AKYNZEO (netupitant 300 mg palonosetron 0.5 mg) Dailymed
Generic: fosnetupitant and palonosetron is used for the treatment of Nausea Vomiting Postoperative Nausea and Vomiting
Go PRO for all pill images
1 Indications And Usage
- AKYNZEO capsules is indicated in combination with dexamethasone in adults for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of cancer chemotherapy, including, but not limited to, highly emetogenic chemotherapy. AKYNZEO capsules is a combination of palonosetron and netupitant: palonosetron prevents nausea and vomiting during the acute phase and netupitant prevents nausea and vomiting during both the acute and delayed phase after cancer chemotherapy.
- AKYNZEO for injection and AKYNZEO injection are indicated in combination with dexamethasone in adults for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy. AKYNZEO for injection is a combination of palonosetron and fosnetupitant, a prodrug of netupitant: palonosetron prevents nausea and vomiting during the acute phase and fosnetupitant prevents nausea and vomiting during both the acute and delayed phase after cancer chemotherapy. Limitations of Use AKYNZEO for injection and AKYNZEO injection have not been studied for the prevention of nausea and vomiting associated with anthracycline plus cyclophosphamide chemotherapy.
- AKYNZEO capsules is indicated in combination with dexamethasone in adults for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of cancer chemotherapy, including, but not limited to, highly emetogenic chemotherapy.
- AKYNZEO for injection and AKYNZEO injection are indicated in combination with dexamethasone in adults for the prevention of acute anddelayed nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy. Limitations of Use
- AKYNZEO for injection and AKYNZEO injection have not been studied for the prevention of nausea and vomiting associated with anthracycline plus cyclophosphamide chemotherapy.
- AKYNZEO is a combination of palonosetron, a serotonin-3 (5-HT3) receptor antagonist, and netupitant or fosnetupitant, substance P/neurokinin-1 (NK-1) receptor antagonists: palonosetron prevents nausea and vomiting during the acute phase and netupitant/fosnetupitant prevents nausea and vomiting during both the acute and delayed phase after cancer chemotherapy. (
1 )
2 Dosage And Administration
Recommended Dosage
- AKYNZEO capsules: The recommended dosage is one AKYNZEO capsule administered 1 hour prior to the start of chemotherapy, with or without food. (
2.1 )
Preparation and Administration
- AKYNZEO injection is supplied either as a Ready-to-Use (with hanger) vial or a To-be-Diluted vial.
(2.2) - AKYNZEO for injection requires dilution prior to administration. (
2.3 )- See full prescribing information for information on preparation, administration, and incompatibilities for each product. (2.2, 2.3,
2.4 )2.1 Recommended Dosage
The recommended dosages of AKYNZEO and dexamethasone in adults for the prevention of nausea and vomiting associated with administration of emetogenic chemotherapy are shown in Table 1.
AKYNZEO capsules can be taken with or without food.
Table 1: Antiemetic Treatment Regimen
Treatment Regimen
Day 1
Days 2 to 4
Highly Emetogenic Chemotherapy, including Cisplatin-Based Chemotherapy
AKYNZEO capsules
1 capsule of AKYNZEO
1 hour before chemotherapy
Dexamethasone 8 mg once a day
Dexamethasone 12 mg
30 minutes before chemotherapy
AKYNZEO for injection and AKYNZEO injection
1 vial of AKYNZEO
Infuse over 30 minutes starting 30 minutes before chemotherapy [see Dosage and Administration (2.2)]
Dexamethasone 8 mg once a day
Dexamethasone 12 mg
30 minutes before chemotherapy
Anthracyclines and Cyclophosphamide-Based Chemotherapy and Chemotherapy Not Considered Highly Emetogenic
AKYNZEO capsules
1 capsule of AKYNZEO
1 hour before chemotherapy
None
Dexamethasone 12 mg
30 minutes before chemotherapy
2.2 Preparation and Administration of AKYNZEO Injection (Ready-to-Use and To-be-Diluted)
AKYNZEO injection is supplied as either a Ready-to-Use (with hanger) vial or a To-be-Diluted vial.
AKYNZEO injection (Ready-to-Use; with hanger) See Table 2 for preparation instructions of AKYNZEO injection (Ready-to-Use) for intravenous infusion. AKYNZEO injection (Ready-to-Use) does not require dilution prior to administration.
Table 2: Preparation and Administration of AKYNZEO Injection (Ready-to-Use) for Intravenous Infusion Step 1  Before administration, inspect the solution for particulate matter and discoloration. Discard the vial if particulates and/or discoloration are observed.  Step 2  Using aseptic technique, insert a vented intravenous set through the septum of the vial. Once the stopper is punctured, use immediately.  Step 3  To administer, invert and hang the vial utilizing the strap affixed to the bottom of the vial.  Step 4  Administer over 30 minutes as an intravenous infusion. At the end of the infusion, flush the infusion line with 0.9% Sodium Chloride Injection, USP or with 5% Dextrose injection, USP to ensure complete drug administration.
AKYNZEO injection (Ready-to-Use) contains no antimicrobial preservatives and is intended for single use only.
Compatibility AKYNZEO injection (Ready-to-Use) is compatible with intravenous dexamethasone sodium phosphate which can be infused simultaneously. Do not add dexamethasone sodium phosphate to the AKYNZEO injection (Ready-to-Use) vial.
Stability and Storage Use immediately once the stopper is punctured.
AKYNZEO Injection (To-be-Diluted) See Table 3 for preparation instructions of AKYNZEO injection (To-be-Diluted) for intravenous infusion with dilution.
Table 3: Preparation and Administration of AKYNZEO Injection (To-be-Diluted) for Intravenous Infusion Step 1  Before administration, inspect the solution for particulate matter and discoloration. Discard the vial if particulates and/or discoloration are observed.  Step 2  Aseptically prepare an infusion vial or bag filled with 30 mL of 5% Dextrose injection, USP or 0.9% Sodium Chloride injection, USP.  Step 3  Aseptically withdraw the entire volume of solution from the AKYNZEO vial (20 mL) and transfer it into the infusion vial or bag containing 30 mL of 5% Dextrose injection, USP or 0.9% Sodium Chloride injection, USP to yield a total volume of 50 mL.  Step 4  Gently invert the vial or bag until complete dissolution.  Step 5  Before administration, inspect the final diluted solution for particulate matter and discoloration. Discard the vial or bag if particulates and/or discoloration are observed.  Step 6  Administer over 30 minutes as an intravenous infusion. At the end of the infusion, flush the infusion line with the same carrier solution to ensure complete drug administration. AKYNZEO injection (To-be-Diluted) contains no antimicrobial preservatives and is intended for single use only.
Compatibility
AKYNZEO injection (To-be-Diluted) is compatible with intravenous dexamethasone sodium phosphate which can be added to the infusion bag containing AKYNZEO solution or infused simultaneously.
Stability and Storage
The total time from dilution to the start of the infusion, with or without intravenous dexamethasone sodium phosphate, should not exceed 24 hours.
Store the final diluted solution at room temperature, 20ÂşC to 25ÂşC (68FÂş to 77ÂşF).
2.3 Preparation and Administration of AKYNZEO for Injection
See Table 4 for preparation instructions of AKYZNEO for injection. AKYNZEO for injection requires dilution prior to administration.
 Table 4: Preparation and Administration of AKYNZEO for Injection Step 1  Aseptically inject 20 mL 5% Dextrose injection, USP or 0.9% Sodium Chloride injection, USP into the vial. Ensure the solvent is added to the vial along the vial wall and not jetted in order to prevent foaming. Swirl the vial gently.  Step 2  Aseptically prepare an infusion vial or bag filled with 30 mL of 5% Dextrose injection, USP or 0.9% Sodium Chloride injection, USP.  Step 3  Aseptically withdraw the entire volume of solution from the AKYNZEO vial and transfer it into the infusion vial or bag containing 30 mL of 5% Dextrose injection, USP or 0.9% Sodium Chloride injection, USP to yield a total volume of 50 mL.  Step 4  Gently invert the vial or bag until complete dissolution.  Step 5  Before administration, inspect the final diluted solution for particulate matter and discoloration. Discard the vial or bag if particulates and/or discoloration are observed.  Step 6  Administer over 30 minutes as an intravenous infusion. At the end of the infusion, flush the infusion line with the same carrier solution to ensure complete drug administration.
AKYNZEO for injection contains no antimicrobial preservatives, is intended for single use only.
Compatibility
AKYNZEO for injection is compatible with intravenous dexamethasone sodium phosphate which can be added to the infusion bag containing AKYNZEO solution or infused simultaneously.
Stability and Storage
The total time from reconstitution to the start of the infusion, with or without intravenous dexamethasone sodium phosphate, should not exceed 24 hours.
Store the reconstituted solution and the final diluted solution at room temperature, 20ÂşC to 25ÂşC (68ÂşF to 77ÂşF).
2.4 Incompatibility of AKYNZEO for Injection and AKYZNEO Injection
AKYNZEO for injection, AKYNZEO injection (Ready-to-Use) and AKYNZEO injection (To-be-Diluted) are incompatible with any solution containing divalent cations (e.g., calcium, magnesium), including Lactated Ringer’s injection and Hartmann's Solution.
Limited data are available on the compatibility of AKYNZEO for injection, AKYNZEO injection (Ready-to-Use), and AKYNZEO injection (To-be-Diluted) with other intravenous substances, additives, or other medications with the exception of intravenous dexamethasone sodium phosphate [see Dosage and Administration ( 2.2 , 2.3 ) ] and they should not be added to the AKYNZEO solution or infused simultaneously. If the same intravenous line is used for sequential infusion of several different drugs, flush the line before and after infusion of AKYNZEO solution with 0.9% Sodium Chloride Injection, USP.
3 Dosage Forms And Strengths
- Capsules: 300 mg netupitant/0.5 mg palonosetron in a hard gelatin capsule with white body and caramel cap with “HE1” printed on the body.
- For Injection: 235 mg fosnetupitant/0.25 mg palonosetron white to off-white lyophilized powder in single-dose vial for reconstitution.
- Injection: 235 mg fosnetupitant/0.25 mg palonosetron per 20 mL (11.75 mg/0.0125 mg per mL) as a clear solution in single-dose vial.
- Ready-to-Use (with hanger)
- To-be-Diluted
- Capsules: 300 mg netupitant/0.5 mg palonosetron. (3)
- For Injection: 235 mg fosnetupitant/0.25 mg palonosetron as a lyophilized powder in single-dose vial for reconstitution. (3)
- Injection: 235 mg fosnetupitant/0.25 mg palonosetron (235 mg/0.25 mg per 20 mL (11.75 mg/0.0125 mg per mL) solution in single-dose vial. (3)
- Ready-to-Use (with hanger)
- To-be-Diluted
4 Contraindications
None.
None (4 )
5 Warnings And Precautions
- Hypersensitivity reactions, including anaphylaxis, have been reported in patients receiving palonosetron, one of the components of AKYNZEO, with or without known hypersensitivity to other 5-HT3 receptor antagonists. (
5.1 )- Serotonin syndrome has been reported with 5-HT3 receptor antagonists alone but particularly with concomitant use of serotonergic drugs. If such symptoms occur, discontinue AKYNZEO and initiate supportive treatment. If concomitant use of AKYNZEO with other serotonergic drugs is clinically warranted, patients should be made aware of a potential increased risk for serotonin syndrome. (
5.2, 7.3 )5.1 Hypersensitivity
Hypersensitivity reactions, including anaphylaxis, have been reported in patients treated with palonosetron, one of the components of AKYNZEO, with or without known hypersensitivity to other 5-HT3 receptor antagonists.
5.2 Serotonin Syndrome
The development of serotonin syndrome has been reported with 5-HT3 receptor antagonists. Most reports have been associated with concomitant use of serotonergic drugs (e.g., selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors, mirtazapine, fentanyl, lithium, tramadol, and intravenous methylene blue). Some of the reported cases were fatal. Serotonin syndrome occurring with overdose of another 5-HT3 receptor antagonist alone has also been reported. The majority of reports of serotonin syndrome related to 5-HT3 receptor antagonist use occurred in a post-anesthesia care unit or an infusion center.Â
Symptoms associated with serotonin syndrome may include the following combination of signs and symptoms: mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, and hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, and incoordination), seizures, with or without gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome, especially with concomitant use of AKYNZEO and other serotonergic drugs. If symptoms of serotonin syndrome occur, discontinue AKYNZEO and initiate supportive treatment. Patients should be informed of the increased risk of serotonin syndrome, especially if AKYNZEO is used concomitantly with other serotonergic drugs [see Drug Interactions ( 7.3)].
6 Adverse Reactions
The following clinically significant adverse reactions are found elsewhere in the labeling:
Most common adverse reactions (≥3%) for AKYNZEO capsules are headache, asthenia, dyspepsia, fatigue, constipation and erythema (6.1 )
The safety profile of AKYNZEO for injection was generally similar to that seen with AKYNZEO capsules. (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact HELSINN at 1-844-357-4668 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
AKYNZEO Capsules
The overall safety of AKYNZEO capsules was evaluated in 1538 cancer patients and healthy subjects in clinical trials. The data described below reflect exposure to AKYNZEO in 1169 cancer patients, receiving at least one cycle of cancer chemotherapy in 3 active-controlled trials [see Clinical Studies ( 14 .1)], including 782 exposed to AKYNZEO for at least 4 cycles and 321 exposed for at least 6 cycles, up to a maximum of 12 cycles of chemotherapy. The median age was 55, 79% were female, 83% were White, 13% were Asian, and 4% were Hispanic. All patients received a single oral dose of AKYNZEO 1 hour prior to the start of each chemotherapy cycle. In all studies, dexamethasone was co-administered with AKYNZEO [see Clinical Studies ( 14.1), Table 16 and Table 18 ].
Cisplatin Based Highly Emetogenic Chemotherapy
In a single-cycle study of patients receiving cisplatin based highly emetogenic chemotherapy, 136 patients were treated with AKYNZEO. Table 5 shows adverse reactions reported at an incidence of at least 3% and for which the AKYNZEO rate exceeded palonosetron alone.
Table 5: Adverse Reactions Occurring in ≥3% of Cancer Patients Receiving AKYNZEO capsules and Cisplatin Based Highly Emetogenic Chemotherapy (Cycle 1) Adverse Reactions AKYNZEOnetupitant 300 mg/ palonosetron 0.5 mg (N=136) Palonosetron 0.5 mg (N=136) Dyspepsia 4% 2% Fatigue 4% 2% Constipation 3% 1% Erythema 3%  2%
Anthracyclines and Cyclophosphamide Based Chemotherapy
In a study of patients receiving anthracycline and cyclophosphamide based chemotherapy, 725 patients were treated with AKYNZEO capsules during Cycle 1, and 635 of these patients continued for up to 8 cycles in a multiple-cycle extension. Table 6 shows adverse reactions reported at an incidence of at least 3% and for which the AKYNZEO capsules rate exceeded palonosetron alone during Cycle 1. The adverse reaction profile in subsequent cycles was similar to that observed in Cycle 1.
Table 6: Adverse Reactions Occurring in ≥3% of Cancer Patients Receiving AKYNZEO capsules and Anthracyclines and Cyclophosphamide Based Chemotherapy (Cycle 1)
Adverse Reactions
AKYNZEOnetupitant 300 mg/ palonosetron 0.5 mg(N=725)
Palonosetron 0.5 mg(N=725)
Headache
9%
7%
Asthenia
8%
7%
Fatigue
7%
5%
In addition to the adverse reactions shown above, there were reports of concomitant elevations of transaminases greater than 3 times the upper limit of normal and total bilirubin in both arms of the two trials that compared AKYNZEO capsules to oral palonosetron, and the frequency of these elevations was comparable between treatment groups. See Table 7.
Table 7: Liver Function Laboratory Abnormalities ULN = upper limit of normal
Laboratory Changes
AKYNZEOnetupitant 300 mg/ palonosetron 0.5 mgN=861
Palonosetron 0.5 mgN=861
AST > 3 x ULN and/or ALT > 3 x ULN with Total Bilirubin > ULN
3 (0.3%)
5 (0.6%)
AST > 10 x ULN and/or ALT > 10 x ULN with Total Bilirubin > ULN
-
2 (0.2%)
AST > 3 x ULN and/or ALT > 3 x ULN with Total Bilirubin ≥ 2 x ULN
1 (0.1%)
1 (0.1%)
In a multi-cycle safety study of 412 patients, the safety profile of AKYNZEO capsules (n = 308) was comparable to aprepitant and palonosetron (n = 104) in patients undergoing initial and repeat cycles (median 5 cycles, range of 1-14 cycles) of chemotherapy, including carboplatin, cisplatin, oxaliplatin, and doxorubicin regimens. There were no reports of concomitant elevations of transaminases greater than 3 times the upper limit of normal and total bilirubin in this study in either arm.
In a randomized, clinical non-inferiority study, that compared oral palonosetron 0.5Â mg to intravenous palonosetron 0.25Â mg in cancer patients scheduled to receive highly emetogenic cisplatin (greater than or equal to 70 mg/m2) based chemotherapy, there were two patients (0.5%; 2/369) in the intravenous palonosetron arm who had concomitant elevations of transaminases and total bilirubin. Neither experienced transaminase elevations greater than 10 times the upper limit of normal.Â
AKYNZEO for Injection
The safety of AKYNZEO for injection was evaluated in 203 patients in an active-controlled multi-cycle (median 4 cycles, range of 1-4 cycles) safety clinical study in patients receiving HEC regimens, not including anthracycline plus cyclophosphamide, (e.g., cisplatin, cyclophosphamide, carmustine, dacarbazine and mechlorethamine) compared to 201 patients receiving AKYNZEO capsules (NCT02517021). The median age was 60 years, 46% were female, 99.5 % were White, 0.3% were Asian, and 0.3% were Hispanic. All patients received a single dose of AKYNZEO for injection 30 minutes prior to the start of each chemotherapy cycle; dexamethasone was co-administered with AKYNZEO. The safety profile of AKYNZEO for injection was generally similar to that seen with AKYNZEO capsules.
7 Drug Interactions
- CYP3A4 Substrates: inhibition of CYP3A4 by netupitant can result in increased plasma concentrations of the concomitant drug for 6 days after single dosage administration of AKYNZEO; avoid concomitant CYP3A4 substrates for one week, if feasible. If not avoidable, consider dose reduction of the CYP3A4 substrate (
7.1 )- CYP3A4 Inducers (e.g., rifampin):Â decreased plasma concentrations of netupitant; avoid use (
7.2 )7.1 Effects of AKYNZEO on Other Drugs
Interaction with CYP3A4 Substrates
Netupitant is a moderate inhibitor of CYP3A4.Â
AKYNZEO should be used with caution in patients receiving concomitant medications that are primarily metabolized through CYP3A4. A single oral dose of netupitant 300 mg significantly inhibits CYP3A4 for 6 days. Avoid concomitant use of drugs that are CYP3A4 substrates for one week, if feasible. If not avoidable, consider dose reduction of CYP3A4 substrates.
Dexamethasone
A single oral dose of netupitant 300 mg or a single fosnetupitant infusion of 235 mg increased the systemic exposure of concomitant dexamethasone more than 2-fold on Days 2 and 4. Administer a reduced dose of dexamethasone with AKYNZEO [see Dosage and Administration ( 2.1), Clinical Pharmacology ( 12.3 )].
Midazolam
When administered with netupitant, the systemic exposure to midazolam was significantly increased. Consider the potential effects of increased plasma concentrations of midazolam or other benzodiazepines metabolized via CYP3A4 (alprazolam, triazolam) when administering these drugs with AKYNZEO [see Clinical Pharmacology ( 12.3 )].
Chemotherapeutic Agents
The systemic exposure of chemotherapy agents metabolized by CYP3A4 can increase when administered with AKYNZEO. Chemotherapy agents that are known to be metabolized by CYP3A4 include docetaxel, paclitaxel, etoposide, irinotecan, cyclophosphamide, ifosfamide, imatinib, vinorelbine, vinblastine, and vincristine [see Clinical Pharmacology ( 12.3 )]. Caution and monitoring for chemotherapeutic related adverse reactions are advised in patients receiving chemotherapy agents metabolized primarily by CYP3A4.
Oral Contraceptives
There is no clinically significant effect of AKYNZEO on the efficacy of oral contraceptives containing levonorgestrel and ethinyl estradiol [see Clinical Pharmacology ( 12.3 )].
Warfarin
Although it was predicted that co-administration of intravenous AKYNZEO with warfarin would not substantially increase the systemic exposure to S-warfarin (CYP2C9 substrate), the active enantiomer, the effects of AKYNZEO for injection and AKYNZEO capsules on INR and prothrombin time have not been studied. Monitor INR and adjust the dosage of warfarin, as needed with concomitant use of AKYNZEO, to maintain the target INR range.
7.2 Effectsof Other Drugs on AKYNZEO
Netupitant is mainly metabolized by CYP3A4.
Palonosetron is mainly metabolized by CYP2D6 and to a lesser extent by CYP3A4 and CYP1A2.Â
CYP3A4 Inducers
Avoid concomitant use of AKYNZEO in patients who are chronically using a strong CYP3A4 inducer such as rifampin. A strong CYP3A inducer can decrease the efficacy of AKYNZEO by substantially reducing plasma concentrations of the netupitant component [see Clinical Pharmacology ( 12.3 )].
CYP3A4 Inhibitors
Concomitant use of AKYNZEO with a strong CYP3A4 inhibitor (e.g., ketoconazole) can increase the systemic exposure to the netupitant component of AKYNZEO. However, no dosage adjustment is necessary for single dose administration of AKYNZEO [see Clinical Pharmacology ( 12.3 )].
7.3 SerotonergicDrugs
Serotonin syndrome (including altered mental status, autonomic instability, and neuromuscular symptoms) has been described following the concomitant use of 5-HT3 receptor antagonists and other serotonergic drugs, including selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs). If symptoms occur, discontinue AKYNZEO and initiate supportive treatment [see Warnings and Precautions (5.2)].
8 Use In Specific Populations
- Pregnancy: May cause fetal harm (
8.1 ).- Hepatic Impairment: Avoid use in patients with severe hepatic impairment (
8.6 )- Renal Impairment: Avoid use in patients with severe renal impairment or end-stage renal disease (
8.7 )8.1 Pregnancy
Risk Summary
Limited available data with AKYNZEO use in pregnant women are insufficient to inform a drug- associated risk of adverse developmental outcomes. In animal reproduction studies with netupitant, no effects on embryo-fetal development were observed following daily oral administration in pregnant rats during the period of organogenesis at doses up to 3.7 times the human AUC (area under the plasma concentration-time curve) at the recommended single dose to be given with each cycle of chemotherapy. However, a dose-dependent increase in adverse effects on embryo-fetal development was observed following daily oral administration of netupitant in pregnant rabbits during the period of organogenesis with doses at least 0.2 times the human AUC at the recommended single dose to be given with each cycle of chemotherapy. Daily oral administration of netupitant in rats up to 3.7 times the human AUC at the recommended dose during organogenesis through lactation produced no adverse effects in the offspring (see Data).
In animal reproduction studies with fosnetupitant, delayed ossification of pubis occurred after intravenous administration in rats during the period of organogenesis at a dose 3 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy. In pregnant rabbits, an increase in resorptions was observed with daily intravenous administration of fosnetupitant during the period of organogenesis at doses up to 9 times the human AUC for fosnetupitant and 0.4 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy. Daily intravenousÂadministration of fosnetupitant (3 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy) in rats during organogenesis through lactation produced lower bodyweight in offspring at birth through maturation, and delayed physical development (see Data).
In animal reproduction studies with palonosetron, no effects on embryo-fetal development were observed following oral administration during the period of organogenesis at doses up to 921 and 1841 times the recommended oral dose in rats and rabbits, respectively (see Data).Based on animal data from netupitant studies, advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated populations are unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Netupitant
Daily oral administration of up to 30 mg/kg netupitant in rats (3.7 times the human AUC at the recommended single dose to be given with each cycle of chemotherapy) during the period of organogenesis produced no effects on embryo-fetal development. However, an increased incidence of external and skeletal abnormalities in rabbit fetuses was observed following daily oral administration of netupitant in rabbits at 10Â mg/kg/day and higher (0.2 times the human AUC at the recommended single dose to be given with each cycle of chemotherapy) during the period of organogenesis. These abnormalities included positional abnormalities in the limbs and paws, and fused sternebrae. Reduction in fetal rabbit weight occurred at 30 mg/kg/day. Maternal toxicity in rabbits (i.e., loss of bodyweight during the treatment period) was also observed at 30 mg/kg/day. Daily oral administration of up to 30 mg/kg netupitant (3.7 times the human AUC at the recommended dose) in rats during organogenesis through lactation produced no adverse effects in the offspring.
Fosnetupitant
Daily intravenous administration of 39 mg/kg/day fosnetupitant in rats (3 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy) during the period of organogenesis produced delayed ossification of pubis. No effects on embryo-fetal development were observed with daily administration of up to 13 mg/kg fosnetupitant in rats (2 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy). Due to the limited systemic exposure to fosnetupitant in pregnant rats, it is not possible to provide an AUC-based comparison of fosnetupitant exposure in rats and humans. An increase in resorptions was observed with daily intravenous administration of fosnetupitant at 6 mg/kg/day and higher in rabbits (9 times the human AUC for fosnetupitant and 0.4 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy) during the period of organogenesis. No effects were observed in rabbits at 3 mg/kg/day (5.4 times the human AUC for fosnetupitant and 0.4 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy). Daily intravenous administration of 39 mg/kg fosnetupitant in rats (3 times the AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy) during organogenesis through lactation produced lower bodyweight in offspring at birth through maturation, and delayed physical development (pinna detachment, eye opening, and preputial separation). These effects were associated with maternal toxicity (reduced weight gain and food consumption). No effects occurred in offspring or dams at 13 mg/kg/day (2 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy).
Palonosetron
In animal reproduction studies with palonosetron, no effects on embryo-fetal development were observed in pregnant rats given oral doses up to 60 mg/kg/day (921 times the recommended oral dose based on body surface area) or pregnant rabbits given oral doses up to 60 mg/kg/day (1841 times the recommended oral dose based on body surface area) during the period of organogenesis.
8.2 Lactation
Risk Summary
There are no data on the presence of netupitant (or fosnetupitant) or palonosetron in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for AKYNZEO and any potential adverse effect on the breastfed child from AKYNZEO or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of AKYNZEO in patients below the age of 18 years have not been established.
8.5 Geriatric Use
Of the 1169 adult cancer patients treated with AKYNZEO capsules in clinical studies, 18% were aged 65 and over, while 2% were aged 75 years and over. The nature and frequency of adverse reactions were similar in elderly and younger patients. Exploratory analyses of the impact of age on efficacy were performed in the two trials that compared AKYNZEO to palonosetron [see Clinical Studies ( 14 )]. In Study 1 in patients treated with cisplatin chemotherapy, among the patients less than age 65 years, 115 were treated with AKYNZEO and 116 were treated with palonosetron alone. Among the patients 65 years or older, 20 were treated with AKYNZEO and 20 were treated with palonosetron alone. The difference in Complete Response (CR) rates between AKYNZEO and palonosetron alone was similar between the two age groups in both the acute and delayed phases. In Study 2 in patients treated with anthracyclines plus cyclophosphamide chemotherapy, among the patients less than age 65 years, 608 were treated with AKYNZEO and 602 were treated with palonosetron alone. Among the patients 65 years or older, 116 were treated with AKYNZEO and 123 were treated with palonosetron alone. The difference in CR rates between AKYNZEO and palonosetron alone (4% in <65 years and 2% in >65 years) was similar between the two age groups in the acute phase. In the delayed phase, the difference in CR rates between AKYNZEO and palonosetron alone (9% in <65 years and 1% in ≥ 65 years) was numerically higher in patients <65 years. This difference between age groups in the delayed phase of Study 2 may be explained, in part, by higher CR in the delayed phase associated with palonosetron alone in the older age group (81%) relative to the younger patients treated with palonosetron alone (67%).
Of the 239 adult cancer patients treated with AKYNZEO for injection in clinical studies, 36% were aged 65 and over, while 4% were aged 75 years and over. The nature and frequency of adverse reactions were similar in elderly and younger patients.
In general, use caution when dosing elderly patients as they have a greater frequency of decreased hepatic, renal or cardiac function and concomitant disease or other drug therapy.
8.6 Hepatic Impairment
No dosage adjustment for AKYNZEO is necessary for patients with mild to moderate hepatic impairment (Child-Pugh score 5 to 8). Limited data are available with AKYNZEO in patients with severe hepatic impairment (Child-Pugh score greater than 9). Avoid use of AKYNZEO in patients with severe hepatic impairment [see Overdosage (10), Clinical Pharmacology (12.3) ] .
8.7 Renal Impairment
No dosage adjustment for AKYNZEO is necessary in patients with mild to moderate renal impairment (creatinine clearance of 30 to 60 mL/min). The pharmacokinetics and safety of netupitant have not been studied in patients with severe renal impairment. Severe renal impairment (creatinine clearance < 30 mL/min) did not substantially affect pharmacokinetics of palonosetron. The pharmacokinetics for netupitant and palonosetron were not studied in patients with end-stage renal disease requiring hemodialysis. Avoid use of AKYNZEO in patients with severe renal impairment or end-stage renal disease [see Clinical Pharmacology (12.3) ] .
10 Overdosage
In the event of overdose, AKYNZEO should be discontinued and general supportive treatment and monitoring should be provided. Because of the antiemetic activity of AKYNZEO, drug- induced emesis may not be effective. Dialysis studies have not been performed; due to the large volume of distribution, dialysis is unlikely to be an effective treatment for AKYNZEO overdose.
A total of 33 adult cancer patients were administered oral palonosetron at a dose of 90 mcg/kg (approximately 12 times the recommended dose in AKYNZEO capsules), as part of a dose ranging study and had a similar incidence of adverse reactions compared to lower doses. A single dose of 600 mg (2 times the recommended dose in AKYNZEO capsules) of oral netupitant was administered to 49 healthy subjects and a similar incidence of adverse reactions was observed when compared to lower doses of netupitant in cancer patients and healthy subjects.
11 Description
AKYNZEO (300 mg netupitant/0.5 mg palonosetron) capsules are an oral combination product of netupitant, a substance P/neurokinin 1 (NK-1) receptor antagonist, and palonosetron hydrochloride, a serotonin-3 (5-HT3) receptor antagonist. Both netupitant and palonosetron hydrochloride are anti-nausea and anti-emetic agents.
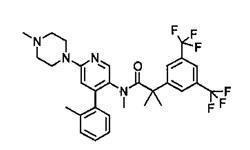
Netupitant is chemically described: 2-[3,5-bis(trifluoromethyl)phenyl]-N, 2 dimethyl-N-[4-(2-methylphenyl)-6-(4-methylpiperazin-1-yl)pyridin-3-yl] propanamide. The empirical formula is C30H32F6N4O, with a molecular weight of 578.61. Netupitant exists as a single isomer and has the following structural formula:
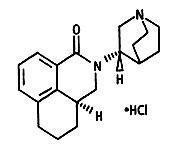
Palonosetron hydrochloride is chemically described: (3aS)-2-[(S)-1-Azabicyclo [2.2.2]oct-3-yl]-2,3,3a,4,5,6-hexahydro-1-oxo-1H-benz[de]isoquinoline hydrochloride. The empirical formula is C19H24N2O.HCl, with a molecular weight of 332.87. Palonosetron hydrochloride exists as a single isomer and has the following structural formula:
Netupitant is white to off-white crystalline powder. It is freely soluble in toluene and acetone, soluble in isopropanol and ethanol, and very slightly soluble in water.
Palonosetron hydrochloride is a white to off-white crystalline powder. It is freely soluble in water, soluble in propylene glycol, and slightly soluble in ethanol and 2-propanol.
Each AKYNZEO capsule is composed of one white-caramel hard gelatin capsule which contains three tablets each containing 100 mg netupitant and one gelatin capsule containing 0.5 mg palonosetron (equivalent to 0.56 mg palonosetron hydrochloride). The inactive ingredients are butylated hydroxyanisole (BHA), croscarmellose sodium, gelatin, glycerin, magnesium stearate, microcrystalline cellulose, mono- and di-glycerides of capryl/capric acid, polyglyceryl dioleate, povidone K-30, purified water, red iron oxide, silicon dioxide, sodium stearyl fumarate, sorbitol, sucrose fatty acid esters, titanium dioxide and yellow iron oxide. It may contain traces of medium-chain triglycerides, lecithin, and denatured ethanol.
AKYNZEO (235 mg fosnetupitant/0.25 mg palonosetron) for injection is a combination product of fosnetupitant, a prodrug of netupitant, which is a substance P/neurokinin 1 (NK-1) receptor antagonist, and palonosetron hydrochloride, a serotonin-3Â (5-HT3) receptor antagonist.
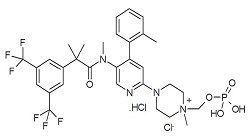
Fosnetupitant chloride hydrochloride is chemically described as 2-(3,5-bis-trifluoromethylphenyl)-N-methyl-N-[6-(4-methyl-4-O-methylene-phosphatepiperazinium-1-yl)-4-o-tolyl-pyridin-3-yl]-isobutyramide chloride hydrochloride. The empirical formula is C31H36F6N4O5P•Cl•HCl, with a molecular weight of 761.53. Fosnetupitant chloride hydrochloride exists as a single isomer and has the following structural formula:
Fosnetupitant chloride hydrochloride is white to off-white to yellowish solid or powder. Its solubility is pH dependent: at acidic pH (pH 2), its solubility is 1.4 mg/mL; at basic pH (pH 10), its solubility is 11.5 mg/mL.
Palonosetron hydrochloride is described above in this section.
AKYNZEO for injection is available for intravenous infusion supplied as a sterile lyophilized powder. Each vial of AKYNZEO for injection contains 235 mg of fosnetupitant (equivalent to 260 mg fosnetupitant chloride hydrochloride) and 0.25 mg of palonosetron (equivalent to 0.28 mg of palonosetron hydrochloride). The inactive ingredients are edetate disodium (6.4 mg), mannitol (760 mg), sodium hydroxide and/or hydrochloric acid (for pH adjustment).
AKYNZEO injection is available for intravenous infusion supplied as a sterile solution in a single-dose vial. Each vial of AKYNZEO injection contains 235 mg of fosnetupitant (equivalent to 260 mg fosnetupitant chloride hydrochloride) and 0.25 mg of palonosetron (equivalent to 0.28 mg of palonosetron hydrochloride). The inactive ingredients are edetate disodium (3.2 mg), mannitol (760 mg), water for injection, sodium hydroxide and/or hydrochloric acid (for pH adjustment).
12 Clinical Pharmacology
12.1 Mechanism of Action
Netupitant is a selective antagonist of human substance P/neurokinin 1 (NK-1) receptors.
Palonosetron is a 5-HT3 receptor antagonist with a strong binding affinity for this receptor and little or no affinity for other receptors. Cancer chemotherapy may be associated with a high incidence of nausea and vomiting, particularly when certain agents, such as cisplatin, are used. 5-HT3 receptors are located on the nerve terminals of the vagus in the periphery and centrally in the chemoreceptor trigger zone of the area postrema. Chemotherapeutic agents produce nausea and vomiting by stimulating the release of serotonin from the enterochromaffin cells of the small intestine. Serotonin then activates 5-HT3 receptors located on vagal afferents to initiate the vomiting reflex. The development of acute emesis is known to depend on serotonin and its 5-HT3 receptors have been demonstrated to selectively stimulate the emetic response.
Delayed emesis has been largely associated with the activation of tachykinin family neurokinin 1 (NK-1) receptors (broadly distributed in the central and peripheral nervous systems) by substance P. As shown in in vitro and in vivo studies, netupitant inhibits substance P mediated responses.
12.2 Pharmacodynamics
NK-1 Receptor Occupancy
The receptor occupancy of netupitant was measured in a human Positron Emission Tomography (PET) study. Netupitant was shown to cross the blood brain barrier with a NK-1 receptor occupancy of 92.5%, 86.5%, 85.0%, 78.0%, and 76.0% in striatum at 6, 24, 48, 72, and 96 hours, respectively, after oral administration of 300Â mg netupitant.
Cardiac Electrophysiology
An AKYNZEO oral dose of 600 mg netupitant (2 times the recommended dose) and 1.5 mg palonosetron (3 times the recommended dose) did not prolong the QT interval to any clinically relevant extent.Â
The recommended dose of AKYNZEO for injection (235 mg fosnetupitant and 0.25 mg palonosetron) did not prolong the QT interval to any clinically relevant extent.Â
12.3 Pharmacokinetics
Netupitant and Palonosetron
Absorption
Upon single oral administration of AKYNZEO capsules to healthy subjects and patients, netupitant and palonosetron were measurable within 1 hour after administration and reached the maximum concentration (Cmax) in approximately 4 to 5 hours (Table 8).Â
Table 8: Systemic Exposure (AUCinf and Cmax) of Netupitant and Palonosetron After a Single Oral Dose of AKYNZEO in Healthy Subjects and Cancer Patients
Parameter
Population
Mean (CV%21 median (min-max); 2CV: coefficient of variation; AUCinf: area under the plasma concentration-time curve from time 0 to infinity; tmax: time to maximum concentration. )
Netupitant
Palonosetron
AUCinf (ngĂ—h/mL)
Healthy Subjects
14,402 (51)
56.7 (33)
Patients
17,365 (39)
58.3 (50)
Cmax (ng/mL)
Healthy Subjects
434 (56)
1.53 (25)
Patients
496 (49)
0.95 (35)
tmax (h)
Healthy Subjects
5 (2 to 12)
5 (1 to 12)
Patients
4 (2 to 8)
5 (1 to 12)
Following oral administration, the absolute bioavailability of palonosetron was approximately 97%.
When AKYNZEO capsules were administered under fed conditions, the systemic exposure to netupitant and palonosetron was similar to the exposure under fasting conditions.
In cancer patients who received a single dose of AKYNZEO capsules 1 hour prior to chemotherapy (docetaxel, etoposide, or cyclophosphamide), the Cmax and the area under the concentration-time curve from time zero to infinity (AUCinf ) of netupitant and its metabolites were similar to those in healthy subjects. The mean Cmax and AUCinf of palonosetron in cancer patients were similar to those in healthy subjects.
No changes in pharmacokinetics of netupitant and palonosetron were observed when 450 mg oral netupitant and 0.75 mg oral palonosetron were given alone or co-administered (1.5 times the recommended dose of AKYNZEO capsules).
Dose Proportionality
Netupitant
There was a greater than dose-proportional increase in the systemic exposure (108-fold AUCinf increase for a 30-fold dose increase) when the oral netupitant dose was increased from 10Â mg (approximately 3% the recommended dose in AKYNZEO capsules) to 300Â mg of netupitant and a dose-proportional increase in the systemic exposure when the netupitant dose was increased from 300 mg to 450 mg of netupitant (1.5 times the recommended dose in AKYNZEO capsules).
Palonosetron
After single oral doses of palonosetron ranging from 0.25 to 6.8 mg (0.5 to 13.6 times the recommended dose in AKYNZEO capsules) using a buffered solution, the mean Cmax and AUCinf were dose proportional in healthy subjects.
Following single intravenous doses of AKYNZEO for injection in patients or fosnetupitant in healthy subjects, Cmax of netupitant and palonosetron were achieved at the end of the 30-minute infusion (Table 9).
Table 9: Systemic Exposure (AUC0-120 and Cmax) of Netupitant and Palonosetron After a Single Intravenous Dose of AKYNZEO for Injection in Cancer Patients or a Single Intravenous Dose of Fosnetupitant in Healthy Subjects
Parameter
Population
Mean (CV%21 median (min-max); 2CV: coefficient of variation; AUCinf: area under the plasma concentration-time curve from time 0 to infinity; tmax: time to maximum concentration. )
Netupitant
Palonosetron
AUC0-120 (ngĂ—h/mL)
Healthy Subjects
12,012 (19)
--
Patients
8,922 (22)
28 (28)
Cmax (ng/mL)
Healthy Subjects
841 (21)
--
Patients
590 (28)
0.8 (35)
tmax (h)
Healthy Subjects
0.5 (0.5 to 0.4)
--
Patients
0.6 (0.5 to 4)
0.6 (0.5 to 6)
Distribution
After single oral administration of AKYNZEO capsules, netupitant and palonosetron were widely distributed throughout the body (Table 10).
Table 10: Volume of Distribution (Vz/F) in Healthy Subjects and Cancer Patients After a Single Oral Dose of AKYNZEO and In Vitro Protein Binding
Parameter
Population
Mean (CV%ca Concentration range: 10 to 1300 ng/mL; b Concentration range: 100 to 200 ng/mL; c CV: coefficient of variation )
Netupitant
Palonosetron
Vz/F (L)
Healthy Subjects
3314 (53)
586 (33)
Patients
1982 (46)
663 (24)
Plasma Protein Binding
In vitro studies
Netupitant: > 99.5% Major Metabolites: > 97%
62%
After administration of single dose of AKYNZEO for injection in patients, the mean ± SD of volume of distribution (Vz) of netupitant and palonosetron were 2627 ± 990 L and 594 ± 239 L, respectively, consistent with previous estimates after single oral administration of AKYNZEO capsules in healthy subjects and cancer patients (Table 10).Â
Elimination – Netupitant
After a single dose of AKYNZEO capsules, netupitant is eliminated from the body in a multi-exponential fashion and the mean ± SD of apparent elimination half-life was of 96 ± 59 hours in healthy subjects and 80 ± 29 hours in cancer patients. The mean ± SD of estimated systemic clearance (CL/F) was 26.3 ± 12.5 L/h in healthy subjects and 20.3 ± 9.2 L/h in patients.
In patients, following intravenous infusion of AKYNZEO for injection, the mean ± SD total body clearance (CL) and terminal half-life (t1/2) of netupitant were 14.1 ± 5.3 L/h and 144 ± 73 hours, respectively.
Metabolism
Once absorbed, netupitant is extensively metabolized to form three major metabolites: desmethyl derivative, M1; N-oxide derivative, M2; and OH-methyl derivative, M3. Metabolism is mediated primarily by CYP3A4 and to a lesser extent by CYP2C9 and CYP2D6. Metabolites M1, M2 and M3 were shown to bind to the substance P/neurokinin 1 (NK-1) receptor.
The mean AUCinf for metabolites M1, M2 and M3 was 29%, 14% and 33% of netupitant, respectively. The median tmax for metabolite M2 was 5 hours and was about 17 to 32 hours for metabolites M1 and M3, respectively.Â
Excretion
After a single oral administration of [14C]Ânetupitant, approximately half the administered radioactivity was recovered from urine and feces within 120 hours of dosing. The total of 3.95% and 70.7% of the radioactive dose was recovered in the urine and feces collected over 336 hours, respectively, and the mean fraction of an oral dose of netupitant excreted unchanged in urine is less than 1% suggesting renal clearance is not a significant elimination route for the netupitant-related entities. About 86.5% and 4.7% of administered radioactivity was estimated to be excreted via the feces and urine within 30 days post-dose.
Elimination - Palonosetron
Following oral administration of AKYNZEO capsules in healthy subjects and cancer patients, the mean ( ± SD) of half-life of palonosetron was 44 ± 15 hours and 50 ± 16 hours, respectively, whereas the mean ± SD of total body clearance (CL/F) was 9.6 ± 2.7 L/h and 10.0 ± 3.4 L/h, respectively.
After a single intravenous palonosetron dose of 10 mcg/kg (approximately 3 times the recommended dose in AKYNZEO for injection), the mean ± SD of total body clearance (CL) of palonosetron in healthy subjects was 12.1 ± 3.7 L/h, and renal clearance (CLR) was 5.1 ± 2.1 L/h.
In patients, following intravenous infusion of AKYNZEO for injection, the mean ± SD total body clearance (CL) and terminal half-life (t1/2) of palonosetron were 7.6 ± 2.6 L/h and 58 ± 27 h, respectively.
Metabolism
Palonosetron is eliminated by multiple routes with approximately 50% metabolized to form two primary metabolites: N-oxide-palonosetron and 6-SÂhydroxy-palonosetron. These metabolites each have less than 1% of the 5-HT3 receptor antagonist activity of palonosetron. In vitro metabolism studies have suggested that CYP2D6 and to a lesser extent CYP3A4 and CYP1A2 are involved in the metabolism of palonosetron. However, clinical pharmacokinetic parameters such as Cmax, AUCinf, CL, CLR, Vz and t1/2 are not significantly different between poor and extensive metabolizers of CYP2D6 substrates.
Excretion
Following administration of a single oral 0.75Â mg dose of [14C]Âpalonosetron (1.5 times the recommended dose in AZKYNZEO capsules) to six healthy subjects, 85% to 93% of the total radioactivity was excreted in urine, and 5% to 8% was eliminated in feces. The amount of unchanged palonosetron excreted in the urine represented approximately 40% of the administered dose.
Fosnetupitant
Absorption
Following single intravenous doses of AKYNZEO for injection in patients (235 mg fosnetupitant and 0.25 mg palonosetron infused in 30 minutes) or fosnetupitant in healthy subjects (235 mg fosnetupitant infused in 30 minutes), maximum concentrations of fosnetupitant were achieved at the end of the 30-minute infusion (Table 11).
Table 11: Systemic Exposure of Fosnetupitant After a Single Intravenous Dose of Fosnetupitant in Healthy Subjects or AKYNZEO for Injection in Cancer Patients
Parameter
Population
Mean (CV%21 median (min-max); 2CV: coefficient of variation; AUCinf: AUC from time 0 to infinity )
Cmax (ng/mL)
Healthy Subjects
6431 (14)
Patients
3478 (45)
tmax (h)
Healthy Subjects
0.5 (0.25 to 0.5)
Patients
0.5 (0.5 to 0.6)
AUCinf (ngĂ—h/mL)
Healthy Subjects
2938 (12)
Patients
1401 (46)
In cross-study comparisons, the mean Cmax and AUCinf of fosnetupitant were lower in patients than in healthy subjects. Similarly, AUC0-120 and Cmax of netupitant in patients were 26% and 30% lower than in healthy subjects, respectively (Table 9). The differences in systemic exposures to netupitant are clinically insignificant.
In healthy subjects, there was a dose-proportional increase in the systemic exposure when the dose of fosnetupitant was increased from 17.6 mg (7.5% of recommended dose in AKYNZEO for injection) to 353 mg (150% of recommended dose in AKYNZEO for injection).
Distribution
The mean ± SD volume of distribution (Vz) of fosnetupitant in healthy subjects and in patients was 124 ± 76 L and 296 ±535 L, respectively. The human plasma protein binding of fosnetupitant was 92% at 1 micromolar and 95% at 10 micromolar.
Elimination
After intravenous administration of AKYNZEO for injection, fosnetupitant plasma concentrations declined in a biexponential manner. Thirty minutes after the end of the infusion, the mean plasma concentration of fosnetupitant was less than 1% of Cmax.Â
The mean ± SD of terminal elimination half-life and systemic plasma clearance (CL) of fosnetupitant were respectively 0.75 ± 0.40 hours and 249 ± 270 L/h in cancer patients after a single IV dose of AKYNZEO. They were 0.96 ± 0.55 hours (mean ± SD) and 90 ± 13 L/h in healthy subjects after a single intravenous dose of fosnetupitant.
Metabolism
Fosnetupitant is converted in vivo to netupitant by metabolic hydrolysis. In patients receiving AKYNZEO intravenously, netupitant exposure was 17-fold fosnetupitant exposure, as determined by their AUCinf ratio. Netupitant metabolites M1, M2 and M3 were generated from the released netupitant. In patients, metabolite M1, M2 and M3 exposures were 32%, 21% and 28% of netupitant exposure. The median tmax for M1, M2, and M3 were 12, 2 and 12 hours, respectively.
Specific Populations
Geriatric Patients
In cancer patients receiving AKYNZEO capsules, population pharmacokinetic analysis indicated that age (within the range of 29 to 75 years) did not influence the pharmacokinetics of netupitant or palonosetron. In healthy elderly subjects (greater than 65 years of age) the mean AUCinf and Cmax was 25% and 36% higher, respectively, for netupitant, and 37% and 10% higher, respectively, for palonosetron compared to those in healthy younger adults (22 to 45 years of age). The increase in the systemic exposure to netupitant in the elderly subjects is not considered to be clinically significant.Â
Male and Female Patients
In a pooled analysis of data following AKYNZEO capsules, the Cmax for netupitant was 35% higher in females than in males while the AUCinf was similar between males and females. In female subjects, the mean AUCinf for palonosetron was 35% higher and the mean Cmax was 26% higher than in male subjects. Sex did not affect the pharmacokinetics of fosnetupitant, netupitant, netupitant metabolites and palonosetron after a single intravenous dose of AKYNZEO in patients. In healthy subjects, no effect of sex was observed on the pharmacokinetics of fosnetupitant, netupitant and its metabolites after a single intravenous dose of fosnetupitant alone. The mean ± SD of netupitant AUCinf and Cmax in patients were 15672 ± 5496 ng×h/mL and 567 ± 174 ng/mL, respectively in males and 15518 ± 4814 ng×h/mL and 609 ± 161 ng/mL, respectively in females.
Patients with Renal Impairment
Population pharmacokinetic analysis showed that mild and moderate renal impairment (creatinine clearance 30 to 60 mL/min) did not significantly affect the pharmacokinetics of netupitant in cancer patients. Netupitant has not been studied in patients with severe renal impairment (creatinine clearance less than 30 mL/min).
Mild to moderate renal impairment does not significantly affect palonosetron pharmacokinetic parameters. In a study with intravenous palonosetron, total systemic exposure to palonosetron increased by approximately 28% in patients with severe renal impairment relative to healthy subjects.
The pharmacokinetics of palonosetron and netupitant have not been studied in subjects with end-stage renal disease (creatinine clearance < 15 mL/min not on dialysis) [see Use in Specific Populations (8.7)].
Patients with Hepatic Impairment
The effects of hepatic impairment on the pharmacokinetics of netupitant and palonosetron were studied following administration of a single oral dose of AKYNZEO to patients with mild (Child-Pugh score 5 to 6), moderate (Child-Pugh score 7 to 9), or severe (Child-Pugh score >9) hepatic impairment.
In patients with mild or moderate hepatic impairment, the mean AUCinf of netupitant was 67% and 86% higher, respectively, than in healthy subjects and the mean Cmax for netupitant was about 40% and 41% higher, respectively, than in healthy subjects.
In patients with mild or moderate hepatic impairment, the mean AUCinf of palonosetron was 33% and 62% higher, respectively, than in healthy subjects and the mean Cmax for palonosetron was about 14% higher and unchanged, respectively, than in healthy subjects.
The pharmacokinetics of netupitant and palonosetron were available from only two patients with severe hepatic impairment. As such the data are too limited to draw a conclusion [see Use in Specific Populations (8.6)].Â
Drug Interaction Studies
Effect of Netupitant/Fosnetupitant and/or Palonosetron on Other Drugs
CYP3A4
In vitro studies have shown that netupitant and its metabolite M1 are inhibitors of CYP3A4. An in vivo study has confirmed that netupitant is a moderate inhibitor of CYP3A4.
Dexamethasone
In healthy subjects, the oral administration of a single AKYNZEO capsule with the CYP3A4 substrate dexamethasone (12 mg on day 1 followed by once-a-day administrations of 8 mg on days 2, 3, 4, 6, 8 and 10), increased the plasma concentrations of dexamethasone for 6 days (Table 12).
Table 12: Effect of a Single Dose of Oral AKYNZEO (Day 1) on the Systemic Exposure of a Co-administered CYP3A4 Substrate (Dexamethasone) in Healthy Subjects *the interacting drug (dexamethasone 12 mg) was administered on day 1 with AKYNZEO and alone (8 mg) on days 2, 3, 4, 6, 8 and 10; AUC0-t: AUC from time zero to time t of last measurable concentration after dexamethasone administration on Days 1, 4, 6 and 8↑ = Increased; ↓ = Decreased
% Change for Dexamethasone
Day 1
Day 4
Day 6
Day 8
Cmax
AUC0-t
Cmax
AUC0-t
Cmax
AUC0-t
Cmax
AUC0-t
2%↓
58%↑
54%↑
139%↑
29%↑
49%↑
7%↑
20%↑
In healthy subjects, co-administration of a single intravenous fosnetupitant dose (235 mg) with a 20 mg oral dexamethasone on day 1 followed by twice-a-day administrations of 8 mg dexamethasone on days 2, 3, and 4, increased dexamethasone exposure 2.4-fold on day 4 (Table 13).
Table 13: Effect of a Single 235 mg Dose of Intravenous Fosnetupitant (Day 1) on the Systemic Exposure of a Co-administered CYP3A4 Substrate (Dexamethasone) in Healthy Subjects *the interacting drug (dexamethasone 20 mg) was administered on day 1 with AKYNZEO and alone (8 mg bid) on Days 2, 3, 4; AUC0-24: AUC from time 0 to 24h after dexamethasone administration on Day 1; AUC84-108: AUC from time 84h to 108h after dexamethasone administration on Day 4 ↑ = Increased; ↓ = Decreased
% Change for Dexamethasone
Day 1
Day 4
Cmax
AUC0-24
Cmax
AUC84-108
3%↓
50%↑
70%↑
142%↑
Considering the limited fosnetupitant exposure in human plasma and its conversion to netupitant within 30 minutes after completion of infusion, the effects are ascribed to netupitant [see Drug Interactions (7.1)].Â
Midazolam
When co-administered with netupitant 300Â mg the mean Cmax and AUCinf of midazolam after single dose oral administration of 7.5Â mg midazolam was 36% and 126% higher, respectively [see Drug Interactions (7.1)].
Chemotherapeutic Agents (docetaxel, etoposide, cyclophosphamide)
Systemic exposure to intravenously administered chemotherapeutic agents that are metabolized by CYP3A4 was higher when AKYNZEO capsules was co-administered in cancer patients than when palonosetron alone was co-administered (see Table 14).
Table 14: Effect of a Single Dose of Oral AKYNZEO on the Systemic Exposure of Co-administered Chemotherapy Agents Metabolized by CYP3A4 in Patients with Cancer
Co-administered Chemotherapeutic Agentaa Following a single oral dose of AKYNZEO compared to co-administered with palonosetron alone bAUC0-t: AUC from time zero to time t of last measurable concentration ↑ = Increased; ↓ = Decreased
Change in Systemic Exposures of Chemotherapeutic Agents when Co-administered with AKYNZEO Capsules Compared to Co-administration with Palonosetron
AUC0-t b
Cmax
Docetaxel 75 to 100 mg/m2
35%↑
49%↑
Etoposide 35 to 100 mg/m2
28%↑
10%↑
Cyclophosphamide 500 to 1000 mg/m2
20%↑
27%↑
The mean AUCinf of palonosetron was about 65% higher when AKYNZEO capsules was co-administered with docetaxel than with etoposide or cyclophosphamide, while the mean AUCinf of netupitant was similar among groups that received docetaxel, etoposide, or cyclophosphamide [see Drug Interactions (7.1)].
Erythromycin
When 500 mg erythromycin was co-administered with netupitant 300Â mg, the systemic exposure of erythromycin was highly variable and the mean Cmax and AUCinf of erythromycin were increased by 92% and 56%, respectively. The change in exposure is not clinically significant.
Oral Contraceptives
A single dose of AKYNZEO capsules, when given with a single oral dose of 60 mcg ethinyl estradiol and 300 mcg levonorgestrel, showed no effect on Cmax and increased the AUC0-t of levonorgestrel by 46%. The Cmax and AUC0-t of ethinyl estradiol increased by 5% and 16% respectively. The change in exposure is not clinically significant [see Drug Interactions (7.1)].
Other CYP P450 enzymes
Based on the in vitro studies, netupitant, and its metabolites are unlikely to have in vivo drug-drug interaction via inhibition of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP2D6 at the clinical dose of oral AKYNZEO.Â
Netupitant and its metabolites, M1, M2 and M3, are not inducers of CYP1A2, CYP2B6, CYP2C9, CYP2C19 and CYP3A4.
In in vitro studies, palonosetron did not inhibit CYP1A2, CYP2A6, CYP2B6, CYP2C9, CYP2D6, CYP2E1 and CYP3A4/5 or induce CYP1A2, CYP2D6 or CYP3A4/5. CYP2C19 was not investigated.
Transporters P-gp and BCRP
Based on in vitro studies, netupitant is an inhibitor of P-glycoprotein (P-gp) and breast cancer resistant protein (BCRP) transporters. In vitro studies indicated that fosnetupitant is an inhibitor of P-gp. However, an in vivo interaction between AKYNZEO for injection and P-gp substrates is considered unlikely.
In vitro, palonosetron was an inhibitor of MATE1, MATE2-K, OCT1, OCT2 and OAT3 transporters. An in vivo interaction between AKYNZEO capsules or injection and transporter substrates is considered unlikely.
Digoxin P-gp Substrate
Co-administration of oral netupitant 450Â mg (1.5 times the recommended dose in AKYNZEO capsules) did not significantly affect the systemic exposure (4% increase of AUC0-24 at steady state) and urinary excretion (2% increase) of oral digoxin, a substrate of P-gp, at steady-state. Concurrent administration of AKYNZEO capsules or AKYNZEO for injection with digoxin is not expected to affect the systemic exposure to digoxin.
Other Transporters
In vitro studies indicate that netupitant and its three major metabolites are unlikely to have in vivo drug-drug interactions with human efflux transporters BSEP, MRP2, and human uptake transporters OATP1B1, OATP1B3, OAT1, OAT3, OCT1, and OCT2 at the clinical dose of 300Â mg.
In vitro studies indicated that fosnetupitant is an inhibitor of OATP1B1 and OATP1B3 transporters. However, an in vivo interaction between AKYNZEO for injection and OATP1B1, OATP1B3, and P-gp substrates is considered unlikely.
In vitro studies indicated that fosnetupitant is not an inhibitor of MATE2-K transporter.
Effects of Other Drugs on Netupitant/Fosnetupitant and/or Palonosetron
Based on in vitro studies, fosnetupitant is not a substrate of BCRP, BSEP, MDR1 and MATE1, MATE2-K, OAT1, OAT3, OATP2B1, OCT1 and OCT2.
Netupitant is not a substrate for P-gp. However, metabolite M2 is a substrate for P-gp.
Netupitant and palonosetron are CYP3A4 substrates. Co-administration of strong CYP3A4 inhibitors, such as ketoconazole, or strong CYP3A4 inducers, such as rifampin, with a single oral administration of AKYNZEO capsules affects with clinical significance the exposure to netupitant but not to palonosetron (Table 15).
Table 15: Change in Systemic Exposure to Netupitant and Palonosetrona When a Single Dose of AKYNZEO is Co‑Administered with Either a CYP3A4 Inhibitor or a CYP3A4 Inducer in Healthy Subjects
Co-administered Drug
Netupitantba Following a single oral dose of AKYNZEO; b Geometric Mean AUCinf and Cmax; ↑ = Increased; ↓ = Decreased
Palonosetronb
AUCinf
Cmax
AUCinf
Cmax
Strong CYP3A4 Inhibitor
Ketoconazole 400Â mg once daily for 12 days
140%↑
25%↑
10%↑
15%↑
Strong CYP3A4 Inducer
Rifampin 600Â mg once daily for 17 days
62%↓
82%↓
19%↓
15%↓
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis,Impairment of Fertility
Netupitant
Long-term studies in animals to evaluate carcinogenic potential have not been performed with netupitant. Netupitant was not genotoxic in the Ames test, the mouse lymphoma cell mutation test, or the in vivo rat micronucleus test.
Daily oral administration of netupitant in rats at doses up to 30 mg/kg (1.9 times the human AUC in male rats and 3.7 times the human AUC in female rats at the recommended dose) had no effects on fertility or reproductive performance.
Fosnetupitant
Long-term studies in animals to evaluate carcinogenic potential have not been performed with fosnetupitant.
Fosnetupitant was not genotoxic in the Ames test and in vivo rat micronucleus test. In human lymphocytes, fosnetupitant did not induce structural chromosomal aberrations.
Daily intravenous administration of fosnetupitant in rats at doses up to 39 mg/kg (1.3 times the human AUC for fosnetupitant and 4.3 times the human AUC for netupitant at the recommended single dose to be given with each cycle of chemotherapy) had no effects on fertility or reproductive performance.
Palonosetron
In a 104-week carcinogenicity study in CD-1 mice, animals were treated with oral doses of palonosetron at 10, 30, and 60 mg/kg/day. Treatment with palonosetron was not tumorigenic. The highest tested dose produced a systemic exposure to palonosetron (plasma AUC) of about 90 to 173 times the human exposure (AUC=49.7 ng•h/mL) at the recommended oral dose of 0.5 mg. In a 104-week carcinogenicity study in Sprague-Dawley rats, male and female rats were treated with oral doses of 15, 30, and 60 mg/kg/day and 15, 45, and 90 mg/kg/day, respectively. The highest doses produced a systemic exposure to palonosetron (plasma AUC) of 82 and 185 times the human exposure at the recommended dose. Treatment with palonosetron produced increased incidences of adrenal benign pheochromocytoma and combined benign and malignant pheochromocytoma, increased incidences of pancreatic Islet cell adenoma and combined adenoma and carcinoma and pituitary adenoma in male rats. In female rats, it produced hepatocellular adenoma and carcinoma and increased the incidences of thyroid C-cell adenoma and combined adenoma and carcinoma.
Palonosetron was not genotoxic in the Ames test, the Chinese hamster ovarian cell (CHO/HGPRT) forward mutation test, the ex vivo hepatocyte unscheduled DNA synthesis (UDS) test, or the mouse micronucleus test. It was, however, positive for clastogenic effects in the Chinese hamster ovarian (CHO) cell chromosomal aberration test. Palonosetron at oral doses up to 60Â mg/kg/day (about 921 times the recommended oral dose based on body surface area) was found to have no effect on fertility and reproductive performance of male and female rats.
14 Clinical Studies
Study 1
In a multicenter, randomized, parallel, double-blind, controlled clinical trial of 694 patients, the efficacy and safety of a single dose of oral netupitant in combination with oral palonosetron was compared with a single oral dose of palonosetron in cancer patients receiving a chemotherapy regimen that included cisplatin (median dose of 75Â mg/m2). The efficacy of AKYNZEO was assessed in 135 patients who received AKYNZEO capsules (300Â mg netupitant and 0.5Â mg palonosetron) and 136 patients who received oral palonosetron 0.5Â mg.
Treatment regimens for the AKYNZEO and palonosetron arms are summarized in Table 16.
Table 16: Oral Antiemetic Treatment Regimen in Study 1
Treatment Regimen
Day 1
Days 2 to 4
AKYNZEO
AKYNZEO capsules:Â 300 mg neupitant/
0.5 mg palonosetron
Dexamethasone 12 mg
Dexamethasone 8 mg once a day
Palonosetron
Palonosetron 0.5 mg
Dexamethasone 20 mg
Dexamethasone 8 mg twice a day
Of the 135 patients who received AKYNZEO, 43% were women, and all patients were White. The age ranged from 19 to 77 years, with a median age of 53 years.
During the study, 86% of the 135 treated patients in the AKYNZEO arm received a concomitant chemotherapeutic agent in addition to protocol-mandated cisplatin. The most common chemotherapeutic agents and the proportion of patients exposed were cyclophosphamide (34%), fluorouracil (24%), etoposide (21%), and doxorubicin (16%).
The key efficacy endpoints were complete response (CR) (defined as no emetic episode and no use of rescue medication) for the 25 to 120 hour interval (delayed phase), CR for the 0 to 24 hour interval (acute phase), and CR within 120 hours (overall phase) after the start of the chemotherapy administration.
A summary of the key results from this study is shown in Table 17.
Table 17: Proportion of Patients Responding by Treatment Group and Phase in Study 1
AKYNZEO Capsules300 mg netupitant/0.5 mg palonosetron (N=135)
Palonosetron0.5 mg (N=136)
p-valueAdjusted p-values for multiple comparisons using Cochran Mantel Haenszel test, stratified by gender.
COMPLETE RESPONSE
Delayed PhaseDelayed phase: 25 to 120 hours post-cisplatin treatment.
90.4
80.1
0.032
Acute PhaseAcute phase: 0 to 24 hours post-cisplatin treatment.
98.5
89.7
0.002
Overall PhaseOverall: 0 to 120 hours post-cisplatin treatment.
89.6
76.5
0.003
Study 2 (NCT01339260)
In a multicenter, randomized, parallel, double-blind, active controlled, superiority trial, the efficacy and safety of a single oral dose of AKYNZEO was compared with a single oral dose of palonosetron 0.5Â mg in cancer patients scheduled to receive the first cycle of an anthracycline and cyclophosphamide (AC) regimen for the treatment of a solid malignant tumor (Study 2). All patients received a single oral dose of dexamethasone. Treatment regimens for the AKYNZEO and palonosetron arms are summarized in Table 18.
Table 18: Oral Antiemetic Treatment Regimen in Study 2
Treatment Regimen
Day 1
Days 2 to 3
AKYNZEO
AKYNZEO capsules: 300 mg netupitant/
0.5 mg palonosetron
Dexamethasone 12 mg
No antiemetic treatment
Palonosetron
Palonosetron 0.5 mg
Dexamethasone 20 mg
No antiemetic treatment
After completion of cycle 1, patients had the option to participate in a multiple-cycle extension, receiving the same treatment as assigned in cycle 1. There was no pre-specified limit of the number of repeat consecutive cycles for any patient.
A total of 1455 patients were randomized to the AKYNZEO arm or palonosetron arm. A total of 1450 patients (AKYNZEO n=725; palonosetron n=725) received study medication: of these, 1438 patients (99%) completed cycle 1 and 1286 patients (88%) continued treatment in the multiple‑cycle extension. A total of 907 patients (62%) completed the multiple‑cycle extension up to a maximum of eight treatment cycles.
Of the 725 patients who received AKYNZEO, 711 (98%) were women; 79% were White, 14% Asian, 6% Hispanic, and <1% were Black or Other. Age ranged from 22 to 79 years, with a median age of 54 years. A total of 724 patients (99.9%) were treated with cyclophosphamide. All patients were additionally treated with either doxorubicin (68%) or epirubicin (32%).
During the first cycle, 32% of the 725 patients treated with AKYNZEO received a concomitant chemotherapeutic agent in addition to protocol-mandated regimens, with the most common chemotherapeutic being fluorouracil (28%) and docetaxel (3%).
The primary efficacy endpoint was the CR rate in the delayed phase, 25 to120 hours after the start of chemotherapy administration.
Major secondary efficacy endpoints included CR for the acute and overall phases. A summary of key results from Study 2 is shown in Table 19.
Table 19: Proportion of Patients Responding by Treatment Group and Phase Cycle 1 in Study 2
AKYNZEO Capsules300 mg netupitant/0.5 mg palonosetronN=724%
Palonosetron0.5 mgN=725%
p-valuep-value from Cochran Mantel Haenszel test, stratified by age class and region.
PRIMARY ENDPOINT
COMPLETE RESPONSE
Delayed PhaseDelayed phase: 25 to 120 hours after anthracycline and cyclophosphamide regimen.
76.9
69.5
0.001
MAJOR SECONDARY ENDPOINTS
COMPLETE RESPONSE
Acute PhaseAcute phase: 0 to 24 hours after anthracycline and cyclophosphamide regimen.
88.4
85.0
0.047
Overall PhaseOverall: 0 to 120 hours after anthracycline and cyclophosphamide regimen.
74.3
66.6
0.001
Multiple Cycles
Patients continued into the Multiple-Cycle extension for up to 7 additional cycles of chemotherapy. The proportion of patients with complete response in the delayed phase by treatment group at each cycle (cycles 2 to 6) is displayed in Figure 1. A limited number of patients received treatment beyond cycle 6. During all cycles the CR rate in the delayed phase was higher for AKYNZEO than for palonosetron. Antiemetic activity of AKYNZEO was maintained throughout repeat cycles for those patients continuing in each of the multiple cycles.
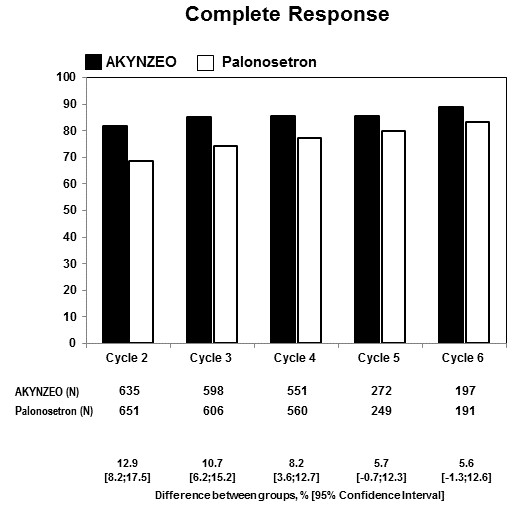
Figure 1: Proportion of Patients with Complete Response in the Delayed Phase by Treatment Group and Cycle in Study 2
Additional clinical trials (Study 3 and Study 4) were conducted to support the efficacy of AKYNZEO.
Study 3 (NCT01376297)
In a separate study, 309 patients undergoing initial and repeat cycles of chemotherapy (including carboplatin, cisplatin, oxaliplatin, and doxorubicin regimens) received AKYNZEO; efficacy was maintained throughout all cycles.
Study 4 (NCT01363479)
In a multicenter, multinational, randomized, active‑controlled, double‑blind, double‑dummy, parallel group, clinical non-inferiority study, the efficacy and safety of a single dose of oral palonosetron 0.5 mg was compared to intravenous palonosetron 0.25 mg in cancer patients scheduled to receive highly emetogenic cisplatin (>70 mg/m2) based chemotherapy. The purpose of this study was to demonstrate that oral palonosetron 0.5 mg contributes to the efficacy of AKYNZEO during the acute phase (first 24 hours after cancer chemotherapy) in the setting of cisplatin based chemotherapy. A total of 739 patients (oral palonosetron n=370; intravenous palonosetron n=369) received study medication.
The primary efficacy endpoint was complete response (CR) (defined as no emetic episode and no use of rescue medication) within 24 hours (acute phase) after the start of cisplatin-based chemotherapy administration. In the oral palonosetron arm, 89.4% of patients achieved a CR in the acute phase compared to 86.2% of patients in the intravenous palonosetron arm, with a difference of 3.2% (99% CI: ‑2.7% to 9.2%). Non‑inferiority of oral palonosetron versus intravenous palonosetron was demonstrated since the lower limit of the two‑sided 99% CI for the difference in proportions of patients with CR was greater (i.e., closer to zero) than the pre‑defined non‑inferiority margin set at ‑15%.
Study 5 (NCT02557035)
In a multicenter, multinational, randomized, active controlled, double blind, double dummy, parallel group, clinical non-inferiority study, the efficacy and safety of a single dose of intravenous palonosetron 0.25 mg administered over 30 minutes (infusion) was compared to intravenous palonosetron 0.25 mg administered over 30 seconds (bolus) in cancer patients scheduled to receive a HEC chemotherapy regimen that included cisplatin administered as a single IV dose of 70 mg/m2, cyclophosphamide 1500 mg/m2, carmustine (BCNU) >250mg/m2, dacarbazine (DTIC) and mechloretamine (nitrogen mustard). The purpose of this study was to demonstrate that intravenous palonosetron 0.25 mg administered over 30 minutes was non-inferior to administration of intravenous palonosetron 0.25 mg administered over 30 seconds for prevention of nausea and vomiting during the acute phase (first 24 hours after cancer chemotherapy) in the HEC setting. A total of 425 patients (intravenous palonosetron infusion n=214; intravenous palonosetron bolus n=211) received study medication and HEC and completed the 0-24 h study period with no major protocol violations and were included in the Per Protocol Population.
The primary efficacy endpoint was complete response (CR defined as no emetic episode and no use of rescue medication) in the 24 hours (acute phase) after the start of the scheduled chemotherapy. In the intravenous palonosetron infusion group, 82.7% of patients achieved CR in the acute phase compared to 86.3% of patients in the intravenous palonosetron bolus group, with a difference of -3.4% (99% CI: - 12.0% to 5.2%). Non-inferiority of administration of intravenous palonosetron over 30 minutes compared to administration of intravenous palonosetron over 30 seconds was demonstrated since the lower limit of the two-sided 99% CI for the difference in proportions of patients with CR was greater (i.e., closer to zero) than the pre-defined non inferiority margin set at -15%.
16 How Supplied/storage And Handling
Capsules
AKYNZEO (300 mg netupitant/0.5 mg palonosetron) capsules: hard gelatin capsules with white body and caramel cap with “HE1” printed on the body. They are supplied as follows:
NDC # 69639-101-01: pack of one capsule in one buler
NDC # 69639-101-04: pack of four capsules (two capsules per buler strip).
Storage
AKYNZEO capsules should be stored at 20 °C to 25 °C (68 °F to 77 °F); excursions permitted from 15 °C to 30 °C (59 °F to 86 °F) [see USP Controlled Room Temperature].
For Injection
AKYNZEO (235 mg fosnetupitant/0.25 mg palonosetron) for injection: sterile, white to off-white lyophilized powder in single-dose vial for reconstitution.
NDC # 69639-102-01: pack of one vial of lyophilized powder
Storage
Store AKYNZEO for injection in carton, protected from light at 2° to 8°C (35.6 F to 46.4°F).
Injection (Ready-to-Use and To-be-Diluted)
AKYNZEO 235 mg fosnetupitant/0.25 mg palonosetron per 20 mL (11.75 mg/0.0125 mg per mL) injection: sterile, clear solution in a single-dose vial.
- NDC # 69639-106-01: pack of one vial of solution with hanger (Ready-to-Use)
- NDC # 69639-105-01: pack of one vial of solution (To-be-Diluted)
Storage
Store AKYNZEO injection in carton, protected from light at 20°C to 25°C (68°F to 77°F).
17 Patient Counseling Information
Advise patients to read the FDA-approved patient labeling (Patient Information).
Administration
Advise patients to take AKYNZEO capsules with or without food approximately 1 hour prior to the start of chemotherapy [see Dosage and Administration (2.1)].
Hypersensitivity ReactionsÂ
Advise patients that hypersensitivity reactions, including anaphylaxis, may occur in patients receiving AKYNZEO. Advise patients to seek immediate medical attention if any signs or symptoms of a hypersensitivity reaction occur while taking AKYNZEOÂ [See Warnings and Precautions (5.1)].
Serotonin Syndrome
Advise patients of the possibility of serotonin syndrome especially with concomitant use of AKYNZEO and another serotonergic agent such as medications to treat depression and migraines. Advise patients to seek immediate medical attention if the following symptoms occur: changes in mental status, autonomic instability, neuromuscular symptoms, with or without gastrointestinal symptoms [see Warnings and Precautions (5.2)].Â
Pregnancy
Inform female patients of reproductive potential that AKYNZEO may cause fetal harm and to inform their prescriber of a known or suspected pregnancy [see Use in Specific Populations (8.1)].
Manufactured by Helsinn Birex Pharmaceuticals, Dublin, Ireland for Helsinn Healthcare SA, Switzerland
Distributed by Helsinn Therapeutics (U.S.), Inc., Iselin, NJ 08830, under license of Helsinn Healthcare SA, Switzerland
AKYNZEO is a registered trademark of Helsinn Healthcare SA, Lugano, Switzerland
Spl Patient Package Insert Section
Patient Information AKYNZEO® (a kin zee oh)(netupitant and palonosetron) capsules, for oral use(fosnetupitant and palonosetron) for injection, for intravenous use
(fosnetupitant and palonosetron) injection, for intravenous use
Read this Patient Information before you start receiving AKYNZEO and each time you are scheduled to receive AKYNZEO. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment.
What is AKYNZEO?
AKYNZEO is a prescription medicine called an antiemetic. AKYNZEO is used in combination with the medicine dexamethasone in people to help prevent the nausea and vomiting that happens right away or later with certain anti-cancer medicines (chemotherapy).
It is not known if AKYNZEO is safe and effective in children under 18 years of age.
Before you take or receive AKYNZEO, tell your doctor about all of your medical conditions, including if you:
- have had an allergic reaction to palonosetron or another medicine for nausea or vomiting.
- have liver problems.
- have kidney problems.
- are pregnant or plan to become pregnant. AKYNZEO may harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if AKYNZEO passes into your breast milk. You and your doctor should decide if you will take AKYNZEO or breastfeed. You should not do both.
Tell your doctor about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
AKYNZEO and certain other medicines can affect each other, causing serious side effects.
How will I take or receive AKYNZEO?
- Take AKYNZEO exactly as your doctor tells you to take it.
- Take 1 AKYNZEO capsule by mouth, about 1 hour before you get your anti-cancer medicine (chemotherapy).
- AKYNZEO for injection will be given to you in your vein by I.V. (intravenous) infusion about 30 minutes before you start your chemotherapy treatment.Â
- Take AKYNZEO capsule with or without food.
- If you take too much AKYNZEO, call your doctor or go to the nearest hospital emergency room right away.
What are the possible side effects of AKYNZEO?
AKYNZEO may cause serious side effects, including:
- allergic reactions, such as anaphylaxis. Get emergency medical help right away if you get any of the following symptoms of a serious allergic reaction with AKYNZEO: hives, swollen face, trouble breathing, or chest pain.
- serotonin syndrome which can happen with AKYNZEO particularly with certain other medicines such as anti-depressants and anti-migraine medicines and can lead to death.Â
- Stop taking AKYNZEO capsules and go to the nearest hospital emergency room right away if you get any of the following symptoms of serotonin syndrome: agitation, hallucinations or other changes in mental status, dizziness, fast heartbeat, sweating, high body temperature, shaking (tremors), unsteady movements, muscle twitching (overactive reflexes), or seizures with or without nausea, vomiting, and diarrhea.
The most common side effects of AKYNZEO capsules and injection include: headache, weakness, fatigue, upset stomach, constipation, and skin redness.
These are not all the possible side effects of AKYNZEO. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store AKYNZEO capsules?
Store AKYNZEO at room temperature between 68°F to 77°F (20°C to 25°C).
General information about the safe and effective use of AKYNZEO
Medicines are sometimes prescribed for purposes other than those uled in a Patient Information leaflet. Do not use AKYNZEO for a condition for which it was not prescribed. Do not give AKYNZEO to other people, even if they have the same symptoms that you have. It may harm them. You can ask your doctor or pharmacist for information about AKYNZEO that is written for health professionals.
What are the ingredients in AKYNZEO capsules?
Active ingredients: netupitant and palonosetron hydrochloride
Inactive ingredients: butylated hydroxyanisole (BHA), croscarmellose sodium, gelatin, glycerin, magnesium stearate, microcrystalline cellulose, mono- and di-glycerides of capryl/capric acid, polyglyceryl dioleate, povidone K-30, purified water, red iron oxide, silicon dioxide, sodium stearyl fumarate, sorbitol, sucrose fatty acid esters, titanium dioxide and yellow iron oxide. It may contain traces of medium-chain triglycerides, lecithin, and denatured ethanol. AKYNZEO may contain small amounts of medium-chain triglycerides, lecithin, and denatured ethanol.
What are the ingredients in AKYNZEO for injection?
Active ingredients: fosnetupitant chloride hydrochoride and palonosetron hydrochloride
Inactive ingredients: mannitol, edetate disodium, sodium hydroxide, and hydrochloric acid may be added for pH adjustment.
What are the ingredients in AKYNZEO injection?
Active ingredients: fosnetupitant chloride hydrochloride and palonosetron hydrochloride Inactive ingredients: edetate disodium, mannitol and water for injection; sodium hydroxide and hydrochloric acid may be added for pH adjustment.
Manufactured by Helsinn Birex Pharmaceuticals, Dublin, IrelandÂ
for Helsinn Healthcare SA, Switzerland
Distributed by Helsinn Therapeutics (U.S.), Inc. Iselin, NJ 08830 under license of Helsinn Healthcare SA, Switzerland
AKYNZEO is a registered trademark of Helsinn Healthcare SA, Lugano, Switzerland
For more information, go to www.akynzeo.com
This Patient Information has been approved by the U.S. Food and Drug Administration.                                              Approved: May 2022
Instructions for opening the AKYNZEO pack of one capsule in one buler:
 1. Press buttons A and B together with one hand. 
 2. Pull the tab card on the right hand side with other hand. 
 3. Release buttons A and B while pulling the tab card. 
 4. Keep pulling the tab card until the pack is fully open. 
Package Label.principal Display Panel
Principal Display Panel NDC 69639-101-01Akynzeo(netupitant and palonosetron)capsules, 300mg/0.5mg

Package Label.principal Display Panel
Principal Display Panel NDC 69639-101-01Akynzeo(netupitant and palonosetron)capsules, 300mg/0.5mg
Package Label.principal Display Panel
Principal Display Panel NDC 69639-101-04Akynzeo(netupitant and palonosetron)capsules, 300mg/0.5mgFor Hospital Use Only

Package Label.principal Display Panel
Principal Display Panel NDC 69639-101-04Akynzeo(netupitant and palonosetron)capsules, 300mg/0.5mgFor Hospital Use Only
Package Label.principal Display Panel
Principal Display Panel NDC 69639-102Akynzeo(fosnetupitant and palonosetron) for injection235mg/0.25mg per vial
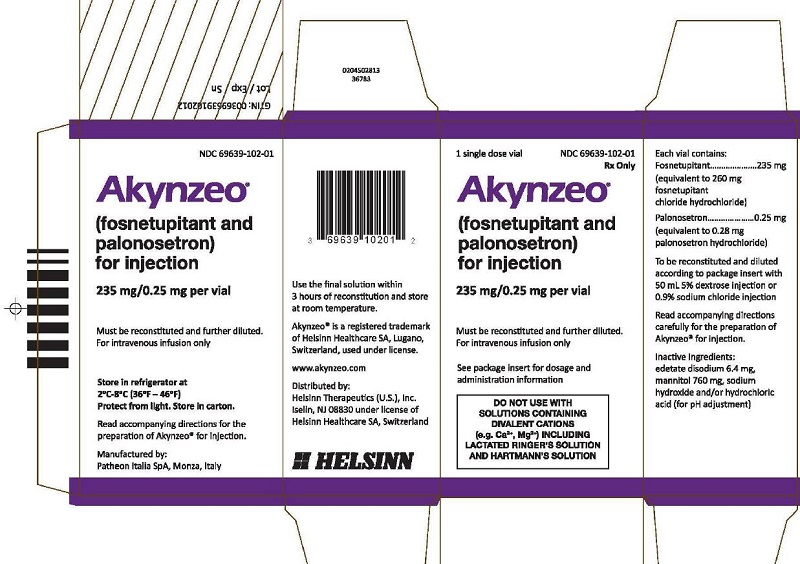
Package Label.principal Display Panel
Principal Display Panel NDC 69639-102Akynzeo(fosnetupitant and palonosetron) for injection235mg/0.25mg per vial
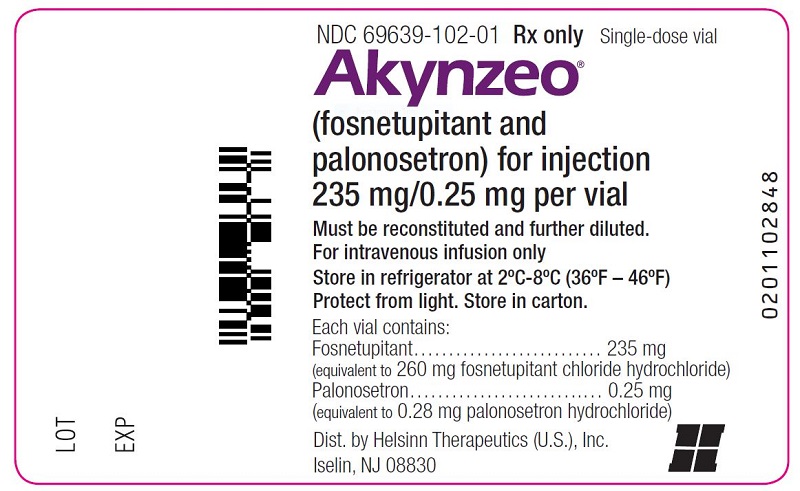
Package Label.principal Display Panel
Principal Display Panel NDC 69639-105Akynzeo(fosnetupitant and palonosetron) injection235mg/0.25mg per vial
Must be diluted. For intravenous infusion only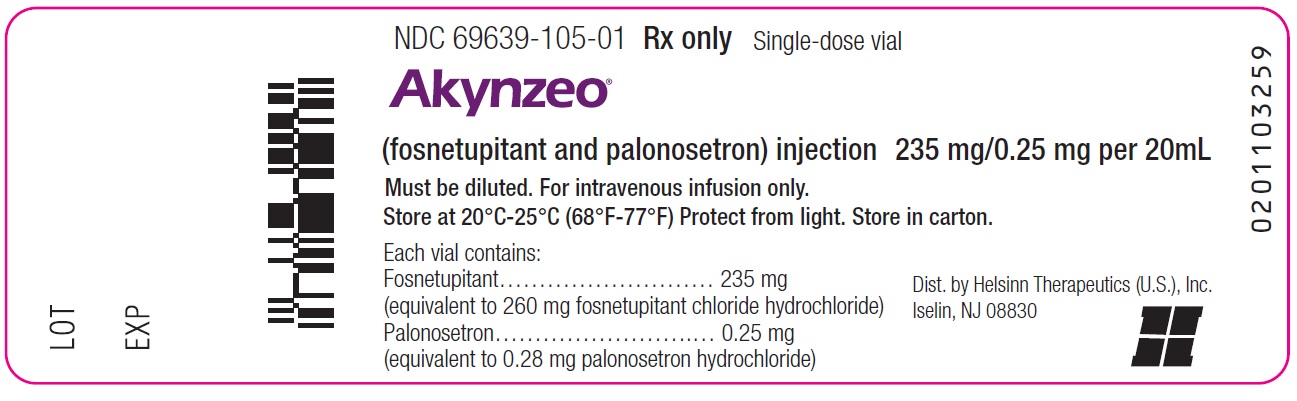
Package Label.principal Display Panel
Principal Display Panel NDC 69639-105Akynzeo(fosnetupitant and palonosetron) injection235mg/0.25mg per vial
Must be diluted. For intravenous infusion onlyMust be diluted. For intravenous infusion only
Package Label.principal Display Panel
Principal Display Panel Label
NDC 69639-106Akynzeo(fosnetupitant and palonosetron) injection235mg/0.25mg per 20mL
For intravenous infusion only.
Ready-to-Use Formulation and does NOT require further dilution
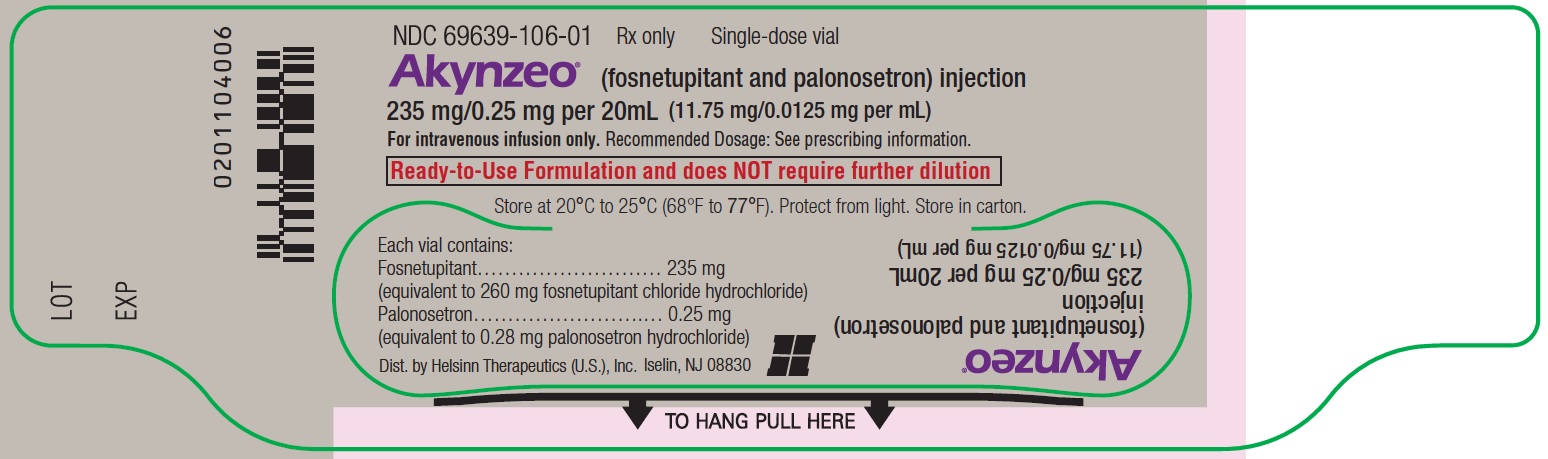
Principal Display Panel Carton
NDC 69639-106Akynzeo(fosnetupitant and palonosetron) injection235mg/0.25mg per 20mL
For intravenous infusion only.
Ready-to-Use Formulation and does NOT require further dilution

DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site

