CALCIUM ACETATE (calcium acetate 667 mg) Dailymed
Generic: calcium acetate is used for the treatment of Hypercalcemia Hypocalcemia Kidney Calculi Kidney Failure, Chronic Osteoporosis Osteoporosis, Postmenopausal Hypophosphatemia
Go PRO for all pill images
1 Indications & Usage
Calcium acetate tablet is a phosphate binder indicated to reduce serum phosphorus in patients with end stage renal disease (ESRD).
- Calcium acetate tablet is a phosphate binder indicated for the reduction of serum   phosphorus in patients with end stage renal disease. (
1 )
2 Dosage & Administration
The recommended initial dose of calcium acetate tablets for the adult dialysis patient is 2 tablets with each meal. Increase the dose gradually to lower serum phosphorus levels to the target range, as long as hypercalcemia does not develop. Most patients require 3 to 4 tablets with each meal.
- Starting dose is 2 tablets with each meal. (2)
- Titrate the dose every 2 to 3 weeks until acceptable serum phosphorus level is reached. Most patients require 3 to 4 tablets with each meal. (2)
3 Dosage Forms & Strengths
Tablet:Â 667 mg calcium acetate per tablet.
- Tablets:Â 667 mg calcium acetate per tablet. (3)
4 Contraindications
Patients with hypercalcemia.
- Hypercalcemia. (4)
5 Warnings And Precautions
- Treat mild hypercalcemia by reducing or interrupting calcium acetate tablet and Vitamin D. Severe hypercalcemia may require hemodialysis and discontinuation of calcium acetate tablets. (5.1)
- Hypercalcemia may aggravate digitalis toxicity. (5.2)
5.1 Hypercalcemia
Patients with end stage renal disease may develop hypercalcemia when treated with calcium, including calcium acetate. Avoid the use of calcium supplements, including calcium-based nonprescription antacids, concurrently with calcium acetate.
An overdose of calcium acetate may lead to progressive hypercalcemia, which may require emergency measures. Therefore, early in the treatment phase during the dosage adjustment period, monitor serum calcium levels twice weekly. Should hypercalcemia develop, reduce the calcium acetate dosage or discontinue the treatment, depending on the severity of hypercalcemia.
More severe hypercalcemia (Ca>12 mg/dL) is associated with confusion, delirium, stupor and coma. Severe hypercalcemia can be treated by acute hemodialysis and discontinuing calcium acetate therapy.
Mild hypercalcemia (10.5 to 11.9 mg/dL) may be asymptomatic or manifest as constipation, anorexia, nausea, and vomiting. Mild hypercalcemia is usually controlled by reducing the calcium acetate dose or temporarily discontinuing therapy. Decreasing or discontinuing Vitamin D therapy is recommended as well.
Chronic hypercalcemia may lead to vascular calcification and other soft-tissue calcification. Radiographic evaluation of suspected anatomical regions may be helpful in early detection of soft tissue calcification. The long term effect of calcium acetate on the progression of vascular or soft tissue calcification has not been determined.
Hypercalcemia (>11 mg/dL) was reported in 16% of patients in a 3-month study of a solid dose formulation of calcium acetate; all cases resolved upon lowering the dose or discontinuing treatment.
Maintain the serum calcium-phosphorus (Ca x P) product below 55 mg2/dL2.
5.2 Concomitant Use with Medications
Hypercalcemia may aggravate digitalis toxicity.
6 Adverse Reactions
Hypercalcemia is discussed elsewhere [see Warnings and Precautions (5.1) ].
- The most common (>10%) adverse reactions are hypercalcemia, nausea, and vomiting. (6.1).
- In clinical studies, patients have occasionally experienced nausea during calcium acetate therapy.(
6 )To report SUSPECTED ADVERSE REACTIONS, contact Avet Pharmaceuticals Inc. at 1-866-901-DRUG (3784) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical studies, calcium acetate has been generally well tolerated.
Calcium acetate was studied in a 3-month, open-label, non-randomized study of 98 enrolled ESRD hemodialysis patients and in a two week double-blind, placebo-controlled, cross-over study with 69 enrolled ESRD hemodialysis patients. Adverse reactions (>2% on treatment) from these trials are presented in Table 1.
Table 1: Adverse Reactions in Patients with End-Stage Renal Disease Undergoing Hemodialysis Preferred Term Total adverse reactions reported for calcium acetate n = 167 n (%) 3 - mo, open-label study of calcium acetate n = 98 n (%) Double-blind, placebo-controlled, cross over study of calcium acetate n = 69 Calcium acetate n (%) Placebo n (%) Nausea 6 (3.6) 6 (6.1) 0 (0.0) 0 (0.0) Vomiting 4 (2.4) 4 (4.1) 0 (0.0) 0 (0.0) Hypercalcemia 21 (12.6) 16 (16.3) 5 (7.2) 0 (0.0) Mild hypercalcemia may be asymptomatic or manifest itself as constipation, anorexia, nausea, and vomiting. More severe hypercalcemia is associated with confusion, delirium, stupor, and coma. Decreasing dialysate calcium concentration could reduce the incidence and severity of calcium acetate-induced hypercalcemia. Isolated cases of pruritus have been reported, which may represent allergic reactions.
6.2 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency or to establish a causal relationship to drug exposure.
The following additional adverse reactions have been identified during post-approval of calcium acetate:Â dizziness, edema, and weakness.
7 Drug Interactions
The drug interaction of calcium acetate is characterized by the potential of calcium to bind to drugs with anionic functions (e.g., carboxyl and hydroxyl groups). Calcium Acetate Tablet may decrease the bioavailability of tetracyclines or fluoroquinolones via this mechanism.
There are no empirical data on avoiding drug interactions between calcium acetate and most concomitant drugs. When administering an oral medication with calcium acetate where a reduction in the bioavailability of that medication would have a clinically significant effect on its safety or efficacy, administer the drug one hour before or three hours after calcium acetate. Monitor blood levels of the concomitant drugs that have a narrow therapeutic range. Patients taking anti-arrhythmic medications for the control of arrhythmias and anti-seizure medications for the control of seizure disorders were excluded from the clinical trials with all forms of calcium acetate.
- Calcium acetate tablet may decrease the bioavailability of tetracyclines or fluoroquinolones. (7)
- When clinically significant drug interactions are expected, administer the drug at least one hour before or at least three hours after calcium acetate tablet, or consider monitoring blood levels of the drug. (7)
7.1 Ciprofloxacin
In a study of 15 healthy subjects, a co-administered single dose of 4 calcium acetate tablets approximately 2.7 g, decreased the bioavailability of ciprofloxacin by approximately 50%.
8 Use In Specific Populations
8.1 PREGNANCY
Pregnancy Category C
Calcium acetate tablets contain calcium acetate. Animal reproduction studies have not been conducted with calcium acetate, and there are no adequate and well controlled studies of calcium acetate use in pregnant women. Patients with end stage renal disease may develop hypercalcemia with calcium acetate treatment [see Warnings and Precautions (5.1)]. Maintenance of normal serum calcium levels is important for maternal and fetal well being. Hypercalcemia during pregnancy may increase the risk for maternal and neonatal complications such as stillbirth, preterm delivery, and neonatal hypocalcemia and hypoparathyroidism. Calcium acetate treatment, as recommended, is not expected to harm a fetus if maternal calcium levels are properly monitored during and following treatment.
8.2 LABOR & DELIVERY
The effects of calcium acetate on labor and delivery are unknown.
8.3 NURSING MOTHERS
Calcium acetate tablet contains calcium acetate and is excreted in human milk. Human milk feeding by a mother receiving calcium acetate is not expected to harm an infant, provided maternal serum calcium levels are appropriately monitored.
8.4 PEDIATRIC USE
Safety and effectiveness in pediatric patients have not been established.
8.5 GERIATRIC USE
Clinical studies of calcium acetate did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
10 Overdosage
Administration of calcium acetate tablet in excess of the appropriate daily dosage may result in hypercalcemia [see Warnings and Precautions (5.1)].
11 Description
Calcium acetate tablet acts as a phosphate binder. Its chemical name is calcium acetate. Its molecular formula is C4H6CaO4, and its molecular weight is 158.17. Its structural formula is:
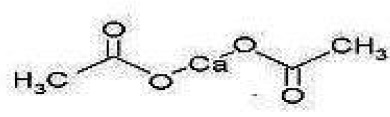
Each calcium acetate tablet contains 667 mg of calcium acetate, (anhydrous; Ca (CH3COO)2; MW = 158.17 grams) equal to 169 mg (8.45 mEq) calcium. In addition, each tablet contains following inactive ingredients: crospovidone, magnesium stearate and sodium lauryl sulfate. Calcium acetate tablets are administered orally for the control of hyperphosphatemia in end stage renal failure.
12 Clinical Pharmacology
Patients with ESRD retain phosphorus and can develop hyperphosphatemia. High serum phosphorus can precipitate serum calcium resulting in ectopic calcification. Hyperphosphatemia also plays a role in the development of secondary hyperparathyroidism in patients with ESRD.
12.1 MECHANISM OF ACTION
Calcium acetate, when taken with meals, combines with dietary phosphate to form an insoluble calcium phosphate complex, which is excreted in the feces, resulting in decreased serum phosphorus concentration.
12.2 PHARMACODYNAMICS
Orally administered calcium acetate from pharmaceutical dosage forms is systemically absorbed up to approximately 40% under fasting conditions and up to approximately 30% under non-fasting conditions. This range represents data from both healthy subjects and renal dialysis patients under various conditions.
13 Nonclinical Toxicology
13.1 CARCINOGENESIS & MUTAGENESIS & IMPAIRMENT OF FERTILITY
No carcinogenicity, mutagenicity, or fertility studies have been conducted with calcium acetate.
14 Clinical Studies
Effectiveness of calcium acetate in decreasing serum phosphorus has been demonstrated in two studies of the calcium acetate solid dosage form.
Ninety-one patients with end-stage renal disease who were undergoing hemodialysis and were hyperphosphatemic (serum phosphorus >5.5 mg/dL) following a 1-week phosphate binder washout period contributed efficacy data to an open-label, non-randomized study.
The patients received calcium acetate tablet [667 mg] at each meal for a period of 12 weeks. The initial starting dose was 2 tablets per meal for 3 meals a day, and the dose was adjusted as necessary to control serum phosphorus levels. The average final dose after 12 weeks of treatment was 3.4 tablets per meal. Although there was a decrease in serum phosphorus, in the absence of a control group the true magnitude of effect is uncertain.
The data presented in Table 2 demonstrate the efficacy of calcium acetate in the treatment of hyperphosphatemia in end-stage renal disease patients. The effects on serum calcium levels are also presented.
Table 2: Average Serum Phosphorous and Calcium Levels at Pre-Study, Interim and Study Completion Time points a Values expressed as mean ± SE.
b Ninety-one patients completed at least 6 weeks of the study.
c ANOVA of difference in values at pre-study and study completion
Parameter Pre-Study Week 4b Week 8 Week 12 p-valuec Phosphorus (mg/dL)a 7.4 ± 0.17 5.9 ± 0.16 5.6 ± 0.17 5.2 ± 0.17 0.01 Calcium (mg/dL)a 8.9 ± 0.09 9.5 ± 0.10 9.7 ± 0.10 9.7 ± 0.10 0.01 There was a 30% decrease in serum phosphorus levels during the 12 week study period (p<0.01). Two-thirds of the decline occurred in the first month of the study. Serum calcium increased 9% during the study mostly in the first month of the study.
Treatment with the phosphate binder was discontinued for patients from the open-label study, and those patients whose serum phosphorus exceeded 5.5 mg/dL were eligible for entry into a double-blind, placebo-controlled, cross-over study. Patients were randomized to receive calcium acetate or placebo, and each continued to receive the same number of tablets as had been individually established during the previous study. Following 2 weeks of treatment, patients switched to the alternative therapy for an additional 2 weeks.
The phosphate binding effect of calcium acetate is shown in the Table 3.
Table 3: Serum Phosphorus and Calcium Levels at Study Initiation and After Completion of Each Treatment Arm
Parameter
Pre-Study
Post-Treatment
p-valueb
Calcium Acetate
Placebo
Phosphorus (mg/dL)a
7.3 ± 0.18
5.9 ± 0.24
7.8 ± 0.22
<0.01
Calcium (mg/dL)a
8.9 ± 0.11
9.5 ± 0.13
8.8 ± 0.12
<0.01
a Values expressed as mean ± SE.
b ANOVA of calcium acetate vs. placebo after 2 weeks of treatment.
Overall, 2 weeks of treatment with calcium acetate statistically significantly (p<0.01) decreased serum phosphorus by a mean of 19% and increased serum calcium by a statistically significant (p<0.01) but clinically unimportant mean of 7%.
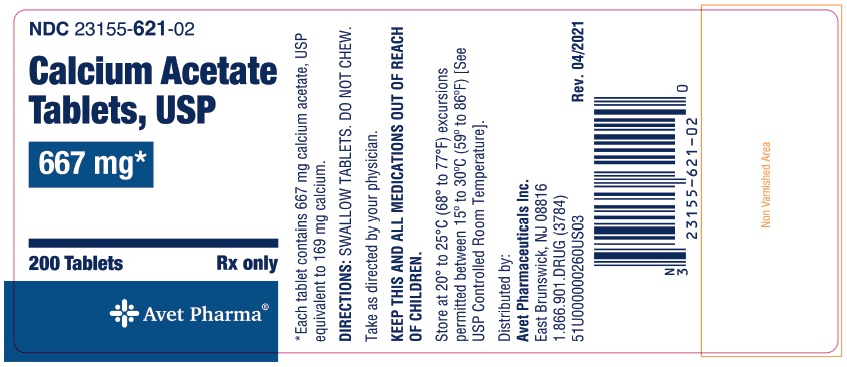
16 How Supplied/storage And Handling
Each Calcium Acetate Tablet USP, intended for oral administration, is white, round tablet, Debossed EP 114 on one side and plain on the reverse side. Each calcium acetate tablet contains 667 mg of calcium acetate (anhydrous Ca(CH3COO)2; MW=158.17 grams) equal to 169 mg (8.45 mEq) calcium and are supplied as follow:
Bottles of 200:Â Â Â NDC 23155-621-02
STORAGE: Store at 20° to 25°C (68° to 77°F) excursions permitted between 15° to 30°C (59° to 86°F) [See USP Controlled Room Temperature].
17 Patient Counseling Information
Inform patients to take calcium acetate tablets with meals, adhere to their prescribed diets, and avoid the use of calcium supplements including nonprescription antacids. Inform the patients about the symptoms of hypercalcemia [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
Advise patients who are taking an oral medication where reduction in the bioavailability of that medication would have clinically significant effect on its safety and efficacy to take the drug one hour before or three hours after calcium acetate tablets.
Distributed by:
Avet Pharmaceuticals Inc.
East Brunswick, NJ 08816
1.866.901.DRUG (3784)

51U000000262US04
Revised: 04/2021
Package Label.principal Display Panel
NDC 23155-621-02
Calcium Acetate Tablets, USP
667 mg
200 Tablets
Rx Only
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


