Amlodipine and Olmesartan Medoxomil (amlodipine besylate 10 mg olmesartan medoxomil 40 mg) Dailymed
Generic: amlodipine and olmesartan medoxomil is used for the treatment of Diabetic Nephropathies Heart Failure Hyperaldosteronism Hypertension Hypotension Pregnancy Ventricular Dysfunction, Left Angina Pectoris, Variant Coronary Artery Disease
IMPRINT: K 29
SHAPE: round
COLOR: orange
All Imprints
amlodipine 5 mg olmesartan medoxomil 20 mg - k 27 round white
Boxed Warning
Warning: Fetal Toxicity
-
When pregnancy is detected, discontinue amlodipine and olmesartan medoxomil as soon as possible (
5.1 ,8.1 ). -
Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus (
5.1 ,8.1 ).
Go PRO for all pill images
Warning: Fetal Toxicity
WARNING: FETAL TOXICITY
See full prescribing information for complete boxed warning.
- When pregnancy is detected, discontinue amlodipine and olmesartan medoxomil as soon as possible (
5.1 ,8.1 ).- Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus (
5.1 ,8.1 ).
1 Indications And Usage
Amlodipine and olmesartan medoxomil tablets are indicated for the treatment of hypertension, alone or with other antihypertensive agents, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular (CV) events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes including the class to which this drug principally belongs. There are no controlled trials demonstrating risk reduction with amlodipine and olmesartan medoxomil tablets. Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than one drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC). Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly. Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal. Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy. Amlodipine and olmesartan medoxomil tablets may also be used as initial therapy in patients who are likely to need multiple antihypertensive agents to achieve their blood pressure goals. Patients with moderate or severe hypertension are at relatively high risk for cardiovascular events (such as strokes, heart attacks, and heart failure), kidney failure, and vision problems, so prompt treatment is clinically relevant. The decision to use a combination as initial therapy should be individualized and should be shaped by considerations such as baseline blood pressure, the target goal, and the incremental likelihood of achieving goal with a combination compared to monotherapy. Individual blood pressure goals may vary based upon the patient’s risk. Data from an 8-week, placebo-controlled, parallel-group factorial study [see Clinical Studies (14.1)] provide estimates of the probability of reaching a blood pressure goal with amlodipine and olmesartan medoxomil tablets compared to amlodipine or olmesartan medoxomil monotherapy. The figures below provide estimates of the likelihood of achieving the targeted systolic or diastolic blood pressure goals with amlodipine and olmesartan medoxomil tablets 10 mg/40 mg compared with amlodipine or olmesartan medoxomil monotherapy, based upon baseline systolic or diastolic blood pressure. The curve of each treatment group was estimated by logistic regression modeling from all available data of that treatment group. The right tail of each curve is less reliable because of small numbers of subjects with high baseline blood pressures.
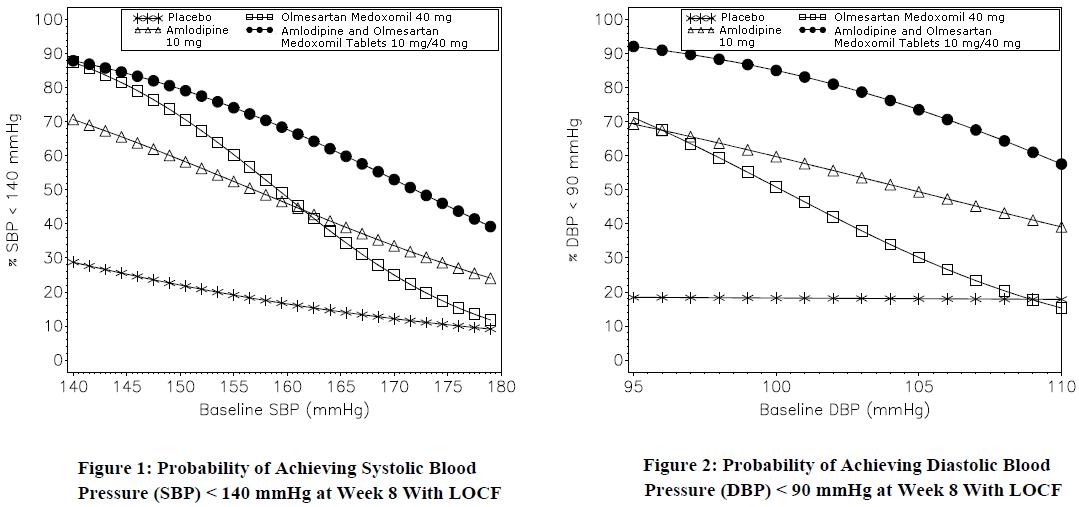
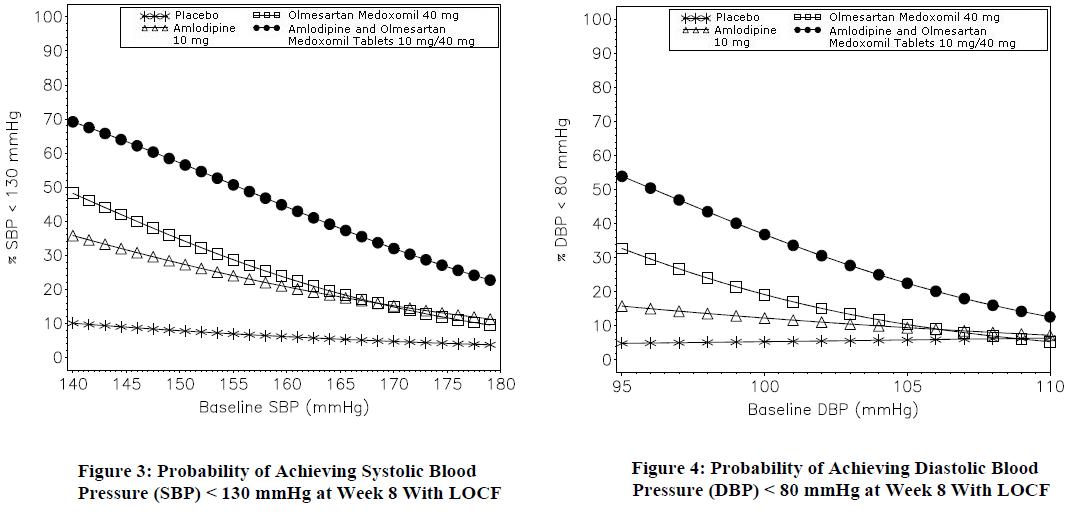
The figures above provide an approximation of the likelihood of reaching a targeted blood pressure goal (e.g., Week 8 SBP <140 mmHg or <130 mmHg or a DBP <90 mmHg or <80 mmHg) for the high-dose treatment groups evaluated in the study. Amlodipine and olmesartan medoxomil tablets 5 mg/20 mg, the lowest dose combination treatment group, increases the probability of reaching blood pressure goal compared with the highest dose monotherapies, amlodipine 10 mg and olmesartan medoxomil 40 mg. For example, a patient with a baseline blood pressure of 160/100 mmHg has about a 48% likelihood of achieving a goal of <140 mmHg (systolic) and a 51% likelihood of achieving a goal of <90 mmHg (diastolic) on monotherapy with olmesartan medoxomil 40 mg, and about a 46% likelihood of achieving a goal of <140 mmHg (systolic) and a 60% likelihood of achieving a goal of <90 mmHg (diastolic) on monotherapy with amlodipine 10 mg. The likelihood of achieving these same goals increases to 63% (systolic) and 71% (diastolic) on amlodipine and olmesartan medoxomil tablets 5 mg/20 mg, and to 68% (systolic) and 85% (diastolic) on amlodipine and olmesartan medoxomil tablets 10 mg/40 mg.
- Amlodipine and olmesartan medoxomil is a combination of amlodipine besylate, a dihydropyridine calcium channel blocker, and olmesartan medoxomil, an angiotensin II receptor blocker, indicated for the treatment of hypertension, alone or with other antihypertensive agents, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions
(1) .- Amlodipine and olmesartan medoxomil tablets may also be used as initial therapy in patients likely to need multiple antihypertensive agents to achieve their blood pressure goals
(1) . 
2 Dosage And Administration
The usual starting dose of amlodipine and olmesartan medoxomil tablets is 5 mg/20 mg once daily. The dosage can be increased after 1 to 2 weeks of therapy to a maximum dose of one 10 mg/40 mg tablet once daily as needed to control blood pressure [see Clinical Studies (14.1)].
- Recommended starting dose: 5 mg/20 mg once daily (
2 ).- Titrate as needed in two-week intervals up to a maximum of 10 mg/40 mg once daily (
2 ).
3 Dosage Forms And Strengths
Amlodipine and olmesartan medoxomil tablets USP are formulated for oral administration in the following strength combinations: Amlodipine and Olmesartan Medoxomil Tablets USP, 5 mg/20 mg are white colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė27‚Äô on the other side. Amlodipine and Olmesartan Medoxomil Tablets USP, 5 mg/40 mg are cream colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė28‚Äô on the other side. Amlodipine and Olmesartan Medoxomil Tablets USP, 10 mg/20 mg are peach colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė29‚Äô on the other side. Amlodipine and Olmesartan Medoxomil Tablets USP, 10 mg/40 mg are white colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė30‚Äô on the other side.
Tablets: (amlodipine/olmesartan medoxomil content) 5 mg/20 mg, 10 mg/20 mg, 5 mg/40 mg, and 10 mg/40 mg(3) .
4 Contraindications
Do not co-administer aliskiren with amlodipine and olmesartan medoxomil tablets in patients with diabetes [see Drug Interactions (7.2)].
- Do not co-administer aliskiren with amlodipine and olmesartan medoxomil tablets in patients with diabetes
(4) .
5 Warnings And Precautions
- Anticipate hypotension in volume- or salt-depleted patients with treatment initiation. Start treatment under close supervision (
5.2 ).- Increased angina or myocardial infarction may occur upon dosage initiation or increase (
5.3 ).- Impaired renal function: changes in renal function may occur (
5.4 ).- Sprue-like enteropathy has been reported. Consider discontinuation of amlodipine and olmesartan medoxomil in cases where no other etiology is found (
5.6 ).5.1 Fetal Toxicity
Amlodipine and olmesartan medoxomil can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue amlodipine and olmesartan medoxomil as soon as possible [see Use in Specific Populations (8.1)].
5.2 Hypotension in Volume- or Salt-Depleted Patients
Olmesartan medoxomil. In patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients (e.g., those being treated with high doses of diuretics) symptomatic hypotension may be anticipated after initiation of treatment with olmesartan medoxomil. Initiate treatment with amlodipine and olmesartan medoxomil under close medical supervision. If hypotension does occur, place the patient in the supine position and, if necessary, give an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
Amlodipine. Symptomatic hypotension is possible, particularly in patients with severe aortic stenosis. Because of the gradual onset of action, acute hypotension is unlikely.
5.3 Increased Angina or Myocardial Infarction
Patients, particularly those with severe obstructive coronary artery disease, may develop increased frequency, duration, or severity of angina or acute myocardial infarction on starting calcium channel blocker therapy or at the time of dosage increase. The mechanism of this effect has not been elucidated.
5.4 Impaired Renal Function
Changes in renal function may be anticipated in susceptible individuals treated with olmesartan medoxomil as a consequence of inhibiting the renin-angiotensin-aldosterone system. In patients whose renal function may depend upon the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe congestive heart failure), treatment with angiotensin converting enzyme inhibitors and angiotensin receptor antagonists has been associated with oliguria or progressive azotemia and (rarely) with acute renal failure and/or death. Similar effects may occur in patients treated with amlodipine and olmesartan medoxomil because of the olmesartan medoxomil component [see Drug Interactions (7) and Clinical Pharmacology (12.3)].
In studies of ACE inhibitors in patients with unilateral or bilateral renal artery stenosis, increases in serum creatinine or blood urea nitrogen (BUN) have been reported. There has been no long-term use of olmesartan medoxomil in patients with unilateral or bilateral renal artery stenosis, but similar effects would be expected with olmesartan medoxomil and amlodipine and olmesartan medoxomil.
5.5 Patients with Hepatic Impairment
Patients with hepatic impairment have decreased clearance of amlodipine. Starting amlodipine or adding amlodipine at 2.5 mg in hepatically impaired patients is recommended. The lowest dose of amlodipine and olmesartan medoxomil is 5/20 mg; therefore, initial therapy with amlodipine and olmesartan medoxomil is not recommended in hepatically impaired patients [see Use in Specific Populations (8.6)].
Since amlodipine is extensively metabolized by the liver and the plasma elimination half-life (t¬Ĺ) is 56 hours in patients with severely impaired hepatic function, titrate slowly when administering to patients with severe hepatic impairment.
5.6 Sprue-like Enteropathy
Severe, chronic diarrhea with substantial weight loss has been reported in patients taking olmesartan months to years after drug initiation. Intestinal biopsies of patients often demonstrated villous atrophy. If a patient develops these symptoms during treatment with olmesartan, exclude other etiologies. Consider discontinuation of amlodipine and olmesartan medoxomil in cases where no other etiology is identified.
5.7 Electrolyte Imbalances
Amlodipine and olmesartan medoxomil contains olmesartan, a drug that inhibits the renin-angiotensin system (RAS). Drugs that inhibit the RAS can cause hyperkalemia. Monitor serum electrolytes periodically.
6 Adverse Reactions
Most common adverse reaction (incidence ‚Č•3%) is edema(6.1) .
To report SUSPECTED ADVERSE REACTIONS, contact Aurobindo Pharma USA, Inc. at 1-866-850-2876 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice. Amlodipine and Olmesartan Medoxomil The data described below reflect exposure to amlodipine and olmesartan medoxomil in more than 1600 patients including more than 1000 exposed for at least 6 months and more than 700 exposed for 1 year. Amlodipine and olmesartan medoxomil was studied in one placebo-controlled factorial trial [se e  Clinical Trials (14.1)]. The population had a mean age of 54 years and included approximately 55% males. Seventy-one percent were Caucasian and 25% were Black. Patients received doses ranging from 5/20 mg to 10/40 mg orally once daily. The overall incidence of adverse reactions on therapy with amlodipine and olmesartan medoxomil was similar to that seen with corresponding doses of the individual components of amlodipine and olmesartan medoxomil, and to placebo. The reported adverse reactions were generally mild and seldom led to discontinuation of treatment (2.6% for amlodipine and olmesartan medoxomil and 6.8% for placebo). Edema Edema is a known, dose-dependent adverse effect of amlodipine but not of olmesartan medoxomil. The placebo-subtracted incidence of edema during the 8-week, randomized, double-blind treatment period was highest with amlodipine 10 mg monotherapy. The incidence was significantly reduced when 20 mg or 40 mg of olmesartan medoxomil was added to the 10 mg amlodipine dose.
Placebo-Subtracted Incidence of Edema During the Double-Blind Treatment Period *12.3% = actual placebo incidence Olmesartan Medoxomil Placebo 20 mg 40 mg Amlodipine Placebo Ôľć* -2.4% 6.2% 5 mg 0.7% 5.7% 6.2% 10 mg 24.5% 13.3% 11.2%
Across all treatment groups, the frequency of edema was generally higher in women than men, as has been observed in previous studies of amlodipine. There was a greater decrease in hemoglobin and hematocrit in patients treated with amlodipine and olmesartan medoxomil as compared to patients receiving either component.
Adverse reactions seen at lower rates during the double-blind period also occurred in the patients treated with amlodipine and olmesartan medoxomil at about the same or greater incidence as in patients receiving placebo. These included hypotension, orthostatic hypotension, rash, pruritus, palpitation, urinary frequency, and nocturia.
The adverse event profile obtained from 44 weeks of open-label combination therapy with amlodipine plus olmesartan medoxomil was similar to that observed during the 8-week, double-blind, placebo-controlled period. Initial Therapy Analyzing the data described above specifically for initial therapy, it was observed that higher doses of amlodipine and olmesartan medoxomil caused slightly more hypotension and orthostatic symptoms, but not at the recommended starting dose of amlodipine and olmesartan medoxomil 5/20 mg. No increase in the incidence of syncope or near syncope was observed. The incidences of discontinuation because of any treatment emergent adverse events in the double-blind phase are summarized in the table below.
Discontinuation for any Treatment Emergent Adverse Event1 1 Hypertension is counted as treatment failure and not as treatment emergent adverse event.N=160 to 163 subjects per treatment group. Olmesartan Medoxomil Placebo 10 mg 20 mg 40 mg Amlodipine Placebo 4.9% 4.3% 5.6% 3.1% 5 mg 3.7% 0.0% 1.2% 3.7% 10 mg 5.5% 6.8% 2.5% 5.6%
Amlodipine. Amlodipine has been evaluated for safety in more than 11,000 patients in U.S. and foreign clinical trials. Most adverse reactions reported during therapy with amlodipine were of mild or moderate severity. In controlled clinical trials directly comparing amlodipine (N=1730) in doses up to 10 mg to placebo (N=1250), discontinuation of amlodipine due to adverse reactions was required in only about 1.5% of amlodipine-­treated patients and about 1% of placebo-treated patients. The most common side effects were headache and edema. The incidence (%) of dose-related side effects was as follows:
Adverse Event PlaceboN=520 2.5 mgN=275 5 mgN=296 10 mgN=268 Edema 0.6 1.8 3.0 10.8 Dizziness 1.5 1.1 3.4 3.4 Flushing 0.0 0.7 1.4 2.6 Palpitation 0.6 0.7 1.4 4.5
For several adverse experiences that appear to be drug- and dose-related, there was a greater incidence in women than men associated with amlodipine treatment as shown in the following table:
Adverse Event Placebo Amlodipine Male=%(N=914) Female=% (N=336) Male=% (N=1218) Female=%(N=512) Edema 1.4 5.1 5.6 14.6 Flushing 0.3 0.9 1.5 4.5 Palpitation 0.9 0.9 1.4 3.3 Somnolence 0.8 0.3 1.3 1.6
Olmesartan medoxomil. Olmesartan medoxomil has been evaluated for safety in more than 3825 patients/subjects, including more than 3275 patients treated for hypertension in controlled trials. This experience included about 900 patients treated for at least 6 months and more than 525 treated for at least 1 year. Treatment with olmesartan medoxomil was well tolerated, with an incidence of adverse events similar to that seen with placebo. Events were generally mild, transient, and without relationship to the dose of olmesartan medoxomil. The overall frequency of adverse events was not dose related. Analysis of gender, age, and race groups demonstrated no differences between olmesartan medoxomil- and placebo-treated patients. The rate of withdrawals due to adverse events in all trials of hypertensive patients was 2.4% (i.e., 79/3278) of patients treated with olmesartan medoxomil and 2.7% (i.e., 32/1179) of control patients. In placebo-controlled trials, the only adverse event that occurred in more than 1% of patients treated with olmesartan medoxomil and at a higher incidence in olmesartan medoxomil treated patients vs. placebo was dizziness (3% vs. 1%).
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post-approval use of the individual components of amlodipine and olmesartan medoxomil. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Amlodipine. The following post-marketing event has been reported infrequently where a causal relationship is uncertain: gynecomastia. In post-marketing experience, jaundice and hepatic enzyme elevations (mostly consistent with cholestasis or hepatitis), in some cases severe enough to require hospitalization, have been reported in association with use of amlodipine. Postmarketing reporting has also revealed a possible association between extrapyramidal disorder and amlodipine. Olmesartan medoxomil. The following adverse reactions have been reported in post-marketing experience:
        Body as a Whole: asthenia, angioedema, anaphylactic reactions, peripheral edema
        Gastrointestinal: vomiting, diarrhea, sprue-like enteropathy [see Warnings and Precautions (5.6)]
        Metabolic and Nutritional Disorders: hyperkalemia
        Musculoskeletal: rhabdomyolysis         Urogenital System: acute renal failure, increased blood creatinine levels         Skin and Appendages: alopecia, pruritus, urticaria  Data from one controlled trial and an epidemiologic study have suggested that high-dose olmesartan may increase cardiovascular (CV) risk in diabetic patients, but the overall data are not conclusive. The randomized, placebo-controlled, double-blind ROADMAP trial (Randomized Olmesartan And Diabetes MicroAlbuminuria Prevention trial, n=4447) examined the use of olmesartan, 40 mg daily, vs. placebo in patients with type 2 diabetes mellitus, normoalbuminuria, and at least one additional risk factor for CV disease. The trial met its primary endpoint, delayed onset of microalbuminuria, but olmesartan had no beneficial effect on decline in glomerular filtration rate (GFR). There was a finding of increased CV mortality (adjudicated sudden cardiac death, fatal myocardial infarction, fatal stroke, revascularization death) in the olmesartan group compared to the placebo group (15 olmesartan vs. 3 placebo, HR 4.9, 95% confidence interval [CI], 1.4, 17), but the risk of nonfatal myocardial infarction was lower with olmesartan (HR 0.64, 95% CI 0.35, 1.18). The epidemiologic study included patients 65 years and older with overall exposure of > 300,000 patient-years. In the sub-group of diabetic patients receiving high-dose olmesartan (40 mg/d) for > 6 months, there appeared to be an increased risk of death (HR 2.0, 95% CI 1.1, 3.8) compared to similar patients taking other angiotensin receptor blockers. In contrast, high-dose olmesartan use in non-diabetic patients appeared to be associated with a decreased risk of death (HR 0.46, 95% CI 0.24, 0.86) compared to similar patients taking other angiotensin receptor blockers. No differences were observed between the groups receiving lower doses of olmesartan compared to other angiotensin blockers or those receiving therapy for < 6 months. Overall, these data raise a concern of a possible increased CV risk associated with the use of high-dose olmesartan in diabetic patients. There are, however, concerns with the credibility of the finding of increased CV risk, notably the observation in the large epidemiologic study for a survival benefit in non-diabetics of a magnitude similar to the adverse finding in diabetics.
7 Drug Interactions
Amlodipine (7.1 ):
- If simvastatin is co-administered with amlodipine, do not exceed 20 mg daily of simvastatin.
- Increased exposure of cyclosporine and tacrolimus.
- Increased exposure of amlodipine when coadministered with CYP3A inhibitors.
Olmesartan medoxomil (7.2 ):
- Nonsteroidal anti-inflammatory drugs (NSAIDS) may lead to increased risk of renal impairment and loss of antihypertensive effect.
- Dual inhibition of the renin-angiotensin system: Increased risk of renal impairment, hypotension, and hyperkalemia.
- Colesevelam hydrochloride: Consider administering olmesartan at least 4 hours before colesevelam hydrochloride dose.
- Lithium: Increases in serum lithium concentrations and lithium toxicity.
7.1 Drug Interactions with Amlodipine
Simvastatin: Co-administration of simvastatin with amlodipine increases the systemic exposure of simvastatin. Limit the dose of simvastatin in patients on amlodipine to 20 mg daily [see Clinical Pharmacology (12.3)].
Immunosuppressants: Amlodipine may increase the systemic exposure of cyclosporine or tacrolimus when co-administered. Frequent monitoring of trough blood levels of cyclosporine and tacrolimus is recommended and adjust the dose when appropriate [see Clinical Pharmacology (12.3)].
CYP3A Inhibitors: Co-administration of amlodipine with CYP3A inhibitors (moderate and strong) results in increased systemic exposure to amlodipine and may require dose reduction. Monitor for symptoms of hypotension and edema when amlodipine is co-administered with CYP3A inhibitors to determine the need for dose adjustment.
CYP3A Inducers: No information is available on the quantitative effects of CYP3A inducers on amlodipine. Blood pressure should be closely monitored when amlodipine is co-administered with CYP3A inducers.
7.2 Drug Interactions with Olmesartan Medoxomil
Non-Steroidal Anti-Inflammatory Agents including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors):
In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, co-administration of NSAIDs, including selective COX-2 inhibitors, with angiotensin II receptor antagonists, including olmesartan medoxomil, may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically in patients receiving olmesartan medoxomil and NSAID therapy.
The antihypertensive effect of angiotensin II receptor antagonists, including olmesartan medoxomil may be attenuated by NSAIDs including selective COX-2 inhibitors.
Dual Blockade of the Renin-Angiotensin System (RAS):
Dual blockade of the RAS with angiotensin receptor blockers, ACE inhibitors, or aliskiren is associated with increased risks of hypotension, hyperkalemia, and changes in renal function (including acute renal failure) compared to monotherapy. Most patients receiving the combination of two RAS inhibitors do not obtain any additional benefit compared to monotherapy. In general, avoid combined use of RAS inhibitors. Closely monitor blood pressure, renal function and electrolytes in patients on amlodipine and olmesartan medoxomil and other agents that affect the RAS.
Do not co-administer aliskiren with amlodipine and olmesartan medoxomil in patients with diabetes [see Contraindications (4)]. Avoid use of aliskiren with amlodipine and olmesartan medoxomil in patients with renal impairment (GFR <60 mL/min).
Use with Colesevelam Hydrochloride:
Concurrent administration of bile acid sequestering agent colesevelam hydrochloride reduces the systemic exposure and peak plasma concentration of olmesartan. Administration of olmesartan at least 4 hours prior to colesevelam hydrochloride decreased the drug interaction effect. Consider administering olmesartan at least 4 hours before the colesevelam hydrochloride dose [see Clinical Pharmacology (12.3)].
Lithium:
Increases in serum lithium concentrations and lithium toxicity have been reported during concomitant administration of lithium with angiotensin II receptor antagonists, including amlodipine and olmesartan medoxomil. Monitor serum lithium levels during concomitant use.
8 Use In Specific Populations
-  Lactation: Breastfeeding is not recommended (
8.2 ).- Geriatric: Not recommended for initial therapy in patients ‚Č•75 years old (
8.5 ).- Hepatic Impairment: Not recommended for initial therapy (
8.6 ).8.1 Pregnancy
Risk Summary
Amlodipine and olmesartan medoxomil can cause fetal harm when administered to a pregnant woman. Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death  [see Clinical Considerations]. Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents.
When pregnancy is detected, discontinue amlodipine and olmesartan medoxomil as soon as possible. Consider alternative antihypertensive therapy during pregnancy.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Hypertension in pregnancy increases the maternal risk for pre-eclampsia, gestational diabetes, premature delivery, and delivery complications (e.g., need for cesarean section and post-partum hemorrhage). Hypertension increases the fetal risk for intrauterine growth restriction and intrauterine death. Pregnant women with hypertension should be carefully monitored and managed accordingly.
Fetal/Neonatal Adverse Reactions
Olmesartan medoxomil
Oligohydramnios in pregnant women who use drugs affecting the renin-angiotensin system in the second and third trimesters of pregnancy can result in the following: reduced fetal renal function leading to anuria and renal failure, fetal lung hypoplasia, skeletal deformations, including skull hypoplasia, hypotension, and death.
Perform serial ultrasound examinations to assess the intra-amniotic environment. Fetal testing may be appropriate, based on the week of gestation. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Closely observe infants with histories of in utero exposure to olmesartan for hypotension, oliguria, and hyperkalemia. In neonates with a history of in utero exposure to olmesartan, if oliguria or hypotension occur, utilize measures to maintain adequate blood pressure and renal perfusion. Exchange transfusions or dialysis may be required as a means of reversing hypotension and supporting renal function [see Use in Specific Populations (8.4)].
Data Animal Data No reproductive studies have been conducted with the combination of olmesartan medoxomil, and amlodipine. However, these studies have been conducted for olmesartan medoxomil and amlodipine alone.
Olmesartan medoxomil
¬† No teratogenic effects were observed when olmesartan medoxomil was administered to pregnant rats at oral doses up to 1000 mg/kg/day (240 times the maximum recommended human dose [MRHD] on a mg/m2 basis) or pregnant rabbits at oral doses up to 1 mg/kg/day (half the MRHD on a mg/m2 basis; higher doses could not be evaluated for effects on fetal development as they were lethal to the does). In rats, significant decreases in pup birth weight and weight gain were observed at doses ‚Č•1.6 mg/kg/day, and delays in developmental milestones (delayed separation of ear auricular, eruption of lower incisors, appearance of abdominal hair, descent of testes, and separation of eyelids) and dose-dependent increases in the incidence of dilation of the renal pelvis were observed at doses ‚Č• 8 mg/kg/day. The no observed effect dose for developmental toxicity in rats is 0.3 mg/kg/day, about one-tenth the MRHD of 40 mg/day.
Amlodipine
No evidence of teratogenicity or other embryo/fetal toxicity was found when pregnant rats and rabbits were treated orally with amlodipine maleate at doses of up to 10 mg amlodipine/kg/day (respectively about 10 and 20 times the maximum recommended human dose of 10 mg amlodipine on a mg/m2 basis) during their respective periods of major organogenesis (calculations based on a patient weight of 60 kg). However, litter size was significantly decreased (by about 50%), and the number of intrauterine deaths was significantly increased (about 5-fold) in rats receiving amlodipine maleate at a dose equivalent to 10 mg amlodipine/kg/day for 14 days before mating and throughout mating and gestation. Amlodipine maleate has been shown to prolong both the gestational period and the duration of labor in rats at this dose.
8.2 Lactation
Risk Summary
There is limited information regarding the presence of amlodipine and olmesartan medoxomil in human milk, the effects on the breastfed infant, or the effects on milk production. Amlodipine is present in human milk. Olmesartan is present in rat milk [see Data]. Because of the potential for adverse effects on the nursing infant, advise a nursing woman that breastfeeding is not recommended during treatment with amlodipine and olmesartan medoxomil.
Data
Presence of olmesartan in milk was observed after a single oral administration of 5 mg/kg [14C] olmesartan medoxomil to lactating rats.
8.4 Pediatric Use
The safety and effectiveness of amlodipine and olmesartan medoxomil in pediatric patients have not been established.
8.5 Geriatric Use
Of the total number of subjects in the double-blind clinical study of amlodipine and olmesartan medoxomil, 20% (384/1940) were 65 years of age or older and 3% (62/1940) were 75 years or older. No overall differences in safety or effectiveness were observed between subjects 65 years of age or older and younger subjects. Elderly patients have decreased clearance of amlodipine. Starting amlodipine or adding amlodipine at 2.5 mg in patients ‚Č•75 years old is recommended. The lowest dose of amlodipine and olmesartan medoxomil is 5/20 mg; therefore, initial therapy with amlodipine and olmesartan medoxomil is not recommended in patients ‚Č•75 years old. Amlodipine. Reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Elderly patients have decreased clearance of amlodipine with a resulting increase of AUC of approximately 40% to 60%, and a lower initial dose may be required. Olmesartan medoxomil. Of the total number of hypertensive patients receiving olmesartan medoxomil in clinical studies, more than 20% were 65 years of age and over, while more than 5% were 75 years of age and older. No overall differences in effectiveness or safety were observed between elderly patients and younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
There are no studies of amlodipine and olmesartan medoxomil in patients with hepatic insufficiency, but both amlodipine and olmesartan medoxomil show moderate increases in exposure in patients with hepatic impairment.
The recommended initial dose of amlodipine in patients with severe hepatic impairment is 2.5 mg, a dose not available with amlodipine and olmesartan medoxomil.
Amlodipine. Amlodipine is extensively metabolized by the liver and the plasma elimination half-life (t¬Ĺ) is 56 hours in patients with severely impaired hepatic function [see Warnings and Precautions (5.5)].
Olmesartan medoxomil. Increases in AUC0-‚ąě and peak plasma concentration (Cmax) for olmesartan were observed with moderate hepatic impairment compared to those in matched controls with an increase in AUC of about 60%.
8.7 Renal Impairment
There are no studies of amlodipine and olmesartan medoxomil in patients with renal impairment. Amlodipine. The pharmacokinetics of amlodipine are not significantly influenced by renal impairment. Patients with renal failure may therefore receive the usual initial dose. Olmesartan medoxomil. Patients with renal insufficiency have elevated serum concentrations of olmesartan compared with patients with normal renal function. After repeated dosing, AUC was approximately tripled in patients with severe renal impairment (creatinine clearance <20 mL/min). No initial dosage adjustment is recommended for patients with moderate to marked renal impairment (creatinine clearance <40 mL/min).
8.8 Black Patients
Of the total number of subjects in the double-blind clinical study of amlodipine and olmesartan medoxomil, 25% (481/1940) were black patients. Amlodipine and olmesartan medoxomil was effective in treating black patients (usually a low-renin population), and the magnitude of blood pressure reduction in black patients approached that observed for non-black patients.
10 Overdosage
There is no information on overdosage with amlodipine and olmesartan medoxomil in humans. Amlodipine. Single oral doses of amlodipine maleate equivalent to 40 mg amlodipine/kg and 100 mg amlodipine/kg in mice and rats, respectively, caused deaths. Single oral amlodipine maleate doses equivalent to 4 or more mg amlodipine/kg or higher in dogs (11 or more times the maximum recommended human dose on a mg/m2 basis) caused a marked peripheral vasodilation and hypotension. Overdosage might be expected to cause excessive peripheral vasodilation with marked hypotension and possibly a reflex tachycardia. In humans, experience with intentional overdosage of amlodipine is limited. If massive overdose should occur, active cardiac and respiratory monitoring should be instituted. Frequent blood pressure measurements are essential. Should hypotension occur, cardiovascular support including elevation of the extremities and the judicious administration of fluids should be initiated. If hypotension remains unresponsive to these conservative measures, administration of vasopressors (such as phenylephrine) should be considered with attention to circulating volume and urine output. Intravenous calcium gluconate may help to reverse the effects of calcium entry blockade. As amlodipine is highly protein bound, hemodialysis is not likely to be of benefit. Olmesartan medoxomil. Limited data are available related to overdosage in humans. The most likely manifestations of overdosage would be hypotension and tachycardia; bradycardia could be encountered if parasympathetic (vagal) stimulation occurs. If symptomatic hypotension should occur, supportive treatment should be initiated. The dialyzability of olmesartan is unknown.
11 Description
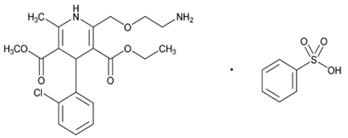
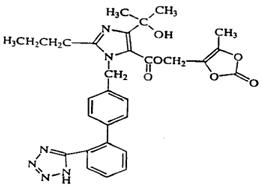
Amlodipine and olmesartan medoxomil tablets USP provided as a tablet for oral administration, is a combination of the calcium channel blocker (CCB) amlodipine besylate and the angiotensin II receptor blocker (ARB) olmesartan medoxomil. The amlodipine besylate component of amlodipine and olmesartan medoxomil tablets USP is chemically described as 3-ethyl-5-methyl (¬Ī)-2-[(2-aminoethoxy)methyl]-4-(2-chlorophenyl)-1,4-dihydro-6-methyl-3,5-pyridinedicarboxylate, monobenzenesulphonate. Its molecular formula is C20H25ClN2O5‚ÄĘC6H6O3S. Olmesartan medoxomil, a prodrug, is hydrolyzed to olmesartan during absorption from the gastrointestinal tract. The olmesartan medoxomil component of amlodipine and olmesartan medoxomil tablets USP is chemically described as 2,3-dihydroxy-2-butenyl 4-(1-hydroxy-1-methylethyl)-2-propyl-1-[p-(o-1H-tetrazol-5-ylphenyl)benzyl]imidazole-5-carboxylate, cyclic 2,3-carbonate. Its molecular formula is C29H30N6O6. The structural formula for amlodipine besylate is:„ÄÄ
The structural formula for olmesartan medoxomil is:„ÄÄ
Amlodipine and olmesartan medoxomil tablets USP contains amlodipine besylate USP, a white or almost white powder, and olmesartan medoxomil USP, a white to off-white, crystalline powder. The molecular weights of amlodipine besylate and olmesartan medoxomil are 567.1 and 558.59, respectively. Amlodipine besylate is slightly soluble in water and sparingly soluble in ethanol. Olmesartan medoxomil is practically insoluble in water and sparingly soluble in methanol. Each tablet of amlodipine and olmesartan medoxomil tablets USP also contains the following inactive ingredients: anhydrous lactose, colloidal silicon dioxide, croscarmellose sodium, macrogol/polyethylene glycol 3350, magnesium stearate, microcrystalline cellulose, polyvinyl alcohol, pregelatinized starch (maize), talc, and titanium dioxide. In addition, the 5 mg/40 mg and 10 mg/20 mg also contain iron oxide red and iron oxide yellow.
12 Clinical Pharmacology
12.1 Mechanism of Action
Amlodipine and olmesartan medoxomil. Amlodipine and olmesartan medoxomil is a combination of two antihypertensive drugs: a dihydropyridine calcium antagonist (calcium ion antagonist or slow-channel blocker), amlodipine besylate, and an angiotensin II receptor blocker, olmesartan medoxomil. The amlodipine component of amlodipine and olmesartan medoxomil inhibits the transmembrane influx of calcium ions into vascular smooth muscle and cardiac muscle, and the olmesartan medoxomil component of amlodipine and olmesartan medoxomil blocks the vasoconstrictor effects of angiotensin II. Amlodipine.   Experimental data suggests that amlodipine binds to both dihydropyridine and nonhydropyridine binding sites. The contractile processes of cardiac muscle and vascular smooth muscle are dependent upon the movement of extracellular calcium ions into these cells through specific ion channels. Amlodipine inhibits calcium ion influx across cell membranes selectively, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells. Negative inotropic effects can be detected in vitro but such effects have not been seen in intact animals at therapeutic doses. Serum calcium concentration is not affected by amlodipine. Within the physiologic pH range, amlodipine is an ionized compound (pKa=8.6), and its kinetic interaction with the calcium channel receptor is characterized by a gradual rate of association and dissociation with the receptor binding site, resulting in a gradual onset of effect. Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle to cause a reduction in peripheral vascular resistance and reduction in blood pressure. Olmesartan medoxomil.  Angiotensin II is formed from angiotensin I in a reaction catalyzed by angiotensin converting enzyme (ACE, kininase II). Angiotensin II is the principal pressor agent of the renin-angiotensin system, with effects that include vasoconstriction, stimulation of synthesis and release of aldosterone, cardiac stimulation and renal reabsorption of sodium. Olmesartan blocks the vasoconstrictor effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT1 receptor in vascular smooth muscle. Its action is, therefore, independent of the pathways for angiotensin II synthesis. An AT2 receptor is found also in many tissues, but this receptor is not known to be associated with cardiovascular homeostasis. Olmesartan has more than a 12,500-fold greater affinity for the AT1 receptor than for the AT2 receptor. Blockade of the renin-angiotensin system with ACE inhibitors, which inhibit the biosynthesis of angiotensin II from angiotensin I, is a mechanism of many drugs used to treat hypertension. ACE inhibitors also inhibit the degradation of bradykinin, a reaction also catalyzed by ACE. Because olmesartan does not inhibit ACE (kininase II), it does not affect the response to bradykinin. Whether this difference has clinical relevance is not yet known. Blockade of the angiotensin II receptor inhibits the negative regulatory feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and circulating angiotensin II levels do not overcome the effect of olmesartan on blood pressure.
12.2 Pharmacodynamics
Amlodipine. Following administration of therapeutic doses to patients with hypertension, amlodipine produces vasodilation resulting in a reduction of supine and standing blood pressures. These decreases in blood pressure are not accompanied by a significant change in heart rate or plasma catecholamine levels with chronic dosing. With chronic once daily oral administration, antihypertensive effectiveness is maintained for at least 24 hours. Plasma concentrations correlate with effect in both young and elderly patients. The magnitude of reduction in blood pressure with amlodipine is also correlated with the height of pretreatment elevation; thus, individuals with moderate hypertension (diastolic pressure 105 to 114 mmHg) had about a 50% greater response than patients with mild hypertension (diastolic pressure 90 to 104 mmHg). Normotensive subjects experienced no clinically significant change in blood pressures (+1/-2 mmHg). In hypertensive patients with normal renal function, therapeutic doses of amlodipine resulted in a decrease in renal vascular resistance and an increase in glomerular filtration rate and effective renal plasma flow without change in filtration fraction or proteinuria. As with other calcium channel blockers, hemodynamic measurements of cardiac function at rest and during exercise (or pacing) in patients with normal ventricular function treated with amlodipine have generally demonstrated a small increase in cardiac index without significant influence on dP/dt or on left ventricular end diastolic pressure or volume. In hemodynamic studies, amlodipine has not been associated with a negative inotropic effect when administered in the therapeutic dose range to intact animals and man, even when co-administered with beta-blockers to man. Similar findings, however, have been observed in normals or well-compensated patients with heart failure with agents possessing significant negative inotropic effects. Amlodipine does not change sinoatrial nodal function or atrioventricular conduction in intact animals or man. In clinical studies in which amlodipine was administered in combination with beta-blockers to patients with either hypertension or angina, no adverse effects on electrocardiographic parameters were observed. Olmesartan medoxomil. Olmesartan medoxomil doses of 2.5 mg to 40 mg inhibit the pressor effects of angiotensin I infusion. The duration of the inhibitory effect was related to dose, with doses of olmesartan medoxomil >40 mg giving >90% inhibition at 24 hours. Plasma concentrations of angiotensin I and angiotensin II and plasma renin activity (PRA) increase after single and repeated administration of olmesartan medoxomil to healthy subjects and hypertensive patients. Repeated administration of up to 80 mg olmesartan medoxomil had minimal influence on aldosterone levels and no effect on serum potassium.
12.3 Pharmacokinetics
The pharmacokinetics of amlodipine and olmesartan medoxomil from amlodipine and olmesartan medoxomil tablets are equivalent to the pharmacokinetics of amlodipine and olmesartan medoxomil when administered separately. The bioavailability of both components is well below 100%, but neither component is affected by food. The effective half-lives of amlodipine (45¬Ī11 hours) and olmesartan (7¬Ī1 hours) result in a 2- to 3- fold accumulation for amlodipine and negligible accumulation for olmesartan with once-daily dosing.
Amlodipine. After oral administration of therapeutic doses of amlodipine, absorption produces peak plasma concentrations between 6 and 12 hours. Absolute bioavailability is estimated as between 64% and 90%.
Olmesartan medoxomil. Olmesartan medoxomil is rapidly and completely bioactivated by ester hydrolysis to olmesartan during absorption from the gastrointestinal tract. The absolute bioavailability of olmesartan medoxomil is approximately 26%. After oral administration, the peak plasma concentration (Cmax) of olmesartan is reached after 1 to 2 hours. Food does not affect the bioavailability of olmesartan medoxomil.
Distribution
Amlodipine. Ex vivo studies have shown that approximately 93% of the circulating drug is bound to plasma proteins in hypertensive patients. Steady-state plasma levels of amlodipine are reached after 7 to 8 days of consecutive daily dosing.
Olmesartan medoxomil. The volume of distribution of olmesartan is approximately 17 L. Olmesartan is highly bound to plasma proteins (99%) and does not penetrate red blood cells. The protein binding is constant at plasma olmesartan concentrations well above the range achieved with recommended doses.
In rats, olmesartan crossed the blood-brain barrier poorly, if at all. Olmesartan passed across the placental barrier in rats and was distributed to the fetus. Olmesartan was distributed to milk at low levels in rats.
Metabolism and Excretion
Amlodipine. Amlodipine is extensively (about 90%) converted to inactive metabolites via hepatic metabolism. Elimination from the plasma is biphasic with a terminal elimination half-life of about 30 to 50 hours. Ten percent of the parent compound and 60% of the metabolites are excreted in the urine.
Olmesartan medoxomil. Following the rapid and complete conversion of olmesartan medoxomil to olmesartan during absorption, there is virtually no further metabolism of olmesartan. Total plasma clearance of olmesartan is 1.3 L/h, with a renal clearance of  0.6 L/h. Approximately 35% to 50% of the absorbed dose is recovered in urine while the remainder is eliminated in feces via the bile.
Olmesartan appears to be eliminated in a biphasic manner with a terminal elimination half-life of approximately 13 hours. Olmesartan shows linear pharmacokinetics following single oral doses of up to 320 mg and multiple oral doses of up to 80 mg. Steady-state levels of olmesartan are achieved within 3 to 5 days and no accumulation in plasma occurs with once-daily dosing.
Specific Populations Geriatric Patients
The pharmacokinetic properties of amlodipine and olmesartan medoxomil in the elderly are similar to those of the individual components.
Amlodipine. Elderly patients have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40% to 60%, and a lower initial dose may be required.
Olmesartan medoxomil. The pharmacokinetics of olmesartan medoxomil were studied in the elderly (‚Č•65 years). Overall, maximum plasma concentrations of olmesartan were similar in young adults and the elderly. Modest accumulation of olmesartan was observed in the elderly with repeated dosing; AUC—ē—ē, ŌĄ was 33% higher in elderly patients, corresponding to an approximate 30% reduction in CLR.
Pediatric Patients
Amlodipine. Sixty-two hypertensive patients aged 6 to 17 years received doses of amlodipine between 1.25 mg and 20 mg. Weight-adjusted clearance and volume of distribution were similar to values in adults.
Olmesartan medoxomil. The pharmacokinetics of olmesartan medoxomil have not been investigated in patients <18 years of age.
Male and Female Patients
Population pharmacokinetic analysis indicated that female patients had approximately 15% smaller clearances of olmesartan than male patients. Gender had no effect on the clearance of amlodipine.
Olmesartan medoxomil. Minor differences were observed in the pharmacokinetics of olmesartan medoxomil in women compared to men. AUC and Cmax were 10% to 15% higher in women than in men.
Patients with Renal Impairment
Amlodipine. The pharmacokinetics of amlodipine are not significantly influenced by renal impairment. Patients with renal failure may therefore receive the usual initial dose.
Olmesartan medoxomil. In patients with renal insufficiency, serum concentrations of olmesartan were elevated compared to subjects with normal renal function. After repeated dosing, the AUC was approximately tripled in patients with severe renal impairment (creatinine clearance <20 mL/min). The pharmacokinetics of olmesartan medoxomil in patients undergoing hemodialysis has not been studied. No initial dosage adjustment is recommended for patients with moderate to marked renal impairment (creatinine clearance <40 mL/min).
Patients with Hepatic Impairment  
Amlodipine. Patients with hepatic insufficiency have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40% to 60%.
Olmesartan medoxomil. Increases in AUC0-‚ąě and Cmax were observed in patients with moderate hepatic impairment compared to those in matched controls, with an increase in AUC of about 60%.
Heart Failure
Amlodipine. Patients with heart failure have decreased clearance of amlodipine with a resulting increase in AUC of approximately 40% to 60%.
Drug Interaction Studies
Simvastatin: Co-administration of multiple doses of 10 mg of amlodipine with 80 mg simvastatin resulted in a 77% increase in exposure to simvastatin compared to simvastatin alone. [see Drug Interactions (7.1)].
CYP3A inhibitors : Co-administration of a 180 mg daily dose of diltiazem with 5 mg amlodipine in elderly hypertensive patients resulted in a 60% increase in amlodipine systemic exposure. Erythromycin co-administration in healthy volunteers did not significantly change amlodipine systemic exposure. However, strong inhibitors of CYP3A (e.g., itraconazole, clarithromycin) may increase the plasma concentrations of amlodipine to a greater extent [see Drug Interactions (7.1)].
Cyclosporine: In a prospective study in renal transplant patients, an average 40% increase   in trough cyclosporine levels was observed in the presence of amlodipine. [see Drug Interactions (7.1)].
Colesevelam: Concomitant administration of 40 mg olmesartan medoxomil and 3750 mg colesevelam hydrochloride in healthy subjects resulted in 28% reduction in Cmax and 39% reduction in AUC of olmesartan. Lesser effects, 4% and 15% reduction in Cmax and AUC respectively, were observed when olmesartan medoxomil was administered 4 hours prior to colesevelam hydrochloride [see Drug Interactions (7.2)].
Cimetidine: Co-administration of amlodipine with cimetidine did not alter the pharmacokinetics of amlodipine.
Grapefruit juice: Co-administration of 240 mL of grapefruit juice with a single oral dose of amlodipine 10 mg in 20 healthy volunteers had no significant effect on the pharmacokinetics of amlodipine.
Maalox¬ģ (antacid): Co-administration of the antacid Maalox¬ģ with a single dose of amlodipine had no significant effect on the pharmacokinetics of amlodipine.
Sildenafil: A single 100 mg dose of sildenafil in subjects with essential hypertension had no effect on the pharmacokinetic parameters of amlodipine. When amlodipine and sildenafil were used in combination, each agent independently exerted its own blood pressure lowering effect.
Atorvastatin: Co-administration of multiple 10 mg doses of amlodipine with 80 mg of atorvastatin resulted in no significant change in the steady state pharmacokinetic parameters of atorvastatin.
Digoxin: Co-administration of amlodipine with digoxin did not change serum digoxin levels or digoxin renal clearance in normal volunteers.
No significant drug interactions were reported in studies in which olmesartan medoxomil was coadministered with digoxin in healthy volunteers. Ethanol (alcohol): Single and multiple 10 mg doses of amlodipine had no significant effect on the pharmacokinetics of ethanol.
Warfarin : Co-administration of amlodipine with warfarin did not change the warfarin prothrombin response time. No significant drug interactions were reported in studies in which olmesartan medoxomil was coadministered with warfarin in healthy volunteers. Antacids : The bioavailability of olmesartan medoxomil was not significantly altered by the co-administration of antacids [Al(OH)3/Mg(OH)2].
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Amlodipine. Rats and mice treated with amlodipine maleate in the diet for up to two years, at concentrations calculated to provide daily dosage levels of amlodipine 0.5, 1.25, and 2.5 mg/kg/day showed no evidence of a carcinogenic effect of the drug. For the mouse, the highest dose was, on a mg/m2 basis, similar to the maximum recommended human dose (MRHD) of amlodipine 10 mg/day. For the rat, the highest dose was, on a mg/m2 basis, about two and a half times the MRHD. (Calculations based on a 60 kg patient.) Mutagenicity studies conducted with amlodipine maleate revealed no drug related effects at either the gene or chromosome level. There was no effect on the fertility of rats treated orally with amlodipine maleate (males for 64 days and females for 14 days prior to mating) at doses of amlodipine up to 10 mg/kg/day (about 10 times the MRHD of 10 mg/day on a mg/m2 basis). Olmesartan medoxomil. Olmesartan was not carcinogenic when administered by dietary administration to rats for up to 2 years. The highest dose tested (2000 mg/kg/day) was, on a mg/m2 basis, about 480 times the maximum recommended human dose (MRHD) of 40 mg/day. Two carcinogenicity studies conducted in mice, a 6-month gavage study in the p53 knockout mouse and a 6-month dietary administration study in the Hras2 transgenic mouse, at doses of up to 1000 mg/kg/day (about 120 times the MRHD), revealed no evidence of a carcinogenic effect of olmesartan. Both olmesartan medoxomil and olmesartan tested negative in the in vitro Syrian hamster embryo cell transformation assay and showed no evidence of genetic toxicity in the Ames (bacterial mutagenicity) test. However, both were shown to induce chromosomal aberrations in cultured cells in vitro (Chinese hamster lung) and tested positive for thymidine kinase mutations in the in vitro mouse lymphoma assay. Olmesartan medoxomil tested negative in vivo for mutations in the MutaMouse intestine and kidney and for clastogenicity in mouse bone marrow (micronucleus test) at oral doses of up to 2000 mg/kg (olmesartan not tested). Fertility of rats was unaffected by administration of olmesartan at dose levels as high as 1000 mg/kg/day (240 times the MRHD) in a study in which dosing was begun 2 (female) or 9 (male) weeks prior to mating.
14 Clinical Studies
14.1 Amlodipine and Olmesartan Medoxomil
An 8-week multicenter, randomized, double-blind, placebo controlled, parallel group factorial study in patients with mild to severe hypertension was conducted to determine if treatment with amlodipine and olmesartan medoxomil was associated with clinically significant reduction in blood pressure compared to the respective monotherapies. The study randomized 1940 patients equally to one of the following 12 treatment arms: placebo, monotherapy treatment with amlodipine 5 mg or 10 mg, monotherapy treatment with olmesartan medoxomil 10 mg, 20 mg, or 40 mg, or combination therapy with amlodipine/olmesartan medoxomil at doses of 5 mg/10 mg, 5 mg/20 mg, 5 mg/40 mg, 10 mg/10 mg, 10 mg/20 mg, and 10 mg/40 mg. Patients discontinued their prior antihypertensive treatment. The mean baseline blood pressure of the study population was 164/102 mmHg. Of the total cohort, 970 patients were treated with the combination as initial therapy. Treatment with amlodipine and olmesartan medoxomil resulted in statistically significant greater reductions in diastolic and systolic blood pressure compared to the respective monotherapy components. Maximum antihypertensive effects were attained within 2 weeks after a change in dose.
The following table presents the results for mean reduction in seated systolic and diastolic blood pressure following 8 weeks of treatment with amlodipine and olmesartan medoxomil. Placebo-adjusted reductions from baseline in blood pressure were progressively greater with increases in dose of both amlodipine and olmesartan medoxomil components of amlodipine and olmesartan medoxomil tablets.
Reduction in Seated Systolic/Diastolic Blood Pressure (mmHg): Combination Therapy vs. Monotherapy Components (Double-Blind Treatment Period)   Olmesartan medoxomil (mmHg) Placebo 10 mg 20 mg 40 mg Amlodipine Placebo Mean Change Placebo-Adjusted Mean Change -5/-3 -- -12/-8 -8/-5 -14/-9 -10/-6 -16/-10 -13/-7 5 mg Mean Change Placebo-Adjusted Mean Change -15/-9 -12/-7 -24/-14 -20/-11 -24/-14 -20/-11 -25/-16 -22/-13 10 mg Mean Change Placebo-Adjusted Mean Change -20/-13 -16/-10 -25/-16 -22/-13 -29/-17 -25/-14 -30/-19 -26/-16
The antihypertensive effect of amlodipine and olmesartan medoxomil was similar in patients with and without prior antihypertensive medication use, in patients with and without diabetes, in patients ‚Č•65 years of age and <65 years of age, and in women and men. Limited data exist in patients ‚Č•75 years of age. Amlodipine and olmesartan medoxomil was effective in treating black patients (usually a low-renin population), and the magnitude of blood pressure reduction in black patients approached that observed for non-Black patients. This effect in black patients has been seen with ACE inhibitors, angiotensin receptor blockers, and beta-blockers. The blood pressure lowering effect was maintained throughout the 24-hour period with amlodipine and olmesartan medoxomil once daily, with trough-to-peak ratios for systolic and diastolic response between 71% and 82%. Upon completing the 8-week, double-blind, placebo-controlled study, 1684 patients entered a 44-week open-label extension and received combination therapy with amlodipine 5 mg plus olmesartan medoxomil 40 mg. During the open-label extension, patients whose blood pressure was not adequately controlled (i.e., did not achieve a blood pressure goal of <140/90 mmHg, or <130/80 mmHg for those patients with diabetes) on amlodipine/olmesartan medoxomil 5 mg/40 mg were titrated to amlodipine/olmesartan medoxomil 10 mg/40 mg. Patients whose blood pressure was still not adequately controlled were offered additional hydrochlorothiazide 12.5 mg and subsequently 25 mg as required to achieve adequate blood pressure goal. There are no trials of amlodipine and olmesartan medoxomil demonstrating reductions in cardiovascular risk in patients with hypertension, but at least one pharmacologically similar drug has demonstrated such benefits.
14.2 Amlodipine
The antihypertensive efficacy of amlodipine has been demonstrated in a total of 15 double-blind, placebo-controlled, randomized studies involving 800 patients on amlodipine and 538 on placebo. Once daily administration produced statistically significant placebo-corrected reductions in supine and standing blood pressures at 24 hours post-dose, averaging about 12/6 mmHg in the standing position and 13/7 mmHg in the supine position in patients with mild to moderate hypertension. Maintenance of the blood pressure effect over the 24-hour dosing interval was observed, with little difference in peak and trough effect.
14.3 Olmesartan Medoxomil
The antihypertensive effects of olmesartan medoxomil have been demonstrated in seven placebo-controlled studies at doses ranging from 2.5 mg to 80 mg for 6 to 12 weeks, each showing statistically significant reductions in peak and trough blood pressure. A total of 2693 patients (2145 olmesartan medoxomil; 548 placebo) with essential hypertension were studied. The blood pressure lowering effect was maintained throughout the 24-hour period with olmesartan medoxomil once daily, with trough-to-peak ratios for systolic and diastolic response between 60% and 80%.
16 How Supplied/storage And Handling
Amlodipine and Olmesartan Medoxomil Tablets USP, 5 mg/20 mg are white colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė27‚Äô on the other side.
¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†Bottles of 30¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬† NDC 65862-854-30 Amlodipine and Olmesartan Medoxomil Tablets USP, 5 mg/40 mg are cream colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė28‚Äô on the other side.
¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†Bottles of 30¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬† NDC 65862-855-30 Amlodipine and Olmesartan Medoxomil Tablets USP, 10 mg/20 mg are peach colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė29‚Äô on the other side.
¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†Bottles of 30¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬† NDC 65862-856-30 Amlodipine and Olmesartan Medoxomil Tablets USP, 10 mg/40 mg are white colored, round shaped, biconvex, film-coated tablets, debossed with ‚ÄėK‚Äô on one side and ‚Äė30‚Äô on the other side.
¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†Bottles of 30¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬†¬† NDC 65862-857-30 Store at 20¬į to 25¬įC (68¬į to 77¬įF); excursions permitted to 15¬į to 30¬įC (59¬į to 86¬įF)¬†[see USP Controlled Room Temperature].
17 Patient Counseling Information
Pregnancy: Advise female patients of childbearing age about the consequences of exposure to amlodipine and olmesartan medoxomil during pregnancy. Discuss treatment options with women planning to become pregnant. Tell patients to report pregnancies to their physicians as soon as possible [see Warnings and Precautions (5.1) and Use in Specific Populations (8.1)].
Lactation : Advise nursing women not to breastfeed during treatment with amlodipine and olmesartan medoxomil [see Use in Specific Populations (8.2)].
Potassium Supplements : Advise patients not to use potassium supplements or salt substitutes containing potassium without consulting their healthcare provider.
Maalox¬ģ is a registered trademark of Novartis Consumer Health, Inc.
Distributed by: Aurobindo Pharma USA, Inc. 279 Princeton-Hightstown RoadEast Windsor, NJ 08520 Manufactured by: Aurobindo Pharma Limited  Hyderabad-500 032, India Revised: 11/2022
Package Label-principal Display Panel - 5 Mg/20 Mg (30 Tablet Bottle)
NDC 65862-854-30 Rx only Amlodipine and Olmesartan Medoxomil Tablets, USP 5 mg/20 mg AUROBINDO                 30 Tablets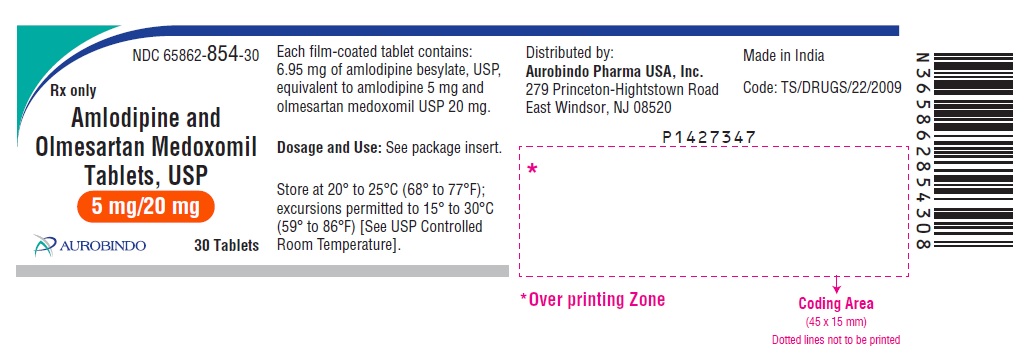
 
Package Label-principal Display Panel - 5 Mg/40 Mg (30 Tablet Bottle)
NDC 65862-855-30 Rx only Amlodipine and Olmesartan Medoxomil Tablets, USP 5 mg/40 mg AUROBINDO                    30 Tablets 
Package Label-principal Display Panel - 10 Mg/20 Mg (30 Tablet Bottle)
NDC 65862-856-30 Rx only Amlodipine and Olmesartan Medoxomil Tablets, USP 10 mg/20 mg AUROBINDO              30 Tablets 
Package Label-principal Display Panel - 10 Mg/40 Mg (30 Tablet Bottle)
NDC 65862-857-30 Rx only Amlodipine and Olmesartan Medoxomil Tablets, USP 10 mg/40 mg AUROBINDO                   30 Tablets 
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


