CYCLOSET (bromocriptine mesylate 0.8 mg) Dailymed
Generic: bromocriptine mesylate is used for the treatment of Acromegaly Adenoma Amenorrhea Galactorrhea Hyperprolactinemia Hypersensitivity Hypertension Hypogonadism Infertility Neuroleptic Malignant Syndrome Parkinson Disease Pregnancy Peripheral Vascular Diseases Myocardial Ischemia
Go PRO for all pill images
Recent Major Changes Section
Warnings and Precautions ( 5.3 )04/2020 Warnings and Precautions ( 5.7 )08/2020
1 Indications And Usage
CYCLOSET is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
CYCLOSET is an ergot derivative indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. (1 )
Limitations of Use:
- Should not be used to treat type 1 diabetes or diabetic ketoacidosis. (
1 )- Limited efficacy data in combination with thiazolidinediones. (
1 )- Efficacy has not been confirmed in combination with insulin. (
1 )
Limitations of Use
- CYCLOSET should not be used to treat type 1 diabetes or diabetic ketoacidosis.
- Limited efficacy data in combination with thiazolidinediones.
- Efficacy has not been confirmed in combination with insulin.
2 Dosage And Administration
- Taken within two hours after waking in the morning with food (
2.1 )- Initial dose is one tablet (0.8 mg) daily increased weekly by one tablet until maximal tolerated daily dose of 1.6 to 4.8 mg is achieved. (
2.2 )- Limit dose to 1.6 mg daily during concomitant use of a moderate CYP3A4 inhibitor. Avoid concomitant use with strong CYP3A4 inhibitors. (
2.3 )2.1 Recommended Dosing
The recommended dose of CYCLOSET is 1.6 mg to 4.8 mg administered once daily within two hours after waking in the morning. CYCLOSET should be taken with food to potentially reduce gastrointestinal side effects such as nausea. If the morning dose is missed, instruct patients to take their usual dose the following morning. Doses of CYCLOSET should not be doubled the following morning.
2.2 Titration
CYCLOSET should be initiated at one tablet (0.8 mg) and increased by one tablet per week until a maximum daily dose of 6 tablets (4.8 mg) or until the maximal tolerated number of tablets between 2 and 6 per day is reached.
2.3 Use with Concomitant Therapy
CYCLOSET dose should not exceed 1.6 mg once daily during concomitant use of a moderate CYP3A4 inhibitor (e.g., erythromycin). Avoid concomitant use of CYCLOSET and strong CYP3A4 inhibitors (e.g., azole antimycotics, HIV protease inhibitors) and ensure adequate washout of the strong CYP3A4 inhibitor drug before initiating CYCLOSET treatment [see Drug Interactions (7), Clinical Pharmacology (12.3)].
3 Dosage Forms And Strengths
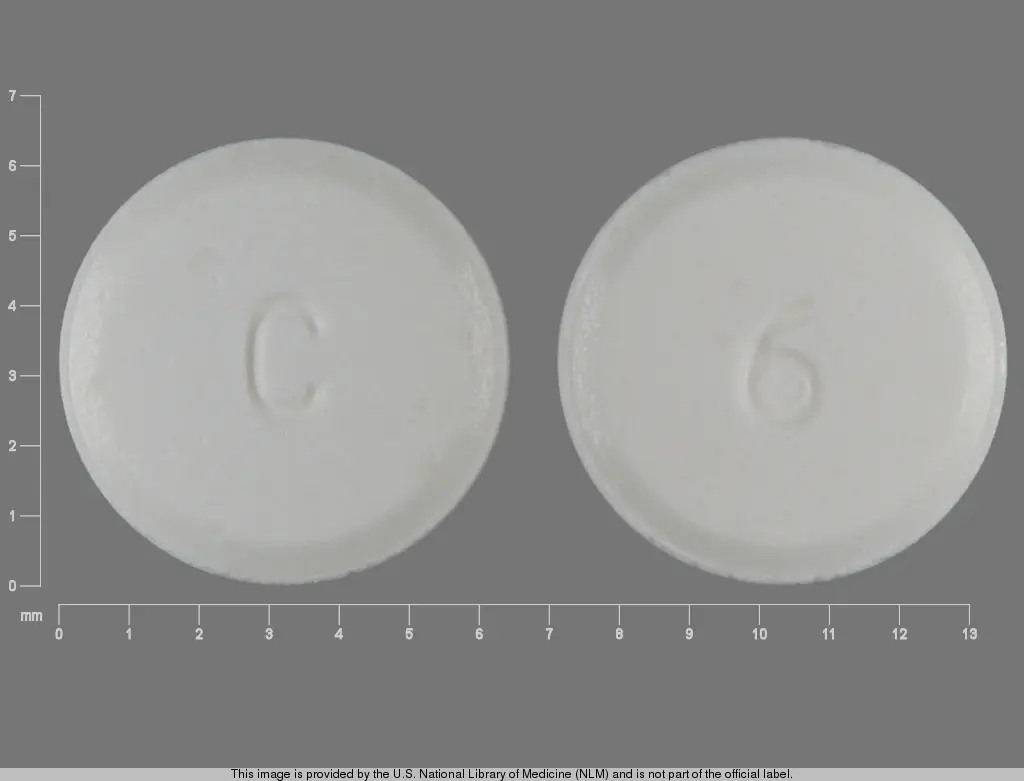
0.8 mg tablets are white and round, imprinted with "C" on one side and "9" on the other.
Tablets: 0.8 mg (3 )
4 Contraindications
CYCLOSET is contraindicated in:
- Patients with known hypersensitivity to bromocriptine, ergot-related drugs, or any of the excipients in CYCLOSET.
- Patients with syncopal migraine. Bromocriptine increases the likelihood of a hypotensive episode among patients with syncopal migraine. Loss of consciousness during a migraine may reflect dopamine receptor hypersensitivity. CYCLOSET is a dopamine receptor agonist and may, therefore, potentiate the risk for syncope in these patients.
- Postpartum patients. Serious and life-threatening adverse reactions have been reported with bromocriptine use in this population [see Warnings and Precautions (5.7), Adverse Reactions (6.2)].
- Lactating patients. CYCLOSET contains bromocriptine which inhibits lactation [see Use in Specific Populations (8.2)].
- Hypersensitivity to ergot-related drugs, bromocriptine or to any of the excipients in CYCLOSET. (
4 )- History of syncopal migraines. (
4 )- Postpartum patients (
4 ,5.7 )- Lactating patients (
4 ,8.2 )
5 Warnings And Precautions
- Hypotension: Can cause orthostatic hypotension and syncope, particularly upon initiation or dose escalation. Use caution in patients taking antihypertensive medications. Assess orthostatic vital signs prior to initiation of CYCLOSET and periodically thereafter. Advise patients during early treatment to avoid situations that could lead to injury if syncope was to occur. (
5.1 ,6.1 )- Psychosis: May exacerbate psychotic disorders or reduce the effectiveness of drugs that treat psychosis. Use in patients with severe psychotic disorders is not recommended. (
5.2 )- Impulse control/compulsive behaviors: Ask patients or their caregivers about new or increased gambling urges, sexual urges, uncontrolled spending, or other urges while being treated with CYCLOSET. Consider dose reduction or stopping CYCLOSET if a patient develops such urges. Use of CYCLOSET in patients with impulse control/compulsive behaviors is not recommended. (
5.3 ,6.2 ).- Somnolence: May cause somnolence. Advise patients not to operate heavy machinery if symptoms of somnolence occur. (
5.4 )- Interaction with dopamine antagonists: Concomitant use with dopamine antagonists such as neuroleptic agents may diminish the effectiveness of both drugs. Concomitant use is not recommended. (
5.5 ,7 )- Other dopamine receptor agonists: Effectiveness and safety are unknown in patients already taking dopamine receptor agonists for other indications. Concomitant use is not recommended. (
5.6 )- Risks in Postpartum Patients: Serious and life-threatening adverse reactions have been reported. (
5.7 ,6.2 )5.1 Hypotension
Hypotension, including orthostatic hypotension, can occur, particularly upon initiation of CYCLOSET therapy and with dose escalation. In a 52-week, randomized clinical trial of 3070 patients, hypotension was reported in 2.2% of patients randomized to CYCLOSET compared to 0.8% of patients randomized to placebo. Among CYCLOSET-treated patients reporting symptomatic hypotension, 98% were on at least one blood pressure medication compared to 73% on such medication in the total study population. In this trial, six CYCLOSET-treated patients (0.3%) reported orthostatic hypotension compared to 2 (0.2%) placebo-treated patients. All six patients were taking antihypertensive medications. Hypotension can result in syncope. In this trial, syncope due to any cause was reported in 1.6% of CYCLOSET-treated patients and 0.7% of placebo-treated patients [see Adverse Reactions (6.1)]. As a precaution, assessment of orthostatic vital signs is recommended prior to initiation of CYCLOSET and periodically thereafter. Advise patients during early treatment with CYCLOSET to make slow postural changes and to avoid situations that could lead to serious injury if syncope was to occur. Use caution in patients taking antihypertensive medications.
5.2 Psychotic Disorders
In patients with severe psychotic disorders, treatment with a dopamine receptor agonist such as CYCLOSET may exacerbate the disorder or may diminish the effectiveness of drugs used to treat the disorder. Therefore, the use of CYCLOSET in patients with severe psychotic disorders is not recommended.
5.3 Impulse Control/Compulsive Behaviors
There have been reports of patients experiencing intense urges to gamble, increased sexual urges, intense urges to spend money uncontrollably, and/or other intense urges, and the inability to control these urges while taking one or more of the medications, including bromocriptine, that increase central dopaminergic tone. In some cases, although not all, these urges were reported to have stopped when the dose was reduced, or the medication was discontinued. Because patients may not recognize these behaviors as abnormal, it is important to specifically ask patients or their caregivers about the development of new or increased gambling urges, sexual urges, uncontrolled spending, or other urges while being treated with CYCLOSET. Consider dose reduction or discontinuation if a patient develops such urges.
5.4 Somnolence
CYCLOSET may cause somnolence. In a 52-week, randomized clinical trial, 4.3% of CYCLOSET-treated patients and 1.3% of placebo-treated patients reported somnolence. None of these events were reported as serious, and the majority of patients reported resolution of somnolence over time. Inform patients of the risk of somnolence, particularly when initiating therapy with CYCLOSET. Patients experiencing somnolence should refrain from driving or operating heavy machinery.
5.5 Interaction with Dopamine Receptor Antagonists
Dopamine receptor antagonists, including neuroleptic agents that have dopamine D2 receptor antagonist properties (e.g., clozapine, olanzapine, ziprasidone), may reduce the effectiveness of CYCLOSET, and CYCLOSET may reduce the effectiveness of these agents. CYCLOSET has not been studied in patients taking neuroleptic drugs. The concomitant use of CYCLOSET and dopamine receptor antagonists, including neuroleptic drugs, is not recommended.
5.6 Other Dopamine Receptor Agonists
Other dopamine receptor agonists are indicated for the treatment of Parkinson's disease, hyperprolactinemia, restless leg syndrome, acromegaly, and other disorders. The effectiveness and safety of CYCLOSET in patients who are already taking one of these other dopamine receptor agonists is unknown. Concomitant use is not recommended.
5.7 Risks in Postpartum Patients
CYCLOSET is contraindicated in postpartum patients. Serious and life-threatening adverse reactions including hypertension, myocardial infarction, seizures, stroke and psychosis have been reported postmarketing in postpartum women who were administered bromocriptine for inhibition of lactation [see Adverse Reactions (6.2)]. These risks may be higher in postpartum patients with cardiovascular disease. The indication for use of bromocriptine for inhibition of postpartum lactation was withdrawn from bromocriptine-containing products and is not approved for CYCLOSET.
6 Adverse Reactions
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hypotension [see Warnings and Precautions (5.1)]
- Psychotic Disorders [see Warnings and Precautions (5.2)]
- Somnolence [see Warnings and Precautions (5.4)]
- Risks in Postpartum Women [see Warnings and Precautions (5.7)]
In controlled clinical trials, adverse reactions reported in ‚Č•5% of patients treated with CYCLOSET and reported more commonly than in patients treated with placebo, included nausea, fatigue, dizziness, vomiting, and headache. (6.1 )
Postmarketing reports with higher doses of bromocriptine used for other indications include psychotic disorders, hallucinations, and fibrotic complications. (6.2 )
To report SUSPECTED ADVERSE REACTIONS, contact VeroScience, LLC at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates reported in one clinical trial may not be easily compared to those rates reported in another clinical trial and may not reflect the rates actually observed in clinical practice.
The CYCLOSET safety trial was a 52-week, placebo-controlled study. A total of 3,070 patients were randomized to CYCLOSET (titrated to 1.6 to 4.8 mg daily, as tolerated) or placebo. The study population had a mean baseline age of 60 years (range 27-80) and 33% were 65 years of age or older. Approximately 43% of the patients were female, 68% were Caucasian, 17% were Black, 13% were Hispanic, and 1% were Asian. The mean baseline body mass index was 32 kg/m2. The mean duration of diabetes at baseline was 8 years, and the mean baseline HbA1c was 7.0% with a mean baseline fasting plasma glucose of 142 mg/dL. At baseline, 12% of patients were treated with diet only, 40% were treated with one oral antidiabetic agent, 33% were treated with two oral antidiabetic agents, and 16% were treated with insulin alone or insulin in combination with an oral antidiabetic agent. At baseline, 76% of patients reported a history of hypercholesterolemia, 75% reported a history of hypertension, 11% reported a history of revascularization surgery, 10% reported a history of myocardial infarction, 10% reported a history of angina, and 5% reported a history of stroke. Forty-seven percent of the CYCLOSET-treated patients and 32% of the placebo-treated patients prematurely discontinued treatment.
Table 1 summarizes the adverse reactions reported in ‚Č•5% of patients treated with CYCLOSET in clinical trials regardless of investigator assessment of causality. The most commonly reported adverse reactions (nausea, fatigue, vomiting, headache, dizziness) lasted a median of 14 days and were more likely to occur during the initial titration of CYCLOSET. There were no differences in the pattern of common adverse reactions across race groups or age groups (<65 years old vs. >65 years old). In the 52-week CYCLOSET safety trial, 11.5% of CYCLOSET-treated women compared to 3.6% of placebo-treated women reported vomiting. In this same trial, 5.4% of CYCLOSET-treated men compared to 2.8% of placebo-treated men reported vomiting.
Table 1: Adverse Reactions Occurring in ‚Č•5% in CYCLOSET-Treated Patients and More Frequent than in Placebo in CYCLOSET Clinical Trials All randomized subjects receiving at least one dose of study drug Monotherapy CYCLOSET 1.6 mg ‚Äď 4.8 mg N (%) Placebo N (%) N = 159 N = 80 N = 79 Nausea 26 (32.5) 6 (7.6) Rhinitis 11 (13.8) 3 (3.8) Headache 10 (12.5) 7 (8.9) Asthenia 10 (12.5) 5 (6.3) Dizziness 10 (12.5) 6 (7.6) Constipation 9 (11.3) 3 (3.8) Sinusitis 8 (10.0) 2 (2.5) Diarrhea 7 (8.8) 4 (5.1) Amblyopia 6 (7.5) 1 (1.3) Dyspepsia 6 (7.5) 2 (2.5) Vomiting 5 (6.3) 1 (1.3) Infection 5 (6.3) 4 (5.1) Anorexia 4 (5.0) 1 (1.3) Adjunct to Sulfonylurea (2 pooled 24-week studies) N = 494 N = 244 N = 250 Nausea 62 (25.4) 12 (4.8) Asthenia 46 (18.9) 20 (8.0) Headache 41 (16.8) 40 (16.0) Flu syndrome 23 (9.4) 19 (7.6) Constipation 24 (9.8) 11 (4.4) Cold 20 (8.2) 20 (8.0) Dizziness 29 (11.9) 14 (5.6) Rhinitis 26 (10.7) 12 (4.8) Sinusitis 18 (7.4) 16 (6.4) Somnolence 16 (6.6) 5 (2.0) Vomiting 13 (5.3) 8 (3.2) Amblyopia 13 (5.3) 6 (2.4) 52-Week Safety Trial The Safety Trial enrolled patients treated with diet or no more than 2 antidiabetic medications (metformin, insulin secretagogues such as a sulfonylurea, thiazolidinediones, alpha glucosidase inhibitors, and/or insulin). N = 3070 N = 2054 N = 1016 Nausea 661 (32.2) 77 (7.6) Dizziness 303 (14.8) 93 (9.2) Fatigue 285 (13.9) 68 (6.7) Headache 235 (11.4) 84 (8.3) Vomiting 167 (8.1) 32 (3.1) Diarrhea 167 (8.1) 81 (8.0) Constipation 119 (5.8) 52 (5.1)
Hypoglycemia
In the monotherapy trial, hypoglycemia, a blood glucose level of less than 60 mg/dL, was reported in 2 CYCLOSET-treated patients (3.7%) and 1 placebo-treated patient (1.3%). In the add-on to sulfonylurea trials, the incidence of hypoglycemia was 8.6% among the CYCLOSET-treated patients and 5.2% among the placebo-treated patients. In the CYCLOSET safety trial, hypoglycemia was defined as any of the following: 1) symptoms suggestive of hypoglycemia that promptly resolved with appropriate intervention, 2) symptoms with a measured glucose <60 mg/dL or 3) measured glucose below 49 mg/dL regardless of symptoms. In the 52-week safety trial, the incidence of hypoglycemia was 6.9% among the CYCLOSET-treated patients and 5.3% among the placebo-treated patients. In the safety trial, severe hypoglycemia was defined as an inability to self-treat neurological symptoms consistent with hypoglycemia that occurred in the setting of a measured blood glucose <50 mg/dL (or evidence of prompt resolution of these symptoms with administration of oral carbohydrates, subcutaneous glucagon, or intravenous glucose if blood glucose was not measured). In this trial, severe hypoglycemia was reported among 0.5% of CYCLOSET-treated patients and 1% of placebo-treated patients.
Syncope
In clinical trials, syncope was reported in 1.4% of the 2,500 CYCLOSET-treated patients and 0.6% of the 1,454 placebo-treated patients. Among the 3,070 patients studied in the 52-week safety trial, 33 CYCLOSET-treated patients (1.6%) and 7 placebo-treated patients (0.7%) reported syncope. In this trial, electrocardiograms were not available at the time of these events, but an assessment of routine electrocardiograms obtained during the course of the trial did not identify arrhythmias or QTc interval prolongation among the CYCLOSET-treated patients reporting syncope.
Central Nervous System
In the 52-week safety trial, somnolence and hypoesthesia were the only adverse reactions within the nervous system organ class that were reported at a rate of <5% and ‚Č•1% and that occurred at a numerically greater frequency among CYCLOSET-treated patients (CYCLOSET 4.3% vs. placebo 1.3% for somnolence; CYCLOSET 1.4% vs. placebo 1.1% for hypoesthesia).
Fibrotic-Related Complications
Among the CYCLOSET-treated patients (n = 2500) in controlled clinical trials, there was one case (0.04% event rate) of an adverse reaction of pulmonary fibrosis.
Serious Adverse Reactions and Cardiovascular Safety
The primary endpoint of the 52-week safety trial was the occurrence of all serious adverse reactions. A secondary endpoint was the occurrence of the composite of myocardial infarction, stroke, coronary revascularization, hospitalization for angina, and hospitalization for congestive heart failure.
All serious adverse reactions and cardiovascular endpoints were adjudicated by an independent event adjudication committee. Serious adverse reactions occurred in 176/2054 (8.5%) CYCLOSET-treated patients and 98/1016 (9.6%) placebo-treated patients. The hazard ratio comparing CYCLOSET to placebo for the time to first occurrence of a serious adverse reaction was 1.02 (upper bound of one-sided 96% confidence interval, 1.27). None of the serious adverse reactions grouped by System-Organ-Class occurred more than 0.3 percentage points higher with CYCLOSET than with placebo. The composite cardiovascular endpoint occurred in 31 (1.5%) CYCLOSET-treated patients and 30 (3.0%) placebo-treated patients. The hazard ratio comparing CYCLOSET to placebo for the time-to-first occurrence of the prespecified composite cardiovascular endpoint was 0.58 (two-sided 95% confidence interval, 0.35 ‚Äď 0.96). Therefore, the incidence of this composite endpoint was not increased with CYCLOSET relative to placebo.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of other formulations of bromocriptine mesylate for indications for which CYCLOSET is not approved (e.g., hyperprolactinemia, acromegaly, and Parkinson's disease), generally at doses higher than those approved for the treatment of type 2 diabetes. Because these reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hallucinations
Hallucinations and mental confusion including delusions have been reported with bromocriptine.
Fibrotic-Related Complications
Fibrotic complications, including cases of retroperitoneal fibrosis, pulmonary fibrosis, pleural effusion, pleural thickening, pericarditis and pericardial effusions have been reported. These complications do not always resolve when bromocriptine is discontinued. Among several studies investigating a possible relation between bromocriptine exposure and cardiac valvulopathy, some events of cardiac valvulopathy have been reported, but no definitive association between bromocriptine mesylate use and clinically significant (moderate to severe) cardiac valvulopathy could be concluded.
Psychotic and Psychiatric Disorders
Psychotic disorders and impulse control/compulsive behaviors (including pathological gambling) have been reported with bromocriptine.
Adverse Reactions in Postpartum Patients
Serious and life-threatening adverse reactions including hypertension, myocardial infarction, seizures, stroke and psychosis have been reported in postpartum women who were administered bromocriptine for inhibition of lactation.
Neuroleptic-Like Malignant Syndrome
A neuroleptic-like malignant syndrome (manifested by high fever and increase in creatinine phosphokinase) has been reported upon cessation of bromocriptine treatment in patients with advanced Parkinson's disease or patients with secondary Parkinsonism.
7 Drug Interactions
- The active ingredient in CYCLOSET (bromocriptine mesylate) is highly bound to serum proteins. Therefore, CYCLOSET may increase the unbound fraction of other concomitantly used highly protein-bound therapies (e.g., salicylates, sulfonamides, chloramphenicol and probenecid), which may alter their effectiveness and risk for side effects.
- CYCLOSET is a dopamine receptor agonist. Concomitant use of dopamine receptor antagonists, such as neuroleptics (e.g., phenothiazines, butyrophenones, thioxanthenes), or metoclopramide may diminish the effectiveness of CYCLOSET, and CYCLOSET may diminish the effectiveness of these other therapies. The concurrent use of CYCLOSET with these agents has not been studied in clinical trials and is not recommended [see Warnings and Precautions (5.5)].
- CYCLOSET in combination with ergot-related drugs may cause an increase in the occurrence of ergot-related side effects, such as nausea, vomiting, and fatigue, and may also reduce the effectiveness of these ergot therapies when used to treat migraine. The concurrent use of these ergot agents within 6 hours of CYCLOSET dosing is not recommended.
- CYCLOSET is extensively metabolized by the liver via CYP3A4. Therefore, potent inhibitors or inducers of CYP3A4 may increase or reduce the circulating levels of CYCLOSET, respectively. Use caution when co-administering drugs that are inhibitors or inducers of CYP3A4. CYCLOSET dose should not exceed 1.6 mg once daily during concomitant use of a moderate CYP3A4 inhibitor (e.g., erythromycin). Concomitant use of strong CYP3A4 inhibitors (e.g., azole antimycotics, HIV protease inhibitors) with CYCLOSET should be avoided. Ensure adequate washout of the strong CYP3A4 inhibitor drug before initiating CYCLOSET treatment [see Clinical Pharmacology (12.3)].
- There are postmarketing reports of hypertension and tachycardia when bromocriptine was co-administered with sympathomimetic drugs (e.g., phenylpropanolamine and isometheptene) in postpartum women. There are limited clinical trial data supporting the safety of co-administering sympathomimetic drugs and CYCLOSET for more than 10 days. Therefore, concomitant use of these agents with CYCLOSET for more than 10 days duration is not recommended. Also, there are limited clinical trial data supporting the safety of selective 5-hydroxytryptamine1B (5-HT1B) agonists (e.g., sumatriptan) used concurrently with CYCLOSET, and the concomitant use of these agents with CYCLOSET should be avoided.
- May increase the unbound fraction of highly protein-bound therapies, altering their effectiveness and safety profiles. (
7 )- May increase ergot-related side effects or reduce ergot effectiveness for migraines if co-administered within 6 hours of ergot-related drugs. (
7 )- Extensively metabolized by CYP3A4. Limit CYCLOSET dose to 1.6 mg/day during concomitant use of moderate CYP3A4 inhibitors. Avoid concomitant use of CYCLOSET with strong CYP3A4 inhibitors. (
2.3 ,7 )
8 Use In Specific Populations
Pediatrics: Safety and effectiveness have not been established. (8.4 )
8.1 Pregnancy
Risk Summary
There are no available data on CYCLOSET use in pregnant women with type 2 diabetes. However, prolonged experience with bromocriptine use in pregnant women for other indications over several decades, based on data from published clinical trials, case reports, and epidemiological studies, have not established a drug-associated risk for major birth defects, miscarriage, or adverse maternal or fetal outcomes. Furthermore, only a trace amount of bromocriptine was shown to be transported across the placenta in vitro in a published ex vivo human placental perfusion model. There are risks to the mother and fetus associated with poorly controlled diabetes in pregnancy (see Clinical Considerations). In animal reproduction studies in which bromocriptine mesylate was administered orally during the period of organogenesis, increased prenatal mortality occurred in rats and rabbits at maternally toxic dosages that were more than 24-times the human dose of 4.8 mg/day based on body surface area. No adverse developmental outcomes were observed in monkeys administered bromocriptine mesylate orally during various periods of gestation at doses up to 10-times a human dose of 4.8 mg daily (see Data).
The estimated background risk of major birth defects is 6-10% in women with pre-gestational diabetes with an HbA1c >7 and has been reported to be as high as 20-25% in women with an HbA1c >10. The estimated background risk of miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Poorly controlled diabetes in pregnancy increases the maternal risk for diabetic ketoacidosis, pre-eclampsia, spontaneous abortions, preterm delivery, and delivery complications. Poorly controlled diabetes increases the fetal risk for major birth defects, stillbirth, and macrosomia related morbidity.
Data
Human Data
While available studies cannot definitively establish the absence of risk, data from published studies have not established an association with bromocriptine use during pregnancy and major birth defects, miscarriage, or adverse maternal or fetal outcomes. Available epidemiological studies have methodological limitations including small sample size and inconsistent comparator groups.
Animal Data
Two strains of pregnant rats were dosed orally with 3, 10, and 30 mg/kg/day from Gestation Day (GD) 6-15 and with a single dose of 10 mg/kg on GD 5. Implantation was inhibited at 10 and 30 mg/kg (24 and 72 times the human 4.8 mg daily dose, based on mg/m2 comparison). When rats were dosed with 3, 10, and 30 mg/kg/day from GD 8-15 there was an increase in resorptions at ‚Č•10 mg/kg. These effects were probably due to the dependence of implantation and maintenance of gestation upon prolactin in the rat and are not clinically relevant as these events in humans are dependent upon luteinizing hormone. There were no drug-related malformations in the rat.
In two strains of pregnant rabbits treated from GD 6-18 with oral doses of 3, 10, 30, 100, and 300 mg/kg/day, there was maternal toxicity and embryolethality (post-implantation loss/early resorptions) at doses ‚Č•10 mg/kg/day (‚Č•48 times the human 4.8 mg daily dose, based on mg/m2 comparison) and a low incidences of fetal abnormalities at maternally toxic doses ‚Č• 100 mg/kg/day (‚Č•480 times the human 4.8 mg daily dose, based on mg/m2 comparison). There were no treatment-related fetal malformations at doses ‚ȧ30 mg/kg/day (140 times the human 4.8 mg daily dose, based on mg/m2 comparison). Implantation was not affected in rabbits treated from GD 1-6 with oral doses of 100-300 mg/kg/day (480-1400 times the human 4.8 mg daily dose, based on mg/m2 comparison).
In a small study in macaque monkeys given oral doses of 2 mg/kg/day (10 times the human 4.8 mg daily dose, based on mg/m2 comparison) during organogenesis, no embryotoxic or teratologic effects were observed.
In developmental toxicity studies in monkeys, an oral dose of 0.3 mg/kg administered prior to pregnancy and through GD 30 or 80, or an oral dose of 2 mg/kg administered from GD 20-24, resulted in no embryotoxicity (doses up to 10 times the human 4.8 mg daily dose based on mg/m2 comparison).
8.2 Lactation
Risk Summary
CYCLOSET is contraindicated in lactating patients because its active ingredient, bromocriptine, inhibits lactation. In addition, serious and life-threatening adverse reactions including hypertension, myocardial infarction, seizures, stroke, and psychosis have been reported postmarketing in postpartum women who were administered bromocriptine for inhibition of lactation. The indication for use of bromocriptine for inhibition of lactation was withdrawn from bromocriptine-containing products and is not approved for CYCLOSET [see Warnings and Precautions (5.7), Adverse Reactions (6.2)].
8.4 Pediatric Use
The safety and effectiveness of CYCLOSET in pediatric patients have not been established.
8.5 Geriatric Use
In the two clinical trials of CYCLOSET add-on to sulfonylurea therapy and in the monotherapy trial, a total of 54 patients randomized to CYCLOSET were ‚Č•65 years old. In the 52-week safety trial, 601 of the 2,054 CYCLOSET-treated patients (29%) were ‚Č•65 years old. No overall differences in safety or effectiveness were observed between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out [See Clinical Studies (14)].
10 Overdosage
With another formulation of bromocriptine mesylate, the most commonly reported signs and symptoms associated with acute overdose were nausea, vomiting, constipation, diaphoresis, dizziness, pallor, severe hypotension, malaise, confusion, lethargy, drowsiness, delusions, hallucinations, and repetitive yawning. The lethal dose has not been established.
Treatment of overdose consists of removal of the drug by emesis (if conscious), gastric lavage, activated charcoal, or saline catharsis. Careful supervision and recording of fluid intake and output is essential. Hypotension should be treated by placing the patient in the Trendelenburg position and administering intravenous fluids. If satisfactory relief of hypotension cannot be achieved by using the above measures to their fullest extent, vasopressors should be considered.
11 Description
CYCLOSET Tablets contain micronized bromocriptine mesylate, an ergot derivative. Bromocriptine mesylate is chemically designated [Ergotaman-3',6',18-trione, 2-bromo-12'-hydroxy-2'-(1-methylethyl)-5'-(2-methylpropyl)-, monomethanesulfonate (salt), (5'őĪ)-]. CYCLOSET is a single enantiomer with absolute configuration 5R, 8R, 2'R, 5'S, 11'S, 12'S.
The structural formula of bromocriptine is shown below:

Bromocriptine mesylate in CYCLOSET is a white or slightly colored micronized crystalline powder with a molecular formula of C32H40BrN5O5‚ąôCH4SO3 and a molecular weight of 750.72. CYCLOSET Tablets contain bromocriptine mesylate USP in an amount equivalent to 0.8 mg. of bromocriptine. Each tablet contains the following inactive ingredients: lactose, corn starch, magnesium stearate, colloidal silicon dioxide, and citric acid.
12 Clinical Pharmacology
12.1 Mechanism of Action
CYCLOSET contains bromocriptine mesylate, a sympatholytic, dopamine D2 receptor agonist. In patients with type 2 diabetes, timed morning administration of CYCLOSET is associated with increased insulin sensitivity and glucose disposal and reduced fasting and postprandial hyperglycemia throughout the meals of the day without raising plasma insulin levels.
12.2 Pharmacodynamics
Postprandial Glucose and Insulin Response to a Meal
Patients with type 2 diabetes and inadequate glycemic control on diet alone were randomized to CYCLOSET or placebo in a 24-week monotherapy clinical trial. At baseline and study end, plasma samples for insulin and glucose were obtained before and 1 hour, and 2 hours after standardized meals for breakfast, lunch, and dinner. In this trial, once-daily (8 a.m.) CYCLOSET improved postprandial glucose without increasing plasma insulin concentrations.
Insulin-Mediated Glucose Disposal
Patients with type 2 diabetes and inadequate glycemic control on sulfonylurea therapy were randomized to CYCLOSET or placebo in a 16-week clinical trial. In this trial CYCLOSET therapy improved insulin-mediated glucose disposal and glucose tolerance and resulted in lower plasma glucose and HbA1c levels.
12.3 Pharmacokinetics
Absorption and Bioavailability
When administered orally, approximately 65-95% of the CYCLOSET dose of bromocriptine mesylate is absorbed. Due to extensive first-pass metabolism, approximately 7% of the dose reaches the systemic circulation. Under fasting conditions the time to maximum plasma concentration is 53 minutes. In contrast, following a standard high-fat meal, the time to maximum plasma concentration is increased to approximately 90-120 minutes. Also, the relative bioavailability of CYCLOSET is increased under fed as compared to fasting conditions by an average of approximately 55-65% (increase in AUCinf).
Distribution
Bromocriptine is 90-96% bound to plasma proteins. The volume of distribution is approximately 61 L.
Metabolism
Bromocriptine mesylate is extensively metabolized in the gastrointestinal tract and liver. Metabolism by CYP3A4 is the major metabolic pathway. Most of the absorbed dose (approximately 93%) undergoes first-pass metabolism. The remaining 7% reaches the systemic circulation.
Excretion
The major route of excretion of bromocriptine is in the bile with the remaining approximately 2-6% of an oral dose excreted via the urine. The elimination half-life is approximately 6 hours. Prior consumption of a standard high-fat meal has little to no effect on the elimination half-life of CYCLOSET.
Specific Populations
Renal Impairment
No pharmacokinetic studies have been conducted in patients with renal impairment. Although the kidney is a minor pathway for elimination of CYCLOSET, caution should be used in patients with renal impairment.
Hepatic Impairment
No pharmacokinetic studies have been conducted in patients with hepatic impairment. Because CYCLOSET is predominantly metabolized by the liver, caution should be used in patients with hepatic impairment.
Gender
The plasma exposure of CYCLOSET is increased 18-30% in females compared to males.
Geriatric
No pharmacokinetic studies have been conducted in geriatric subjects.
Pediatric
Studies characterizing the pharmacokinetics of CYCLOSET in pediatric patients have not been performed.
Race
Studies characterizing the pharmacokinetics of CYCLOSET among different ethnic groups have not been performed.
Drug Interactions
In Vitro Assessment
Although bromocriptine is a competitive inhibitor of CYP3A4, in vivo drug interaction potential is low because the inhibitory potency for CYP3A4 is approximately 10,000-fold higher than the maximum plasma levels reached in vivo (Cmax of approximately 80-125 pg/mL) following a 4.8 mg oral dose of CYCLOSET.
Agents inducing CYP3A4 activity such as rifampin or dexamethasone would be expected to decrease CYCLOSET plasma levels. There was no significant in vitro inhibition of other major CYP450 enzymes (1A2, 2C9/19, 2D6) by bromocriptine.
In Vivo Assessment
The concomitant use of macrolide antibiotics such as erythromycin (250 mg four times a day), a known inhibitor of CYP3A4, along with bromocriptine (5 mg) was shown to increase the AUC (2.8-fold) and Cmax (4.6-fold) of bromocriptine [see Dosage and Administration (2.3), Drug Interactions (7)].
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a 74-week dietary study in mice at doses up to 50 mg/kg/day (60 times the human 4.8 mg daily dose, based on mg/m2 comparison), there was no evidence of tumorigenicity.
In a 100-week dietary carcinogenicity study in rats at doses of 1.8, 9.9 and 44.5 mg/kg/day (up to 107 times the human 4.8 mg daily dose, based on mg/m2 comparison), there was a significant increase in the incidence of malignant uterine neoplasms at ‚Č•9.9 mg/kg/day (‚Č•24-times the human 4.8 mg daily dose, based on mg/m2 comparison). The increase in uterine neoplasms was probably due to the inhibition of prolactin-stimulated progesterone secretion resulting in estrogen domination and endometrial stimulation in the aging rat. Because prolactin does not play a role in human progesterone production, this finding is unlikely to be clinically relevant.
Mutagenicity
Bromocriptine was not mutagenic in the in vitro Ames bacterial mutation assay, the V79 Chinese hamster fibroblast mutagenicity test, the in vivo bone marrow micronucleus test in mice and the in vivo Chinese hamster bone marrow chromosomal aberration test.
Impairment of Fertility
There was no effect on fertility in female rats treated with oral doses of 1 and 3 mg/kg (2 to 7 times the human 4.8 mg daily dose, based on mg/m2 comparison) from two weeks prior to mating through two weeks post mating or throughout lactation. Postnatal pup weight gain was reduced dose-dependently in treated groups, probably due to lactation inhibition.
In male rats administered oral doses of 2, 10, and 50 mg/kg/day (up to 120 times the human 4.8 mg daily dose, based on mg/m2 comparison) that were mated with untreated females, there was no effect on mating or fertility. However, there was a slight increase in postnatal (post-partum days 0-21) pup mortality in the 10 and 50 mg/kg/day groups (24-120 times the human 4.8 mg daily dose, based on mg/m2 comparison).
14 Clinical Studies
A total of 3,723 patients with type 2 diabetes were randomized across 4 double-blind, placebo-controlled clinical trials conducted to evaluate the safety and glycemic efficacy of CYCLOSET. In the pooled 24-week monotherapy trial and the two 24-week add-on to sulfonylurea trials (N = 653), the mean age of the CYCLOSET-treated patients (N = 324) was 55 years, 71% were male and 73% Caucasian. In the 52-week safety trial (N = 3,070), the mean age for the entire study population was 60 years and 43% of patients were female, 68% were Caucasian, 17% were Black, 13% were Hispanic, and 1% were Asian.
In all 4 clinical trials, patients assigned to treatment with CYCLOSET received an initial dose of 0.8 mg, which was increased by 0.8 mg each week for 6 weeks (4.8 mg/day final dose) if no intolerance occurred or until the maximum tolerated dose ‚Č•1.6 mg/day was reached. In patients with type 2 diabetes, treatment with CYCLOSET produced clinically significant improvements in HbA1c and postprandial glucose (PPG).
14.1 Monotherapy
A total of 159 adults with type 2 diabetes, overweight (body mass index ‚Č•26.0 kg/m2 for males and ‚Č•28.0 kg/m2 for females), and inadequate glycemic control (HbA1c 7.5-11%) participated in a 24-week, placebo-controlled, monotherapy trial that evaluated the efficacy and safety of CYCLOSET as an adjunct to diet and exercise. Mean body weight at baseline was 93 kg in the CYCLOSET group and 96 kg in the placebo group. Mean HbA1c at baseline was 9.0% in the CYCLOSET group and 8.8% in the placebo group. Mean duration of diabetes at baseline was 5 years in the CYCLOSET group and 4 years in the placebo group. Of the 80 patients in the CYCLOSET group, 69% (N = 55) achieved the maximum daily dose of 4.8 mg. CYCLOSET improved HbA1c and fasting plasma glucose compared to placebo (Table 2). Mean change from baseline in body weight was +0.2 kg in the CYCLOSET group (N = 78) and +0.5 kg in the placebo group (N = 77).
Table 2: Changes in Glycemic Parameters in a 24-Week Placebo-Controlled Study of CYCLOSET as Monotherapy in Patients with Type 2 Diabetes intent-to-treat population with last observation carried forward CYCLOSET N = 80 (1.6 - 4.8 mg) Placebo N = 79 P-value calculated by ANOVA; HbA1c (%) N = 74 N = 74   Baseline (mean) 9.0 8.8   Change from baseline (adj. mean) -0.1 0.3   Difference from placebo (adj. mean) -0.4 p = 0.05, Fasting Plasma Glucose (mg/dL) N = 76 N = 75   Baseline (mean) 215 205   Change from baseline (adj. mean) 0 23   Difference from placebo (adj. mean) -23 p = 0.005 14.2 Combination Therapy
CYCLOSET Add-on to Sulfonylurea Therapy
Patients with type 2 diabetes and inadequate glycemic control (HbA1c 7.8-12.5%) on sulfonylurea therapy (mean HbA1c 9.4%) participated in Study L, a 24-week, randomized, double-blind, placebo-controlled trial that evaluated the safety and glycemic efficacy of CYCLOSET when added to stable sulfonylurea therapy. The mean duration of diabetes was 6 years in the CYCLOSET group and 8 years in the placebo group. The range of body mass index was 26-40 kg/m2 for men and 28-40 kg/m2 for women, with a mean of 32 kg/m2 in both treatment groups. Of the 122 patients in the CYCLOSET group, 83 (68%) achieved the maximum dose of study drug. The mean change from baseline in body weight was +0.9 kg in the CYCLOSET group and +0.5 kg in the placebo group.
In another similarly designed trial, Study K, patients with type 2 diabetes and inadequate glycemic control (HbA1c 7.8-12.5 %) on stable sulfonylurea therapy were randomized to add-on therapy with either CYCLOSET (N = 122) or placebo (N = 123). The range of body mass index was 26-40 kg/m2 for men and 28-40 kg/m2 for women, with a mean of 32 kg/m2 in the CYCLOSET group and 33 kg/m2 in the placebo group. Of the 122 patients in the CYCLOSET group, 91 (75%) achieved the maximum dose of study drug. Mean change from baseline in body weight was +1.4 kg in the CYCLOSET group and +0.5 kg in the placebo group. CYCLOSET improved HbA1c and fasting blood glucose concentrations compared to placebo (Table 3).
Table 3: Changes in Glycemic Parameters for CYCLOSET Versus Placebo in Two Add-on to Sulfonylurea Trials Study K intent-to-treat population using last observation carried forward between-group change from baseline in HbA1c Study L CYCLOSET Add-on to Sulfonylurea N = 122 Placebo Add-on to Sulfonylurea N = 123 CYCLOSET Add-on to Sulfonylurea N = 122 Placebo Add-on to Sulfonylurea N = 127 P-value calculated by ANOVA; HbA1c (%) n = 114 n = 122 n = 114 n = 123 ¬†¬†Baseline (mean) 9.3 9.4 9.3 9.4 ¬†¬†Change from baseline (adj. mean) -0.1 0.4 -0.4 0.3 ¬†¬†Difference from placebo (adj. mean) -0.5 p‚ȧ 0.001, -0.6 Fasting Plasma Glucose (mg/dL) n = 116 n = 119 n = 113 n = 123 ¬†¬†Baseline (mean) 216 227 220 226 ¬†¬†Change from baseline (adj. mean) 10 28 3 23 ¬†¬†Difference from placebo (adj. mean) -18 p = 0.02; -20 p = 0.006
CYCLOSET Add-on to Various Oral Antidiabetic Agents
Patients with type 2 diabetes receiving various antidiabetic therapies (mean baseline HbA1c 8.3%) participated in a 52-week randomized, double-blind, placebo-controlled safety trial [see Adverse Reactions (6.1)]. The daily CYCLOSET dose was initiated at 0.8 mg and increased by 0.8 mg each week for 6 weeks if no intolerance occurred or until the maximum tolerated dose ‚Č•1.6 mg/day was reached. Approximately 70% of patients assigned to treatment with CYCLOSET reached the maximum daily dose of 4.8 mg. Physicians were instructed to adjust the dosage of concomitant diabetes therapies to avert hypoglycemia or uncontrolled hyperglycemia. Doses of background antidiabetic medications could be adjusted at any time during the trial and additional antidiabetic medications were permitted after week 12, if needed to maintain ideal glycemic control. Mean baseline HbA1c was 7.0% in both treatment groups. The least-squares mean change in HbA1c from baseline to week 24 was 0.0% with CYCLOSET (N = 2049) and +0.2% with placebo (N = 1015). Because many patients (60%) were already at treatment goal at baseline (HbA1c <7%), pre-specified subgroup analyses of glycemic efficacy (change in HbA1c from baseline to week 24) were conducted for patients who had inadequate glycemic control (baseline HbA1c ‚Č•7.5%) on 1-2 oral antidiabetic therapies at the time of study entry. Patients receiving CYCLOSET, compared to placebo, experienced a significant improvement in HbA1c when used as adjunctive therapy to 1-2 oral antidiabetic medications, including the subgroup of patients treated only with background metformin + sulfonylurea (Table 4). The mean change in body weight for the glycemic efficacy subgroup (N = 559) from baseline to week 24 was -0.1 kg with CYCLOSET and +0.1 kg. The mean change in body weight for the entire study population (N = 3070) from baseline to week 52 was +0.2 kg with CYCLOSET and +0.1 kg with placebo.
Table 4: Changes in HbA1c from Baseline to Week 24 in the CYCLOSET Safety Trial Subgroup of Patients with Type 2 Diabetes and Inadequate Glycemic Control (Baseline HbA1c ‚Č•7.5%) on 1-2 Oral Antidiabetic Medications intent-to-treat population using last observation carried forward between-group change from baseline in HbA1c 24-Week Intent-to-Treat CYCLOSET Placebo P-value is based on an ANCOVA model with treatment and center as fixed effects, and baseline HbA1c as covariates; Adjunct to 1-2 Oral Antidiabetic Medications N = 376 N = 183 HbA1c (%) ¬†¬†Baseline mean 8.3 8.4 ¬†¬†Change from baseline (adjusted mean) -0.4 0.0 ¬†¬†Difference from placebo (adjusted mean) -0.5 p<0.001 % Patients achieving HbA1c of ‚ȧ7.0 25 9 Adjunct to Metformin + Sulfonylurea Only patients in the "metformin + sulfonylurea only" subgroup are also counted in the "adjunct to 1-2 oral antidiabetic medications" subgroup N = 177 N = 90 HbA1c (%) ¬†¬†Baseline mean 8.3 8.3 ¬†¬†Change from baseline (adjusted mean) -0.5 0.0 ¬†¬†Difference from placebo (adjusted mean) -0.5 % Patients achieving HbA1c of ‚ȧ7.0 27 9 14.3 Changes in Lipids and Blood Pressure
CYCLOSET does not have an unfavorable effect on fasting plasma lipids.
CYCLOSET has not demonstrated an unfavorable hypertensive effect on blood pressure. Hypotension has been reported with use of CYCLOSET in clinical trials [see Warnings and Precautions (5.1)].
16 How Supplied/storage And Handling
CYCLOSET 0.8 mg tablets are WHITE and round with "C" on one side and "9"on the other.
The tablets are supplied as follows: NDC 68012-258-20 unit-of-use bottles of 200 NDC 68012-258-21 unit-of-use bottles of 21 (samples only).
STORAGE AND HANDLING SECTION
Storage
Store and dispense: At 20-25¬įC (68-77¬įF) in a tight, light-resistant container. See USP Controlled Room Temperature.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Hypotension
Advise patients that they may develop postural (orthostatic) hypotension with or without symptoms such as dizziness, nausea, and diaphoresis. Hypotension and syncope may occur more frequently during initial therapy or with an increase in dose at any time. During early treatment with CYCLOSET, advise patients to make slow postural changes and to avoid situations that could predispose to serious injury if syncope was to occur [see Warnings and Precautions (5.1)].
Impulse Control/Compulsive Behaviors
Advise patients that they may experience impulse control and/or compulsive behaviors while taking CYCLOSET and to inform their physician or healthcare provider if they develop new or increased gambling urges, sexual urges, uncontrolled spending, binge or compulsive eating, or other urges while being treated with CYCLOSET [see Warnings and Precautions (5.3)].
Somnolence
Advise patients that CYCLOSET may cause somnolence. Advise patients not to operate heavy machinery if symptoms of somnolence occur [see Warnings and Precautions (5.4)].
Pregnancy and Lactation
Advise patients not to take CYCLOSET postpartum or while lactating [see Warnings and Precautions (5.7), Use in Specific Populations (8.2)]. Serious and life-threatening adverse reactions including hypertension, myocardial infarction, seizures, stroke and psychosis have been reported in postpartum women who were administered bromocriptine for inhibition of lactation.
Missed Doses
Advise patients to take CYCLOSET within 2 hours after waking in the morning. If the morning dose is missed, instruct patients to take their usual dose the following morning. Doses of CYCLOSET should not be doubled the following morning.
Manufactured for: VeroScience, LLC Tiverton, RI 02878 USA
Distributed by: Salix Pharmaceuticals, a division of Bausch Health US, LLC Bridgewater, NJ 08807 USA
Printed in USA
For information for healthcare professionals, call 1-800-321-4576.
For patent information: http://veroscience.com/products/patents.html
Cycloset is a registered trademark of VeroScience LLC, Tiverton, RI 02878 USA used under license.
9625403 70014086
Spl Patient Package Insert Section
Patient Information CYCLOSET¬ģ (Sikloset) (bromocriptine mesylate tablets) for oral use This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 08/2020¬†¬†¬†¬† Read this Patient Information that comes with CYCLOSET before you start taking it and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or treatment. What is CYCLOSET?
- CYCLOSET is a prescription medicine used with diet and exercise to lower blood sugar in adults with type 2 diabetes.
- CYCLOSET is not for people with type 1 diabetes.
- CYCLOSET is not for people with diabetic ketoacidosis.
- It is not known if CYCLOSET is safe and effective in children.
Who should not take CYCLOSET? Do not take CYCLOSET if you:
- are allergic to bromocriptine or any of the ingredients in CYCLOSET. See the end of this Patient Information leaflet for a complete ul of ingredients in CYCLOSET.
- are allergic to ergot medicines. Ask your healthcare provider for a ul of these medicines, if you are not sure.
- have fainting (syncopal) migraine headaches.
- are a woman who has recently given birth to a child (postpartum). CYCLOSET can cause serious and life-threatening problems including high blood pressure (hypertension), heart attack, seizures, stroke and psychosis (losing touch with reality).
- are breastfeeding.
Talk to your healthcare provider before taking CYCLOSET if you have any of these conditions. What should I tell my healthcare provider before taking CYCLOSET? Before taking CYCLOSET, tell your healthcare provider about all of your medical conditions, including if you:
- have ever passed out (fainted).
- have migraine headaches.
- have or have had low blood pressure (hypotension).
- take medicines for high blood pressure (hypertension).
- have or have had a mental health problem, especially a psychotic disorder.
- are pregnant or plan to become pregnant. It is not known if CYCLOSET will harm your unborn baby. If you are pregnant, talk with your healthcare provider about the best way to control your blood sugar while you are pregnant.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take:
- medicines for mental health problems, especially anti-psychotic medicines called dopamine receptor antagonists
- medicines for migraine or other types of headaches
- other medicines that work like CYCLOSET (dopamine receptor agonists) to treat conditions such as Parkinson's disease, high levels of a hormone called prolactin in your blood (hyperprolactinemia), restless leg syndrome and too much growth hormone (acromegaly)
- medicines for type 2 diabetes
Ask your healthcare provider or pharmacist for a ul of these medicines if you are not sure. CYCLOSET may affect the way other medicines work, and other medicines may affect how CYCLOSET works. Know the medicines you take. Keep a ul of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine. How should I take CYCLOSET?
- Take CYCLOSET exactly as your healthcare provider tells you to take it.
- Take CYCLOSET by mouth each morning with food.
- Take CYCLOSET within 2 hours after waking in the morning.
- If you miss your morning dose, wait until the next morning to take your medication. Do not take a double dose of CYCLOSET.
- During periods of stress on the body, such as fever, trauma, infection, or surgery, your medication needs may change. Contact your healthcare provider right away as your medication needs change.
- If you take too much CYCLOSET, call your healthcare provider or go to the nearest emergency department right away.
- While taking CYCLOSET:
- check your blood sugar as your healthcare provider tells you to
- stay on your prescribed diet and exercise program
- talk to your doctor about how to prevent, recognize, and manage low blood sugar (hypoglycemia), high blood sugar (hyperglycemia), and complications of diabetes
- see your healthcare provider for regular blood tests, including your blood sugar levels and hemoglobin A1C
What are the possible side effects of CYCLOSET? CYCLOSET may cause serious side effects, including:
- Low blood pressure (hypotension) including low blood pressure when you suddenly change positions (orthostatic hypotension). This can happen more often when first starting CYCLOSET or if your dose is increased. Symptoms of low blood pressure when you suddenly change positions can include dizziness, nausea, sweating, fainting or light-headedness. Stand up slowly when moving from a sitting or lying position. You should avoid activities that could cause injury if you feel light-headed or faint.
- Feeling tired and sleepy (somnolence). Tiredness and sleepiness can happen with CYCLOSET, especially when first starting CYCLOSET. Tiredness and sleepiness are common but can also be serious. If you feel tired and sleepy while taking CYCLOSET, you should not drive or operate heavy machinery.
- Uncontrollable (compulsive) behaviors. CYCLOSET is in a class of medicines that may cause some people to get urges to behave in a way that may be unusual for them. Examples of these behaviors include strong urges to gamble, increased sexual urges, strong urges to spend money, binge eating or eating that you cannot control. If you or your family members notice that you are developing any unusual behaviors, talk to your healthcare provider. These behaviors may go away if your dose of CYCLOSET is lowered or stopped.
- Serious and life-threatening problems in women who have recently given birth to a child (postpartum). See " Who should not take CYCLOSET? "
The most common side effects of CYCLOSET include:
- nausea
- headache
- dizziness
- vomiting
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of CYCLOSET. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store CYCLOSET?
- Store CYCLOSET at room temperature between 68¬įF and 77¬įF (20¬įC and 25¬įC).
- Store CYCLOSET in a tight, light resistant container.
Keep CYCLOSET and all medicines out of the reach of children. General information about the safe and effective use of CYCLOSET. Medicines are sometimes prescribed for purposes other than those uled in a Patient Information leaflet. Do not use CYCLOSET for a condition for which it was not prescribed. Do not give CYCLOSET to other people, even if they have the same symptoms that you have. It may harm them. This leaflet summarizes the most important information about CYCLOSET. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about CYCLOSET that is written for health professionals. What are the ingredients in CYCLOSET? Active ingredient: bromocriptine mesylate Inactive ingredients: lactose, corn starch, magnesium stearate, colloidal silicon dioxide, and citric acid Manufactured for: VeroScience, LLC Tiverton, RI 02878 Distributed by: Salix Pharmaceuticals, a division of Bausch Health US, LLC Bridgewater, NJ 08807 USA For information for healthcare professionals, call 1-800-321-4576. CYCLOSET is a registered trademark of: VeroScience, LLC Tiverton, RI 02878 For more information, go to www.CYCLOSET.com or call 1-800-321-4576.
Principal Display Panel - 0.8 Mg Tablet Bottle Label
NDC 68012-258-21
CYCLOSET¬ģ bromocriptine mesylate tablets
0.8 mg
21 TabletsRx only
Professional Samples ‚ÄďNot For Sale

DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site