Bupropion Hydrochloride (bupropion hydrochloride 150 mg) Dailymed
Generic: bupropion hydrochloride
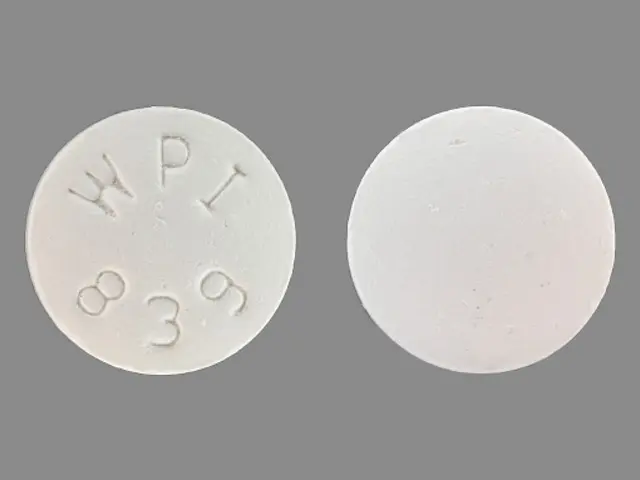
IMPRINT: WPI 839
SHAPE: round
COLOR: white
All Imprints
bupropion hydrochloride 150 mg - wpi 839 round white
12 hr bupropion hydrochloride 150 mg extended release oral tablet - wpi 839 round white
bupropion hydrochloride - 12 hr bupropion hydrochloride 150 mg extended release oral tablet - wpi 839 round white
bupropion hydrochloride 200 mg - wpi 3385 round white
bupropion hydrochloride 100 mg - wpi 858 round white
Boxed Warning
Boxed Warning
Go PRO for all pill images
Boxed Warning
Suicidality and Antidepressant Drugs Use in Treating Psychiatric Disorders:
WARNINGS: Clinical Worsening and Suicide Risk in Treating Psychiatric Disorders
PRECAUTIONS: Information for Patients
, and
PRECAUTIONS: Pediatric Use
).
Use in Smoking Cessation Treatment:
Wellbutrinbupropion hydrochloride extended-release tablets (SR), and Wellbutrin XLare not approved for smoking cessation treatment, but bupropion under the name Zybanis approved for this use. Serious neuropsychiatric events, including but not limited to depression, suicidal ideation, suicide attempt, and completed suicide have been reported in patients taking bupropion for smoking cessation. Some cases may have been complicated by the symptoms of nicotine withdrawal in patients who stopped smoking. Depressed mood may be a symptom of nicotine withdrawal. Depression, rarely including suicidal ideation, has been reported in smokers undergoing a smoking cessation attempt without medication. However, some of these symptoms have occurred in patients taking bupropion who continued to smoke. All patients being treated with bupropion for smoking cessation treatment should be observed for neuropsychiatric symptoms including changes in behavior, hostility, agitation, depressed mood, and suicide-related events, including ideation, behavior, and attempted suicide. These symptoms, as well as worsening of pre-existing psychiatric illness and completed suicide have been reported in some patients attempting to quit smoking while taking Zybanin the postmarketing experience. When symptoms were reported, most were during treatment with Zybanbut some were following discontinuation of treatment with Zyban
Advise patients and caregivers that the patient using bupropion for smoking cessation should stop taking bupropion and contact a healthcare provider immediately if agitation, hostility, depressed mood, or changes in thinking or behavior that are not typical for the patient are observed, or if the patient develops suicidal ideation or suicidal behavior.
In many postmarketing cases, resolution of symptoms after discontinuation of Zyban The risks of using bupropion for smoking cessation should be weighed against the benefits of its use. Zybanhas been demonstrated to increase the likelihood of abstinence from smoking for as long as 6 months compared to treatment with placebo. The health benefits of quitting smoking are immediate and substantial. (See WARNINGS: Neuropsychiatric Symptoms and Suicide Risk in Smoking Cessation Treatment and PRECAUTIONS: Information for Patients.)
Description
dimethylethyl)amino]-1 -propanone hydrochloride. The molecular weight is 276.2. The molecular formula is C13H18ClNOHCl. Bupropion hydrochloride powder is white, crystalline, and highly soluble in water. It has a bitter taste and produces the sensation of local anesthesia on the oral mucosa. The structural formula is:Bupropion hydrochloride extended-release tablets (SR) are supplied for oral administration as 100 mg, 150 mg, and 200 mg white to off-white, film-coated, extended-release tablets. Each tablet contains the labeled amount of bupropion hydrochloride and the following inactive ingredients: hydroxypropyl cellulose, microcrystalline cellulose, colloidal silicon dioxide, stearic acid, magnesium stearate, and diluted hydrochloric acid. The film coating contains lactose monohydrate, hydroxypropyl cellulose, titanium dioxide, and polyethylene glycol.
Clinical Pharmacology
Pharmacodynamics:
Bupropion is a relatively weak inhibitor of the neuronal uptake of norepinephrine and dopamine, and does not inhibit monoamine oxidase or the re-uptake of serotonin. While the mechanism of action of bupropion, as with other antidepressants, is unknown, it is presumed that this action is mediated by noradrenergic and/or dopaminergic mechanisms.
Pharmacokinetics:
Bupropion is a racemic mixture. The pharmacologic activity and pharmacokinetics of the individual enantiomers have not been studied. The mean elimination half-life (of bupropion after chronic dosing is 21 (hours, and steady-state plasma concentrations of bupropion are reached within 8 days. In a study comparing chronic dosing with bupropion hydrochloride extended-release tablets (SR) 150 mg twice daily to the immediate-release formulation of bupropion at 100 mg 3 times daily, peak plasma concentrations of bupropion at steady state for bupropion hydrochloride extended-release tablets (SR) were approximately 85% of those achieved with the immediate-release formulation. There was equivalence for bupropion AUCs, as well as equivalence for both peak plasma concentration and AUCs for all 3 of the detectable bupropion metabolites. Thus, at steady state, bupropion hydrochloride extended-release tablets (SR), given twice daily, and the immediate-release formulation of bupropion, given 3 times daily, are essentially bioequivalent for both bupropion and the 3 quantitatively important metabolites.
Absorption:
Following oral administration of bupropion hydrochloride extended-release tablets (SR) to healthy volunteers, peak plasma concentrations of bupropion are achieved within 3 hours. Food increased Cmax and AUC of bupropion by 11% and 17%, respectively, indicating that there is no clinically significant food effect.
Distribution:
In vitro tests show that bupropion is 84% bound to human plasma proteins at concentrations up to 200 mcg/mL. The extent of protein binding of the hydroxybupropion metabolite is similar to that for bupropion, whereas the extent of protein binding of the threohydrobupropion metabolite is about half that seen with bupropion.
Metabolism:
Bupropion is extensively metabolized in humans. Three metabolites have been shown to be active: hydroxybupropion, which is formed via hydroxylation of the tert-butyl group of bupropion, and the amino-alcohol isomers threohydrobupropion and erythrohydrobupropion, which are formed via reduction of the carbonyl group. In vitro findings suggest that cytochrome P450IIB6 (CYP2B6) is the principal isoenzyme involved in the formation of hydroxybupropion, while cytochrome P450 isoenzymes are not involved in the formation of threohydrobupropion. Oxidation of the bupropion side chain results in the formation of a glycine conjugate of metachlorobenzoic acid, which is then excreted as the major urinary metabolite. The potency and toxicity of the metabolites relative to bupropion have not been fully characterized. However, it has been demonstrated in an antidepressant screening test in mice that hydroxybupropion is one half as potent as bupropion, while threohydrobupropion and erythrohydrobupropion are 5-fold less potent than bupropion. This may be of clinical importance because the plasma concentrations of the metabolites are as high or higher than those of bupropion. Because bupropion is extensively metabolized, there is the potential for drug-drug interactions, particularly with those agents that are metabolized by or which inhibit/induce the cytochrome P450IIB6 (CYP2B6) isoenzyme, such as ritonavir. In a healthy volunteer study, ritonavir at a dose of 100 mg twice daily reduced the AUC and Cmax of bupropion by 22% and 21%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 23%, the threohydrobupropion decreased by 38% and the erythrohydrobupropion decreased by 48%. In a second healthy volunteer study, ritonavir at a dose of 600 mg twice daily decreased the AUC and the Cmax of bupropion by 66% and 62%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 78%, the threohydrobupropion decreased by 50% and the erythrohydrobupropion decreased by 68%. In another healthy volunteer study, KALETRA*(lopinavir 400 mg/ritonavir 100 mg twice daily) decreased bupropion AUC and Cmax by 57%. The AUC and Cmax of hydroxybupropion were decreased by 50% and 31%, respectively, (see PRECAUTIONS: Drug Interactions). Although bupropion is not metabolized by cytochrome P450IID6 (CYP2D6), there is the potential for drug-drug interactions when bupropion is coadministered with drugs metabolized by this isoenzyme (see
PRECAUTIONS: Drug Interactions
). Following a single dose in humans, peak plasma concentrations of hydroxybupropion occur approximately 6 hours after administration of bupropion hydrochloride extended-release tablets (SR). Peak plasma concentrations of hydroxybupropion are approximately 10 times the peak level of the parent drug at steady state. The elimination half-life of hydroxybupropion is approximately 20 (hours, and its AUC at steady state is about 17 times that of bupropion. The times to peak concentrations for the erythrohydrobupropion and threohydrobupropion metabolites are similar to that of the hydroxybupropion metabolite. However, their elimination half-lives are longer, 33 (and 37 (hours, respectively, and steady-state AUCs are 1.5 and 7 times that of bupropion, respectively. Bupropion and its metabolites exhibit linear kinetics following chronic administration of 300 to 450 mg/day.
Elimination:
Following oral administration of 200 mg of 14C-bupropion in humans, 87% and 10% of the radioactive dose were recovered in the urine and feces, respectively. However, the fraction of the oral dose of bupropion excreted unchanged was only 0.5%, a finding consistent with the extensive metabolism of bupropion.
Population Subgroups:
Factors or conditions altering metabolic capacity (e.g., liver disease, congestive heart failure [CHF], age, concomitant medications, etc.) or elimination may be expected to influence the degree and extent of accumulation of the active metabolites of bupropion. The elimination of the major metabolites of bupropion may be affected by reduced renal or hepatic function because they are moderately polar compounds and are likely to undergo further metabolism or conjugation in the liver prior to urinary excretion.
Hepatic:
The effect of hepatic impairment on the pharmacokinetics of bupropion was characterized in 2 single-dose studies, one in patients with alcoholic liver disease and one in patients with mild-to-severe cirrhosis. The first study showed that the half-life of hydroxybupropion was significantly longer in 8 patients with alcoholic liver disease than in 8 healthy volunteers (32hours versus 21hours, respectively). Although not statistically significant, the AUCs for bupropion and hydroxybupropion were more variable and tended to be greater (by 53% to 57%) in patients with alcoholic liver disease. The differences in half-life for bupropion and the other metabolites in the 2 patient groups were minimal. The second study showed no statistically significant differences in the pharmacokinetics of bupropion and its active metabolites in 9 patients with mild-to-moderate hepatic cirrhosis compared to 8 healthy volunteers. However, more variability was observed in some of the pharmacokinetic parameters for bupropion (AUC, Cmax, and Tmax) and its active metabolites (tfor hydroxybupropion and about 2for threo/erythrohydrobupropion. The median Tmax was observed 19 hours later for hydroxybupropion and 31 hours later for threo/erythrohydrobupropion. The mean half-lives for hydroxybupropion and threo/erythrohydrobupropion were increased 5- and 2-fold, respectively, in patients with severe hepatic cirrhosis compared to healthy volunteers (see
WARNINGS
,
PRECAUTIONS
, and
DOSAGE AND ADMINISTRATION
).
Renal:
There is limited information on the pharmacokinetics of bupropion in patients with renal impairment. An inter-study comparison between normal subjects and patients with end-stage renal failure demonstrated that the parent drug Cmax and AUC values were comparable in the 2 groups, whereas the hydroxybupropion and threohydrobupropion metabolites had a 2.3- and 2.8- fold increase, respectively, in AUC for patients with end-stage renal failure. A second study, comparing normal subjects and patients with moderate-to-severe renal impairment (GFR 30.910.8 mL/min) showed that exposure to a single 150 mg dose of sustained-release bupropion was approximately 2-fold higher in patients with impaired renal function while levels of the hydroxybupropion and threo/erythrohydrobupropion (combined) metabolites were similar in the 2 groups. The elimination of bupropion and/or the major metabolites of bupropion may be reduced by impaired renal function (see
PRECAUTIONS: Renal Impairment
).
Left Ventricular Dysfunction:
During a chronic dosing study with bupropion in 14 depressed patients with left ventricular dysfunction (history of CHF or an enlarged heart on x-ray), no apparent effect on the pharmacokinetics of bupropion or its metabolites was revealed, compared to healthy volunteers.
Age:
PRECAUTIONS: Geriatric Use
).
Gender:
A single-dose study involving 12 healthy male and 12 healthy female volunteers revealed no sex-related differences in the pharmacokinetic parameters of bupropion.
Smokers:
CLINICAL TRIALS Although there are not as yet independent trials demonstrating the antidepressant effectiveness of the sustained-release formulation of bupropion, studies have demonstrated the bioequivalence of the immediate-release and sustained-release forms of bupropion under steady-state conditions, i.e., bupropion sustained-release 150 mg twice daily was shown to be bioequivalent to 100 mg 3 times daily of the immediate-release formulation of bupropion, with regard to both rate and extent of absorption, for parent drug and metabolites. In a longer-term study, outpatients meeting DSM-IV criteria for major depressive disorder, recurrent type, who had responded during an 8-week open trial on bupropion (150 mg twice daily of the sustained-release formulation) were randomized to continuation of their same dose of bupropion or placebo, for up to 44 weeks of observation for relapse. Response during the open phase was defined as CGI Improvement score of 1 (very much improved) or 2 (much improved) for each of the final 3 weeks. Relapse during the double-blind phase was defined as the investigator's judgment that drug treatment was needed for worsening depressive symptoms. Patients receiving continued bupropion treatment experienced significantly lower relapse rates over the subsequent 44 weeks compared to those receiving placebo.
Indications & Usage
Bupropion hydrochloride extended-release tablets (SR) are indicated for the treatment of major depressive disorder. The efficacy of bupropion in the treatment of a major depressive episode was established in two 4-week controlled trials of depressed inpatients and in one 6-week controlled trial of depressed outpatients whose diagnoses corresponded most closely to the Major Depression category of the APA Diagnostic and Statistical Manual (DSM) (see
CLINICAL PHARMACOLOGY
). A major depressive episode (DSM-IV) implies the presence of 1) depressed mood or 2) loss of interest or pleasure; in addition, at least 5 of the following symptoms have been present during the same 2-week period and represent a change from previous functioning: depressed mood, markedly diminished interest or pleasure in usual activities, significant change in weight and/or appetite, insomnia or hypersomnia, psychomotor agitation or retardation, increased fatigue, feelings of guilt or worthlessness, slowed thinking or impaired concentration, a suicide attempt or suicidal ideation. The efficacy of bupropion in maintaining an antidepressant response for up to 44 weeks following 8 weeks of acute treatment was demonstrated in a placebo-controlled trial (see
CLINICAL PHARMACOLOGY
). Nevertheless, the physician who elects to use bupropion hydrochloride extended-release tablets (SR) for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
Contraindications
Bupropion hydrochloride extended-release tablets (SR) are contraindicated in patients with a seizure disorder. Bupropion hydrochloride extended-release tablets (SR) are contraindicated in patients treated with Zyban Bupropion hydrochloride extended-release tablets (SR) are contraindicated in patients with a current or prior diagnosis of bulimia or anorexia nervosa because of a higher incidence of seizures noted in patients treated for bulimia with the immediate-release formulation of bupropion. Bupropion hydrochloride extended-release tablets (SR) are contraindicated in patients undergoing abrupt discontinuation of alcohol or sedatives (including benzodiazepines). The concurrent administration of bupropion hydrochloride extended-release tablets (SR) and a monoamine oxidase (MAO) inhibitor is contraindicated. At least 14 days should elapse between discontinuation of an MAO inhibitor and initiation of treatment with bupropion hydrochloride extended-release tablets (SR). Bupropion hydrochloride extended-release tablets (SR) are contraindicated in patients who have shown an allergic response to bupropion or the other ingredients that make up bupropion hydrochloride extended-release tablets (SR).
Warnings
Precautions
General: Agitation and Insomnia: Patients in placebo-controlled trials with bupropion hydrochloride extended-release tablets (SR) experienced agitation, anxiety, and insomnia as shown in Table 2. Table 2. Incidence of Agitation, Anxiety, and Insomnia in Placebo-Controlled Trials Adverse Event TermBupropion Hydrochloride Sustained-Release Formulation 300 mg/day (n=376)Bupropion Hydrochloride Sustained-Release Formulation 400 mg/day (n=114)Placebo (n=385)Agitation Anxiety Insomnia3% 5% 11%9% 6% 16%2% 3% 6%In clinical studies, these symptoms were sometimes of sufficient magnitude to require treatment with sedative/hypnotic drugs. Symptoms were sufficiently severe to require discontinuation of treatment in 1% and 2.6% of patients treated with 300 and 400 mg/day, respectively, of bupropion hydrochloride extended-release tablets (SR) and 0.8% of patients treated with placebo. Psychosis, Confusion, and Other Neuropsychiatric Phenomena: Depressed patients treated with an immediate-release formulation of bupropion or with bupropion hydrochloride extended-release tablets (SR) have been reported to show a variety of neuropsychiatric signs and symptoms, including delusions, hallucinations, psychosis, concentration disturbance, paranoia, and confusion. In some cases, these symptoms abated upon dose reduction and/or withdrawal of treatment. Activation of Psychosis and/or Mania: Antidepressants can precipitate manic episodes in bipolar disorder patients during the depressed phase of their illness and may activate latent psychosis in other susceptible patients. The sustained-release formulation of bupropion is expected to pose similar risks. Altered Appetite and Weight: In placebo-controlled studies, patients experienced weight gain or weight loss as shown in Table 3. Table 3. Incidence of Weight Gain and Weight Loss in Placebo-Controlled Trials Weight ChangeBupropion Hydrochloride Sustained-Release Formulation 300 mg/day (n=339)Bupropion Hydrochloride Sustained-Release Formulation 400 mg/day (n=112)Placebo (n=347)Gained >5 lbs Lost >5 lbs3% 14%2% 19%4% 6%In studies conducted with the immediate-release formulation of bupropion, 35% of patients receiving tricyclic antidepressants gained weight, compared to 9% of patients treated with the immediate-release formulation of bupropion. If weight loss is a major presenting sign of a patient's depressive illness, the anorectic and/or weight-reducing potential of bupropion hydrochloride extended-release tablets (SR) should be considered. Allergic Reactions: Anaphylactoid/anaphylactic reactions characterized by symptoms such as pruritus, urticaria, angioedema, and dyspnea requiring medical treatment have been reported in clinical trials with bupropion. In addition, there have been rare spontaneous postmarketing reports of erythema multiforme, Stevens-Johnson syndrome, and anaphylactic shock associated with bupropion. A patient should stop taking bupropion hydrochloride extended-release tablets (SR) and consult a doctor if experiencing allergic or anaphylactoid/anaphylactic reactions (e.g., skin rash, pruritus, hives, chest pain, edema, and shortness of breath) during treatment. Arthralgia, myalgia, and fever with rash and other symptoms suggestive of delayed hypersensitivity have been reported in association with bupropion. These symptoms may resemble serum sickness.
Cardiovascular Effects: In clinical practice, hypertension, in some cases severe, requiring acute treatment, has been reported in patients receiving bupropion alone and in combination with nicotine replacement therapy. These events have been observed in both patients with and without evidence of preexisting hypertension. Data from a comparative study of the sustained-release formulation of bupropion (ZybanSustained-Release Tablets), nicotine transdermal system (NTS), the combination of sustained-release bupropion plus NTS, and placebo as an aid to smoking cessation suggest a higher incidence of treatment-emergent hypertension in patients treated with the combination of sustained-release bupropion and NTS. In this study, 6.1% of patients treated with the combination of sustained-release bupropion and NTS had treatment-emergent hypertension compared to 2.5%, 1.6%, and 3.1% of patients treated with sustained-release bupropion, NTS, and placebo, respectively. The majority of these patients had evidence of preexisting hypertension. Three patients (1.2%) treated with the combination of Zybanand NTS and 1 patient (0.4%) treated with NTS had study medication discontinued due to hypertension compared to none of the patients treated with Zybanor placebo. Monitoring of blood pressure is recommended in patients who receive the combination of bupropion and nicotine replacement. There is no clinical experience establishing the safety of bupropion hydrochloride extended-release tablets (SR) in patients with a recent history of myocardial infarction or unstable heart disease. Therefore, care should be exercised if it is used in these groups. Bupropion was well tolerated in depressed patients who had previously developed orthostatic hypotension while receiving tricyclic antidepressants, and was also generally well tolerated in a group of 36 depressed inpatients with stable congestive heart failure (CHF). However, bupropion was associated with a rise in supine blood pressure in the study of patients with CHF, resulting in discontinuation of treatment in 2 patients for exacerbation of baseline hypertension.
Hepatic Impairment:
Bupropion hydrochloride extended-release tablets (SR) should be used with extreme caution in patients with severe hepatic cirrhosis. In these patients, a reduced frequency and/or dose is required. Bupropion hydrochloride extended-release tablets (SR) should be used with caution in patients with hepatic impairment (including mild-to-moderate hepatic cirrhosis) and reduced frequency and/or dose should be considered in patients with mild-to-moderate hepatic cirrhosis. All patients with hepatic impairment should be closely monitored for possible adverse effects that could indicate high drug and metabolite levels (see
CLINICAL PHARMACOLOGY
,
WARNINGS
, and
DOSAGE AND ADMINISTRATION
).
Renal Impairment:
There is limited information on the pharmacokinetics of bupropion in patients with renal impairment. An inter-study comparison between normal subjects and patients with end-stage renal failure demonstrated that the parent drug Cmax and AUC values were comparable in the 2 groups, whereas the hydroxybupropion and threohydrobupropion metabolites had a 2.3- and 2.8-fold increase, respectively, in AUC for patients with end-stage renal failure. A second study, comparing normal subjects and patients with moderate-to-severe renal impairment (GFR 30.910.8 mL/min) showed that exposure to a single 150 mg dose of sustained-release bupropion was approximately 2-fold higher in patients with impaired renal function while levels of the hydroxybupropion and threo/erythrohydrobupropion (combined) metabolites were similar in the 2 groups. Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and subsequently excreted by the kidneys. Bupropion hydrochloride extended-release tablets (SR) should be used with caution in patients with renal impairment and a reduced frequency and/or dose should be considered as bupropion and the metabolites of bupropion may accumulate in such patients to a greater extent than usual. The patient should be closely monitored for possible adverse effects that could indicate high drug or metabolite levels.
Information For Patients
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with bupropion hydrochloride extended-release tablets (SR) and should counsel them in its appropriate use. A patient Medication Guide aboutAntidepressant Medicines, Depression and Other Serious Mental Illnesses, and Suicidal Thoughts or ActionsQuitting Smoking, Quit-Smoking Medication, Changes in Thinking and Behavior, Depression, and Suicidal Thoughts or Actions,andWhat Other Important Information Should I Know About bupropion hydrochloride extended-release tablets (SR)?" is available for bupropion hydrochloride extended-release tablets (SR). The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document. Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking bupropion hydrochloride extended-release tablets (SR).
Clinical Worsening and Suicide Risk in Treating Psychiatric Disorders:
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Neuropsychiatric Symptoms and Suicide Risk in Smoking Cessation Treatment:
Although bupropion hydrochloride extended-release tablets (SR) are not indicated for smoking cessation treatment, it contains the same active ingredient as Zybanwhich is approved for this use. Patients should be informed that quitting smoking, with or without Zybanmay be associated with nicotine withdrawal symptoms (including depression or agitation), or exacerbation of pre-existing psychiatric illness. Furthermore, some patients have experienced changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide when attempting to quit smoking while taking ZybanIf patients develop agitation, hostility, depressed mood, or changes in thinking or behavior that are not typical for them, or if patients develop suicidal ideation or behavior, they should be urged to report these symptoms to their healthcare provider immediately.
Bupropion-Containing Products:
Patients should be made aware that bupropion hydrochloride extended-release tablets (SR) contain the same active ingredient found in Zybanused as an aid to smoking cessation treatment, and that bupropion hydrochloride extended-release tablets should not be used in combination with Zybanor any other medications that contain bupropion hydrochloride (such as Wellbutrinthe immediate-release formulation and Wellbutrin XLthe extended-release formulation). As dose is increased during initial titration to doses above 150 mg/day, patients should be instructed to take bupropion hydrochloride extended-release tablets (SR) in 2 divided doses, preferably with at least 8 hours between successive doses, to minimize the risk of seizures. Patients should be told that bupropion hydrochloride extended-release tablets (SR) should be discontinued and not restarted if they experience a seizure while on treatment Patients should be told that any CNS-active drug like bupropion hydrochloride extended-release tablets (SR) may impair their ability to perform tasks requiring judgment or motor and cognitive skills. Consequently, until they are reasonably certain that bupropion hydrochloride extended-release tablets (SR) do not adversely affect their performance, they should refrain from driving an automobile or operating complex, hazardous machinery. Patients should be told that the excessive use or abrupt discontinuation of alcohol or sedatives (including benzodiazepines) may alter the seizure threshold. Some patients have reported lower alcohol tolerance during treatment with bupropion hydrochloride extended-release tablets (SR). Patients should be advised that the consumption of alcohol should be minimized or avoided. Patients should be advised to inform their physicians if they are taking or plan to take any prescription or over-the-counter drugs. Concern is warranted because bupropion hydrochloride extended-release tablets (SR) and other drugs may affect each other's metabolism. Patients should be advised to notify their physicians if they become pregnant or intend to become pregnant during therapy. Patients should be advised to swallow bupropion hydrochloride extended-release tablets (SR) whole so that the release rate is not altered. Do not chew, divide, or crush tablets, as this may lead to an increased risk of adverse effects, including seizures.
Laboratory Tests
There are no specific laboratory tests recommended.
Drug Interactions
Few systemic data have been collected on the metabolism of bupropion following concomitant administration with other drugs or, alternatively, the effect of concomitant administration of bupropion on the metabolism of other drugs. Because bupropion is extensively metabolized, the coadministration of other drugs may affect its clinical activity. In vitro studies indicate that bupropion is primarily metabolized to hydroxybupropion by the CYP2B6 isoenzyme. Therefore, the potential exists for a drug interaction between bupropion and drugs that are substrates of or inhibitors/inducers of the CYP2B6 isoenzyme (e.g., orphenadrine, thiotepa, cyclophosphamide, ticlopidine, and clopidogrel). In addition, in vitro studies suggest that paroxetine, sertraline, norfluoxetine, and fluvoxamine as well as nelfinavir and efavirenz inhibit the hydroxylation of bupropion. No clinical studies have been performed to evaluate this finding. The threohydrobupropion metabolite of bupropion does not appear to be produced by the cytochrome P450 isoenzymes. The effects of concomitant administration of cimetidine on the pharmacokinetics of bupropion and its active metabolites were studied in 24 healthy young male volunteers. Following oral administration of two 150 mg bupropion hydrochloride extended-release tablets (SR) with and without 800 mg of cimetidine, the pharmacokinetics of bupropion and hydroxybupropion were unaffected. However, there were 16% and 32% increases in the AUC and Cmax, respectively, of the combined moieties of threohydrobupropion and erythrohydrobupropion. In a series of studies in healthy volunteers, ritonavir (100 mg twice daily or 600 mg twice daily) or ritonavir 100 mg plus lopinavir (KALETRA) 400 mg twice daily reduced the exposure of bupropion and its major metabolites in a dose dependent manner by approximately 20% to 80%. This effect is thought to be due to the induction of bupropion metabolism. Patients receiving ritonavir may need increased doses of bupropion, but the maximum recommended dose of bupropion should not be exceeded (see CLINICAL PHARMACOLOGY: Metabolism). While not systematically studied, certain drugs may induce the metabolism of bupropion (e.g., carbamazepine, phenobarbital, phenytoin). Multiple oral doses of bupropion had no statistically significant effects on the single dose pharmacokinetics of lamotrigine in 12 healthy volunteers. Animal data indicated that bupropion may be an inducer of drug-metabolizing enzymes in humans. In one study, following chronic administration of bupropion, 100 mg 3 times daily to 8 healthy male volunteers for 14 days, there was no evidence of induction of its own metabolism. Nevertheless, there may be the potential for clinically important alterations of blood levels of coadministered drugs.
Drugs Metabolized By Cytochrome P450IID6 (CYP2D6):
Many drugs, including most antidepressants (SSRIs, many tricyclics), beta-blockers, antiarrhythmics, and antipsychotics are metabolized by the CYP2D6 isoenzyme. Although bupropion is not metabolized by this isoenzyme, bupropion and hydroxybupropion are inhibitors of CYP2D6 isoenzyme in vitro. In a study of 15 male subjects (ages 19 to 35 years) who were extensive metabolizers of the CYP2D6 isoenzyme, daily doses of bupropion given as 150 mg twice daily followed by a single dose of 50 mg desipramine increased the Cmax, AUC, and tof desipramine by an average of approximately 2-, 5-, and 2-fold, respectively. The effect was present for at least 7 days after the last dose of bupropion. Concomitant use of bupropion with other drugs metabolized by CYP2D6 has not been formally studied. Therefore, coadministration of bupropion with drugs that are metabolized by CYP2D6 isoenzyme including certain antidepressants (e.g., nortriptyline, imipramine, desipramine, paroxetine, fluoxetine, sertraline), antipsychotics (e.g., haloperidol, risperidone, thioridazine), beta-blockers (e.g., metoprolol), and Type 1C antiarrhythmics (e.g., propafenone, flecainide), should be approached with caution and should be initiated at the lower end of the dose range of the concomitant medication. If bupropion is added to the treatment regimen of a patient already receiving a drug metabolized by CYP2D6, the need to decrease the dose of the original medication should be considered, particularly for those concomitant medications with a narrow therapeutic index. Although citalopram is not primarily metabolized by CYP2D6, in one study bupropion increased the Cmax and AUC of citalopram by 30% and 40%, respectively. Citalopram did not affect the pharmacokinetics of bupropion and its three metabolites.
MAO Inhibitors:
Studies in animals demonstrate that the acute toxicity of bupropion is enhanced by the MAO inhibitor phenelzine (see
CONTRAINDICATIONS
).
Levodopa and Amantadine:
Limited clinical data suggest a higher incidence of adverse experiences in patients receiving bupropion concurrently with either levodopa or amantadine. Administration of bupropion hydrochloride extended-release tablets (SR) to patients receiving either levodopa or amantadine concurrently should be undertaken with caution, using small initial doses and gradual dose increases.
Drugs That Lower Seizure Threshold:
Concurrent administration of bupropion hydrochloride extended-release tablets (SR) and agents (e.g., antipsychotics, other antidepressants, theophylline, systemic steroids, etc.) that lower seizure threshold should be undertaken only with extreme caution (see
WARNINGS
). Low initial dosing and gradual dose increases should be employed.
Nicotine Transdermal System:
(see
PRECAUTIONS: Cardiovascular Effects
).
Alcohol:
In postmarketing experience, there have been rare reports of adverse neuropsychiatric events or reduced alcohol tolerance in patients who were drinking alcohol during treatment with bupropion extended-release tablets (SR). The consumption of alcohol during treatment with bupropion extended-release tablets (SR) should be minimized or avoided (also see
CONTRAINDICATIONS
).
Carcinogenesis & Mutagenesis & Impairment Of Fertility
Bupropion produced a positive response (2 to 3 times control mutation rate) in 2 of 5 strains in the Ames bacterial mutagenicity test and an increase in chromosomal aberrations in 1 of 3 in vivo rat bone marrow cytogenetic studies. A fertility study in rats at doses up to 300 mg/kg/day revealed no evidence of impaired fertility.
Pregnancy
Teratogenic Effects:
When rats were administered bupropion at oral doses of up to 300 mg/kg/day (approximately 7 times the MRHD on a mg/m2 basis) prior to mating and throughout pregnancy and lactation, there were no apparent adverse effects on offspring development. One study has been conducted in pregnant women. This retrospective, managed-care database study assessed the risk of congenital malformations overall, and cardiovascular malformations specifically, following exposure to bupropion in the first trimester compared to the risk of these malformations following exposure to other antidepressants in the first trimester and bupropion outside of the first trimester. This study included 7,005 infants with antidepressant exposure during pregnancy, 1,213 of whom were exposed to bupropion in the first trimester. The study showed no greater risk for congenital malformations overall, or cardiovascular malformations specifically, following first trimester bupropion exposure compared to exposure to all other antidepressants in the first trimester, or bupropion outside of the first trimester. The results of this study have not been corroborated. Bupropion hydrochloride extended-release tablets (SR) should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Labor & Delivery
The effect of bupropion hydrochloride extended-release tablets (SR) on labor and delivery in humans is unknown.
Nursing Mothers
Like many other drugs, bupropion and its metabolites are secreted in human milk. Because of the potential for serious adverse reactions in nursing infants from bupropion hydrochloride extended-release tablets (SR), a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established (see
BOX WARNING
and
WARNINGS: Clinical Worsening and Suicide Risk in Treating Psychiatric Disorders
). Anyone considering the use of bupropion in a child or adolescent must balance the potential risks with the clinical need.
Geriatric Use
Of the approximately 6,000 patients who participated in clinical trials with bupropion sustained-release tablets (depression and smoking cessation studies), 275 were 65 and over and 47 were 75 and over. In addition, several hundred patients 65 and over participated in clinical trials using the immediate-release formulation of bupropion (depression studies). No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. A single-dose pharmacokinetic study demonstrated that the disposition of bupropion and its metabolites in elderly subjects was similar to that of younger subjects; however, another pharmacokinetic study, single and multiple dose, has suggested that the elderly are at increased risk for accumulation of bupropion and its metabolites (see
CLINICAL PHARMACOLOGY
). Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and excreted by the kidneys. The risk of toxic reaction to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function (see
PRECAUTIONS: Renal Impairment
and
DOSAGE AND ADMINISTRATION
).
Adverse Reactions
(See also
WARNINGS
and
PRECAUTIONS
.) The information included under the Incidence in Controlled Trials subsection of ADVERSE REACTIONS is based primarily on data from controlled clinical trials with bupropion hydrochloride extended-release tablets (SR). Information on additional adverse events associated with the sustained-release formulation of bupropion in smoking cessation trials, as well as the immediate-release formulation of bupropion, is included in a separate section (see Other Events Observed During the Clinical Development and Postmarketing Experience of Bupropion).
Incidence in Controlled Trials With Bupropion: Adverse Events Associated With Discontinuation of Treatment Among Patients Treated With Bupropion Hydrochloride Extended-Release Tablets (SR):
In placebo-controlled clinical trials, 9% and 11% of patients treated with 300 and 400 mg/day, respectively, of bupropion hydrochloride extended-release tablets (SR) and 4% of patients treated with placebo discontinued treatment due to adverse events. The specific adverse events in these trials that led to discontinuation in at least 1% of patients treated with either 300 mg/day or 400 mg/day of bupropion hydrochloride extended-release tablets (SR) and at a rate at least twice the placebo rate are uled in Table 4. Table 4. Treatment Discontinuations Due to Adverse Events in Placebo-Controlled Trials Adverse Event TermBupropion Hydrochloride Sustained-Release Formulation 300 mg/day (n=376)Bupropion Hydrochloride Sustained-Release Formulation 400 mg/day (n=114)Placebo (n=385)Rash Nausea Agitation Migraine2.4% 0.8% 0.3% 0.0%0.9% 1.8% 1.8% 1.8%0.0% 0.3% 0.3% 0.3%
Adverse Events Occurring at an Incidence of 1% or More Among Patients Treated With Bupropion Hydrochloride Extended-Release Tablets (SR):
Table 5 enumerates treatment-emergent adverse events that occurred among patients treated with 300 and 400 mg/day of bupropion hydrochloride extended-release tablets (SR) and with placebo in placebo-controlled trials. Events that occurred in either the 300- or 400-mg/day group at an incidence of 1% or more and were more frequent than in the placebo group are included. Reported adverse events were classified using a COSTART-based Dictionary. Accurate estimates of the incidence of adverse events associated with the use of any drug are difficult to obtain. Estimates are influenced by drug dose, detection technique, setting, physician judgments, etc. The figures cited cannot be used to predict precisely the incidence of untoward events in the course of usual medical practice where patient characteristics and other factors differ from those that prevailed in the clinical trials. These incidence figures also cannot be compared with those obtained from other clinical studies involving related drug products as each group of drug trials is conducted under a different set of conditions. Finally, it is important to emphasize that the tabulation does not reflect the relative severity and/or clinical importance of the events. A better perspective on the serious adverse events associated with the use of bupropion hydrochloride extended-release tablets (SR) is provided in the WARNINGS and PRECAUTIONS sections. Table 5. Treatment-Emergent Adverse Events in Placebo-Controlled Trials* Body System/ Adverse EventBupropion Hydrochloride Sustained-Release Formulation 300 mg/day (n=376)Bupropion Hydrochloride Sustained-Release Formulation 400 mg/day (n=114)Placebo (n=385)* Adverse events that occurred in at least 1% of patients treated with either 300 or 400 mg/day of bupropion hydrochloride extended-release tablets (SR), but equally or more frequently in the placebo group, were: abnormal dreams, accidental injury, acne, appetite increased, back pain, bronchitis, dysmenorrhea, dyspepsia, flatulence, flu syndrome, hypertension, neck pain, respiratory disorder, rhinitis, and tooth disorder.Incidence based on the number of female patients.- Hyphen denotes adverse events occurring in greater than 0 but less than 0.5% of patients.Body (General)Headache26%25%23%Infection8%9%6%Abdominal pain3%9%2%Asthenia2%4%2%Chest pain3%4%1%Pain2%3%2%Fever1%2%-CardiovascularPalpitation2%6%2%Flushing1%4%-Migraine1%4%1%Hot flashes1%3%1%DigestiveDry mouth17%24%7%Nausea13%18%8%Constipation10%5%7%Diarrhea5%7%6%Anorexia5%3%2%Vomiting4%2%2%Dysphagia0%2%0%MusculoskeletalMyalgia2%6%3%Arthralgia1%4%1%Arthritis0%2%0%Twitch1%2%-Nervous systemInsomnia11%16%6%Dizziness7%11%5%Agitation3%9%2%Anxiety5%6%3%Tremor6%3%1%Nervousness5%3%3%Somnolence2%3%2%Irritability3%2%2%Memory decreased-3%1%Paresthesia1%2%1%Central nervoussystem stimulation2%1%1%RespiratoryPharyngitis3%11%2%Sinusitis3%1%2%Increased cough1%2%1%SkinSweating6%5%2%Rash5%4%1%Pruritus2%4%2%Urticaria2%1%0%Special sensesTinnitus6%6%2%Taste perversion2%4%-Blurred vision or diplopia3%2%2%UrogenitalUrinary frequency2%5%2%Urinary urgency-2%0%Vaginal hemorrhage0%2%-Urinary tract infection1%0%-
Incidence of Commonly Observed Adverse Events in Controlled Clinical Trials:
Adverse events from Table 5 occurring in at least 5% of patients treated with bupropion hydrochloride extended release tablets (SR) and at a rate at least twice the placebo rate are uled below for the 300- and 400-mg/day dose groups.
Bupropion Extended-release Tablets (SR) 300 mg/day:
Anorexia, dry mouth, rash, sweating, tinnitus, and tremor.
Bupropion Extended-release Tablets (SR) 400 mg/day:
Abdominal pain, agitation, anxiety, dizziness, dry mouth, insomnia, myalgia, nausea, palpitation, pharyngitis, sweating, tinnitus, and urinary frequency.
Other Events Observed During the Clinical Development and Postmarketing Experience of Bupropion:
In addition to the adverse events noted above, the following events have been reported in clinical trials and postmarketing experience with the sustained-release formulation of bupropion in depressed patients and in nondepressed smokers, as well as in clinical trials and postmarketing clinical experience with the immediate-release formulation of bupropion. Adverse events for which frequencies are provided below occurred in clinical trials with the sustained-release formulation of bupropion. The frequencies represent the proportion of patients who experienced a treatment-emergent adverse event on at least one occasion in placebo-controlled studies for depression (n = 987) or smoking cessation (n = 1,013), or patients who experienced an adverse event requiring discontinuation of treatment in an open-label surveillance study with bupropion hydrochloride extended-release tablets (SR) (n = 3,100). All treatment-emergent adverse events are included except those uled in Tables 2 through 5, those events uled in other safety-related sections, those adverse events subsumed under COSTART terms that are either overly general or excessively specific so as to be uninformative, those events not reasonably associated with the use of the drug, and those events that were not serious and occurred in fewer than 2 patients. Events of major clinical importance are described in the WARNINGS and PRECAUTIONS sections of the labeling. Events are further categorized by body system and uled in order of decreasing frequency according to the following definitions of frequency: Frequent adverse events are defined as those occurring in at least 1/100 patients. Infrequent adverse events are those occurring in 1/100 to 1/1,000 patients, while rare events are those occurring in less than 1/1,000 patients. Adverse events for which frequencies are not provided occurred in clinical trials or postmarketing experience with bupropion. Only those adverse events not previously uled for sustained-release bupropion are included. The extent to which these events may be associated with bupropion is unknown.
Body (General):
Infrequent were chills, facial edema, musculoskeletal chest pain, and photosensitivity. Rare was malaise. Also observed were arthralgia, myalgia, and fever with rash and other symptoms suggestive of delayed hypersensitivity. These symptoms may resemble serum sickness (see
PRECAUTIONS
).
Cardiovascular:
Infrequent were postural hypotension, stroke, tachycardia, and vasodilation. Rare was syncope. Also observed were complete atrioventricular block, extrasystoles, hypotension, hypertension (in some cases severe, see
PRECAUTIONS
), myocardial infarction, phlebitis, and pulmonary embolism.
Digestive:
Infrequent were abnormal liver function, bruxism, gastric reflux, gingivitis, glossitis, increased salivation, jaundice, mouth ulcers, stomatitis, and thirst. Rare was edema of tongue. Also observed were colitis, esophagitis, gastrointestinal hemorrhage, gum hemorrhage, hepatitis, intestinal perforation, liver damage, pancreatitis, and stomach ulcer.
Endocrine:
Also observed were hyperglycemia, hypoglycemia, and syndrome of inappropriate antidiuretic hormone.
Hemic and Lymphatic:
Infrequent was ecchymosis. Also observed were anemia, leukocytosis, leukopenia, lymphadenopathy, pancytopenia, and thrombocytopenia. Altered PT and/or INR, infrequently associated with hemorrhagic or thrombotic complications, were observed when bupropion was coadministered with warfarin.
Metabolic and Nutritional:
Infrequent were edema and peripheral edema. Also observed was glycosuria.
Musculoskeletal:
Infrequent were leg cramps. Also observed were muscle rigidity/fever/rhabdomyolysis and muscle weakness.
Nervous System:
Infrequent were abnormal coordination, decreased libido, depersonalization, dysphoria, emotional lability, hostility, hyperkinesia, hypertonia, hypesthesia, suicidal ideation, and vertigo. Rare were amnesia, ataxia, derealization, and hypomania. Also observed were abnormal electroencephalogram (EEG), akinesia, aggression, aphasia, coma, completed suicide, delirium, delusions, dysarthria, dyskinesia, dystonia, euphoria, extrapyramidal syndrome, hallucinations, hypokinesia, increased libido, manic reaction, neuralgia, neuropathy, paranoid ideation, restlessness, suicide attempt, and unmasking tardive dyskinesia.
Respiratory:
Rare was bronchospasm. Also observed was pneumonia.
Skin:
Rare was maculopapular rash. Also observed were alopecia, angioedema, exfoliative dermatitis, and hirsutism.
Special Senses:
Infrequent were accommodation abnormality and dry eye. Also observed were deafness, diplopia, increased intraocular pressure, and mydriasis.
Urogenital:
Infrequent were impotence, polyuria, and prostate disorder. Also observed were abnormal ejaculation, cystitis, dyspareunia, dysuria, gynecomastia, menopause, painful erection, salpingitis, urinary incontinence, urinary retention, and vaginitis.
Drug Abuse And Dependence
Controlled Substance Class:
Bupropion is not a controlled substance.
Humans:
Controlled clinical studies of bupropion (immediate-release formulation) conducted in normal volunteers, in subjects with a history of multiple drug abuse, and in depressed patients showed some increase in motor activity and agitation/exclient. In a population of individuals experienced with drugs of abuse, a single dose of 400 mg of bupropion produced mild amphetamine-like activity as compared to placebo on the Morphine-Benzedrine Subscale of the Addiction Research Center Inventories (ARCI), and a score intermediate between placebo and amphetamine on the Liking Scale of the ARCI. These scales measure general feelings of euphoria and drug desirability. Findings in clinical trials, however, are not known to reliably predict the abuse potential of drugs. Nonetheless, evidence from single-dose studies does suggest that the recommended daily dosage of bupropion when administered in divided doses is not likely to be especially reinforcing to amphetamine or stimulant abusers. However, higher doses that could not be tested because of the risk of seizure might be modestly attractive to those who abuse stimulant drugs.
Animals:
Studies in rodents and primates have shown that bupropion exhibits some pharmacologic actions common to psychostimulants. In rodents, it has been shown to increase locomotor activity, elicit a mild stereotyped behavioral response, and increase rates of responding in several schedule-controlled behavior paradigms. In primate models to assess the positive reinforcing effects of psychoactive drugs, bupropion was self-administered intravenously. In rats, bupropion produced amphetamine-like and cocaine-like discriminative stimulus effects in drug discrimination paradigms used to characterize the subjective effects of psychoactive drugs.
Overdosage
Human Overdose Experience:
Overdoses of up to 30 g or more of bupropion have been reported. Seizure was reported in approximately one-third of all cases. Other serious reactions reported with overdoses of bupropion alone included hallucinations, loss of consciousness, sinus tachycardia, and ECG changes such as conduction disturbances (including QRS prolongation) or arrhythmias. Fever, muscle rigidity, rhabdomyolysis, hypotension, stupor, coma, and respiratory failure have been reported mainly when bupropion was part of multiple drug overdoses. Although most patients recovered without sequelae, deaths associated with overdoses of bupropion alone have been reported in patients ingesting large doses of the drug. Multiple uncontrolled seizures, bradycardia, cardiac failure, and cardiac arrest prior to death were reported in these patients.
Overdosage Management:
Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. EEG monitoring is also recommended for the first 48 hours post-ingestion. General supportive and symptomatic measures are also recommended. Induction of emesis is not recommended. Activated charcoal should be administered. There is no experience with the use of forced diuresis, dialysis, hemoperfusion, or exchange transfusion in the management of bupropion overdoses. No specific antidotes for bupropion are known. Due to the dose-related risk of seizures with bupropion hydrochloride extended-release tablets (SR), hospitalization following suspected overdose should be considered. Based on studies in animals, it is recommended that seizures be treated with intravenous benzodiazepine administration and other supportive measures, as appropriate. In managing overdosage, consider the possibility of multiple drug involvement. The physician should consider contacting a poison control center for additional information on the treatment of any overdose. Telephone numbers for certified poison control centers are uled in the Physicians'Desk Reference (PDR).
Dosage & Administration
General Dosing Considerations:
It is particularly important to administer bupropion hydrochloride extended-release tablets (SR) in a manner most likely to minimize the risk of seizure (see
WARNINGS
). Gradual escalation in dosage is also important if agitation, motor restlessness, and insomnia, often seen during the initial days of treatment, are to be minimized. If necessary, these effects may be managed by temporary reduction of dose or the short-term administration of an intermediate to long-acting sedative hypnotic. A sedative hypnotic usually is not required beyond the first week of treatment. Insomnia may also be minimized by avoiding bedtime doses. If distressing, untoward effects supervene, dose escalation should be stopped. Bupropion hydrochloride extended-release tablets (SR) should be swallowed whole and not crushed, divided, or chewed, as this may lead to increased risk of adverse effects including seizures.
Initial Treatment:
The usual adult target dose for bupropion hydrochloride extended-release tablets (SR) is 300 mg/day, given as 150 mg twice daily. Dosing with bupropion hydrochloride extended-release tablets (SR) should begin at 150 mg/day given as a single daily dose in the morning. If the 150 mg initial dose is adequately tolerated, an increase to the 300 mg/day target dose, given as 150 mg twice daily, may be made as early as day 4 of dosing. There should be an interval of at least 8 hours between successive doses.
Increasing the Dosage Above 300 mg/day:
As with other antidepressants, the full antidepressant effect of bupropion hydrochloride extended-release tablets (SR) may not be evident until 4 weeks of treatment or longer. An increase in dosage to the maximum of 400 mg/day, given as 200 mg twice daily, may be considered for patients in whom no clinical improvement is noted after several weeks of treatment at 300 mg/day.
Maintenance Treatment:
It is generally agreed that acute episodes of depression require several months or longer of sustained pharmacological therapy beyond response to the acute episode. In a study in which patients with major depressive disorder, recurrent type, who had responded during 8 weeks of acute treatment with bupropion hydrochloride extended-release tablets (SR) were assigned randomly to placebo or to the same dose of bupropion hydrochloride extended-release tablets (SR) (150 mg twice daily) during 44 weeks of maintenance treatment as they had received during the acute stabilization phase, longer-term efficacy was demonstrated (see
CLINICAL TRIALS
under
CLINICAL PHARMACOLOGY
). Based on these limited data, it is unknown whether or not the dose of bupropion hydrochloride extended-release tablets (SR) needed for maintenance treatment is identical to the dose needed to achieve an initial response. Patients should be periodically reassessed to determine the need for maintenance treatment and the appropriate dose for such treatment.
Dosage Adjustment for Patients with Impaired Hepatic Function:
Bupropion hydrochloride extended-release tablets (SR) should be used with extreme caution in patients with severe hepatic cirrhosis. The dose should not exceed 100 mg every day or 150 mg every other day in these patients. Bupropion hydrochloride extended-release tablets (SR) should be used with caution in patients with hepatic impairment (including mild-to-moderate hepatic cirrhosis) and a reduced frequency and/or dose should be considered in patients with mild-to-moderate hepatic cirrhosis (see
CLINICAL PHARMACOLOGY
,
WARNINGS
, and
PRECAUTIONS
).
Dosage Adjustment for Patients with Impaired Renal Function:
Bupropion hydrochloride extended-release tablets (SR) should be used with caution in patients with renal impairment and a reduced frequency and/or dose should be considered (see
CLINICAL PHARMACOLOGY
and
PRECAUTIONS
).
How Supplied
Storage And Handling
Store at 20to 25(68to 77[See USP Controlled Room Temperature]. Dispense in a tight, light-resistant container as defined in the USP.
Spl Medguide
Package Label.principal Display Panel Section
DRUG: Bupropion Hydrochloride GENERIC: Bupropion Hydrochloride DOSAGE: TABLET ADMINSTRATION: ORAL NDC: 49349-726-02 STRENGTH:150 mg COLOR: white SHAPE: ROUND SCORE: No score SIZE: 11 mm IMPRINT: 30 QTY: 30![]()
![]()
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site