150 mg b.i.d.
8.00
(6.35, 10.1)
4.05
2.94, 5.59
2.29
(1.46, 3.59)CYP3A and/or P-gp Inducers
Efavirenz
600 mg q.d.12 100 mg b.i.d.
0.55
(0.43, 0.72)
0.552
(0.492, 0.620)
0.486
(0.377, 0.626)
Efavirenz
600 mg q.d.
12
200 mg b.i.d.
(+efavirenz):
100 mg b.i.d. (alone)
1.09
(0.89, 1.35)
1.15
(0.98, 1.35)
1.16
(0.87, 1.55)
Rifampicin
600 mg q.d.12 100 mg b.i.d.
0.22
(0.17, 0.28)
0.368
(0.328, 0.413)
0.335
(0.260, 0.431)
Rifampicin
600 mg q.d.12
200 mg b.i.d.
(+rifampicin):
100 mg b.i.d. (alone)
0.66
(0.54, 0.82)
1.04
(0.89, 1.22)
0.97
(0.72, 1.29)
Etravirine
200 mg b.i.d.14 300 mg b.i.d.
0.609
(0.525, 0.707)
0.468
(0.381, 0.576)
0.400
(0.282, 0.566)
Nevirapinea
200 mg b.i.d. (+ lamivudine 150 mg b.i.d., tenofovir 300 mg q.d.)8 300 mg SD -
1.01
(0.65, 1.55)
1.54
(0.94, 2.51)CYP3A and/or P-gp Inhibitors and Inducers
Lopinavir/ritonavir + efavirenz
400 mg/100 mg b.i.d. + 600 mg q.d.11 300 mg b.i.d.
6.29
(4.72, 8.39)
2.53
(2.24, 2.87)
1.25
(1.01, 1.55)
Saquinavir(soft gel capsules) /ritonavir + efavirenz
1000 mg/100 mg b.i.d. + 600 mg q.d.11 100 mg b.i.d.
8.42
(6.46, 10.97)
5.00
(4.26, 5.87)
2.26
(1.64, 3.11)
Darunavir/ritonavir + etravirine
600 mg/100 mg b.i.d. + 200 mg b.i.d.10 150 mg b.i.d.
5.27
(4.51, 6.15)
3.10
(2.57, 3.74)
1.77
(1.20, 2.60)
Tipranavir/ritonavir
500 mg/200 mg b.i.d.12 150 mg b.i.d.
1.80
(1.55, 2.09)
1.02
(0.850, 1.23)
0.86
(0.61, 1.21)Other
Raltegravir
400 mg b.i.d.17 300 mg b.i.d.
0.90
(0.85, 0.96)
0.86
(0.80, 0.92)
0.79
(0.67, 0.94)
aCompared with historical data.
  Effect of Maraviroc on the Pharmacokinetics of Concomitant Drugs: Maraviroc is unlikely to inhibit the metabolism of coadministered drugs metabolized by the following cytochrome P enzymes (CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP3A) because maraviroc did not inhibit activity of those enzymes at clinically relevant concentrations in vitro. Maraviroc does not induce CYP1A2 in vitro.
In vitro results indicate that maraviroc could inhibit P-glycoprotein in the gut and may thus affect bioavailability of certain drugs.
Drug interaction studies were performed with maraviroc and other drugs likely to be coadministered or commonly used as probes for pharmacokinetic interactions (see Table 6). Maraviroc had no effect on the pharmacokinetics of zidovudine or lamivudine. Maraviroc decreased the Cmin and AUC of raltegravir by 27% and 37%, respectively, which is not clinically significant. Maraviroc had no clinically relevant effect on the pharmacokinetics of midazolam, the oral contraceptives ethinylestradiol and levonorgestrel, no effect on the urinary 6ő≤-hydroxycortisol/cortisol ratio, suggesting no induction of CYP3A in vivo. Maraviroc had no effect on the debrisoquine metabolic ratio (MR) at 300¬†mg twice daily or less in vivo and did not cause inhibition of CYP2D6 in vitro until concentrations >100¬†¬ĶM. However, there was 234% increase in debrisoquine MR on treatment compared with baseline at 600¬†mg once daily, suggesting potential inhibition of CYP2D6 at higher dose.
12.4 Microbiology
Mechanism of Action: Maraviroc is a member of a therapeutic class called CCR5 co-receptor antagonists. Maraviroc selectively binds to the human chemokine receptor CCR5 present on the cell membrane, preventing the interaction of HIV-1 gp120 and CCR5 necessary for CCR5-tropic HIV-1 to enter cells.  CXCR4-tropic and dual-tropic HIV-1 entry is not inhibited by maraviroc.
Antiviral Activity in Cell Culture: Maraviroc inhibits the replication of CCR5-tropic laboratory strains and primary isolates of HIV-1 in models of acute peripheral blood leukocyte infection. The mean EC50 value (50% effective concentration) for maraviroc against HIV-1 group M isolates (subtypes A to J and circulating recombinant form AE) and group O isolates ranged from 0.1 to 4.5 nM (0.05 to 2.3 ng/mL) in cell culture.
When used with other antiretroviral agents in cell culture, the combination of maraviroc was not antagonistic with NNRTIs (delavirdine, efavirenz, and nevirapine), NRTIs (abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir, zalcitabine, and zidovudine), or protease inhibitors (amprenavir, atazanavir, darunavir, indinavir, lopinavir, nelfinavir, ritonavir, saquinavir, and tipranavir). Maraviroc was additive/synergistic with the HIV fusion inhibitor enfuvirtide. Maraviroc was not active against CXCR4-tropic and dual-tropic viruses (EC50 value >10¬†¬ĶM). The antiviral activity of maraviroc against HIV-2 has not been evaluated.
Resistance in Cell Culture: HIV-1 variants with reduced susceptibility to maraviroc have been selected in cell culture, following serial passage of 2 CCR5-tropic viruses (CC1/85 and RU570). The maraviroc-resistant viruses remained CCR5-tropic with no evidence of a change from a CCR5-tropic virus to a CXCR4-using virus. Two amino acid residue substitutions in the V3-loop region of the HIV-1 envelope glycoprotein (gp160), A316T, and I323V (HXB2 numbering), were shown to be necessary for the maraviroc-resistant phenotype in the HIV-1 isolate CC1/85. In the RU570 isolate a 3-amino acid residue deletion in the V3 loop, őĒQAI (HXB2 positions 315 to 317), was associated with maraviroc resistance. The relevance of the specific gp120 mutations observed in maraviroc-resistant isolates selected in cell culture to clinical maraviroc resistance is not known. Maraviroc-resistant viruses were characterized phenotypically by concentration-response curves that did not reach 100% inhibition in phenotypic drug assays, rather than increases in EC50 values.
Cross-Resistance in Cell Culture: Maraviroc had antiviral activity against HIV-1 clinical isolates resistant to NNRTIs, NRTIs, PIs, and the fusion inhibitor enfuvirtide in cell culture (EC50 values ranged from 0.7 to 8.9 nM (0.36 to 4.57 ng/mL). Maraviroc-resistant viruses that emerged in cell culture remained susceptible to the enfuvirtide and the protease inhibitor saquinavir.
Clinical Resistance: Virologic failure on maraviroc can result from genotypic and phenotypic resistance to maraviroc, through outgrowth of undetected CXCR4-using virus present before maraviroc treatment (see Tropism below), through resistance to background therapy drugs (Table 11), or due to low exposure to maraviroc [see Clinical Pharmacology (12.2)].
Antiretroviral Treatment-Experienced Subjects (Studies A4001027 and A4001028): Week 48 data from treatment-experienced subjects failing maraviroc-containing regimens with CCR5-tropic virus (n¬†=¬†58) have identified 22¬†viruses that had decreased susceptibility to maraviroc characterized in phenotypic drug assays by concentration-response curves that did not reach 100% inhibition. Additionally, CCR5-tropic virus from 2 of these treatment-failure subjects had ‚Č•3-fold shifts in EC50 values for maraviroc at the time of failure.
Fifteen of these viruses were sequenced in the gp120 encoding region and multiple amino acid substitutions with unique patterns in the heterogeneous V3 loop region were detected. Changes at either amino acid position 308 or 323 (HXB2 numbering) were seen in the V3 loop in 7 of the subjects with decreased maraviroc susceptibility. Substitutions outside the V3 loop of gp120 may also contribute to reduced susceptibility to maraviroc.
Antiretroviral Treatment-Naive Subjects (Study A4001026): Treatment-naive subjects receiving SELZENTRY had more virologic failures and more treatment-emergent resistance to the background regimen drugs compared with those receiving efavirenz (Table 11).
 
Table 11. Development of Resistance to MVC or EFV and Background Drugs in Antiretroviral Treatment-Naive Trial A4001026 for Patients with CCR5-Tropic Virus at Screening Using Enhanced Sensitivity Trofile¬ģ Assay MVC EFV Total N in Dataset (As-Treated) 273 241 Total Virologic Failures (As-Treated) 85(31%) 56 (23%) Evaluable Virologic Failures With Post Baseline Genotypic and Phenotypic Data 73 43
- Lamivudine Resistance
39 (53%) 13 (30%)
- Zidovudine Resistance
2 (3%) 0
- Efavirenz Resistance
-- 23 (53%)
- Phenotypic Resistance to MVCa
19 (26 % )
a Includes subjects failing with CXCR4- or dual/mixed-tropism because these viruses are not intrinsically susceptible to maraviroc.
¬† In an as-treated analysis of treatment-naive subjects at 96¬†weeks, 32¬†subjects failed a maraviroc-containing regimen with CCR5-tropic virus and had a tropism result at failure; 7 of these subjects had evidence of maraviroc phenotypic resistance defined as concentration-response curves that did not reach 95% inhibition. One additional subject had a ‚Č•3-fold shift in the EC50 value for maraviroc at the time of failure. A clonal analysis of the V3 loop amino acid envelope sequences was performed from 6 of the 7¬†subjects. Changes in V3 loop amino acid sequence differed between each of these different subjects, even for those infected with the same virus clade suggesting that that there are multiple diverse pathways to maraviroc resistance. The subjects who failed with CCR5-tropic virus and without a detectable maraviroc shift in susceptibility were not evaluated for genotypic resistance.
Of the 32 maraviroc virologic failures failing with CCR5-tropic virus, 20(63%) also had genotypic and/or phenotypic resistance to background drugs in the regimen (lamivudine, zidovudine).
Tropism: In both treatment-experienced and treatment-naive subjects, detection of CXCR4-using virus prior to initiation of therapy has been associated with a reduced virologic response to maraviroc.
Antiretroviral Treatment-Experienced Subjects: In the majority of cases, treatment failure on maraviroc was associated with detection of CXCR4-using virus (i.e., CXCR4- or dual/mixed-tropic) which was not detected by the tropism assay prior to treatment. CXCR4-using virus was detected at failure in approximately 55% of subjects who failed treatment on maraviroc by Week 48, as compared with 9% of subjects who experienced treatment failure in the placebo arm. To investigate the likely origin of the on-treatment CXCR4-using virus, a detailed clonal analysis was conducted on virus from 20 representative subjects (16 subjects from the maraviroc arms and 4 subjects from the placebo arm) in whom CXCR4-using virus was detected at treatment failure. From analysis of amino acid sequence differences and phylogenetic data, it was determined that CXCR4-using virus in these subjects emerged from a low level of pre-existing CXCR4-using virus not detected by the tropism assay (which is population-based) prior to treatment rather than from a coreceptor switch from CCR5-tropic virus to CXCR4-using virus resulting from mutation in the virus.
Detection of CXCR4-using virus prior to initiation of therapy has been associated with a reduced virological response to maraviroc. Furthermore, subjects failing maraviroc twice daily at Week 48 with CXCR4-using virus had a lower median increase in CD4+ cell counts from baseline (+41 cells/mm3) than those subjects failing with CCR5-tropic virus (+162 cells/mm3). The median increase in CD4+ cell count in subjects failing in the placebo arm was +7 cells/mm3.
Antiretroviral Treatment-Naive Subjects: In a 96-week study of antiretroviral treatment-naive subjects, 14% (12/85) who had CCR5-tropic virus at screening with an enhanced sensitivity tropism assay (Trofile¬ģ) and failed therapy on maraviroc had CXCR4-using virus at the time of treatment failure. A detailed clonal analysis was conducted in 2¬†previously antiretroviral treatment-naive subjects enrolled in a Phase 2a monotherapy study who had CXCR4-using virus detected after 10¬†days treatment with maraviroc. Consistent with the detailed clonal analysis conducted in treatment-experienced subjects, the CXCR4-using variants appear to emerge from outgrowth of a pre-existing undetected CXCR4-using virus. Screening with an enhanced sensitivity tropism assay reduced the number of maraviroc virologic failures with CXCR4- or dual/mixed-tropic virus at failure to 12 compared with 24 when screening with the original tropism assay. All but one (11/12; 92%) of the maraviroc failures failing with CXCR4 or dual/mixed-tropic virus also had genotypic and phenotypic resistance to the background drug lamivudine at failure and 33% (4 /12) developed zidovudine-associated resistance substitutions.
Subjects who had CCR5-tropic virus at baseline and failed maraviroc therapy with CXCR4-using virus had a median increase in CD4+ cell counts from baseline of +113 cells/mm3 while those subjects failing with CCR5-tropic virus had an increase of +135 cells/mm3. The median increase in CD4+ cell count in subjects failing in the efavirenz arm was + 95 cells/mm3.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: Long-term oral carcinogenicity studies of maraviroc were carried out in rasH2 transgenic mice (6 months) and in rats for up to 96 weeks (females) and 104 weeks (males). No drug-related increases in tumor incidence were found in mice at 1,500 mg/kg/day and in male and female rats at 900 mg/kg/day. The highest exposures in rats were approximately 11 times those observed in humans at the therapeutic dose of 300 mg twice daily for the treatment of HIV-1 infection.
Mutagenesis: Maraviroc was not genotoxic in the reverse mutation bacterial test (Ames test in Salmonella and E. coli), a chromosome aberration test in human lymphocytes and rat bone marrow micronucleus test.
Impairment of Fertility: Maraviroc did not impair mating or fertility of male or female rats and did not affect sperm of treated male rats at approximately 20-fold higher exposures (AUC) than in humans given the recommended 300-mg twice daily dose.
14 Clinical Studies
The clinical efficacy and safety of SELZENTRY is derived from analyses of data from 3 ongoing studies in adult subjects infected with CCR5-tropic HIV-1: A4001027 and A4001028 in antiretroviral treatment-experienced adult subjects and A4001026 in treatment-naive subjects. These studies are supported by a 48-week study in antiretroviral treatment-experienced adult subjects infected with dual/mixed-tropic HIV-1, A4001029.
14.1 Studies in CCR5-Tropic, Treatment-Experienced Subjects
Studies A4001027 and A4001028 are ongoing, double-blind, randomized, placebo-controlled, multicenter studies in subjects infected with CCR5-tropic HIV-1. Subjects were required to have an HIV-1 RNA of greater than 5,000¬†copies/mL despite at least 6¬†months of prior therapy with at least 1¬†agent from 3 of the 4¬†antiretroviral drug classes (‚Č•1¬†NRTI, ‚Č•1¬†NNRTI, ‚Č•2¬†PIs, and/or enfuvirtide) or documented resistance to at least 1¬†member of each class. All subjects received an optimized background regimen consisting of 3 to 6 antiretroviral agents (excluding low-dose ritonavir) selected on the basis of the subject‚Äôs prior treatment history and baseline genotypic and phenotypic viral resistance measurements. In addition to the optimized background regimen, subjects were then randomized in a 2:2:1 ratio to maraviroc 300¬†mg once daily, maraviroc 300¬†mg twice daily, or placebo. Doses were adjusted based on background therapy as described in Dosing and Administration, Table 1.
In the pooled analysis for A4001027 and A4001028, the demographics and baseline characteristics of the treatment groups were comparable (Table 12). Of the 1,043 subjects with a CCR5 tropism result at screening, 7.6% had a dual/mixed tropism result at the baseline visit 4 to 6 weeks later. This illustrates the background change from CCR5 to dual/mixed tropism result over time in this treatment-experienced population, prior to a change in antiretroviral regimen or administration of a CCR5 co-receptor antagonist.
 
Table 12. Demographic and Baseline Characteristics of Subjects in Studies A4001027 and A4001028
SELZENTRY
Twice Daily
(N = 426)
Placebo
(N = 209)Age (years) Mean (range) 46.3 (21-73) 45.7 (29-72) Sex Male 382 (89.7%) 185 (88.5%) Female 44 (10.3%) 24 (11.5%) Race White 363 (85.2%) 178 (85.2%) Black 51 (12.0%) 26 (12.4%) Other 12 (2.8%) 5 (2.4%) Region U.S. 276 (64.8%) 135 (64.6%) Non-U.S. 150 (35.2%) 74 (35.4%) Subjects with Previous Enfuvirtide Use 142 (33.3%) 62 (29.7) Subjects with Enfuvirtide as Part of OBT 182 (42.7%) 91 (43.5%)
Baseline Plasma HIV-1 RNA (log10 copies/mL)
Mean (range)4.85 (2.96-6.88) 4.86 (3.46-7.07)
Subjects with Screening
Viral Load >100,000 copies/mL179 (42.0%) 84 (40.2%)
Baseline CD4+ Cell Count (cells/mm3)
Median (Range)167 (2-820) 171 (1-675) Subjects with Baseline CD4+ Cell Count ‚ȧ200¬†cells/mm3) 250 (58.7%) 118 (56.5%) Subjects with Overall Susceptibility Score (OSS):a 0 57 (13.4%) 35 (16.7%) 1 136 (31.9%) 44 (21.1%) 2 104 (24.4%) 59 (28.2%) ‚Č•3 125 (29.3%) 66 (31.6%) Subjects with Enfuvirtide Resistance Mutations 90 (21.2%) 45 (21.5%) Median Number of Resistance-Associated:b PI mutations 10 10 NNRTI mutations 1 1 NRTI mutations 6 6
a OSS - Sum of active drugs in OBT based on combined information from genotypic and phenotypic testing.
b Resistance mutations based on IAS guidelines.1
The Week 48 results for the pooled Studies A4001027 and A4001028 are shown in Table 13.
Table 13. Outcomes of Randomized Treatment at Week 48 Studies A4001027 and A4001028 Outcome
SELZENTRY
Twice Daily
(N = 426)
Placebo
(N = 209)Mean Difference Mean change from Baseline to Week 48 in HIV-1 RNA (log10 copies/mL) -1.84 -0.78 -1.05 <400 copies/mL at Week 48 239 (56%) 47 (22%) 34% <50 copies/mL at Week 48 194 (46%) 35 (17%) 29% Discontinuations Insufficient Clinical Response 97 (23%) 113 (54%) Adverse Events 19 (4%) 11 (5%) Other 27 (6%) 18 (9%) Subjects with treatment-emergent CDC Category C events 22 (5%) 16 (8%) Deaths (during study or within 28 days of last dose) 9 (2%)a 1 (0.5%)
a One additional subject died while receiving open-label maraviroc therapy subsequent to discontinuing double-blind placebo due to insufficient response.
After 48¬†weeks of therapy, the proportions of subjects with HIV-1 RNA <400¬†copies/mL receiving maraviroc compared with placebo were 56% and 22%, respectively. The mean changes in plasma HIV-1 RNA from baseline to Week 48 were ‚Äď1.84 log10¬†copies/mL for subjects receiving maraviroc + OBT compared with ‚Äď0.78 log10¬†copies/mL for subjects receiving OBT only. The mean increase in CD4+ counts was higher on maraviroc twice daily + OBT (124¬†cells/mm3) than on placebo + OBT (60¬†cells/mm3 ).
14.2 Study in Dual/Mixed-Tropic, Treatment-Experienced Subjects
Study A4001029 was an exploratory, randomized, double-blind, multicenter trial to determine the safety and efficacy of maraviroc in subjects infected with dual/mixed coreceptor tropic HIV-1. The inclusion/exclusion criteria were similar to those for Studies A4001027 and A4001028 above and the subjects were randomized in a 1:1:1 ratio to SELZENTRY once daily, SELZENTRY twice daily, or placebo. No increased risk of infection or HIV disease progression was observed in the subjects who received SELZENTRY. Use of SELZENTRY was not associated with a significant decrease in HIV-1 RNA compared with placebo in these subjects and no adverse effect on CD4 count was noted.
14.3 Study in Treatment-Naive Subjects
Study A4001026 is an ongoing, randomized, double-blind, multicenter study in subjects infected with CCR5-tropic HIV-1 classified by the original Trofile¬ģ tropism assay. Subjects were required to have plasma HIV-1 RNA ‚Č•2,000¬†copies/mL and could not have: 1) previously received any antiretroviral therapy for >14¬†days, 2) an active or recent opportunistic infection or a suspected primary HIV-1 infection, or 3) phenotypic or genotypic resistance to zidovudine, lamivudine, or efavirenz. Subjects were randomized in a 1:1:1 ratio to maraviroc 300¬†mg once daily, maraviroc 300¬†mg twice daily, or efavirenz 600¬†mg once daily, each in combination with zidovudine/lamivudine. The efficacy and safety of SELZENTRY are based on the comparison of SELZENTRY twice daily versus efavirenz. In a pre-planned interim analysis at 16¬†weeks, the maraviroc 300-mg once-per-day treatment arm failed to meet the pre-specified criteria for demonstrating non-inferiority and was discontinued.
The demographic and baseline characteristics of the maraviroc and efavirenz treatment groups were comparable (Table 14). Subjects were stratified by screening HIV-1 RNA levels and by geographic region. The median CD4 cell counts and mean HIV-1 RNA at baseline were similar for both treatment groups.
Table 14. Demographic and Baseline Characteristics of Subjects in Study A4001026
SELZENTRY 300 mg b.i.d. + zidovudine/lamivudine
(N = 360)
Efavirenz 600 mg q.d. + zidovudine/lamivudine
(N = 361)Age (years) Mean 36.7 37.4 Range 20-69 18-77 Female, n% 104 (29) 102 (28) Race, n%
White
Black
204 (57) 198 (55) Black 123 (34) 133 (37) Asian 6 (2) 5 (1) Other 27 (8) 25 (7) Median (Range) CD4 cell count (cells/¬ĶL) 241 (5-1,422) 254 (8-1,053) Median (Range) HIV-1 RNA (log10 copies/mL 4.9 ( 3-7) 4.9 (3-7)
The treatment outcomes at 96¬†weeks for Study A4001026 are shown in Table 15. Treatment outcomes are based on reanalysis of the screening samples using a more sensitive tropism assay, Enhanced sensitivity TROFILE¬ģ HIV tropism assay, which became available after the Week 48 analysis, approximately 15% of the subjects identified as CCR5-tropic in the original analysis had Dual/Mixed- or CXCR4-tropic virus. Screening with enhanced sensitivity version of the Trofile¬ģ tropism assay reduced the number of maraviroc virologic failures with CXCR4- or Dual/Mixed-tropic virus at failure to 12 compared with 24 when screening with the original TROFILE HIV tropism assay.
 
Table 15: Study Outcome (Snapshot) at Week 96 Using Enhanced Sensitivity Assaya Outcome at Week 96b
SELZENTRY 300 mg b.i.d. + zidovudine/lamivudine
N = 311
n (%)
Efavirenz 600 mg q.d. +
zidovudine/lamivudine
N = 303
n (%)
Virologic Responders:
(HIV-1 RNA <400 copies/mL)199 (64) 195 (64) Virologic Failure:
- Non-sustained HIV-1 RNA suppression
39 (13) 22 (7)
- HIV-1 RNA never suppressed
9 (3) 1 (<1)
Virologic Responders:
(HIV-1 RNA <50 copies/mL)183 (59) 190 (63) Virologic Failure:
- Non-sustained HIV-1 RNA suppression
43 (14) 25 (8)
- HIV-1 RNA never suppressed
21 (7) 3 (1) Discontinuations due to:
- Adverse Events
19 (6) 47 (16)
- Death
2 (1) 2 (1)
- Otherc
43 (14) 36 (12)
aThe total number of subjects (Ns) in Table 15 represents the subjects who had a CCR5-tropic virus in the reanalysis of screening samples using the more sensitive tropism assay. This reanalysis reclassified approximately 15% of subjects shown in Table 14 as having Dual/Mixed- or CXCR4-tropic virus. These numbers are different than those presented in Table 14 because the numbers in Table 14 reflect the subjects with CCR5-tropic virus according to the original tropism assay.
b Week 48 results: Virologic responders (<400): 228/311 (73%) in SELZENTRY, 219/303 (72%) in efavirenz;
Virologic responders (<50): 213/311 (69 %) in SELZENTRY, 207/303 (68%) in efavirenz
c Other reasons for discontinuation include lost to follow-up, withdrawn, protocol violation, and other.
The median increase from baseline in CD4+ cell counts at Week 96 was 184 cells/mm3 for the arm receiving SELZENTRY compared with 155 cells/mm3 for the efavirenz arm.
15 References
- IAS-USA Drug Resistance Mutations Figures. http://www.iasusa.org/pub/topics/2006/issue3/125.pdf
16 How Supplied/storage And Handling
SELZENTRY film-coated tablets are available as follows:
150- and 300-mg tablets are blue, biconvex, oval, film-coated tablets debossed with ‚ÄúPfizer‚ÄĚ on one side and ‚ÄúMVC 150‚ÄĚ or ‚ÄúMVC 300‚ÄĚ on the other.
Bottle packs 150-mg tablets: 60 tablets (NDC 49702-215-18).
Bottle packs 300-mg tablets: 60 tablets (NDC 49702-216-18).
SELZENTRY film-coated tablets should be stored at 25oC (77oF); excursions permitted between 15oC and 30oC (59oF-86oF) [see USP Controlled Room Temperature].
Shelf life is 24 months.
17 Patient Counseling Information
See Medication Guide.
Patients should be informed that if they develop signs or symptoms of hepatitis or allergic reaction following use of SELZENTRY (rash, skin, or eyes look yellow; dark urine; vomiting; abdominal pain), they should stop SELZENTRY and seek medical evaluation immediately [see Warnings and Precautions (5.1)].
Patients should be informed that SELZENTRY is not a cure for HIV infection and patients may still develop illnesses associated with HIV infection, including opportunistic infections. The use of SELZENTRY has not been shown to reduce the risk of transmission of HIV to others through sexual contact, sharing needles, or blood contamination.
Patients should be advised that it is important to:
- remain under the care of a physician when using SELZENTRY;
- take SELZENTRY every day as prescribed and in combination with other antiretroviral drugs;
- report to their physician the use of any other prescription or nonprescription medication or herbal products;
- inform their physician if they are pregnant, plan to become pregnant or become pregnant while taking SELZENTRY;
- not change the dose or dosing schedule of SELZENTRY or any antiretroviral medication without consulting their physician.
Patients should be advised that it is important to take all their anti-HIV medicines as prescribed and at the same time(s) each day.
Patients should be advised that when their SELZENTRY supply starts to run low, they should ask their doctor or pharmacist for a refill.
Patients should be advised that if they forget to take a dose, they should take the next dose of SELZENTRY as soon as possible and then take their next scheduled dose at its regular time. If it is less than 6 hours before their next scheduled dose, they should not take the missed dose and should instead wait and take the next dose at the regular time.
Caution should be used when administering SELZENTRY  in patients with a history of postural hypotension or on concomitant medication known to lower blood pressure. Patients should be advised that if they experience dizziness while taking SELZENTRY, they should avoid driving or operating machinery.
TROFILE¬ģ is a registered trademark of Monogram Biosciences, Inc.
Manufactured for:
ViiV Healthcare
Research Triangle Park, NC 27709
by:
Pfizer Manufacturing Deutschland GmbH
Freiburg, Germany
©2010, ViiV Healthcare. All rights reserved.
November 2010
SEL: 21PI
Spl Medguide Section
MEDICATION GUIDE
SELZENTRY ¬ģ (sell-ZEN-tree) Tablets
(maraviroc)
Read the Medication Guide that comes with SELZENTRY before you start taking it and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or treatment.
What is the most important information I should know about SELZENTRY?
Serious side effects have occurred with SELZENTRY, including liver problems (liver toxicity). An allergic reaction may happen before liver problems occur. Stop taking SELZENTRY and call your healthcare provider right away if you get any of the following symptoms:
- an itchy rash on your body (allergic reaction)
- yellowing of your skin or whites of your eyes (jaundice)
- dark (tea-colored) urine
- vomiting
- upper right stomach area (abdominal) pain
What is SELZENTRY?
SELZENTRY is an anti-HIV medicine called a CCR5 antagonist. HIV (Human Immunodeficiency Virus) is the virus that causes AIDS (Acquired Immune Deficiency Syndrome).
SELZENTRY is used with other anti-HIV medicines in adults with CCR5-tropic HIV-1 infection.
Use of SELZENTRY is not recommended in people with dual/mixed or CXCR4-tropic HIV-1.
- SELZENTRY will not cure HIV infection.
- People taking SELZENTRY may still develop infections, including opportunistic infections or other conditions that happen with HIV infection.
- It is very important that you stay under the care of your healthcare provider during treatment with SELZENTRY.
- The long-term effects of SELZENTRY are not known at this time.
SELZENTRY has not been studied in children less than 16 years of age.
Does SELZENTRY lower the risk of passing HIV to other people?
No, SELZENTRY does not lower the risk of passing HIV to other people through sexual contact, sharing needles, or being exposed to your blood.
- Continue to practice safer sex.
- Use latex or polyurethane condoms or other barrier methods to lower the chance of sexual contact with any body fluids. This includes semen from a man, vaginal secretions from a woman, or blood.
- Never re-use or share needles.
- Ask your healthcare provider if you have any questions about safer sex or how to prevent passing HIV to other people.
How does SELZENTRY work?
HIV enters cells in your blood by attaching itself to structures on the surface of the cell called receptors. SELZENTRY blocks a specific receptor called CCR5 that CCR5-tropic HIV-1 uses to enter CD4 or T-cells in your blood. Your healthcare provider will do a blood test to see if you have been infected with CCR5-tropic HIV-1 before prescribing SELZENTRY for you.
- When used with other anti-HIV medicines, SELZENTRY may:
- reduce the amount of HIV in your blood. This is called ‚Äúviral load‚ÄĚ.
- increase the number of white blood cells called T (CD4) cells.
SELZENTRY does not work in all people with CCR5-tropic HIV-1 infection.
Who should not take SELZENTRY?
People with severe kidney problems or who are on hemodialysis and are taking certain other medications should not take SELZENTRY. Talk to your healthcare provider before taking this medicine if you have kidney problems.
What should I tell my healthcare provider before taking SELZENTRY?
Before you take SELZENTRY, tell your healthcare provider if you:
- have liver problems including a history of hepatitis B or C.
- have heart problems.
- have kidney problems.
- have low blood pressure or take medicines to lower blood pressure.
- have any other medical condition.
- are pregnant or plan to become pregnant. It is not known if SELZENTRY may harm your unborn baby.
Antiretroviral Pregnancy Registry. There is a pregnancy registry for women who take antiviral medicines during pregnancy. The purpose of the registry is to collect information about the health of you and your baby. Talk to your healthcare provider about how you can take part in this registry.
- are breastfeeding or plan to breastfeed. It is recommended that HIV-positive women should not breastfeed their babies. This is because of the chance of passing HIV to your baby. You should not breastfeed if you are taking SELZENTRY because the risk to your baby is unknown. Talk with your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Certain other medicines may affect the levels of SELZENTRY in your blood. Your healthcare provider may need to change your dose of SELZENTRY when you take it with certain medicines.
The levels of SELZENTRY in your blood may change and your healthcare provider may need to adjust your dose of SELZENTRY when taking any of the following medications together with SELZENTRY:
- darunavir (Prezista¬ģ) - delavirdine (Rescriptor¬ģ)
- lopinavir/ritonavir (Kaletra¬ģ, Norvir¬ģ) - ketoconazole (Nizoral¬ģ)
- atazanavir (Reyataz¬ģ) - itraconazole (Sporanox¬ģ)
- saquinavir (Invirase¬ģ) - clarithromycin (Biaxin¬ģ)
- nelfinavir (Viracept¬ģ) - nefazodone (Serzone¬ģ)
- indinavir (Crixivan¬ģ) - telithromycin (Ketek¬ģ)
- fosamprenavir (Lexiva¬ģ) - efavirenz (Sustiva¬ģ, Atripla¬ģ)
- etravirine (Intelence¬ģ) - rifampin (Rifadin¬ģ, Rifater¬ģ)
- carbamezepine (Tegretol¬ģ) - phenobarbital (Luminal¬ģ)
- phenytoin (Dilantin¬ģ)
- Ritonavir (Norvir¬ģ)
Do not take products that contain St. John’s Wort (hypericum perforatum). St. John’s Wort may lower the levels of SELZENTRY in your blood so that it will not work to treat your CCR5-tropic HIV infection.
Know the medicines you take. Keep a ul of your medicines. Show the ul to your healthcare provider and pharmacist when you get a new medicine.
How should I take SELZENTRY?
Take SELZENTRY exactly as prescribed by your healthcare provider. SELZENTRY comes in 150 mg and 300 mg tablets. Your healthcare provider will prescribe the dose that is right for you.
- Take SELZENTRY 2 times a day.
- Swallow SELZENTRY tablets whole. Do not chew the tablets.
- Take SELZENTRY tablets with or without food.
- Always take SELZENTRY with other anti-HIV drugs as prescribed by your healthcare provider.
Do not change your dose or stop taking SELZENTRY or your other anti-HIV medicines without first talking with your healthcare provider.
- If you take too much SELZENTRY, call your healthcare provider or the poison control center right away.
- If you forget to take SELZENTRY, take the next dose of SELZENTRY as soon as possible and then take your next scheduled dose at its regular time. If it is less than 6 hours before your next dose, do not take the missed dose. Wait and take the next dose at the regular time. Do not take a double dose to make up for a missed dose.
- It is very important to take all your anti-HIV medicines as prescribed. This can help your medicines work better. It also lowers the chance that your medicines will stop working to fight HIV (drug resistance).
- When your SELZENTRY supply starts to run low, ask your healthcare provider or pharmacist for a refill. This is very important because the amount of virus in your blood may increase and SELZENTRY could stop working if it is stopped for even a short period of time.
What are the possible side effects of SELZENTRY?
There have been serious side effects when SELZENTRY has been given with other anti-HIV drugs including:
- Liver problems. See ‚ÄúWhat is the most important information I should know about SELZENTRY?‚ÄĚ
- Heart problems including heart attack.
- Low blood pressure when standing up (postural hypotension). Low blood pressure when standing up can cause dizziness or fainting. Do not drive a car or operate heavy machinery if you have dizziness while taking SELZENTRY.
- Changes in your immune system. A condition called Immune Reconstitution Syndrome can happen when you start taking HIV medicines. Your immune system may get stronger and could begin to fight infections that have been hidden in your body such as pneumonia, herpes virus or tuberculosis. Tell your healthcare provider if you develop new symptoms after starting your HIV medicines.
- Possible chance of infection or cancer. SELZENTRY affects other immune system cells and therefore may possibly increase your chance for getting other infections or cancer.
The most common side effects of SELZENTRY include colds, cough, fever, rash, and dizziness.
Tell your healthcare provider about any side effect that bothers you or does not go away.
These are not all of the side effects with SELZENTRY. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store SELZENTRY?
- Store SELZENTRY tablets at room temperature from 59‚ó¶F to 86‚ó¶F (15‚ó¶C to 30‚ó¶C).
- Safely throw away medicine that is out of date or that you no longer need.
Keep SELZENTRY and all medicines out of the reach of children.
General information about SELZENTRY
Medicines are sometimes prescribed for conditions that are not mentioned in Medication Guides. Do not use SELZENTRY for a condition for which it was not prescribed. Do not give SELZENTRY to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes the most important information about SELZENTRY. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for more information about SELZENTRY that is written for health professionals.
For more information, go to www.selzentry.com.
What are the ingredients in SELZENTRY?
Active ingredient: maraviroc
Inactive ingredients: microcrystalline cellulose, dibasic calcium phosphate (anhydrous), sodium starch glycolate, magnesium stearate
Film-coat: FD&C blue #2 aluminum lake, soya lecithin, polyethylene glycol (macrogol 3350), polyvinyl alcohol, talc, and titanium dioxide
The brands uled are the trademarks or registered marks of their respective owners and are not trademarks of ViiV Healthcare. The makers of these brands are not affiliated with and do not endorse ViiV Healthcare or its products.
This Medication Guide has been approved by the US Food and Drug Administration.
Manufactured for:
ViiV Healthcare
Research Triangle Park, NC 27709
by:
Pfizer Manufacturing Deutschland GmbH
Freiburg, Germany
©2010, ViiV Healthcare. All rights reserved.
November 2010
SEL: 2MG
Principal Display Panel
NDC 49702-215-18
Selzentry¬ģ
(maraviroc) tablets
150 mg
60 Tablets
Rx only
ALWAYS DISPENSE WITH MEDICATION GUIDE
Store at 25¬įC (77¬įF); excursions permitted between 15¬įC and 30¬įC (59¬įF - 86¬įF) [see USP Controlled Room Temperature].
Dispense in tight containers (USP).
DOSAGE AND USE
See prescribing information for dosage information.
Each tablet contains 150 mg of maraviroc.
Manufactured for:
ViiV Healthcare
Research Triangle Park, NC 27709
by:
Pfizer Manufacturing Deutschland GmbH
Freiburg, Germany
Made in Ireland
Rev. 11/10
412988
![]()
Principal Display Panel
NDC 49702-216-18
Selzentry¬ģ
(maraviroc) tablets
300 mg
60 Tablets
Rx only
ALWAYS DISPENSE WITH MEDICATION GUIDE
Store at 25¬įC (77¬įF); excursions permitted between 15¬įC and 30¬įC (59¬įF - 86¬įF) [see USP Controlled Room Temperature].
Dispense in tight containers (USP).
DOSAGE AND USE
See prescribing information for dosage information.
Each tablet contains 300 mg of maraviroc.
Manufactured for:
ViiV Healthcare
Research Triangle Park, NC 27709
by:
Pfizer Manufacturing Deutschland GmbH
Freiburg, Germany
Made in Ireland
Rev. 11/10
412999
![]()
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site