Betamethasone Sodium Phosphate and Betamethasone Acetate Dailymed
Generic: betamethasone sodium phosphate and betamethasone acetate is used for the treatment of Dermatitis, Atopic Facial Dermatoses Foot Dermatoses Hand Dermatoses Inflammation Leg Dermatoses Mycoses Pruritus Ani Psoriasis Scalp Dermatoses Dermatitis, Seborrheic Purpura, Thrombocytopenic, Idiopathic
Go PRO for all pill images
Description
Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is a sterile aqueous suspension containing 3 mg per milliliter betamethasone (equivalent to 3.95 mg betamethasone sodium phosphate USP) and 3 mg per milliliter betamethasone acetate. Inactive ingredients per mL: 8.9 mg dibasic sodium phosphate dihydrate; 3.8 mg monobasic sodium phosphate dihydrate; 0.1 mg edetate disodium; and 0.2 mg benzalkonium chloride as preservative. The pH is between 6.8 and 7.2.
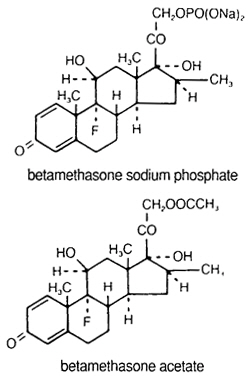
The formula for betamethasone sodium phosphate is C22H28FNa2O8P and it has a molecular weight of 516.40. Chemically, it is 9-Fluoro-11β,17,21-trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 21-(disodium phosphate).
The formula for betamethasone acetate is C24H31FO6 and it has a molecular weight of 434.50. Chemically, it is 9-Fluoro-11β,17,21-trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 21-acetate.
The chemical structures for betamethasone sodium phosphate and betamethasone acetate are as follows:
Betamethasone sodium phosphate is a white to practically white, odorless powder, and is hygroscopic. It is freely soluble in water and in methanol, but is practically insoluble in acetone and in chloroform.
Betamethasone acetate is a white to creamy white, odorless powder that sinters and resolidifies at about 165°C, and remelts at about 200°C-220°C with decomposition. It is practically insoluble in water, but freely soluble in acetone, and is soluble in alcohol and in chloroform.
Clinical Pharmacology
Glucocorticoids, naturally occurring and synthetic, are adrenocortical steroids that are readily absorbed from the gastrointestinal tract.
Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their anti-inflammatory effects in disorders of many organ systems. A derivative of prednisolone, betamethasone has a 16β-methyl group that enhances the anti-inflammatory action of the molecule and reduces the sodium- and water-retaining properties of the fluorine atom bound at carbon 9.
Betamethasone sodium phosphate, a soluble ester, provides prompt activity, while betamethasone acetate is only slightly soluble and affords sustained activity.
Indications And Usage
When oral therapy is not feasible, the intramuscular use of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is indicated as follows:
Allergic States
Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in asthma, atopic dermatitis, contact dermatitis, drug hypersensitivity reactions, perennial or seasonal allergic rhinitis, serum sickness, transfusion reactions.
Dermatologic Diseases
Bullous dermatitis herpetiformis, exfoliative erythroderma, mycosis fungoides, pemphigus, severe erythema multiforme (Stevens-Johnson syndrome).
Endocrine Disorders
Congenital adrenal hyperplasia, hypercalcemia associated with cancer, nonsuppurative thyroiditis.
Hydrocortisone or cortisone is the drug of choice in primary or secondary adrenocortical insufficiency. Synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation is of particular importance.
Gastrointestinal Diseases
To tide the patient over a critical period of the disease in regional enteritis and ulcerative colitis.
Hematologic Disorders
Acquired (autoimmune) hemolytic anemia, Diamond-Blackfan anemia, pure red cell aplasia, selected cases of secondary thrombocytopenia.
Miscellaneous
Trichinosis with neurologic or myocardial involvement, tuberculous meningitis with subarachnoid block or impending block when used with appropriate antituberculous chemotherapy.
Neoplastic Diseases
For palliative management of leukemias and lymphomas.
Nervous System
Acute exacerbations of multiple sclerosis; cerebral edema associated with primary or metastatic brain tumor or craniotomy.
Ophthalmic Diseases
Sympathetic ophthalmia, temporal arteritis, uveitis and ocular inflammatory conditions unresponsive to topical corticosteroids.
Renal Diseases
To induce diuresis or remission of proteinuria in idiopathic nephrotic syndrome or that due to lupus erythematosus.
Respiratory Diseases
Berylliosis, fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy, idiopathic eosinophilic pneumonias, symptomatic sarcoidosis.
Rheumatic Disorders
As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in acute gouty arthritis; acute rheumatic carditis; ankylosing spondylitis; psoriatic arthritis; rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy). For the treatment of dermatomyositis, polymyositis, and systemic lupus erythematosus.
The intra-articular or soft tissue administration of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is indicated as adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in acute gouty arthritis, acute and subacute bursitis, acute nonspecific tenosynovitis, epicondylitis, rheumatoid arthritis, synovitis of osteoarthritis.
The intralesional administration of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is indicated for alopecia areata; discoid lupus erythematosus; keloids; localized hypertrophic, infiltrated, inflammatory lesions of granuloma annulare, lichen planus, lichen simplex chronicus (neurodermatitis), and psoriatic plaques; necrobiosis lipoidica diabeticorum.
Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension may also be useful in cystic tumors of an aponeurosis or tendon (ganglia).
Contraindications
Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is contraindicated in patients who are hypersensitive to any components of this product (see DESCRIPTION ).
Intramuscular corticosteroid preparations are contraindicated for idiopathic thrombocytopenic purpura.
Warnings
Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension should not be administered intravenously.
Serious Neurologic Adverse Reactions with Epidural Administration
Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids have not been established, and corticosteroids are not approved for this use.
General
Rare instances of anaphylactoid/anaphylactic reactions with a possibility of shock have occurred in patients receiving parenteral corticosteroid therapy (see ADVERSE REACTIONS ). Use caution in patients who have a history of allergic reactions to corticosteroids.
In patients on corticosteroid therapy subjected to any unusual stress, hydrocortisone or cortisone is the drug of choice as a supplement during and after the event.
Cardio-renal
Average and large doses of corticosteroids can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Literature reports suggest an apparent association between use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure (see PRECAUTIONS , Drug Interactions ,Amphotericin B Injection and Potassium-Depleting Agents section).
Endocrine
Corticosteroids can produce reversible hypothalamic pituitary adrenal (HPA) axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment.
Metabolic clearance of corticosteroids is decreased in hypothyroid patients and increased in hyperthyroid patients. Changes in thyroid status of the patient may necessitate adjustment in dosage.
Pheochromocytoma crisis, which may be fatal, has been reported after administration of systemic corticosteroids, including betamethasone. In patients with suspected or identified pheochromocytoma, consider the risk of pheochromocytoma crisis prior to administering corticosteroids.
Immunosuppression and Increased Risk of Infection
Corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
- Reduce resistance to new infections
- Exacerbate existing infections
- Increase the risk of disseminated infections
- Increase the risk of reactivation or exacerbation of latent infections
- Mask some signs of infection
Corticosteroid-associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
Monitor for the development of infection and consider Betamethasone Sodium Phosphate and Betamethasone Acetate withdrawal or dosage reduction as needed.
Do not administer Betamethasone Sodium Phosphate and Betamethasone Acetate by an intraarticular, intrabursal, intratendinous or intralesional route in the presence of acute local infection.
Tuberculosis
If Betamethasone Sodium Phosphate and Betamethasone Acetate is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of the disease may occur. During prolonged Betamethasone Sodium Phosphate and Betamethasone Acetate therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella Zoster and Measles Viral Infections
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
- If a Betamethasone Sodium Phosphate and Betamethasone Acetate-treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If varicella develops, treatment with antiviral agents may be considered.
- If a Betamethasone Sodium Phosphate and Betamethasone Acetate-treated patient is exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated.
Hepatitis B Virus Reactivation
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (eg, prolonged) treatment with Betamethasone Sodium Phosphate and Betamethasone Acetate. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate, may exacerbate systemic fungal infections; therefore, avoid Betamethasone Sodium Phosphate and Betamethasone Acetate use in the presence of such infections unless Betamethasone Sodium Phosphate and Betamethasone Acetate is needed to control drug reactions. For patients on chronic Betamethasone Sodium Phosphate and Betamethasone Acetate therapy who develop systemic fungal infections, Betamethasone Sodium Phosphate and Betamethasone Acetate withdrawal or dosage reduction is recommended.
Corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating Betamethasone Sodium Phosphate and Betamethasone Acetate in patients who have spent time in the tropics or patients with unexplained diarrhea.
Corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
Avoid corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate, in patients with cerebral malaria.
Administration of live or live, attenuated vaccines is contraindicated in patients receiving immunosuppressive doses of corticosteroids. Killed or inactivated vaccines may be administered. However, the response to such vaccines cannot be predicted. Immunization procedures may be undertaken in patients who are receiving corticosteroids as replacement therapy, eg, for Addison's disease.
Neurologic
Reports of severe medical events have been associated with the intrathecal route of administration (see ADVERSE REACTIONS, Gastrointestinal and Neurologic/Psychiatric sections).
Results from one multicenter, randomized, placebo-controlled study with methylprednisolone hemisuccinate, an IV corticosteroid, showed an increase in early mortality (at 2 weeks) and late mortality (at 6 months) in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of corticosteroids, including Betamethasone Sodium Phosphate and Betamethasone Acetate, should not be used for the treatment of traumatic brain injury.
Ophthalmic
Use of corticosteroids may produce posterior subcapsular cataracts, increased intraocular pressure, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi, or viruses. Consider referral to an ophthalmologist for patients who develop ocular symptoms or use corticosteroid-containing products for more than 6 weeks. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should not be used in active ocular herpes simplex.
Kaposis Sarcoma
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma.
Precautions
General
This product, like many other steroid formulations, is sensitive to heat. Therefore, it should not be autoclaved when it is desirable to sterilize the exterior of the vial.
The lowest possible dose of corticosteroid should be used to control the condition under treatment. When reduction in dosage is possible, the reduction should be gradual.
Since complications of treatment with glucocorticoids are dependent on the size of the dose and the duration of treatment, a risk/benefit decision must be made in each individual case as to dose and duration of treatment and as to whether daily or intermittent therapy should be used.
Cardio-renal
As sodium retention with resultant edema and potassium loss may occur in patients receiving corticosteroids, these agents should be used with caution in patients with congestive heart failure, hypertension, or renal insufficiency.
Endocrine
Drug-induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy. Therefore, in any situation of stress occurring during that period, naturally occurring glucocorticoids (hydrocortisone cortisone), which also have salt-retaining properties, rather than betamethasone, are the appropriate choices as replacement therapy in adrenocortical deficiency states.
Gastrointestinal
Steroids should be used with caution in active or latent peptic ulcers, diverticulitis, fresh intestinal anastomoses, and nonspecific ulcerative colitis, since they may increase the risk of a perforation.
Signs of peritoneal irritation following gastrointestinal perforation in patients receiving corticosteroids may be minimal or absent.
There is an enhanced effect of corticosteroids in patients with cirrhosis.
Intra-Articular and Soft Tissue Administration
Intra-articular injected corticosteroids may be systemically absorbed.
Appropriate examination of any joint fluid present is necessary to exclude a septic process.
A marked increase in pain accompanied by local swelling, further restriction of joint motion, fever, and malaise are suggestive of septic arthritis. If this complication occurs and the diagnosis of sepsis is confirmed, appropriate antimicrobial therapy should be instituted.
Injection of a steroid into an infected site is to be avoided. Local injection of a steroid into a previously injected joint is not usually recommended.
Corticosteroid injection into unstable joints is generally not recommended.
Intra-articular injection may result in damage to joint tissues (see ADVERSE REACTIONS, Musculoskeletal section).
Musculoskeletal
Corticosteroids decrease bone formation and increase bone resorption both through their effect on calcium regulation (ie, decreasing absorption and increasing excretion) and inhibition of osteoblast function. This, together with a decrease in the protein matrix of the bone secondary to an increase in protein catabolism, and reduced sex hormone production, may lead to inhibition of bone growth in pediatric patients and the development of osteoporosis at any age. Special consideration should be given to patients at increased risk of osteoporosis (ie, postmenopausal women) before initiating corticosteroid therapy.
Neuro-psychiatric
Although controlled clinical trials have shown corticosteroids to be effective in speeding the resolution of acute exacerbations of multiple sclerosis, they do not show that they affect the ultimate outcome or natural history of the disease. The studies do show that relatively high doses of corticosteroids are necessary to demonstrate a significant effect (see DOSAGE AND ADMINISTRATION ).
An acute myopathy has been observed with the use of high doses of corticosteroids, most often occurring in patients with disorders of neuromuscular transmission (eg, myasthenia gravis), or in patients receiving concomitant therapy with neuromuscular blocking drugs (eg, pancuronium). This acute myopathy is generalized, may involve ocular and respiratory muscles, and may result in quadriparesis. Elevation of creatinine kinase may occur. Clinical improvement or recovery after stopping corticosteroids may require weeks to years.
Psychic derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression to frank psychotic manifestations. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids.
Information for Patients
Patients should be warned not to discontinue the use of corticosteroids abruptly or without medical supervision, to advise any medical attendants that they are taking corticosteroids and to seek medical advice at once should they develop fever or other signs of infection.
Persons who are on corticosteroids should be warned to avoid exposure to chickenpox or measles. Patients should also be advised that if they are exposed, medical advice should be sought without delay.
Drug Interactions
Aminoglutethimide may lead to a loss of corticosteroid-induced adrenal suppression.
When corticosteroids are administered concomitantly with potassium-depleting agents (ie, amphotericin B, diuretics), patients should be observed closely for development of hypokalemia. There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure.
Macrolide antibiotics have been reported to cause a significant decrease in corticosteroid clearance.
Concomitant use of anticholinesterase agents and corticosteroids may produce severe weakness in patients with myasthenia gravis. If possible, anticholinesterase agents should be withdrawn at least 24 hours before initiating corticosteroid therapy.
Coadministration of corticosteroids and warfarin usually results in inhibition of response to warfarin, although there have been some conflicting reports. Therefore, coagulation indices should be monitored frequently to maintain the desired anticoagulant effect.
Because corticosteroids may increase blood glucose concentrations, dosage adjustments of antidiabetic agents may be required.
Serum concentrations of isoniazid may be decreased.
Cholestyramine may increase the clearance of corticosteroids.
Increased activity of both cyclosporine and corticosteroids may occur when the two are used concurrently. Convulsions have been reported with this concurrent use.
Patients on digitalis glycosides may be at increased risk of arrhythmias due to hypokalemia.
Estrogens may decrease the hepatic metabolism of certain corticosteroids, thereby increasing their effect.
Drugs which induce hepatic microsomal drug-metabolizing enzyme activity may enhance the metabolism of corticosteroids and require that the dosage of the corticosteroid be increased.
Corticosteroids (including betamethasone) are metabolized by CYP3A4.
Ketoconazole has been reported to decrease the metabolism of certain corticosteroids by up to 60%, leading to an increased risk of corticosteroid side effects.
Coadministration with other strong CYP3A4 inhibitors (eg, itraconazole, clarithromycin, ritonavir, cobicistat-containing products) may lead to increased exposures of corticosteroids and therefore the potential for increased risk of systemic corticosteroid side effects.
Consider the benefit of coadministration versus the potential risk of systemic corticosteroid effects, in which case patients should be monitored for systemic corticosteroid side effects.
Concomitant use of aspirin (or other nonsteroidal anti-inflammatory agents) and corticosteroids increases the risk of gastrointestinal side effects. Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia. The clearance of salicylates may be increased with concurrent use of corticosteroids.
Corticosteroids may suppress reactions to skin tests.
Patients on prolonged corticosteroid therapy may exhibit a diminished response to toxoids and live or inactivated vaccines due to inhibition of antibody response. Corticosteroids may also potentiate the replication of some organisms contained in live attenuated vaccines. Route administration of vaccines or toxoids should be deferred until corticosteroid therapy is discontinued if possible (see WARNINGS, Infections, Vaccination section).
Carcinogenesis, Mutagenesis, Impairment of Fertility
No adequate studies have been conducted in animals to determine whether corticosteroids have a potential for carcinogenesis or mutagenesis.
Steroids may increase or decrease motility and number of spermatozoa in some patients.
Pregnancy
Corticosteroids have been shown to be teratogenic in many species when given in doses equivalent to the human dose. Animal studies in which corticosteroids have been given to pregnant mice, rats, and rabbits have yielded an increased incidence of cleft palate in the offspring. There are no adequate and well-controlled studies in pregnant women. Corticosteroids should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Infants born to mothers who have received corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Nursing Mothers
Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. Caution should be exercised when corticosteroids are administered to a nursing woman.
Pediatric Use
The efficacy and safety of corticosteroids in the pediatric population are based on the well-established course of effect of corticosteroids, which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome (>2 years of age), and aggressive lymphomas and leukemias (>1 month of age). Other indications for pediatric use of corticosteroids, eg, severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults, on the premises that the course of the diseases and their pathophysiology are considered to be substantially similar in both populations.
The adverse effects of corticosteroids in pediatric patients are similar to those in adults (see ADVERSE REACTIONS ). Like adults, pediatric patients should be carefully observed with frequent measurements of blood pressure, weight, height, intraocular pressure, and clinical evaluation for the presence of infection, psychosocial disturbances, thromboembolism, peptic ulcers, cataracts, and osteoporosis. Pediatric patients who are treated with corticosteroids by any route, including systemically administered corticosteroids, may experience a decrease in their growth velocity. This negative impact of corticosteroids on growth has been observed at low systemic doses and in the absence of laboratory evidence of HPA axis suppression (ie, cosyntropin stimulation and basal cortisol plasma levels). Growth velocity may therefore be a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA axis function. The linear growth of pediatric patients treated with corticosteroids should be monitored, and the potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of treatment alternatives. In order to minimize the potential growth effects of corticosteroids, pediatric patients should be titrated to the lowest effective dose.
Neonatal hypoglycemia has been reported after antenatal administration, especially in preterm, low birth weight infants, and when betamethasone is administered close to the time of delivery.
Geriatric Use
No overall differences in safety or effectiveness were observed between elderly subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and young patients, but greater sensitivity of some older individuals cannot be ruled out.
Adverse Reactions (listed Alphabetically, Under Each Subsection)
Allergic Reactions Anaphylactoid reaction, anaphylaxis, angioedema.
Cardiovascular Bradycardia, cardiac arrest, cardiac arrhythmias, cardiac enlargement, circulatory collapse, congestive heart failure, fat embolism, hypertension, hypertrophic cardiomyopathy in premature infants, myocardial rupture following recent myocardial infarction (see WARNINGS ), pulmonary edema, syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis.
Dermatologic Acne, allergic dermatitis, cutaneous and subcutaneous atrophy, dry scaly skin, ecchymoses and petechiae, edema, erythema, hyperpigmentation, hypopigmentation, impaired wound healing, increased sweating, rash, sterile abscess, striae, suppressed reactions to skin tests, thin fragile skin, thinning scalp hair, urticaria.
Endocrine Decreased carbohydrate and glucose tolerance, development of cushingoid state, glucosuria, hirsutism, hypertrichosis, increased requirements for insulin or oral hypoglycemic adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery, or illness), suppression of growth in pediatric patients.
Fluid and Electrolyte Disturbances Congestive heart failure in susceptible patients, fluid retention, hypokalemic alkalosis, potassium loss, sodium retention.
Gastrointestinal Abdominal distention, bowel/bladder dysfunction (after intrathecal administration), elevation in serum liver enzyme levels (usually reversible upon discontinuation), hepatomegaly, increased appetite, nausea, pancreatitis, peptic ulcer with possible perforation and hemorrhage, perforation of the small and large intestine (particularly in patients with inflammatory bowel disease), ulcerative esophagitis.
Metabolic Negative nitrogen balance due to protein catabolism.
Musculoskeletal Aseptic necrosis of femoral and humeral heads, calcinosis (following intra-articular or intralesional use), Charcot-like arthropathy, loss of muscle mass, muscle weakness, osteoporosis, pathologic fracture of long bones, postinjection flare (following intra-articular use), steroid myopathy, tendon rupture, vertebral compression fractures.
Neurologic/Psychiatric Convulsions, depression, emotional instability, euphoria, headache, increased intracranial pressure with papilledema (pseudotumor cerebri) usually following discontinuation of treatment, insomnia, mood swings, neuritis, neuropathy, paresthesia, personality changes, psychic disorders, vertigo. Arachnoiditis, meningitis, paraparesis/paraplegia, and sensory disturbances have occurred after intrathecal administration (see WARNINGS, Neurologic section).
Ophthalmic Exophthalmos, glaucoma, increased intraocular pressure, posterior subcapsular cataracts, rare instances of blindness associated with periocular injections, vision blurred.
Other Abnormal fat deposits, decreased resistance to infection, hiccups, increased or decreased motility and number of spermatozoa, malaise, moon face, weight gain.
Overdosage
Treatment of acute overdose is by supportive and symptomatic therapy. For chronic overdosage in the face of severe disease requiring continuous steroid therapy, the dosage of the corticosteroid may be reduced only temporarily, or alternate day treatment may be introduced.
Dosage And Administration
Benzyl alcohol as a preservative has been associated with a fatal "Gasping Syndrome" in premature infants and infants of low birth weight. Solutions used for further dilution of this product should be preservative-free when used in the neonate, especially the premature infant. The initial dosage of parenterally administered Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension may vary from 0.25 to 9.0 mg per day depending on the specific disease entity being treated. However, in certain overwhelming, acute, life-threatening situations, administrations in dosages exceeding the usual dosages may be justified and may be in multiples of the oral dosages.
It Should Be Emphasized That Dosage Requirements Are Variable and Must Be Individualized on the Basis of the Disease Under Treatment and the Response of the Patient. After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial drug dosage in small decrements at appropriate time intervals until the lowest dosage which will maintain an adequate clinical response is reached. Situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient's individual drug responsiveness, and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment. In this latter situation it may be necessary to increase the dosage of the corticosteroid for a period of time consistent with the patient's condition. If after long-term therapy the drug is to be stopped, it is recommended that it be withdrawn gradually rather than abruptly.
In the treatment of acute exacerbations of multiple sclerosis, daily doses of 30 mg of betamethasone for a week followed by 12 mg every other day for 1 month are recommended (see PRECAUTIONS, Neuro-psychiatric section).
In pediatric patients, the initial dose of betamethasone may vary depending on the specific disease entity being treated. The range of initial doses is 0.02 to 0.3 mg/kg/day in three or four divided doses (0.6 to 9 mg/m2bsa/day).
For the purpose of comparison, the following is the equivalent milligram dosage of the various glucocorticoids:
Cortisone, 25 Triamcinolone, 4 Hydrocortisone, 20 Paramethasone, 2 Prednisolone, 5 Betamethasone, 0.75 Prednisone, 5 Dexamethasone, 0.75 Methylprednisolone, 4
These dose relationships apply only to oral or intravenous administration of these compounds. When these substances or their derivatives are injected intramuscularly or into joint spaces, their relative properties may be greatly altered.
If coadministration of a local anesthetic is desired, Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension may be mixed with 1% or 2% lidocaine hydrochloride, using the formulations which do not contain parabens. Similar local anesthetics may also be used. Diluents containing methylparaben, propylparaben, phenol, etc., should be avoided, since these compounds may cause flocculation of the steroid. The required dose of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is first withdrawn from the vial into the syringe. The local anesthetic is then drawn in, and the syringe shaken briefly. Do not inject local anesthetics into the vial of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension.
Bursitis, Tenosynovitis, Peritendinitis
In acute subdeltoid, subacromial, olecranon, and prepatellar bursitis, one intrabursal injection of 1.0 mL Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension can relieve pain and restore full range of movement. Several intrabursal injections of corticosteroids are usually required in recurrent acute bursitis and in acute exacerbations of chronic bursitis. Partial relief of pain and some increase in mobility can be expected in both conditions after one or two injections. Chronic bursitis may be treated with reduced dosage once the acute condition is controlled. In tenosynovitis and tendinitis, three or four local injections at intervals of 1 to 2 weeks between injections are given in most cases. Injections should be made into the affected tendon sheaths rather than into the tendons themselves. In ganglions of joint capsules and tendon sheaths, injection of 0.5 mL directly into the ganglion cysts has produced marked reduction in the size of the lesions.
Rheumatoid Arthritis and Osteoarthritis
Following intra-articular administration of 0.5 to 2.0 mL of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension, relief of pain, soreness, and stiffness may be experienced. Duration of relief varies widely in both diseases. Intra-articular Injection of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is well tolerated in joints and periarticular tissues. There is virtually no pain on injection, and the "secondary flare" that sometimes occurs a few hours after intra-articular injection of corticosteroids has not been reported with Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension. Using sterile technique, a 20- to 24-gauge needle on an empty syringe is inserted into the synovial cavity and a few drops of synovial fluid are withdrawn to confirm that the needle is in the joint. The aspirating syringe is replaced by a syringe containing Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension and injection is then made into the joint.
Recommended Doses for Intra-articular Injection Size of joint Location Dose (mL) Very large Hip 1.0-2.0 Large Knee, ankle, shoulder 1.0 Medium Elbow, wrist 0.5-1.0 Small (metacarpophalangeal, interphalangeal) (sternoclavicular) Hand, chest 0.25-0.5
A portion of the administered dose of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is absorbed systemically following intra-articular injection. In patients being treated concomitantly with oral or parenteral corticosteroids, especially those receiving large doses, the systemic absorption of the drug should be considered in determining intra-articular dosage.
Dermatologic Conditions
In intralesional treatment, 0.2 mL/cm2 of Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is injected intradermally (not subcutaneously) using a tuberculin syringe with a 25-gauge, ½-inch needle. Care should be taken to deposit a uniform depot of medication intradermally. A total of no more than 1.0 mL at weekly intervals is recommended.
Disorders of the Foot
A tuberculin syringe with a 25-gauge, ¾-inch needle is suitable for most injections into the foot. The following doses are recommended at intervals of 3 days to a week.
Diagnosis Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension Dose (mL) Bursitis   under heloma durum or heloma molle 0.25-0.5   under calcaneal spur 0.5   over hallux rigidus or digiti quinti varus 0.5 Tenosynovitis,   periostitis of cuboid 0.5 Acute gouty arthritis 0.5-1.0
How Supplied
Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension is supplied as follows:
NDC 51754-5060-1:
Betamethasone Sodium Phosphate and Betamethasone Acetate Injectable Suspension, 5-mL multiple-dose vial; box of one. Inactive ingredients per mL: 8.9 mg dibasic sodium phosphate dihydrate; 3.8 mg monobasic sodium phosphate dihydrate; 0.1 mg edetate disodium; and 0.2 mg benzalkonium chloride as preservative.
STORAGE AND HANDLING SECTION
SHAKE WELL BEFORE USING.
Store at 25°C (77°F); excursions permitted to 15°C-30°C (59°-86°F) [see USP Controlled Room Temperature].
Protect from light.
Rx only
Distributed by: Exela Pharma Sciences, LLC, Lenoir, NC 28645, USA
© 2024 Organon group of companies. All rights reserved.
Revised: 7/2024
uspi-gog5166a-soi-2407r003
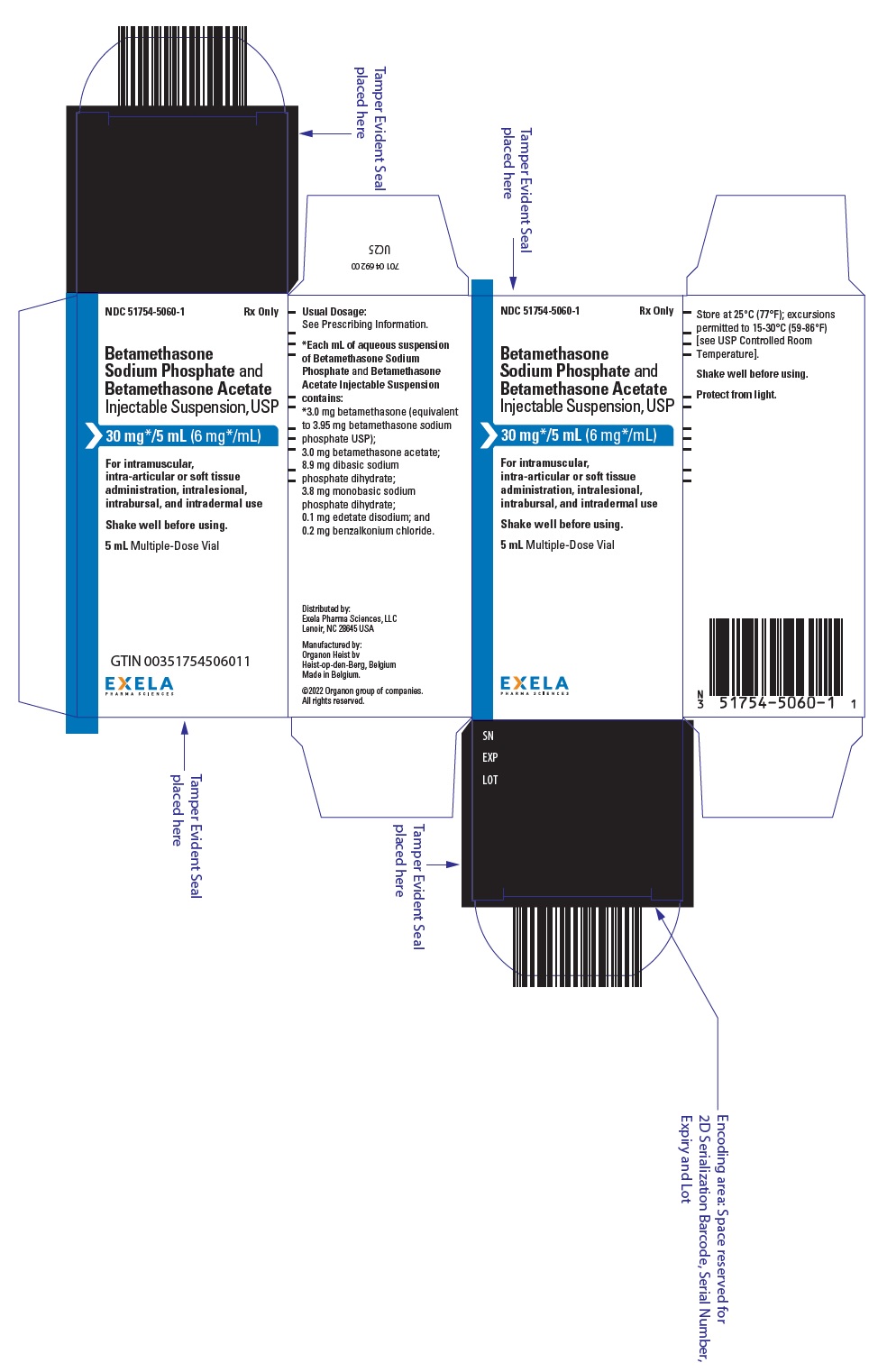
Principal Display Panel - 5 Ml Vial Box
NDC 51754-5060-1Rx Only
BetamethasoneSodium Phosphate and Betamethasone Acetate Injectable Suspension, USP
30 mg * /5 mL (6 mg*/mL)
For intramuscular, intra-articular or soft tissue administration, intralesional, intrabursal, and intradermal use
Shake well before using.
5 mL Multiple-Dose Vial
EXELA PHARMA SCIENCES
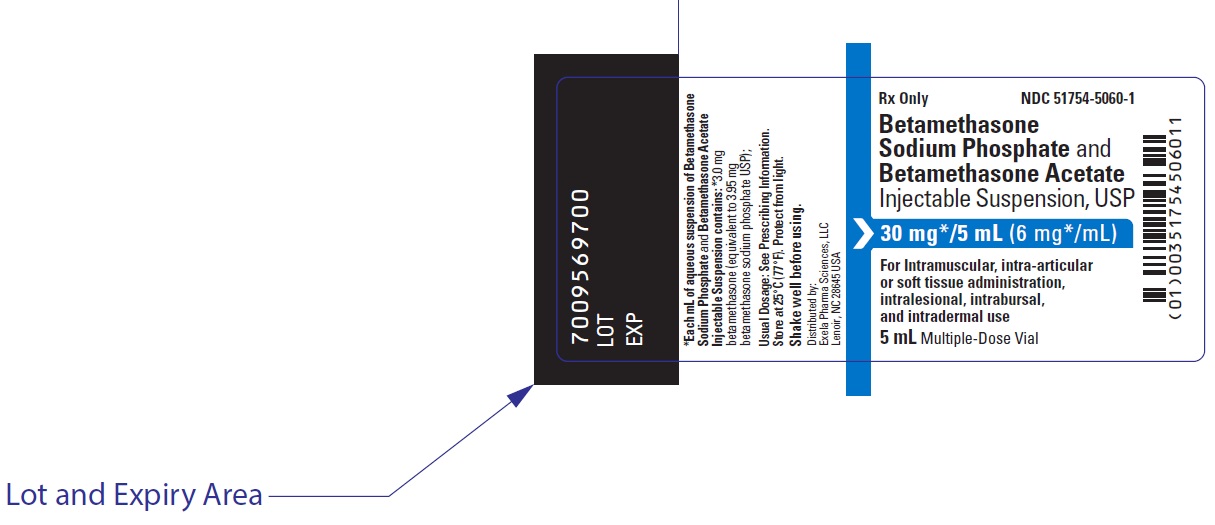
Principal Display Panel - 5 Ml Vial Label
Rx Only
NDC 51754-5060-1
BetamethasoneSodium Phosphate and Betamethasone Acetate Injectable Suspension, USP
30 mg * /5 mL (6 mg * /mL)
For Intramuscular, intra-articularor soft tissue administration,intralesional, intrabursal,and intradermal use
5 mL Multiple-Dose Vial
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site

