Clindamycin Hydrochloride Dailymed
Generic: clindamycin hydrochloride is used for the treatment of Acne Vulgaris Actinomycetales Infections Bacteroides Infections Endocarditis, Bacterial Enterocolitis, Pseudomembranous Pneumonia, Pneumocystis Staphylococcal Infections Streptococcal Infections Toxoplasmosis Vaginosis, Bacterial Liver Failure
Boxed Warning
Boxed Warning
Go PRO for all pill images
Boxed Warning
WARNING
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including clindamycin hydrochloride and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon, leading to overgrowth of C. difficile.
Because clindamycin hydrochloride therapy has been associated with severe colitis which may end fatally, it should be reserved for serious infections where less toxic antimicrobial agents are inappropriate, as described in the INDICATIONS AND USAGE section. It should not be used in patients with nonbacterial infections such as most upper respiratory tract infections.
C. difficile produces toxins A and B, which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated
Description
Clindamycin hydrochloride is the hydrated hydrochloride salt of clindamycin. Clindamycin is a semisynthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent compound lincomycin.
Clindamycin Hydrochloride Capsules, USP contain clindamycin hydrochloride equivalent to 150 mg or 300 mg of clindamycin.
Inactive ingredients: anhydrous lactose, magnesium stearate, starch (corn) and talc. The capsule shells contain: D&C Red No. 28, FD&C Blue No. 1, FD&C Red No. 40, gelatin, and titanium dioxide. The 150 mg capsule shell also contains black iron oxide and yellow iron oxide.
The structural formula is represented below:
[Structural formula of clindamycin hydrochloride]
C18H33CIN2O5SâąHClââââââââââM.W. 461.44
The chemical name for clindamycin hydrochloride is Methyl 7-chloro-6,7,8-trideoxy-6-(1-methyl-trans-4-propyl-L-2-pyrrolidinecarboxamido)-1-thio-L-threo-α-D-galacto-octopyranoside monohydrochloride.
Clinical Pharmacology
Human Pharmacology
Absorption Serum level studies with a 150 mg oral dose of clindamycin hydrochloride in 24 normal adult volunteers showed that clindamycin was rapidly absorbed after oral administration. An average peak serum level of 2.50 mcg/mL was reached in 45 minutes; serum levels averaged 1.51 mcg/mL at 3 hours and 0.70 mcg/mL at 6 hours. Absorption of an oral dose is virtually complete (90%), and the concomitant administration of food does not appreciably modify the serum concentrations; serum levels have been uniform and predictable from person to person and dose to dose. Serum level studies following multiple doses of clindamycin hydrochloride for up to 14 days show no evidence of acÂcumÂulation or altered metabolism of drug. Doses of up to 2 grams of clindamycin per day for 14 days have been well tolerated by healthy volunteers, except that the incidence of gastrointestinal side effects is greater with the higher doses.
Distribution Concentrations of clindamycin in the serum increased linearly with increased dose. Serum levels exceed the MIC (minimum inhibitory concentration) for most indicated organisms for at least six hours following administration of the usually recommended doses. Clindamycin is widely distributed in body fluids and tissues (including bones). No significant levels of clindamycin are attained in thecerebrospinal fluid, even in the presence of inflamed meninges.
Excretion The average biological half-life is 2.4 hours. Approximately 10% of the bioactivity is excreted in the urine and 3.6% in the feces; the remainder is excreted as bioinactive metabolites.
Special Populations Renal Impairment Serum half-life of clindamycin is increased slightly in patients with markedly reduced renal function. Hemodialysis and peritoneal dialysis are not effective in removing clindamycin from the serum.
Use in Elderly Pharmacokinetic studies in elderly volunteers (61 to 79 years) and younger adults (18 to 39 years) indicate that age alone does not alter clindamycin pharmacokinetics (clearance, elimination half-life, volume of distribution, and area under the serum concentration-time curve) after IV administration of clindamycin phosphate. After oral administration of clindamycin hydrochloride, elimination half-life is inÂcreased to approximately 4.0 hours (range 3.4 to 5.1 h) in the elderly compared to 3.2 hours (range 2.1 to 4.2 h) in younger adults. The extent of absorption, however, is not different between age groups and no dosage alteration is necessary for the elderly with normal hepatic function and normal (age-adjusted) renal function.
Microbiology
Mechanism of Action
Clindamycin inhibits bacterial protein synthesis by binding to the 23S RNA of the 50S subunit of the ribosome. Clindamycin is bacteriostatic.
Mechanism of Resistance
Resistance to clindamycin is most often caused by modification of specific bases of the 23S ribosomal RNA. Cross-resistance between clindamycin and lincomycin is complete. Because the binding sites for these antibiotics overlap, cross-resistance is sometimes observed among lincosamides, macrolides and streptogramin B. Macrolide-inducible resistance to clindamycin occurs in some isolates of macrolide-resistant bacteria. Macrolide-resistant isolates of staphylococci and beta-hemolytic streptococci should be screened for clindamycin inducible resistance using the D-zone test.
Clindamycin has been shown to be active against most of the isolates of the following microorganisms, both in vitro and in clinical infections, as described in the INDICATIONS AND USAGE section.
Gram-positive Aerobes Staphylococcus aureus (methicillin-susceptible strains) Streptococcus pneumoniae (penicillin-susceptible strains) Streptococcus pyogenes
Anaerobes Clostridium perfringens Fusobacterium necrophorum Fusobacterium nucleatum Peptostreptococcus anaerobius Prevotella melaninogenica
At least 90% of the microorganisms uled below exhibit in vitro minimum inhibitory concentrations (MICs) less than or equal to the clindamycin susceptible MIC breakpoint for organisms of a similar type to those shown in Table 1. However, the efficacy of clindamycin in treating clinical infections due to these microorganisms has not been established in adequate and well-controlled clinical trials.
Gram-positive Aerobes Staphylococcus epidermidis (methicillin-susceptible strains) Streptococcus agalactiae Streptococcus anginosus Streptococcus mitis Streptococcus oralis
Anaerobes Actinomyces israelii Clostridium clostridioforme Eggerthella lentum Finegoldia (âPeptostreptococcusâ) magna Micromonas (âPeptostreptococcusâ) micros Prevotella bivia Prevotella intermedia Propionibacterium acnes
Susceptibility Testing Methods When available, the clinical microbiology laboratory should provide cumulative in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial.
Dilution Techniques Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure based on dilution methods (broth, agar or microdilution)2,3 or equivalent using standardized inoculum and concentrations of clindamycin. The MIC values should be interpreted according to the criteria provided in Table 1.
Diffusion Techniques Quantitative methods that require the measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. The zone size should be determined using a standardized method 2,4. This procedure uses paper disks impregnated with 2 mcg of clindamycin to test the susceptibility of bacteria to clindamycin. The disk diffusion breakpoints are provided in Table 1.
Anaerobic Techniques For anaerobic bacteria, the susceptibility to clindamycin can be determined by a method2,5. The MIC values obtained should be interpreted according to the criteria provided in Table 1.
Table 1. Susceptibility Interpretive Criteria for Clindamycin
Pathogen
Susceptibility Interpretive Criteria
Minimal
Inhibitory Concentrations (MIC in mcg/mL)
Disk
Diffusion (Zone Diameters in mm)
Staphylococcus spp.
S
†0.5
I
1 to 2
R
â„4
S
â„21
I
15 to 20
R
â€14
Streptococcus
pneumoniae and other Streptococcus spp.
â€0.25
0.5
â„1
â„19
16 to 18
â€15
Anaerobic Bacteria
â€2
4
â„8
NA
NA
NA
NA=not applicable
A report of Susceptible (S) indicates that the antimicrobial drug is likely to inhibit growth of the pathogen if the antimicrobial drug reaches the concentration usually achievable at the site of infection. A report of Intermediate (I) indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone that prevents small, uncontrolled technical factors from causing major discrepancies in interpretation. A report of Resistant (R) indicates that the antimicrobial drug if the antimicrobial drug reaches the concentrations usually achievable at the infection site; other therapy should be selected.
Quality Control Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of the supplies and reagents used in the assay, and the techniques of the individuals performing the test.2,3,4,5 Standard clindamycin powder should provide the MIC ranges in Table 2. For the disk diffusion technique using the 2 mcg clindamycin disk the criteria provided in Table 2 should be achieved.
Table 2. Acceptable Quality Control Ranges for Clindamycin to be Used in Validation of Susceptibility Test Results
QC Strain
Acceptable Quality Control Ranges
Minimum Inhibitory
Concentration Range
(mcg/mL)
Disk Diffusion Range
(Zone Diameters in mm)
Enterococcus faecalis1 ATCC 29212
4 to 16
NA
Staphylococcus aureus ATCC 29213
0.06 to 0.25
NA
Staphylococcus aureus ATCC 25923
NA
24 to 30
Streptococcus pneumoniae ATCC 49619
0.03 to 0.12
19 to 25
Bacteroides fragilis ATCC 25285
0.5 to 2
NA
Bacteroides thetaiotaomicron ATCC 29741
2 to 8
NA
Clostridium difficile2 ATCC 700057
2 to 8
Eggerthella lenta ATCC 43055
0.06 to 0.25 NA
1Enterococcus faecalis has been included in this table for quality control purposes only. 2 Quality control for C. difficile is performed using the agar dilution method only, all other obligate anaerobes may be tested by either broth microdilution or agar diffusion methods NA=Not applicable ATCCÂź is a registered trademark of the American Type Culture Collection
Indications And Usage
Clindamycin is indicated in the treatment of serious infections caused by susceptible anaerobic bacteria.
Clindamycin is also indicated in the treatment of serious infections due to susceptible strains of streptococci, pneumococci, and staphylococci. Its use should be reÂserved for penicillin-allergic patients or other patients for whom, in the judgment of the physician, a penicillin is inappropriate. Because of the risk of coÂliÂtis, as described in the WARNING box, before selecting clindamycin, the physician should consider the nature of the infection and the suitability of less toxic alternatives (e.g., erythromycin).
Anaerobes: Serious respiratory tract infections such as empyema, anaerobic pneumonitis, and lung abscess; serious skin and soft tissue infections; septicemia; intra-abdominal infections such as peritonitis and intra-abdominal abscess (typically resulting from anaerobic organisms resident in the normal gastrointestinal tract); infections of the female pelvis and genital tract such as endometritis, nongonococcal tubo-ovarian abscess, pelvic cellulitis, and postsurgical vaginal cuff infection.
Streptococci: Serious respiratory tract infections; serious skin and soft tissue infections.
Staphylococci: Serious respiratory tract infections; serious skin and soft tissue infections.
Pneumococci: Serious respiratory tract infections.
Bacteriologic studies should be performed to determine the causative organisms and their susceptibility to clindamycin.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of clindamycin hydrochloride and other antibacterial drugs, clindamycin hydrochloride should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Contraindications
Clindamycin hydrochloride is contraindicated in individuals with a history of hypersensitivity to preparations containing clindamycin or lincomycin.
Warnings
See WARNING box.
Clostridium difficile associated diarrhea
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including clindamycin hydrochloride, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon, leading to overgrowth of C. difficile.
C. difficile produces toxins A and B, which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy.
CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Severe Skin Reactions
Severe skin reactions such as Toxic Epidermal Necrolysis, some with fatal outcome, have been reported. In case of such an event, treatment should be permanently discontinued.
A careful inquiry should be made concerning previous sensitivities to drugs and other allergens.
Usage in Meningitis
Since clindamycin does not diffuse adequately into the cerebrospinal fluid, the drug should not be used in the treatment of meningitis.
Precautions
General
Review of experience to date suggests that a subgroup of older patients with associated severe illness may tolerate diarrhea less well. When clindamycin is indicated in these patients, they should be carefully monitored for change in bowel frequency.
Clindamycin hydrochloride should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis.
Clindamycin hydrochloride should be prescribed with caution in atopic individuals.
Indicated surgical procedures should be performed in conjunction with antibiotic therapy.
The use of clindamycin hydrochloride occasionally results in overgrowth of nonsusceptible organismsâparticularly yeasts. Should superinfections occur, appropriate measures should be taken as indicated by the clinical situation.
Clindamycin dosage modification may not be necessary in patients with renal disease. In patients with moderate to severe liver disease, prolongation of clindamycin half-life has been found. However, it was postulated from studies that when given every eight hours, acÂcumÂulation should rarely occur. ThereÂfore, dosage modification in patients with liver disease may not be necessary. However, periodic liver enzyme deterÂminaÂtions should be made when treating patients with severe liver disease.
Prescribing clindamycin hydrochloride in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
Patients should be counseled that antibacterial drugs, including clindamycin hydrochloride should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When clindamycin hydrochloride is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by clindamycin hydrochloride or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Laboratory Tests
During prolonged therapy, periodic liver and kidney function tests and blood counts should be performed.
Drug Interactions
Clindamycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used with caution in patients receiving such agents.
Antagonism has been demonstrated between clindamycin and erythromycin in vitro. Because of possible clinical significance, these two drugs should not be administered concurrently.
Carcinogenesis, Mutagenesis, ImpairÂment of Fertility
Long-term studies in animals have not been performed with clindamycin to evaluate carcinogenic potential. GenoÂtoxicity tests performed included a rat micronucleus test and an Ames Salmonella reversion test. Both tests were negative.
Fertility studies in rats treated orally with up to 300 mg/kg/day (approximately 1.6 times the highest recommended adult human dose based on mg/m2) revealed no effects on fertility or mating ability.
Pregnancy: Teratogenic effects
Pregnancy Category B
In clinical trials with pregnant women, the systemic administration of clindamycin during the second and third trimesters, has not been associated with an increased frequency of congenital abnormalities.
Clindamycin should be used during the first trimester of pregnancy only if clearly needed. There are no adequate and well-controlled studies in pregnant women during the first trimester of pregnancy. Because animal reproduction studies are not always predictive of the human response, this drug should be used during pregnancy only if clearly needed.
Reproduction studies performed in rats and mice using oral doses of clindamycin up to 600 mg/kg/day (3.2 and 1.6 times the highest recommended adult human dose based on mg/m2, respectively) or subcutaneous doses of clindamycin up to 250 mg/kg/day (1.3 and 0.7 times the highest recommended adult human dose based on mg/m2, respectively) revealed no evidence of teratogenicity.
Nursing Mothers
Clindamycin has been reported to appear in breast milk in the range of 0.7 to 3.8 mcg/mL. Because of the potential for serious adverse reactions in nursing infants, clindamycin should not be taken by nursing mothers.
Pediatric Use
When clindamycin hydrochloride is adÂministered to the pediatric population (birth to 16 years), appropriate monitoring of organ system functions is desirable.
Geriatric Use
Clinical studies of clindamycin did not include sufficient numbers of patients age 65 and over to determine whether they respond differently from younger patients. However, other reported clinical experience indicates that antibiotic-associated colitis and diarrhea (due to Clostridium difficile) seen in association with most antibiotics occur more frequently in the elderly (greater than 60 years) and may be more severe. These patients should be carefully monitored for the development of diarrhea.
Pharmacokinetic studies with clindamycin have shown no clinically important differences between young and elderly subjects with normal hepatic function and normal (age-adjusted) renal function after oral or intravenous administration.
Adverse Reactions
The following reactions have been reported with the use of clindamycin.
Gastrointestinal:
Abdominal pain, pseuÂdoÂmembranous colitis, esophagitis, nausea, vomiting, and diarrhea (see WARNING box). The onset of pseudoÂmembranous colitis symptoms may occur during or after antibacterial treatment (see WARNINGS). Esophageal ulcer has been reported.
Hypersensitivity Reactions:
Generalized mild to moderate morbilliform-like (maculopapular) skin rashes are the most frequently reported adverse reactions. Vesiculobullous rashes, as well as urticaria, have been observed during drug therapy. Severe skin reactions such as Toxic Epidermal Necrolysis, some with fatal outcome, have been reported (see WARNINGS). Cases of Acute Generalized Exanthematous Pustulosis (AGEP), erythema multiforme, some resembling Stevens-Johnson syndrome, and anaphylactoid reactions have also been reported.
Skin and Mucous Membranes:
Pruritus, vaginitis, and rare instances of exfoliative dermatitis have been reported. (See HYPERSENSITIVITY REACTIONS.)
Liver:
Jaundice and abnormalities in liver function tests have been observed during clindamycin therapy.
Renal:
Although no direct relationship of clindamycin to renal damage has been established, renal dysfunction as evidenced by azotemia, oliguria, and/or proteinuria has been observed.
Hematopoietic:
Transient neutropenia (leukopenia) and eosinophilia have been reported. Reports of agranulocytosis and thrombocytopenia have been made. No direct etiologic relationship to concurrent clindamycin therapy could be made in any of the foregoing.
Immune System:
Drug reaction with eosinophilia and systemic symptoms (DRESS) cases have been reported.
Musculoskeletal:
Cases of polyarthritis have been reported.
To report SUSPECTED ADVERSE EVENTS, contact Actavis at 1-800-272-5525 or FDA at 1-800-FDA-1088 or http://www.fda.gov/ for voluntary reporting of adverse reactions.
Overdosage
Significant mortality was observed in mice at an intravenous dose of 855 mg/kg and in rats at an oral or subcutaneous dose of approximately 2618 mg/kg. In the mice, convulsions and depression were observed.
Hemodialysis and peritoneal dialysis are not effective in removing clindamycin from the serum.
Dosage And Administration
If significant diarrhea occurs during therapy, this antibiotic should be discontinued (see WARNING box).
Adults: Serious infectionsâ150 to 300 mg every 6 hours. More severe infectionsâ300 to 450 mg every 6 hours.
Pediatric Patients: Serious infectionsâ8 to 16 mg/kg/day (4 to 8 mg/lb/day) divided into three or four equal doses. More severeinfectionsâ16 to 20 mg/kg/day (8 to 10 mg/lb/day) divided into three or four equal doses.
To avoid the possibility of esophageal irritation, clindamycin hydrochloride capsules should be taken with a full glass of water.
Serious infections due to anaerobic bacteria are usually treated with clindamycin injection. However, in clinically appropriate circumstances, the physician may elect to initiate treatment or continue treatment with clindamycin hydrochloride capsules.
In cases of ÎČ-hemolytic streptococcal infections, treatment should continue for at least 10 days.
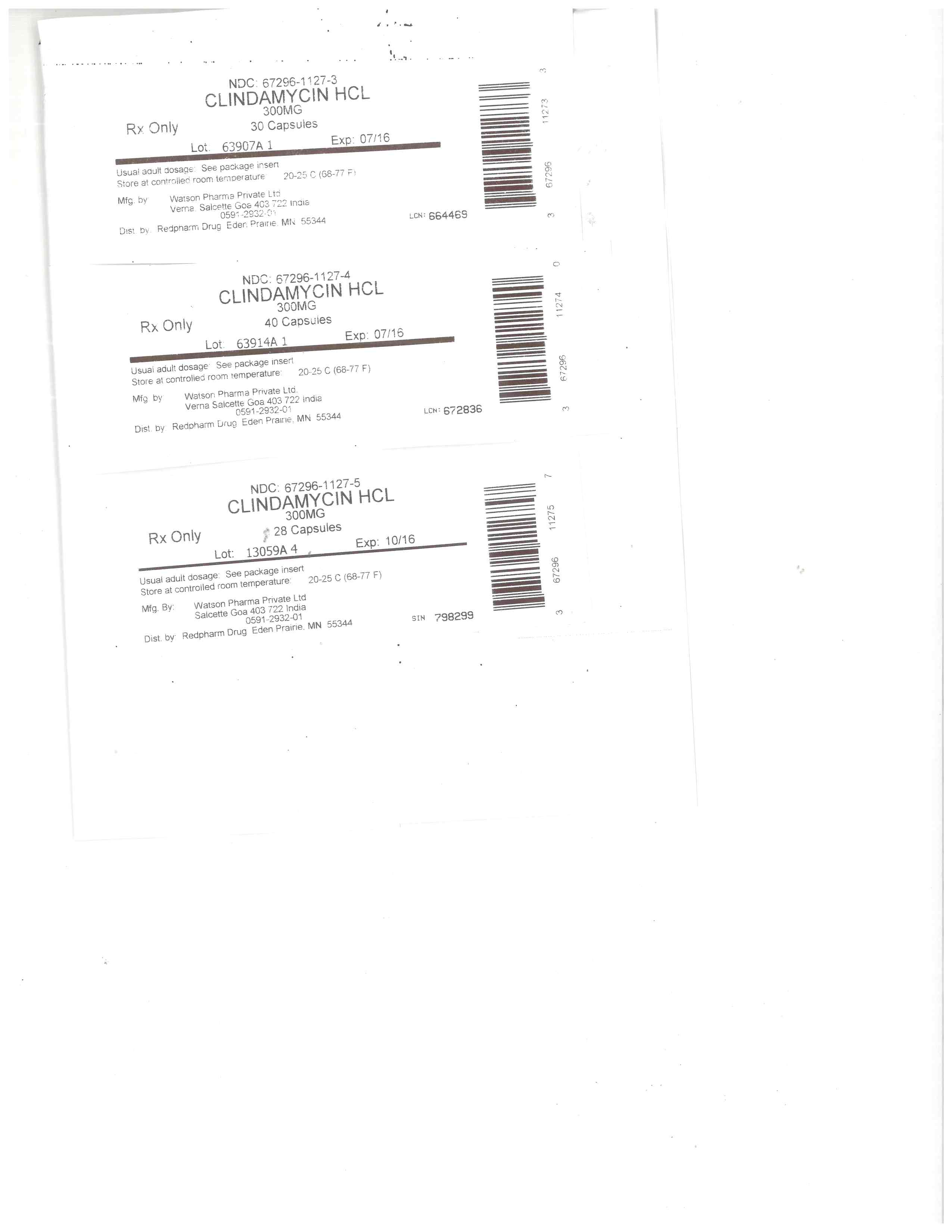
How Supplied
Clindamycin hydrochloride capsules, USP (equivalent to 150 mg of clindamycin) are opaque gray and opaque pink capsules imprinted âDAN 5708â supplied in bottles of 100.
Clindamycin hydrochloride capsules, USP (equivalent to 300 mg of clindamycin) are opaque pink capsules imprinted âDAN 3120â supplied in bottles of 16 and 100.
Dispense in a tight container with a child-resistant closure.
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
References
1. Smith RB, Phillips JP: Evaluation of CLEOCIN HCl and CLEOCIN Phosphate in an Aged Population. Upjohn TR 8147-82-9122-021, December 1982.
2. CLSI. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-sixth Informational Supplement. CLSI document M 100-S26. Wayne, PA: Clinical and Laboratory Standards Institute; 2016.
3. CLSI. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically; Approved Standard â Tenth Edition. CLSI document M07-A10. Wayne, PA: Clinical and Laboratory Standards Institute; 2015.
4. CLSI. Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard -Twelfth Edition. CLSI document M02-A12. Wayne, PA: Clinical and Laboratory Standards Institute; 2015.
5. CLSI. Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria; Approved Standard-Eighth Edition. CLSI document M11-A8. Wayne, PA: Clinical and Laboratory Standards Institute; 2012.
Manufactured by: Watson Pharma Private Limited Verna, Salcette Goa 403 722 INDIA
Distributed by: Actavis Pharma, Inc. Parsippany, NJ 07054 USA
Revised: May 2016
Principal Display Panel
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site