SEGLUROMET (ertugliflozin pidolate 2.5 mg metformin hydrochloride 500 mg) Dailymed
Generic: ertugliflozin and metformin hydrochloride is used for the treatment of Kidney Failure, Chronic Renal Insufficiency Acidosis Diabetes Mellitus, Type 2 Liver Diseases Diabetic Ketoacidosis
IMPRINT: 2 5 500
SHAPE: oval
COLOR: pink
All Imprints
ertugliflozin 2.5 mg / metformin hydrochloride 500 mg oral tablet [segluromet] - 2 5 500 oval pink
ertugliflozin 2.5 mg / metformin hydrochloride 1000 mg oral tablet [segluromet] - 2 5 1000 oval pink
ertugliflozin 7.5 mg / metformin hydrochloride 500 mg oral tablet [segluromet] - 7 5 500 oval red
ertugliflozin 7.5 mg / metformin hydrochloride 1000 mg oral tablet [segluromet] - 7 5 1000 oval red
Boxed Warning
Warning: Lactic Acidosis
-
Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. Symptoms included malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Laboratory abnormalities included elevated blood lactate levels, anion gap acidosis, increased lactate/pyruvate ratio, and metformin plasma levels generally >5 mcg/mL. ( 5.1 ) -
Risk factors include renal impairment, concomitant use of certain drugs, age ‚Č•65 years old, radiological studies with contrast, surgery and other procedures, hypoxic states, excessive alcohol intake, and hepatic impairment. Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided in the Full Prescribing Information. ( 5.1 ) -
If lactic acidosis is suspected, discontinue SEGLUROMET and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended. ( 5.1 )
Go PRO for all pill images
Recent Major Changes Section
- Indications and Usage (
1 )- Dosage and Administration (
2.1 ,2.4 )- Warnings and Precautions (
5.2 )
09/2023
09/2023
09/2023
Warning: Lactic Acidosis
Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis was characterized by elevated blood lactate levels (>5 mmol/Liter), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate/pyruvate ratio, and metformin plasma levels generally >5 mcg/mL [seeWarnings and Precautions (5.1)].
Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (e.g., carbonic anhydrase inhibitors such as topiramate), age 65 years old or greater, having a radiological study with contrast, surgery and other procedures, hypoxic states (e.g., acute congestive heart failure), excessive alcohol intake, and hepatic impairment.
Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided in the Full Prescribing Information [seeDosage and Administration (2.2),Contraindications (4),Warnings and Precautions (5.1),Drug Interactions (7), andUse in Specific Populations (8.6,8.7)].
If metformin-associated lactic acidosis is suspected, immediately discontinue SEGLUROMET and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended [seeWarnings and Precautions (5.1)].
WARNING: LACTIC ACIDOSIS
See full prescribing information for complete boxed warning.
Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. Symptoms included malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Laboratory abnormalities included elevated blood lactate levels, anion gap acidosis, increased lactate/pyruvate ratio, and metformin plasma levels generally >5 mcg/mL. ( 5.1 )Risk factors include renal impairment, concomitant use of certain drugs, age ‚Č•65 years old, radiological studies with contrast, surgery and other procedures, hypoxic states, excessive alcohol intake, and hepatic impairment. Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided in the Full Prescribing Information. ( 5.1 )If lactic acidosis is suspected, discontinue SEGLUROMET and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended. ( 5.1 )
1 Indications And Usage
SEGLUROMET¬ģ is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus.
SEGLUROMET is a combination of ertugliflozin, a sodium glucose co-transporter 2 (SGLT2) inhibitor, and metformin, a biguanide, indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. (1 )
Limitations of Use:
Not recommended for use to improve glycemic control in patients with type 1 diabetes mellitus. (1 )
Limitations of Use
Not recommended for use to improve glycemic control in patients with type 1 diabetes mellitus [see Warnings and Precautions (5.2)].
2 Dosage And Administration
- Assess renal function prior to initiation and as clinically indicated. (
2.1 )- Correct volume depletion before initiation. (
2.1 )- Individualize the starting dose based on the patient's current regimen. (
2.2 )- Maximum recommended dose is 7.5 mg ertugliflozin/1,000 mg metformin twice daily. (
2.2 )- Take twice daily with meals, with gradual dose escalation. (
2.2 )
- Do not use in patients with an estimated glomerular filtration rate (eGFR) below 30 mL/minute/1.73 m2.
- Use is not recommended in patients with an eGFR less than 45 mL/min/1.73 m2. (
2.2 )- Use is contraindicated in patients with severe renal impairment (eGFR less than 30 mL/min/1.73 m2), end stage-renal disease (ESRD), or on dialysis. (
2.2 )- SEGLUROMET may need to be discontinued at time of, or prior to, iodinated contrast imaging procedures. (
2.3 )- Withhold SEGLUROMET for at least 4 days, if possible, prior to major surgery or procedures associated with prolonged fasting. (
2.4 )2.1Prior to Initiation of SEGLUROMET
- Assess renal function prior to initiation of SEGLUROMET and as clinically indicated [see Warnings and Precautions (5.2)].
Assess volume status. In patients with volume depletion, correct this condition before initiating SEGLUROMET [see Warnings and Precautions (5.4), Use in Specific Populations (8.5, 8.6)]. 2.2Recommended Dosage
- Individualize the starting dose of SEGLUROMET, ertugliflozin and metformin hydrochloride (HCl), based on the patient’s current regimen, while not exceeding the maximum recommended daily dose of 15 mg ertugliflozin and 2,000 mg metformin HCl:
- In patients on metformin HCl, switch to SEGLUROMET tablets containing 2.5 mg ertugliflozin, with a similar total daily dose of metformin HCl.
- In patients on ertugliflozin, switch to SEGLUROMET tablets containing 500 mg metformin HCl, with a similar total daily dose of ertugliflozin.
- In patients already treated with ertugliflozin and metformin HCl, switch to SEGLUROMET tablets containing the same total daily dose of ertugliflozin and a similar daily dose of metformin HCl.
- Take SEGLUROMET twice daily with meals, with gradual dose escalation for those initiating metformin HCl to reduce the gastrointestinal side effects due to metformin [seeAdverse Reactions (6.1)].
- Dosing may be adjusted based on effectiveness and tolerability.
- Use of SEGLUROMET is not recommended in patients with an eGFR less than 45 mL/min/1.73 m2.
- Use of SEGLUROMET is contraindicated in patients with severe renal impairment (eGFR less than 30 mL/min/1.73 m2), end stage-renal disease (ESRD), or on dialysis [see Contraindications (4)].
2.3Discontinuation for Iodinated Contrast Imaging Procedures
Discontinue SEGLUROMET at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR less than 60 mL/min/1.73 m2; in patients with a history of liver disease, alcoholism or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure; restart SEGLUROMET if renal function is stable [seeWarnings and Precautions (5.1)].
2.4 Temporary Interruption for Surgery
Withhold SEGLUROMET for at least 4 days, if possible, prior to major surgery or procedures associated with prolonged fasting. Resume SEGLUROMET when the patient is clinically stable and has resumed oral intake [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].
3 Dosage Forms And Strengths
- Tablets: ertugliflozin 2.5 mg and metformin HCl 500 mg, pink, oval, debossed with "2.5/500" on one side and plain on the other side.
- Tablets: ertugliflozin 2.5 mg and metformin HCl 1,000 mg, pink, oval, debossed with "2.5/1000" on one side and plain on the other side.
- Tablets: ertugliflozin 7.5 mg and metformin HCl 500 mg, red, oval, debossed with "7.5/500" on one side and plain on the other side.
- Tablets: ertugliflozin 7.5 mg and metformin HCl 1,000 mg, red, oval, debossed with "7.5/1000" on one side and plain on the other side.
Tablets:
- Ertugliflozin 2.5 mg and metformin hydrochloride 500 mg (
3 )- Ertugliflozin 2.5 mg and metformin hydrochloride 1,000 mg (
3 )- Ertugliflozin 7.5 mg and metformin hydrochloride 500 mg (
3 )- Ertugliflozin 7.5 mg and metformin hydrochloride 1,000 mg (
3 )
4 Contraindications
- Hypersensitivity to ertugliflozin, metformin, or any excipient in SEGLUROMET, reactions such as angioedema or anaphylaxis have occurred [see Adverse Reactions (6.2)].
- Patients with severe renal impairment (eGFR less than 30 mL/min/1.73 m2), end stage-renal disease (ESRD), or on dialysis [see Use in Specific Populations (8.6)].
- Acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma.
- Severe renal impairment (eGFR less than 30 mL/min/1.73 m2), end stage-renal disease, or patients on dialysis. (
4 )- Metabolic acidosis, including diabetic ketoacidosis. (
4 )- Hypersensitivity to ertugliflozin, metformin or any excipient. (
4 )
5 Warnings And Precautions
- Lactic Acidosis: See
boxed warning . (5.1 )- Diabetic Ketoacidosis in Patients with Type 1 Diabetes Mellitus and Other Ketoacidosis: Consider ketone monitoring in patients at risk for ketoacidosis, as indicated. Assess for ketoacidosis regardless of presenting blood glucose levels and discontinue SEGLUROMET if ketoacidosis is suspected. Monitor patients for resolution of ketoacidosis before restarting. (
5.2 )- Lower Limb Amputation: Consider factors that may increase the risk of amputation before initiating SEGLUROMET. Monitor patients for infections or ulcers of lower limbs, and discontinue if these occur. (
5.3 )- Volume Depletion: May result in acute kidney injury. Before initiating, assess and correct volume status in patients with renal impairment, low systolic blood pressure, elderly patients, or patients on diuretics. Monitor for signs and symptoms during therapy. (
5.4 )- Urosepsis and Pyelonephritis: Evaluate patients for signs and symptoms of urinary tract infections and treat promptly, if indicated. (
5.5 )- Hypoglycemia: Consider a lower dose of insulin or insulin secretagogue to reduce risk of hypoglycemia when used in combination. (
5.6 )- Necrotizing Fasciitis of the Perineum (Fournier's Gangrene): Serious, life-threatening cases have occurred in both females and males. Assess patients presenting with pain or tenderness, erythema, or swelling in the genital or perineal area, along with fever or malaise. If suspected, institute prompt treatment. (
5.7 )- Genital Mycotic Infections: Monitor and treat if indicated. (
5.8 )- Vitamin B12 Deficiency: Metformin may lower vitamin B12 levels. Measure hematological parameters annually. (
5.9 )5.1Lactic Acidosis
There have been postmarketing cases of metformin-associated lactic acidosis, including fatal cases. These cases had a subtle onset and were accompanied by nonspecific symptoms such as malaise, myalgias, abdominal pain, respiratory distress, or increased somnolence; however, hypothermia, hypotension and resistant bradyarrhythmias have occurred with severe acidosis. Metformin-associated lactic acidosis was characterized by elevated blood lactate concentrations (>5 mmol/Liter), anion gap acidosis (without evidence of ketonuria or ketonemia), and an increased lactate: pyruvate ratio; metformin plasma levels were generally >5 mcg/mL. Metformin decreases liver uptake of lactate increasing lactate blood levels which may increase the risk of lactic acidosis, especially in patients at risk.
If metformin-associated lactic acidosis is suspected, general supportive measures should be instituted promptly in a hospital setting, along with immediate discontinuation of SEGLUROMET. In SEGLUROMET-treated patients with a diagnosis or strong suspicion of lactic acidosis, prompt hemodialysis is recommended to correct the acidosis and remove accumulated metformin (metformin hydrochloride is dialyzable, with a clearance of up to 170 mL/minute under good hemodynamic conditions). Hemodialysis has often resulted in reversal of symptoms and recovery.
Educate patients and their families about the symptoms of lactic acidosis and if these symptoms occur instruct them to discontinue SEGLUROMET and report these symptoms to their healthcare provider.
For each of the known and possible risk factors for metformin-associated lactic acidosis, recommendations to reduce the risk of and manage metformin-associated lactic acidosis are provided below:
Renal Impairment: The postmarketing metformin-associated lactic acidosis cases primarily occurred in patients with significant renal impairment. The risk of metformin accumulation and metformin-associated lactic acidosis increases with the severity of renal impairment because metformin is substantially excreted by the kidney [seeWarnings and Precautions (5.4)andClinical Pharmacology (12.3)].
- Before initiating SEGLUROMET, obtain an eGFR.
- Use of SEGLUROMET is not recommended in patients with an eGFR less than 45 mL/min/1.73 m2.
- SEGLUROMET is contraindicated in patients with severe renal impairment (an eGFR less than 30 mL/min/1.73 m2), end stage-renal disease (ESRD), or on dialysis.
- Obtain an eGFR at least annually in all patients taking SEGLUROMET. In patients at increased risk for the development of renal impairment (e.g., the elderly), renal function should be assessed more frequently.
Drug Interactions: The concomitant use of SEGLUROMET with specific drugs may increase the risk of metformin-associated lactic acidosis: those that impair renal function, result in significant hemodynamic change, interfere with acid-base balance or increase metformin accumulation (e.g., cationic drugs) [seeDrug Interactions (7)]. Therefore, consider more frequent monitoring of patients.
Age 65 or Greater: The risk of metformin-associated lactic acidosis increases with the patient's age because elderly patients have a greater likelihood of having hepatic, renal, or cardiac impairment than younger patients. Assess renal function more frequently in elderly patients [seeUse in Specific Populations (8.5)].
Radiological Studies with Contrast: Administration of intravascular iodinated contrast agents in metformin-treated patients has led to an acute decrease in renal function and the occurrence of lactic acidosis. Stop SEGLUROMET at the time of, or prior to, an iodinated contrast imaging procedure in patients with an eGFR less than 60 mL/min/1.73 m2; in patients with a history of hepatic impairment, alcoholism, or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure, and restart SEGLUROMET if renal function is stable.
Surgery and Other Procedures: Withholding of food and fluids during surgical or other procedures may increase the risk for volume depletion, hypotension and renal impairment. SEGLUROMET should be temporarily discontinued while patients have restricted food and fluid intake.
Hypoxic States: Several of the postmarketing cases of metformin-associated lactic acidosis occurred in the setting of acute congestive heart failure (particularly when accompanied by hypoperfusion and hypoxemia). Cardiovascular collapse (shock), acute myocardial infarction, sepsis, and other conditions associated with hypoxemia have been associated with lactic acidosis and may also cause pre-renal azotemia. When such events occur, discontinue SEGLUROMET.
Excessive Alcohol Intake: Alcohol potentiates the effect of metformin on lactate metabolism and this may increase the risk of metformin-associated lactic acidosis. Warn patients against excessive alcohol intake while receiving SEGLUROMET.
Hepatic Impairment: Patients with hepatic impairment have developed metformin-associated lactic acidosis. This may be due to impaired lactate clearance resulting in higher lactate blood levels. Therefore, avoid use of SEGLUROMET in patients with clinical or laboratory evidence of hepatic disease.
5.2 Diabetic Ketoacidosis in Patients with Type 1 Diabetes Mellitus and Other Ketoacidosis
In patients with type 1 diabetes mellitus, SEGLUROMET significantly increases the risk of diabetic ketoacidosis, a life-threatening event, beyond the background rate. In placebo-controlled trials of patients with type 1 diabetes mellitus, the risk of ketoacidosis was markedly increased in patients who received sodium glucose transporter 2 (SGLT2) inhibitors compared to patients who received placebo; this risk may be greater with higher doses. SEGLUROMET is not indicated for glycemic control in patients with type 1 diabetes mellitus.
Type 2 diabetes mellitus and pancreatic disorders (e.g., history of pancreatitis or pancreatic surgery) are also risk factors for ketoacidosis. There have been postmarketing reports of fatal events of ketoacidosis in patients with type 2 diabetes mellitus using SGLT2 inhibitors.
Precipitating conditions for diabetic ketoacidosis or other ketoacidosis include under-insulinization due to insulin dose reduction or missed insulin doses, acute febrile illness, reduced caloric intake, ketogenic diet, surgery, volume depletion, and alcohol abuse.
Signs and symptoms are consistent with dehydration and severe metabolic acidosis and include nausea, vomiting, abdominal pain, generalized malaise, and shortness of breath. Blood glucose levels at presentation may be below those typically expected for diabetic ketoacidosis (e.g., less than 250 mg/dL). Ketoacidosis and glucosuria may persist longer than typically expected. Urinary glucose excretion persists for 4 days after discontinuing SEGLUROMET [see Clinical Pharmacology (12.2)]; however, there have been postmarketing reports of ketoacidosis and/or glucosuria lasting greater than 6 days and some up to 2 weeks after discontinuation of SGLT2 inhibitors.
Consider ketone monitoring in patients at risk for ketoacidosis if indicated by the clinical situation. Assess for ketoacidosis regardless of presenting blood glucose levels in patients who present with signs and symptoms consistent with severe metabolic acidosis. If ketoacidosis is suspected, discontinue SEGLUROMET, promptly evaluate, and treat ketoacidosis, if confirmed. Monitor patients for resolution of ketoacidosis before restarting SEGLUROMET.
Withhold SEGLUROMET, if possible, in temporary clinical situations that could predispose patients to ketoacidosis. Resume SEGLUROMET when the patient is clinically stable and has resumed oral intake [see Dosage and Administration (2.4)].
Educate all patients on the signs and symptoms of ketoacidosis and instruct patients to discontinue SEGLUROMET and seek medical attention immediately if signs and symptoms occur.
5.3Lower Limb Amputation
In a long-term cardiovascular outcomes study [seeClinical Studies (14.2)], in patients with type 2 diabetes and established cardiovascular disease, the occurrence of non-traumatic lower limb amputations was reported with event rates of 4.7, 5.7, and 6.0 events per 1,000 patient-years in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg treatment arms, respectively.
Amputation of the toe and foot were most frequent (81 out of 109 patients with lower limb amputations). Some patients had multiple amputations, some involving both lower limbs.
Lower limb infections, gangrene, and diabetic foot ulcers were the most common precipitating medical events leading to the need for an amputation. Patients with amputations were more likely to be male, have higher A1C (%) at baseline, have a history of peripheral arterial disease, amputation or peripheral revascularization procedure, diabetic foot, and to have been taking diuretics or insulin.
Across seven ertugliflozin clinical trials, non-traumatic lower limb amputations were reported in 1 (0.1%) patient in the comparator group, 3 (0.2%) patients in the ertugliflozin 5 mg group, and 8 (0.5%) patients in the ertugliflozin 15 mg group.
Before initiating SEGLUROMET, consider factors in the patient history that may predispose them to the need for amputations, such as a history of prior amputation, peripheral vascular disease, neuropathy and diabetic foot ulcers. Counsel patients about the importance of routine preventative foot care. Monitor patients receiving SEGLUROMET for signs and symptoms of infection (including osteomyelitis), new pain or tenderness, sores or ulcers involving the lower limbs, and discontinue SEGLUROMET if these complications occur.
5.4Volume Depletion
SEGLUROMET can cause intravascular volume contraction which may sometimes manifest as symptomatic hypotension or acute transient changes in creatinine [see Adverse Reactions (6.1)]. There have been postmarketing reports of acute kidney injury, some requiring hospitalization and dialysis, in patients with type 2 diabetes mellitus receiving SGLT2 inhibitors, including SEGLUROMET. Patients with impaired renal function (eGFR less than 60 mL/min/1.73 m2) [see Use in Specific Populations (8.6)], elderly patients, patients with low systolic blood pressure, or patients on loop diuretics may be at increased risk for volume depletion or hypotension. Before initiating SEGLUROMET in patients with one or more of these characteristics, assess volume status and renal function. In patients with volume depletion, correct this condition before initiating SEGLUROMET. Monitor for signs and symptoms of volume depletion, and renal function after initiating therapy.
5.5Urosepsis and Pyelonephritis
There have been postmarketing reports of serious urinary tract infections, including urosepsis and pyelonephritis, requiring hospitalization in patients receiving medicines containing SGLT2 inhibitors. Treatment with medicines containing SGLT2 inhibitors increases the risk for urinary tract infections. Evaluate patients for signs and symptoms of urinary tract infections and treat promptly, if indicated [see Adverse Reactions (6)].
5.6Hypoglycemia with Concomitant Use with Insulin and Insulin Secretagogues
Insulin and insulin secretagogues (e.g., sulfonylurea) are known to cause hypoglycemia. SEGLUROMET may increase the risk of hypoglycemia when used in combination with insulin and/or an insulin secretagogue [seeAdverse Reactions (6.1)]. Therefore, a lower dose of insulin or insulin secretagogue may be required to minimize the risk of hypoglycemia when used in combination with SEGLUROMET.
5.7Necrotizing Fasciitis of the Perineum (Fournier's Gangrene)
Reports of necrotizing fasciitis of the perineum (Fournier’s Gangrene), a rare but serious and life-threatening necrotizing infection requiring urgent surgical intervention, have been identified in postmarketing surveillance in patients with diabetes mellitus receiving SGLT2 inhibitors, including ertugliflozin. Cases have been reported in females and males. Serious outcomes have included hospitalization, multiple surgeries, and death.
Patients treated with SEGLUROMET presenting with pain or tenderness, erythema, or swelling in the genital or perineal area, along with fever or malaise, should be assessed for necrotizing fasciitis. If suspected, start treatment immediately with broad-spectrum antibiotics and, if necessary, surgical debridement. Discontinue SEGLUROMET, closely monitor blood glucose levels, and provide appropriate alternative therapy for glycemic control.
5.8Genital Mycotic Infections
Ertugliflozin increases the risk of genital mycotic infections. Patients who have a history of genital mycotic infections or who are uncircumcised are more likely to develop genital mycotic infections [seeAdverse Reactions (6.1)]. Monitor and treat appropriately.
5.9 Vitamin B Deficiency
In metformin clinical trials of 29-week duration, a decrease to subnormal levels of previously normal serum vitamin B12 levels was observed in approximately 7% of patients. Such decrease, possibly due to interference with B12 absorption from the B12-intrinsic factor complex, may be associated with anemia but appears to be rapidly reversible with discontinuation of metformin or vitamin B12 supplementation. Certain individuals (those with inadequate vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal vitamin B12 levels. Measure hematologic parameters on an annual basis and vitamin B12 at 2 to 3 year intervals in patients on metformin and manage any abnormalities [see Adverse Reactions (6.1)].
6 Adverse Reactions
The following important adverse reactions are described elsewhere in the labeling:
- Lactic Acidosis [seeBoxed WarningandWarnings and Precautions (5.1)]
- Diabetic Ketoacidosis in Patients with Type 1 Diabetes and Other Ketoacidosis [seeWarnings and Precautions (5.2)]
- Lower Limb Amputation [seeWarnings and Precautions (5.3)]
- Volume Depletion [seeWarnings and Precautions (5.4)]
- Urosepsis and Pyelonephritis [seeWarnings and Precautions (5.5)]
- Hypoglycemia with Concomitant Use with Insulin and Insulin Secretagogues [seeWarnings and Precautions (5.6)]
- Necrotizing Fasciitis of the Perineum (Fournier's Gangrene) [see Warnings and Precautions (5.7)]
- Genital Mycotic Infections [seeWarnings and Precautions (5.8)]
- Vitamin B12 Deficiency [seeWarnings and Precautions (5.9)]
- Most common adverse reactions associated with ertugliflozin (incidence ‚Č•5%) were female genital mycotic infections. (
6.1 )- Most common adverse reactions associated with metformin (incidence ‚Č•5%) were diarrhea, nausea, vomiting, flatulence, abdominal discomfort, indigestion, asthenia, and headache. (
6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme LLC at 1-877-888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
6.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Ertugliflozin and Metformin Hydrochloride
The incidence and type of adverse reactions in the two 26-week, placebo-controlled trials of ertugliflozin 5 mg and 15 mg added to metformin, representing a majority of data from the three 26-week, placebo-controlled trials, were similar to the adverse reactions described in Table 1.
Ertugliflozin
Metformin
The most common (5% or greater incidence) established adverse reactions due to initiation of metformin therapy are diarrhea, nausea, vomiting, flatulence, abdominal discomfort, indigestion, asthenia, and headache.
In controlled clinical trials of metformin of 29 weeks duration, a decrease to subnormal levels of previously normal serum vitamin B12 levels was observed in approximately 7% of patients.
Laboratory Tests
6.2Postmarketing Experience
Additional adverse reactions have been identified during post approval use. Because these reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Necrotizing fasciitis of the perineum (Fournier’s Gangrene)
- Angioedema
- Rash
- Cholestatic, hepatocellular, and mixed hepatocellular liver injury have been reported with postmarketing use of metformin.
7 Drug Interactions
Table 3: Clinically Significant Drug Interactions with SEGLUROMET Carbonic Anhydrase Inhibitors Clinical Impact: The risk of lactic acidosis may increase due to concomitant use of Topiramate or other carbonic anhydrase inhibitors (e.g., zonisamide, acetazolamide or dichlorphenamide) with metformin. These drugs frequently cause a decrease in serum bicarbonate and induce non-anion gap, hyperchloremic metabolic acidosis. Intervention: more frequent monitoring of these patients. Drugs that Reduce Metformin Clearance Clinical Impact: The risk of lactic acidosis may increase due to concomitant use of drugs that interfere with common renal tubular transport systems involved in the renal elimination of metformin (e.g., organic cationic transporter-2 [OCT2] / multidrug and toxin extrusion [MATE] inhibitors such as ranolazine, vandetanib, dolutegravir, and cimetidine) which increase systemic exposure to metformin Intervention Consider the benefits and risks of concomitant use. Alcohol Clinical Impact: Potentiate the effect of metformin on lactate metabolism. Intervention: Warn patients against excessive alcohol intake while receiving SEGLUROMET. Insulin and Insulin Secretagogues Clinical Impact: The risk of hypoglycemia when ertugliflozin is used in combination with insulin and/or an insulin secretagogue. Intervention: A lower dose of insulin or insulin secretagogue may be required to minimize the risk of hypoglycemia when used in combination with SEGLUROMET. Drugs that Affect Glycemic Control Clinical Impact: Certain drugs tend to produce hyperglycemia and may lead to loss of glycemic control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, calcium channel blocking drugs, and isoniazid. Intervention: When a patient is receiving SEGLUROMET along with such drugs, the patient should be closely observed to maintain adequate glycemic control. Lithium Clinical Impact: Concomitant use of an SGLT2 inhibitor with lithium may decrease serum lithium concentrations. Intervention: Monitor serum lithium concentration more frequently during SEGLUROMET initiation and dosage changes. Positive Urine Glucose Test Clinical Impact: SGLT2 inhibitors increase urinary glucose excretion and will lead to positive urine glucose tests. Intervention: Monitoring glycemic control with urine glucose tests is not recommended in patients taking SEGLUROMET. Use alternative methods to monitor glycemic control. Interference with 1,5-anhydroglucitol (1,5-AG) Assay Clinical Impact: Measurements of 1,5-AG are unreliable in assessing glycemic control in patients taking SGLT2 inhibitors. Intervention: Monitoring glycemic control with 1,5-AG assay is not recommended. Use alternative methods to monitor glycemic control.
- Carbonic Anhydrase Inhibitors: May increase risk of lactic acidosis. Consider more frequent monitoring. (
7.2 )- Drugs that Reduce Metformin Clearance: May increase risk of lactic acidosis. Consider benefits and risks of concomitant use. (
7.2 )- See full prescribing information for additional drug interactions and information on interference of SEGLUROMET with laboratory tests. (
7 )
8 Use In Specific Populations
- Pregnancy: Advise females of the potential risk to a fetus, especially during the second and third trimesters. (
8.1 )- Lactation: Breastfeeding not recommended. (
8.2 )- Females and Males of Reproductive Potential: Advise premenopausal females of the potential for an unintended pregnancy. (
8.3 )- Geriatrics: Higher incidence of adverse reactions related to reduced intravascular volume. (
8.5 )- Renal impairment: Higher incidence of adverse reactions related to reduced intravascular volume and renal function. (
8.6 )- Hepatic impairment : Avoid use in patients with hepatic impairment. (
8.7 )8.1 Pregnancy
Risk Summary
Based on animal data showing adverse renal effects, from ertugliflozin, SEGLUROMET is not recommended during the second and third trimesters of pregnancy. Published studies with metformin use during pregnancy have not reported a clear association with metformin and major birth defect or miscarriage risk (seeData).
The limited available data with SEGLUROMET in pregnant women are not sufficient to determine a drug-associated risk for major birth defects or miscarriage. There are risks to the mother and fetus associated with poorly controlled diabetes in pregnancy (seeClinical Considerations).
In animal studies, adverse renal changes were observed in rats when ertugliflozin was administered during a period of renal development corresponding to the late second and third trimesters of human pregnancy. Doses approximately 13 times the maximum clinical dose caused renal pelvic and tubule dilatations and renal mineralization that were not fully reversible. There was no evidence of fetal harm in rats or rabbits at exposures of ertugliflozin approximately 300 times higher than the maximal clinical dose of 15 mg/day when administered during organogenesis (seeData).
The estimated background risk of major birth defects is 6-10% in women with pre-gestational diabetes with a HbA1c >7 and has been reported to be as high as 20-25% in women with HbA1c >10. The estimated background risk of miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Poorly-controlled diabetes in pregnancy increases the maternal risk for diabetic ketoacidosis, pre-eclampsia, spontaneous abortions, preterm delivery, and delivery complications. Poorly controlled diabetes increases the fetal risk for major birth defects, stillbirth, and macrosomia related morbidity.
Data
Human Data
Published data from postmarketing studies have not reported a clear association with metformin and major birth defects, miscarriage, or adverse maternal or fetal outcomes when metformin was used during pregnancy. However, these studies cannot definitely establish the absence of any metformin-associated risk because of methodological limitations, including small sample size and inconsistent comparator groups.
Animal Data
8.2 Lactation
Risk Summary
There is no information regarding the presence of SEGLUROMET or ertugliflozin in human milk, the effects on the breastfed infant, or the effects on milk production. Limited published studies report that metformin is present in human milk (seeData). However, there is insufficient information on the effects of metformin on the breastfed infant and no available information on the effects of metformin on milk production. Ertugliflozin (seeData) and metformin are present in the milk of lactating rats. Since human kidney maturation occurs in utero and during the first 2 years of life when lactational exposure may occur, there may be risk to the developing human kidney, based on data with ertugliflozin. Because of the potential for serious adverse reactions in a breastfed infant, advise women that the use of SEGLUROMET is not recommended while breastfeeding.
Data
The lacteal excretion of radiolabeled ertugliflozin in lactating rats was evaluated 10 to 12 days after parturition. Ertugliflozin derived radioactivity exposure in milk and plasma were similar, with a milk/plasma ratio of 1.07, based on AUC. Juvenile rats directly exposed to ertugliflozin during a developmental period corresponding to human kidney maturation were associated with a risk to the developing kidney (persistent increased organ weight, renal mineralization, and renal pelvic and tubular dilatations).
Published clinical lactation studies report that metformin is present in human milk, which resulted in infant doses approximately 0.11% to 1% of the maternal weight-adjusted dosage and a milk/plasma ratio ranging between 0.13 and 1. However, the studies were not designed to definitely establish the risk of use of metformin during lactation because of small sample size and limited adverse event data collected in infants.
8.3 Females and Males of Reproductive Potential
Discuss the potential for unintended pregnancy with premenopausal women as therapy with metformin may result in ovulation in some anovulatory women.
8.4 Pediatric Use
Safety and effectiveness of SEGLUROMET in pediatric patients under 18 years of age have not been established.
8.5 Geriatric Use
SEGLUROMET
No dosage adjustment of SEGLUROMET is recommended based on age. Elderly patients are more likely to have decreased renal function. Because renal function abnormalities can occur after initiating ertugliflozin, and metformin is known to be substantially excreted by the kidneys, care should be taken in dose selection in the elderly. Assess renal function in elderly patients prior to initiating dosing and periodically thereafter [see Dosage and Administration (2.1) and Warnings and Precautions (5.1, 5.4)].
Ertugliflozin
In ertugliflozin clinical trials, a total of 876 (25.7%) patients treated with ertugliflozin were 65 years and older, and 152 (4.5%) patients treated with ertugliflozin were 75 years and older. Patients 65 years and older had a higher incidence of adverse reactions related to volume depletion compared to younger patients; events were reported in 1.1%, 2.2%, and 2.6% of patients treated with comparator, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively [see Warnings and Precautions (5.4) and Adverse Reactions (6.1)].
In VERTIS CV, a total of 2780 (50.5%) patients treated with ertugliflozin were 65 years and older, and 595 (10.8%) patients treated with ertugliflozin were 75 years and older. Safety and efficacy were generally similar for patients age 65 years and older compared to patients younger than 65.
Metformin HCl
Controlled clinical studies of metformin did not include sufficient numbers of elderly patients to determine whether they respond differently from younger patients, although other reported clinical experience has not identified differences in responses between the elderly and young patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy and the higher risk of lactic acidosis. Assess renal function more frequently in elderly patients [seeContraindications (4),Warnings and Precautions (5.1), andClinical Pharmacology (12.3)].
8.6Renal Impairment
A 26-week placebo-controlled study of 313 patients with Stage 3 Chronic Kidney Disease (eGFR ‚Č•30 to less than 60 mL/min/1.73 m2) treated with ertugliflozin did not have improvement in glycemic control.
In the VERTIS CV study, there were 1370 patients (25%) with an eGFR ‚Č•90 mL/min/1.73 m2, 2929 patients (53%) with an eGFR of ‚Č•60 to less than 90 mL/min/1.73 m2, 879 patients (16%) with an eGFR of ‚Č•45 to less than 60 mL/min/1.73 m2, and 299 patients (5%) with eGFR of 30 to <45 mL/min/1.73 m2 treated with ertugliflozin. Similar effects on glycemic control at Week 18 were observed in patients treated with ertugliflozin in each eGFR subgroup and also in the overall patient population.
SEGLUROMET is contraindicated in patients with severe renal impairment (eGFR less than 30 mL/min/1.73 m2), ESRD, or on dialysis [seeContraindications (4)].
No dosage adjustment is needed in patients with eGFR ‚Č•45 mL/min/1.73 m2.
Metformin is substantially excreted by the kidney, and the risk of metformin accumulation and lactic acidosis increases with the degree of renal impairment.
8.7Hepatic Impairment
Use of metformin in patients with hepatic impairment has been associated with some cases of lactic acidosis. SEGLUROMET is not recommended in patients with hepatic impairment [seeWarnings and Precautions (5.1)].
10 Overdosage
SEGLUROMET
In the event of an overdose with SEGLUROMET, contact the Poison Control Center. Employ the usual supportive measures as dictated by the patient's clinical status.
Ertugliflozin
Removal of ertugliflozin by hemodialysis has not been studied.
Metformin HCl
Overdose of metformin hydrochloride has occurred, including ingestion of amounts greater than 50 g (25 times the maximum recommended daily dose). Hypoglycemia was reported in approximately 10% of cases, but no causal association with metformin hydrochloride has been established. Lactic acidosis has been reported in approximately 32% of metformin overdose cases [seeWarnings and Precautions (5.1)]. Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Therefore, hemodialysis may be useful for removal of accumulated drug from patients in whom metformin overdosage is suspected.
11 Description
SEGLUROMET (ertugliflozin and metformin hydrochloride) tablet for oral use contains ertugliflozin L-pyroglutamic acid, a SGLT2 inhibitor, and metformin HCl, a member of the biguanide class.
Ertugliflozin
The chemical name of ertugliflozin L-pyroglutamic acid is (1S,2S,3S,4R,5S)-5-(4-chloro-3-(4-ethoxybenzyl)phenyl)-1-(hydroxymethyl)-6,8-dioxabicyclo[3.2.1]octane-2,3,4-triol, compound with (2S)-5-oxopyrrolidine-2-carboxylic acid. The molecular formula is C27H32ClNO10 and the molecular weight is 566.00.
The chemical structure is:
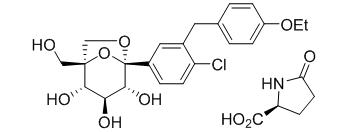
Ertugliflozin L-pyroglutamic acid is a white to off-white powder that is soluble in ethyl alcohol and acetone, slightly soluble in ethyl acetate and acetonitrile and very slightly soluble in water.
Metformin HCl
Metformin hydrochloride (N,N-dimethylimidodicarbonimidic diamide hydrochloride) is not chemically or pharmacologically related to any other classes of oral antihyperglycemic agents. The structural formula is as shown:
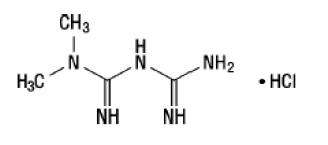
Metformin HCl is a white to off-white crystalline compound with a molecular formula of C4H11N5‚ąôHCl and a molecular weight of 165.63. Metformin hydrochloride is freely soluble in water and is practically insoluble in acetone, ether and chloroform. The pKa of metformin is 12.4. The pH of a 1% aqueous solution of metformin hydrochloride is 6.68.
SEGLUROMET is available as film-coated tablets containing:
- 3.24 mg ertugliflozin L-pyroglutamic acid equivalent to 2.5 mg of ertugliflozin and 500 mg metformin HCl (SEGLUROMET 2.5/500)
- 3.24 mg ertugliflozin L-pyroglutamic acid equivalent to 2.5 mg of ertugliflozin and 1,000 mg metformin HCl (SEGLUROMET 2.5/1000)
- 9.71 mg ertugliflozin L-pyroglutamic acid equivalent to 7.5 mg of ertugliflozin and 500 mg metformin HCl (SEGLUROMET 7.5/500)
- 9.71 mg ertugliflozin L-pyroglutamic acid equivalent to 7.5 mg of ertugliflozin and 1,000 mg metformin HCl (SEGLUROMET 7.5/1000)
Inactive ingredients are povidone, microcrystalline cellulose, crospovidone, sodium lauryl sulfate, and magnesium stearate.
The film coating contains: hypromellose, hydroxypropyl cellulose, titanium dioxide, iron oxide red, and carnauba wax.
12 Clinical Pharmacology
12.1 Mechanism of Action
SEGLUROMET
SEGLUROMET combines two antihyperglycemic agents with complementary mechanisms of action to improve glycemic control in patients with type 2 diabetes mellitus: ertugliflozin, a SGLT2 inhibitor, and metformin hydrochloride, a member of the biguanide class.
Ertugliflozin
SGLT2 is the predominant transporter responsible for reabsorption of glucose from the glomerular filtrate back into the circulation. Ertugliflozin is an inhibitor of SGLT2. By inhibiting SGLT2, ertugliflozin reduces renal reabsorption of filtered glucose and lowers the renal threshold for glucose, and thereby increases urinary glucose excretion.
Metformin HCl
Metformin is an antihyperglycemic agent which improves glucose tolerance in patients with type 2 diabetes mellitus, lowering both basal and postprandial plasma glucose. Its pharmacologic mechanisms of action are different from other classes of oral antihyperglycemic agents. Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. Metformin does not produce hypoglycemia in either patients with type 2 diabetes mellitus or normal subjects (except in special circumstances) [seeWarnings and Precautions (5.5)] and does not cause hyperinsulinemia. With metformin therapy, insulin secretion remains unchanged while fasting insulin levels and day-long plasma insulin response may actually decrease.
12.2 Pharmacodynamics
Ertugliflozin
Urinary Glucose Excretion and Urinary Volume
Dose-dependent increases in the amount of glucose excreted in urine were observed in healthy subjects and in patients with type 2 diabetes mellitus following single- and multiple-dose administration of ertugliflozin. Dose-response modeling indicates that ertugliflozin 5 mg and 15 mg result in near maximal urinary glucose excretion (UGE). Enhanced UGE is maintained after multiple-dose administration. UGE with ertugliflozin also results in increases in urinary volume.
Cardiac Electrophysiology
The effect of ertugliflozin on QTc interval was evaluated in a Phase 1 randomized, placebo- and positive-controlled 3-period crossover study in 42 healthy subjects. At 6.7 times the therapeutic exposures with maximum recommended dose, ertugliflozin does not prolong QTc to any clinically relevant extent.
12.3 Pharmacokinetics
General Introduction
Ertugliflozin
The pharmacokinetics of ertugliflozin are similar in healthy subjects and patients with type 2 diabetes mellitus. The steady state mean plasma AUC and Cmax were 398 ng‚ąôhr/mL and 81.3 ng/mL, respectively, with 5 mg ertugliflozin once-daily treatment, and 1,193 ng‚ąôhr/mL and 268 ng/mL, respectively, with 15 mg ertugliflozin once-daily treatment. Steady-state is reached after 4 to 6 days of once-daily dosing with ertugliflozin. Ertugliflozin does not exhibit time-dependent pharmacokinetics and accumulates in plasma up to 10-40% following multiple dosing.
Absorption
SEGLUROMET
The effects of a high-fat meal on the pharmacokinetics of ertugliflozin and metformin when administered as SEGLUROMET tablets are comparable to those reported for the individual tablets. Food had no meaningful effect on AUCinf of ertugliflozin and metformin, but reduced mean ertugliflozin Cmax by approximately 41% and metformin Cmax by approximately 29% compared to the fasted condition.
Ertugliflozin
Following single-dose oral administration of 5 mg and 15 mg of ertugliflozin, peak plasma concentrations of ertugliflozin occur at 1 hour postdose (median Tmax) under fasted conditions. Plasma Cmax and AUC of ertugliflozin increase in a dose-proportional manner following single doses from 0.5 mg (0.1 times the lowest recommended dose) to 300 mg (20 times the highest recommended dose) and following multiple doses from 1 mg (0.2 times the lowest recommended dose) to 100 mg (6.7 times the highest recommended dose). The absolute oral bioavailability of ertugliflozin following administration of a 15 mg dose is approximately 100%.
Metformin hydrochloride
The absolute bioavailability of a metformin HCl 500-mg tablet given under fasting conditions is approximately 50-60%. Studies using single oral doses of metformin hydrochloride tablets 500 mg to 1,500 mg, and 850 mg to 2,550 mg (approximately 1.3 times the maximum recommended daily dosage), indicate that there is a lack of dose proportionality with increasing doses, which is due to decreased absorption rather than an alternation in elimination. Food decreases the extent of and slightly delays the absorption of metformin, as shown by approximately a 40% lower mean peak plasma concentration (Cmax), a 25% lower area under the plasma concentration versus time curve (AUC), and a 35-minute prolongation of time to peak plasma concentration (Tmax) following administration of a single 850-mg tablet of metformin with food, compared to the same tablet strength administered fasting. The clinical relevance of these decreases is unknown.
Distribution
Ertugliflozin
The mean steady-state volume of distribution of ertugliflozin following an intravenous dose is 85.5 L. Plasma protein binding of ertugliflozin is 93.6% and is independent of ertugliflozin plasma concentrations. Plasma protein binding is not meaningfully altered in patients with renal or hepatic impairment. The blood-to-plasma concentration ratio of ertugliflozin is 0.66.
Metformin
The apparent volume of distribution (V/F) of metformin following single oral doses of metformin hydrochloride tablets 850 mg averaged 654 ¬Ī 358 L. Metformin is negligibly bound to plasma proteins, in contrast to sulfonylureas, which are more than 90% protein bound. Metformin partitions into erythrocytes, most likely as a function of time. At usual clinical doses and dosing schedules of metformin hydrochloride tablets, steady-state plasma concentrations of metformin are reached within 24-48 hours and are generally <1 mcg/mL. During controlled clinical trials of metformin, maximum metformin plasma levels did not exceed 5 mcg/mL, even at maximum doses.
Elimination
Metabolism
Excretion
Ertugliflozin
The mean systemic plasma clearance following an intravenous 100 ¬Ķg dose was 11.2 L/hr. The mean elimination half-life in type 2 diabetic patients with normal renal function was estimated to be 16.6 hours based on the population pharmacokinetic analysis. Following administration of an oral [14C]-ertugliflozin solution to healthy subjects, approximately 40.9% and 50.2% of the drug-related radioactivity was eliminated in feces and urine, respectively. Only 1.5% of the administered dose was excreted as unchanged ertugliflozin in urine and 33.8% as unchanged ertugliflozin in feces, which is likely due to biliary excretion of glucuronide metabolites and subsequent hydrolysis to parent.
Metformin
Renal clearance is approximately 3.5 times greater than creatinine clearance, which indicates that tubular secretion is the major route of metformin elimination. Following oral administration, approximately 90% of the absorbed drug is eliminated via the renal route within the first 24 hours, with a plasma elimination half-life of approximately 6.2 hours. In blood, the elimination half-life is approximately 17.6 hours, suggesting that the erythrocyte mass may be a compartment of distribution.
Specific Populations
Patients with Renal Impairment
Patients with Hepatic Impairment
Effects of Age, Body Weight, Gender, and Race
Drug Interaction Studies
SEGLUROMET
Coadministration of single dose of ertugliflozin (15 mg) and metformin (1,000 mg) did not meaningfully alter the pharmacokinetics of either ertugliflozin or metformin in healthy subjects.
Pharmacokinetic drug interaction studies with SEGLUROMET have not been performed; however, such studies have been conducted with ertugliflozin and metformin, the individual components of SEGLUROMET.
Ertugliflozin
Metformin hydrochloride
Table 4: Effect of Metformin HCl on Systemic Exposure of Coadministered Drugs Coadministered Drug Dose of Coadministered Drug All doses administered as single dose unless otherwise specified. Dose of Metformin HCl Geometric Mean Ratio(ratio with/without metformin)No Effect = 1.00 AUC AUC is reported as AUC0-‚ąě unless otherwise specified. Cmax No dosing adjustments required for the following: Cimetidine 400 mg 850 mg Cimetidine 0.95 AUC0-24hr. 1.01 Glyburide 5 mg 500 mg Metformin HCl extended-release tablets 500 mg. Glyburide 0.78 Ratio of arithmetic means, p value of difference <0.05. 0.63 Furosemide 40 mg 850 mg Furosemide 0.87 0.69 Nifedipine 10 mg 850 mg Nifedipine 1.10 1.08 Propranolol 40 mg 850 mg Propranolol 1.01 0.94 Ibuprofen 400 mg 850 mg Ibuprofen 0.97 Ratio of arithmetic means. 1.01
Table 5: Effect of Coadministered Drugs on Systemic Exposure of Metformin HCl Coadministered Drug Dose of Coadministered Drug All doses administered as single dose unless otherwise specified. Dose of Metformin HCl Geometric Mean Ratio(ratio with/without coadministered drug)No Effect = 1.00 AUC AUC is reported as AUC0-‚ąě unless otherwise specified. Cmax No dosing adjustments required for the following: Glyburide 5 mg 500 mg Metformin hydrochloride extended-release tablets 500 mg. Metformin 0.98 Ratio of arithmetic means. 0.99 Furosemide 40 mg 850 mg Metformin 1.09 1.22 Nifedipine 10 mg 850 mg Metformin 1.16 1.21 Propranolol 40 mg 850 mg Metformin 0.90 0.94 Ibuprofen 400 mg 850 mg Metformin 1.05 1.07 Drugs that are eliminated by renal tubular secretion may increase the accumulation of metformin [seeWarnings and Precautions (5.1)andDrug Interactions (7.2)]. Cimetidine 400 mg 850 mg Metformin 1.40 1.61 Carbonic anhydrase inhibitors may cause metabolic acidosis [seeWarnings and Precautions (5.1)andDrug Interactions (7.2)]. Topiramate 100 mg Steady-state 100 mg topiramate every 12 hr + metformin 500 mg every 12 hr AUC = AUC0-12hr. 500 mg Metformin 1.25 1.17
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Ertugliflozin
Carcinogenicity was evaluated in CD-1 mice and Sprague-Dawley rats. In the mouse study, ertugliflozin was administered by oral gavage at doses of 5, 15, and 40 mg/kg/day for up to 97 weeks in males and 102 weeks in females. There were no ertugliflozin-related neoplastic findings at doses up to 40 mg/kg/day (approximately 50 times human exposure at the maximum recommended human dose [MRHD] of 15 mg/day based on AUC). In the rat study, ertugliflozin was administered by oral gavage at doses of 1.5, 5, and 15 mg/kg/day for up to 92 weeks in females and 104 weeks in males. Ertugliflozin-related neoplastic findings included an increased incidence of adrenal medullary pheochromocytoma (PCC) in male rats at 15 mg/kg/day. Although the molecular mechanism remains unknown, this finding may be related to carbohydrate malabsorption leading to altered calcium homeostasis, which has been associated with PCC development in rats and has unclear relevancy to human risk. The no-observed-effect level (NOEL) for neoplasia was 5 mg/kg/day (approximately 16 times human exposure at the MRHD of 15 mg/day, based on AUC).
Metformin HCl
Long-term carcinogenicity studies have been performed in rats (dosing duration of 104 weeks) and mice (dosing duration of 91 weeks) at doses up to and including 900 mg/kg/day and 1,500 mg/kg/day, respectively. These doses are both approximately four times the maximum recommended human daily dose of 2,000 mg based on body surface area comparisons. No evidence of carcinogenicity with metformin was found in either male or female mice. Similarly, there was no tumorigenic potential observed with metformin in male rats. There was, however, an increased incidence of benign stromal uterine polyps in female rats treated with 900 mg/kg/day.
Mutagenesis
Ertugliflozin
Ertugliflozin was not mutagenic or clastogenic with or without metabolic activation in the microbial reverse mutation, in vitro cytogenetic (human lymphocytes), and in vivo rat micronucleus assays.
Metformin
There was no evidence of a mutagenic potential of metformin in the following in vitro tests: Ames test (S. typhimurium), gene mutation test (mouse lymphoma cells), or chromosomal aberrations test (human lymphocytes). Results in the in vivo mouse micronucleus test were also negative.
Impairment of Fertility
Ertugliflozin
In the rat fertility and embryonic development study, male and female rats were administered ertugliflozin at 5, 25, and 250 mg/kg/day. No effects on fertility were observed at 250 mg/kg/day (approximately 480 and 570 times male and female human exposures, respectively, at the MRHD of 15 mg/day based on AUC comparison).
Metformin HCl
Fertility of male or female rats was unaffected by metformin when administered at doses as high as 600 mg/kg/day, which is approximately three times the maximum recommended human daily dose based on body surface area comparisons.
14 Clinical Studies
14.1Glycemic Control Trials in Patients with Type 2 Diabetes Mellitus
The efficacy and safety of ertugliflozin in combination with metformin have been studied in 4 multicenter, randomized, double-blind, placebo- and active comparator-controlled, clinical studies involving 3,643 patients with type 2 diabetes mellitus. These studies included White, Hispanic, Black, Asian, and other racial and ethnic groups, and patients with an age range of 21 to 86 years.
In VERTIS CV, ertugliflozin has been studied as add on to insulin (with or without metformin) and as add on to metformin plus a sulfonylurea in substudies.
In patients with type 2 diabetes mellitus, treatment with ertugliflozin in combination with metformin reduced hemoglobin A1c (HbA1c) compared to placebo.
In patients with type 2 diabetes mellitus treated with ertugliflozin in combination with metformin, the reduction in HbA1c was generally similar across subgroups defined by age, sex, race, geographic region, baseline body mass index (BMI), and duration of type 2 diabetes mellitus.
Ertugliflozin as Add-on Combination Therapy with Metformin
A total of 621 patients with type 2 diabetes mellitus inadequately controlled (HbA1c between 7% and 10.5%) on metformin monotherapy (‚Č•1,500 mg/day for ‚Č•8 weeks) participated in a randomized, double-blind, multi-center, 26-week, placebo-controlled study (NCT02033889) to evaluate the efficacy and safety of ertugliflozin in combination with metformin. Patients entered a 2-week, single-blind, placebo run-in, and were randomized to placebo, ertugliflozin 5 mg, or ertugliflozin 15 mg administered once daily in addition to continuation of background metformin therapy.
At Week 26, statistically significant reductions in HbA1c were observed in the ertugliflozin 5 mg and 15 mg groups compared to placebo. Ertugliflozin also resulted in a greater proportion of patients achieving an HbA1c <7% compared to placebo (seeTable 6andFigure 3).
Table 6: Results at Week 26 from a Placebo-Controlled Study for Ertugliflozin Used in Combination with Metformin in Patients with Type 2 Diabetes Mellitus N includes all randomized and treated patients with a baseline measurement of the outcome variable. At Week 26, the primary HbA1c endpoint was missing for 12%, 6%, and 9% of patients, and during the trial, rescue medication was initiated by 18%, 3%, and 1% of patients randomized to placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Missing Week 26 measurements were imputed using multiple imputation with a mean equal to the baseline value of the patient. Results include measurements collected after initiation of rescue medication. For those patients who did not receive rescue medication and had values measured at 26 weeks, the mean changes from baseline for HbA1c were -0.2%, -0.7%, and -1.0% for placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Placebo Ertugliflozin 5 mg Ertugliflozin 15 mg HbA1c (%) N = 207 N = 205 N = 201   Baseline (mean) 8.2 8.1 8.1   Change from baseline (LS mean Intent-to-treat analysis using ANCOVA adjusted for baseline value, prior antihyperglycemic medication, menopausal status and baseline eGFR. )-0.2 -0.7 -0.9   Difference from placebo (LS mean , 95% CI) -0.5 p<0.001 compared to placebo. (-0.7, -0.4)-0.7 (-0.9, -0.5) Patients [N (%)] with HbA1c <7% 38 (18.4) 74 (36.3) 87 (43.3) FPG (mg/dL) N = 202 N = 199 N = 201   Baseline (mean) 169.1 168.1 167.9   Change from baseline (LS mean ) -8.7 -30.3 -40.9   Difference from placebo (LS mean , 95% CI) -21.6 (-27.8, -15.5) -32.3 (-38.5, -26.0)
The mean baseline body weight was 84.5 kg, 84.9 kg, and 85.3 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 26 were-1.4 kg, -3.2 kg, and -3.0 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The difference from placebo (95% CI) for ertugliflozin 5 mg was -1.8 kg (-2.4, -1.2) and for ertugliflozin 15 mg was -1.7 kg (-2.2, -1.1).
The mean baseline systolic blood pressure was 129.3 mmHg, 130.5 mmHg, and 130.2 mmHg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 26 were -1.8 mmHg, -5.1 mmHg, and -5.7 mmHg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The difference from placebo (95% CI) for ertugliflozin 5 mg was -3.3 mmHg (-5.6, -1.1) and for ertugliflozin 15 mg was -3.8 mmHg (-6.1, -1.5).
Figure 3: HbA1c (%) Change over Time in a 26-Week Placebo-Controlled Study for Ertugliflozin Used in Combination with Metformin in Patients with Type 2 Diabetes Mellitus Data to the left of the vertical line are observed means (non-model-based) excluding values occurring post glycemic rescue. Data to the right of the vertical line represent the final Week 26 data, including all values regardless of use of glycemic rescue medication and use of study drug, with missing Week 26 values imputed using multiple imputation (26-MI) with a mean equal to the baseline value of the patient (seeTable 6). 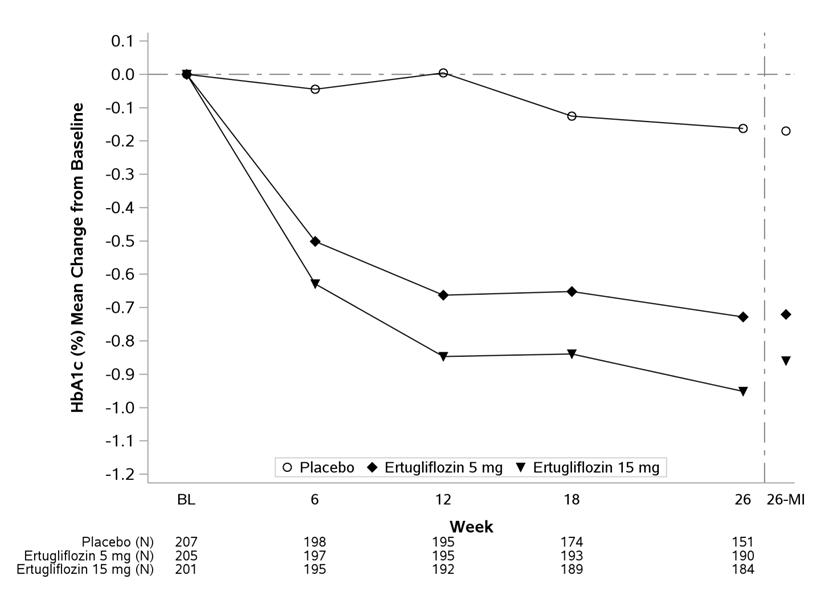
In Combination with Sitagliptin versus Ertugliflozin Alone and Sitagliptin Alone, as Add-on to Metformin
A total of 1,233 patients with type 2 diabetes mellitus with inadequate glycemic control (HbA1c between 7.5% and 11%) on metformin monotherapy (‚Č•1,500 mg/day for ‚Č•8 weeks) participated in a randomized, double-blind, 26-week, active controlled study (NCT02099110) to evaluate the efficacy and safety of ertugliflozin 5 mg or 15 mg in combination with sitagliptin 100 mg compared to the individual components. Patients were randomized to one of five treatment arms: ertugliflozin 5 mg, ertugliflozin 15 mg, sitagliptin 100 mg, ertugliflozin 5 mg + sitagliptin 100 mg, or ertugliflozin 15 mg + sitagliptin 100 mg.
At Week 26, ertugliflozin 5 mg or 15 mg + sitagliptin 100 mg provided statistically significantly greater reductions in HbA1c compared to ertugliflozin (5 mg or 15 mg) alone or sitagliptin 100 mg alone. The mean change from baseline in HbA1c was -1.4% for ertugliflozin 5 mg or 15 mg + sitagliptin 100 mg versus -1.0%, for ertugliflozin 5 mg, ertugliflozin 15 mg, or sitagliptin 100 mg, respectively. More patients receiving ertugliflozin 5 mg or 15 mg + sitagliptin 100 mg achieved an HbA1c <7% (53.3% and 50.9%, for ertugliflozin 5 mg or 15 mg, respectively, + sitagliptin 100 mg) compared to the individual components (29.3%, 33.7%, and 38.5% for ertugliflozin 5 mg, ertugliflozin 15 mg, or sitagliptin 100 mg, respectively).
Ertugliflozin as Add-on Combination Therapy with Metformin and Sitagliptin
A total of 463 patients with type 2 diabetes mellitus inadequately controlled (HbA1c between 7% and 10.5%) on metformin (‚Č•1,500 mg/day for ‚Č•8 weeks) and sitagliptin 100 mg once daily participated in a randomized, double-blind, multi-center, 26-week, placebo-controlled study (NCT02036515) to evaluate the efficacy and safety of ertugliflozin. Patients entered a 2-week, single-blind, placebo run-in period and were randomized to placebo, ertugliflozin 5 mg, or ertugliflozin 15 mg.
At Week 26, treatment with ertugliflozin at 5 mg or 15 mg daily provided statistically significant reductions in HbA1c. Ertugliflozin also resulted in a higher proportion of patients achieving an HbA1c <7% compared to placebo (seeTable 7).
Table 7: Results at Week 26 from an Add-on Study of Ertugliflozin in Combination with Metformin and Sitagliptin in Patients with Type 2 Diabetes Mellitus N includes all randomized and treated patients with a baseline measurement of the outcome variable. At Week 26, the primary HbA1c endpoint was missing for 10%, 11%, and 7% of patients and during the trial, rescue medication was initiated by 16%, 1%, and 2% of patients randomized to placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Missing Week 26 measurements were imputed using multiple imputation with a mean equal to the baseline value of the patient. Results include measurements collected after initiation of rescue medication. For those patients who did not receive rescue medication and had values measured at 26 weeks, the mean changes from baseline for HbA1c were -0.2%, -0.8%, and -0.9% for placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Placebo Ertugliflozin 5 mg Ertugliflozin 15 mg HbA1c (%) N = 152 N = 155 N = 152   Baseline (mean) 8.0 8.1 8.0   Change from baseline (LS mean Intent-to-treat analysis using ANCOVA adjusted for baseline value, prior antihyperglycemic medication and baseline eGFR. )-0.2 -0.7 -0.8   Difference from placebo (LS mean , 95% CI) -0.5 p<0.001 compared to placebo. (-0.7, -0.3)-0.6 (-0.8, -0.4) Patients [N (%)] with HbA1c <7% 31 (20.2) 54 (34.6) 64 (42.3) FPG (mg/dL) N = 152 N = 156 N = 152   Baseline (mean) 169.6 167.7 171.7   Change from baseline (LS mean ) -6.5 -25.7 -32.1   Difference from placebo (LS mean , 95% CI) -19.2 (-26.8, -11.6) -25.6 (-33.2, -18.0)
The mean baseline body weight was 86.5 kg, 87.6 kg, and 86.6 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 26 were -1.0 kg, -3.0 kg, and -2.8 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The difference from placebo (95% CI) for ertugliflozin 5 mg was -1.9 kg (-2.6, -1.3) and for ertugliflozin 15 mg was -1.8 kg (-2.4, -1.2).
The mean baseline systolic blood pressure was 130.2 mmHg, 132.1 mmHg, and 131.6 mmHg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 26 were -0.2 mmHg, -3.8 mmHg, and -4.5 mmHg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The difference from placebo (95% CI) for ertugliflozin 5 mg was -3.7 mmHg (-6.1, -1.2) and for ertugliflozin 15 mg was -4.3 mmHg (-6.7, -1.9).
Active Controlled Study of Ertugliflozin Versus Glimepiride as Add-on Combination Therapy with Metformin
A total of 1,326 patients with type 2 diabetes mellitus inadequately controlled (HbA1c between 7% and 9%) on metformin monotherapy participated in a randomized, double-blind, multi-center, 52-week, active comparator-controlled study (NCT01999218) to evaluate the efficacy and safety of ertugliflozin in combination with metformin. These patients, who were receiving metformin monotherapy (‚Č•1,500 mg/day for ‚Č•8 weeks), entered a 2-week, single-blind, placebo run-in period and were randomized to glimepiride, ertugliflozin 5 mg, or ertugliflozin 15 mg administered once daily in addition to continuation of background metformin therapy. Glimepiride was initiated at 1 mg/day and titrated up to a maximum dose of 6 or 8 mg/day (depending on maximum approved dose in each country) or a maximum tolerated dose or down-titrated to avoid or manage hypoglycemia. The mean daily dose of glimepiride was 3.0 mg.
Ertugliflozin 15 mg was non-inferior to glimepiride after 52 weeks of treatment. (SeeTable 8.)
Table 8: Results at Week 52 from an Active-Controlled Study Comparing Ertugliflozin to Glimepiride as Add-on Therapy in Patients with Type 2 Diabetes Mellitus Inadequately Controlled on Metformin N includes all randomized and treated patients with a baseline measurement of the outcome variable. At Week 52, the primary HbA1c endpoint was missing for 15%, 20%, and 16% of patients and during the trial, rescue medication was initiated by 3%, 6%, and 4% of patients randomized to glimepiride, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Missing Week 52 measurements were imputed using multiple imputation with a mean equal to the baseline value of the patient. Results include measurements collected after initiation of rescue medication. For those patients who did not receive rescue medication and had values measured at 52 weeks, the mean changes from baseline for HbA1c were -0.8%, -0.6%, and -0.7% for glimepiride, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Glimepiride Ertugliflozin 5 mg Ertugliflozin 15 mg HbA1c (%) N = 437 N = 447 N = 440   Baseline (mean) 7.8 7.8 7.8   Change from baseline (LS mean Intent-to-treat analysis using ANCOVA adjusted for baseline value, prior antihyperglycemic medication and baseline eGFR. )-0.6 -0.5 -0.5   Difference from glimepiride (LS mean , 95% CI) 0.2 Non-inferiority is declared when the upper bound of the two-sided 95% confidence interval (CI) for the mean difference is less than 0.3%. (0.0, 0.3)0.1 (-0.0, 0.2) Patients [N (%)] with HbA1c <7% 208 (47.7) 177 (39.5) 186 (42.2)
The mean baseline body weight was 86.8 kg, 87.9 kg, and 85.6 kg in the glimepiride, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 52 were 0.6 kg, -2.6 kg, and -3.0 kg in the glimepiride, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The difference from glimepiride (95% CI) for ertugliflozin 5 mg was -3.2 kg (-3.7, -2.7) and for ertugliflozin 15 mg was -3.6 kg (-4.1, -3.1).
Ertugliflozin as Add-on Combination Therapy with Insulin (With or Without Metformin)
In an 18-week randomized, double-blind, multi-center, placebo-controlled, glycemic sub-study of VERTIS CV (NCT01986881, study details see 14.2), a total of 1065 patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease with inadequate glycemic control (HbA1c between 7% and 10.5%) on background therapy of insulin ‚Č•20 units/day (59% also on metformin ‚Č•1,500 mg/day) were randomized to placebo, ertugliflozin 5 mg or ertugliflozin 15 mg once daily treatment.
At Week 18, treatment with ertugliflozin at 5 mg or 15 mg daily provided statistically significant reductions in HbA1c compared to placebo (see Table 9).
Table 9: Results at Week 18 from an Add-on Study of Ertugliflozin in Combination with Insulin (with or without Metformin) in Patients with Type 2 Diabetes Mellitus N includes all randomized and treated patients with a baseline measurement of the outcome variable. At Week 18, the primary HbA1c endpoint was missing for 10%, 9%, and 12% of patients and during the trial, rescue medication was initiated by 12%, 7%, and 6% of patients randomized to placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Results include measurements collected after initiation of rescue medication. Prior to Week 18, background antidiabetic medication was held stable. Missing Week 18 measurements were imputed using multiple imputation with a mean equal to the baseline value of the patient (Return to Baseline analysis). Placebo Ertugliflozin 5 mg Ertugliflozin 15 mg SE: standard error. HbA1c (%) N = 346 N = 346 N = 367   Baseline (mean) 8.4 8.4 8.4   Change from baseline (LS mean Intent-to-treat analysis using ANCOVA adjusted for baseline value, insulin stratum, and baseline eGFR. , SE)-0.2 (0.05) -0.7 (0.05) -0.7 (0.05)   Difference from placebo (LS mean , 95% CI) -0.5 p<0.001 compared to placebo. (-0.6, -0.4)-0.5 (-0.7, -0.4) Patients [N (%)] with HbA1c <7% Missing values imputed as not meeting the <7% criterion. 37 (10.7) 79 (22.8) 81 (22.1) FPG (mg/dL) N = 343 N = 346 N = 368   Baseline (mean) 167.4 173.8 175.4   Change from baseline (LS mean , SE) -6.3 (2.91) -25.6 (2.90) -29.8 (2.86)   Difference from placebo (LS mean , 95% CI) -19.2 (-26.8, -11.6) -23.4 (-30.9, -16.0)
The mean baseline body weights were 93.3 kg, 93.8 kg, and 92.1 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 18 were -0.2 kg, - 1.6 kg, and -1.9 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The differences from placebo (95% CI) for ertugliflozin 5 mg were - 1.4 kg (- 1.9, - 0.9) and for ertugliflozin 15 mg was -1.6 kg (-2.1, -1.1).
The mean baseline systolic blood pressures were 134.0 mmHg, 135.6 mmHg, and 133.7 mmHg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 18 were 0.7 mmHg, -2.2 mmHg, and -1.7 mmHg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The differences from placebo (95% CI) for ertugliflozin 5 mg was ‚Äď 2.9 mmHg (-4.9, -1.0) and for ertugliflozin 15 mg were -2.5 mmHg (- 4.4, - 0.5).
Add-on Combination Therapy with Metformin and Sulfonylurea
In an 18-week randomized, double-blind, multi-center, placebo-controlled, glycemic sub-study of VERTIS CV (NCT01986881, study details see 14.2), a total of 330 patients with type 2 diabetes mellitus and established atherosclerotic cardiovascular disease with inadequate glycemic control (HbA1c between 7% and 10.5%) with background therapy of metformin ‚Č•1,500 mg/day and a sulfonylurea (SU) were randomized to placebo, ertugliflozin 5 mg or ertugliflozin 15 mg once daily treatment.
At Week 18, treatment with ertugliflozin at 5 mg or 15 mg daily provided statistically significant reductions in HbA1c compared to placebo (see Table 10).
Table 10: Results at Week 18 from an Add-on Study of Ertugliflozin in Combination with Metformin and a SU in Patients with Type 2 Diabetes Mellitus N includes all randomized and treated patients with a baseline measurement of the outcome variable. At Week 18, the primary HbA1c endpoint was missing for 9%, 8%, and 6% of patients and during the trial, rescue medication was initiated by 10%, 7%, and 3% of patients randomized to placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg, respectively. Results include measurements collected after initiation of rescue medication. Missing Week 18 measurements were imputed using multiple imputation with a mean equal to the baseline value of the patient (Return to Baseline analysis). Placebo Ertugliflozin 5 mg Ertugliflozin 15 mg SE: standard error HbA1c (%) N = 116 N = 99 N = 113   Baseline (mean) 8.3 8.4 8.3   Change from baseline (LS mean Intent-to-treat analysis using ANCOVA adjusted for baseline value and baseline eGFR. , SE)-0.3 (0.08) -0.8 (0.09) -0.9 (0.08)   Difference from placebo (LS mean , 95% CI) -0.6 p<0.001 compared to placebo. (-0.8, -0.3)-0.7 (-0.9, -0.4) Patients [N (%)] with HbA1c <7% Missing values imputed as not meeting the <7% criterion. 17 (14.7) 39 (39.4) 38 (33.6) FPG (mg/dL) N = 117 N = 99 N = 113   Baseline (mean) 177.3 183.5 174.0   Change from baseline (LS mean , SE) -3.5 (3.65) -31.3 (3.87) -33.0 (3.67)   Difference from placebo (LS mean , 95% CI) -27.9 (-37.8, -17.9) -29.5 (-39.0, -19.9)
The mean baseline body weights were 90.5 kg, 92.1 kg, and 92.9 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The mean changes from baseline to Week 18 were - 0.6 kg, -2.0 kg, and - 2.2 kg in the placebo, ertugliflozin 5 mg, and ertugliflozin 15 mg groups, respectively. The differences from placebo (95% CI) for ertugliflozin 5 mg were - 1.4 kg (- 2.2, - 0.7) and for ertugliflozin 15 mg was - 1.6 kg (- 2.3, - 0.9).
14.2 Ertugliflozin Cardiovascular Outcomes in Patients with Type 2 Diabetes and Established Cardiovascular Disease
The effect of ertugliflozin on cardiovascular risk in adult patients with type 2 diabetes and established atherosclerotic cardiovascular disease was evaluated in the VERTIS CV study (NCT 01986881), a multicenter, multi-national, randomized, double-blind, placebo-controlled, event-driven trial. The study compared the risk of experiencing a major adverse cardiovascular event (MACE) between ertugliflozin and placebo when these were added to and used concomitantly with standard of care treatments for diabetes and atherosclerotic cardiovascular disease.
A total of 8246 patients were randomized (placebo N=2747, ertugliflozin 5 mg N=2752, ertugliflozin 15 mg N=2747) and followed for a median of 3 years. Approximately 88% of the study population was Caucasian, 6% Asian, and 3% Black. The mean age was 64 years and approximately 70% were male.
All patients in the study had inadequately controlled type 2 diabetes mellitus at baseline (HbA1c greater than or equal to 7%). The mean duration of type 2 diabetes mellitus was 13 years, the mean HbA1c at baseline was 8.2% and the mean eGFR was 76 mL/min/1.73 m2. At baseline, patients were treated with one (32%) or more (67%) antidiabetic medications including biguanides (metformin) (76%), insulin (47%), sulfonylureas (41%), DPP-4 inhibitors (11%) and GLP-1 receptor agonists (3%).
Almost all patients (99%) had established atherosclerotic cardiovascular disease at baseline including: a documented history of coronary artery disease (76%), cerebrovascular disease (23%) or peripheral artery disease (19%). Approximately 24% patients had a history of heart failure (HF). At baseline, the mean systolic blood pressure was 133 mmHg, the mean diastolic blood pressure was 77 mmHg, the mean LDL was 89 mg/dL, and the mean HDL was 44 mg/dL. At baseline, approximately 81% of patients were treated with renin angiotensin system inhibitors, 69% with beta-blockers, 43% with diuretics, 82% with statins, 4% ezetimibe, and 89% with antiplatelet agents.
The primary endpoint in VERTIS CV was the time to first occurrence of a Major Adverse Cardiac Event (MACE). A major adverse cardiovascular event was defined as occurrence of either a cardiovascular death or a nonfatal myocardial infarction (MI) or a nonfatal stroke. The statistical analysis plan pre-specified that the 5 and 15 mg doses would be combined for the analysis. A Cox proportional hazards model was used to test for non-inferiority against the pre-specified risk margin of 1.3 for the hazard ratio of MACE. Type-1 error was controlled across multiple tests using a hierarchical testing strategy.
The incidence rate of MACE was similar between the ertugliflozin-treated and placebo-treated patients. The estimated hazard ratio of MACE associated with ertugliflozin relative to placebo was 0.97 with 95.6% confidence interval (0.85, 1.11). The upper bound of this confidence interval excluded a risk larger than 1.3 (Table 11). Results for the 5 mg and 15 mg doses were consistent with results for the combined dose group.
Table 11: Analysis of MACE and its Components from the VERTIS-CV Study Intent-to-treat analysis set. Endpoint MACE was evaluated in subjects who took at least one dose of study medication and, for subjects who discontinued study medication prior to the end of the study, censored events that occurred more than 365 days after the last dose of study medication. Other endpoints were evaluated using all randomized subjects and events that occurred any time after the first dose of study medication until the last contact date. The total number of first events was analyzed for each endpoint. Placebo (N=2747) ertugliflozin (N=5499) Hazard Ratio vs Placebo (CI) HR and CI are based on Cox proportional hazards regression model, stratified by cohorts. For MACE a 95.6% CI is presented, for other endpoints a 95% CI is presented. N (%) Event Rate (per 100 person-years) N (%) Event Rate (per 100 person-years) N=Number of patients, CI=Confidence interval, CV=Cardiovascular, MI=Myocardial infarction. MACE (CV death, non-fatal MI, or non-fatal stroke) Composite 327 (11.9) 4.0 653 (11.9) 3.9 0.97(0.85, 1.11) Components of Composite Endpoint Non-fatal MI 148 (5.4) 1.6 310 (5.6) 1.7 1.04(0.86, 1.27) Non-fatal Stroke 78 (2.8) 0.8 157 (2.9) 0.8 1.00(0.76, 1.32) CV death 184 (6.7) 1.9 341 (6.2) 1.8 0.92(0.77, 1.11)
16 How Supplied/storage And Handling
SEGLUROMET (ertugliflozin and metformin hydrochloride) tablets are available as follows:
¬†Strength ¬†Description ¬†How Supplied ¬†NDC ertugliflozin 2.5 mg and metformin hydrochloride 500 mg tablets pink, oval, debossed with ‚Äú2.5/500‚ÄĚ on one side and plain on the other side unit-of-use bottles of 60 0006-5369-03 unit-of-use bottles of 180 0006-5369-06 ertugliflozin 2.5 mg and metformin hydrochloride 1,000 mg tablets pink, oval, debossed with ‚Äú2.5/1000‚ÄĚ on one side and plain on the other side unit-of-use bottles of 60 0006-5373-03 unit-of-use bottles of 180 0006-5373-06 ertugliflozin 7.5 mg and metformin hydrochloride 500 mg tablets red, oval, debossed with ‚Äú7.5/500‚ÄĚ on one side and plain on the other side unit-of-use bottles of 60 0006-5370-03 unit-of-use bottles of 180 0006-5370-06 ertugliflozin 7.5 mg and metformin hydrochloride 1,000 mg tablets red, oval, debossed with ‚Äú7.5/1000‚ÄĚ on one side and plain on the other side unit-of-use bottles of 60 0006-5374-03 unit-of-use bottles of 180 0006-5374-06 STORAGE AND HANDLING SECTION
Store at 20¬įC-25¬įC (68¬įF-77¬įF), excursions permitted between 15¬įC-30¬įC (between 59¬įF-86¬įF) [see USP Controlled Room Temperature]. Protect from moisture. Store in a dry place.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Lactic Acidosis
Inform patients of the risks of lactic acidosis due to the metformin component, its symptoms, and conditions that predispose to its development [seeWarnings and Precautions (5.1)]. Advise patients to discontinue SEGLUROMET immediately and to notify their doctor promptly if unexplained hyperventilation, malaise, myalgia, unusual somnolence, slow or irregular heartbeat, sensation of feeling cold (especially in the extremities), or other nonspecific symptoms occur. GI symptoms are common during initiation of metformin treatment and may occur during initiation of SEGLUROMET therapy; however, advise patients to consult their doctor if they develop unexplained symptoms. Although GI symptoms that occur after stabilization are unlikely to be drug related, such an occurrence of symptoms should be evaluated to determine if it may be due to metformin-induced lactic acidosis or other serious disease.
Diabetic Ketoacidosis in Patients with Type 1 Diabetes Mellitus and Other Ketoacidosis
Inform patients that SEGLUROMET can cause potentially fatal ketoacidosis and that type 2 diabetes mellitus and pancreatic disorders (e.g., history of pancreatitis or pancreatic surgery) are risk factors.
Educate all patients on precipitating factors (such as insulin dose reduction or missed insulin doses, infection, reduced caloric intake, ketogenic diet, surgery, dehydration, and alcohol abuse) and symptoms of ketoacidosis (including nausea, vomiting, abdominal pain, tiredness, and labored breathing). Inform patients that blood glucose may be normal even in the presence of ketoacidosis.
Advise patients that they may be asked to monitor ketones. If symptoms of ketoacidosis occur, instruct patients to discontinue SEGLUROMET and seek medical attention immediately [seeWarnings and Precautions (5.2)].
Amputation
Inform patients of the potential for an increased risk of amputations. Counsel patients about the importance of routine preventative foot care. Instruct patients to monitor for new pain or tenderness, sores or ulcers, or infections involving the leg or foot and to seek medical advice immediately if such signs or symptoms develop [seeWarnings and Precautions (5.3)].
Volume Depletion
Inform patients that symptomatic hypotension may occur with SEGLUROMET and advise them to contact their doctor if they experience such symptoms [see Warnings and Precautions (5.4)]. Inform patients that dehydration may increase the risk for hypotension, and to have adequate fluid intake.
Serious Urinary Tract Infections
Inform patients of the potential for urinary tract infections, which may be serious. Provide them with information on the symptoms of urinary tract infections. Advise them to seek medical advice if such symptoms occur [see Warnings and Precautions (5.5)].
Hypoglycemia with Concomitant Use of Insulin and/or Insulin Secretagogue
Inform patients that the incidence of hypoglycemia may increase when SEGLUROMET is added to insulin and/or an insulin secretagogue. Educate patients or caregivers on the signs and symptoms of hypoglycemia [see Warnings and Precautions (5.6)].
Necrotizing Fasciitis of the Perineum (Fournier's Gangrene)
Inform patients that necrotizing infections of the perineum (Fournier's Gangrene) have occurred with SGLT2 inhibitors. Counsel patients to promptly seek medical attention if they develop pain or tenderness, redness, or swelling of the genitals or the area from the genitals back to the rectum, along with a fever above 100.4¬įF or malaise [see Warnings and Precautions (5.7)].
Genital Mycotic Infections in Females (e.g., Vulvovaginitis)
Inform female patients that vaginal yeast infections may occur and provide them with information on the signs and symptoms of vaginal yeast infection. Advise them of treatment options and when to seek medical advice [seeWarnings and Precautions (5.8)].
Genital Mycotic Infections in Males (e.g., Balanitis or Balanoposthitis)
Inform male patients that yeast infections of the penis (e.g., balanitis or balanoposthitis) may occur, especially in uncircumcised males. Provide them with information on the signs and symptoms of balanitis and balanoposthitis (rash or redness of the glans or foreskin of the penis). Advise them of treatment options and when to seek medical advice [seeWarnings and Precautions (5.8)].
Fetal Toxicity
Advise pregnant patients of the potential risk to a fetus with treatment with SEGLUROMET. Instruct patients to immediately inform their healthcare provider if pregnant or planning to become pregnant [see Use in Specific Populations (8.1)].
Lactation
Advise patients that use of SEGLUROMET is not recommended while breastfeeding [see Use in Specific Populations (8.2)].
Pregnancy
Inform female patients that treatment with metformin may result in an unintended pregnancy in some premenopausal anovulatory females due to its effect on ovulation [see Use in Specific Populations (8.3)].
Laboratory Tests
Due to the mechanism of action of ertugliflozin, inform patients that their urine will test positive for glucose while taking SEGLUROMET.
Missed Dose
Instruct patients to take SEGLUROMET only as prescribed. If a dose is missed, it should be taken as soon as the patient remembers. Advise patients not to double their next dose.
Manufactured for: Merck Sharp & Dohme LLC Rahway, NJ 07065, USA
For patent information: www.msd.com/research/patent
Copyright © 2017-2024 Merck & Co., Inc., Rahway, NJ, USA, and its affiliates. All rights reserved.
uspi-mk8835b-t-2406r009
Spl Medguide Section
Medication GuideSEGLUROMET¬ģ [seg-LUR-oh-met](ertugliflozin and metformin hydrochloride)tablets, for oral use This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 09/2023 Read this Medication Guide carefully before you start taking SEGLUROMET and each time you get a refill. There may be new information. This information does not take the place of talking with your healthcare provider about your medical condition or your treatment. What is the most important information I should know about SEGLUROMET? SEGLUROMET may cause serious side effects, including: Lactic Acidosis. Metformin, one of the medicines in SEGLUROMET, can cause a rare but serious condition called lactic acidosis (a buildup of an acid in the blood) that can cause death. Lactic acidosis is a medical emergency and must be treated in the hospital. Call your healthcare provider right away if you have any of the following symptoms, which could be signs of lactic acidosis:
- you feel cold in your hands or feet
- you feel very weak or tired
- you have trouble breathing
- you have stomach pains, nausea or vomiting
- you have a slow or irregular heartbeat
- you have unusual (not normal) muscle pain
- you have unusual sleepiness or sleep longer than usual
- you feel dizzy or lightheaded
Most people who have had lactic acidosis had other conditions that, in combination with metformin use, led to the lactic acidosis. Tell your healthcare provider if you have any of the following, because you have a higher chance for getting lactic acidosis with SEGLUROMET if you: The best way to keep from having a problem with lactic acidosis from metformin is to tell your healthcare provider if you have any of the problems in the ul above. Your healthcare provider may decide to stop your SEGLUROMET for a while if you have any of these things.
- have severe kidney problems or your kidneys are affected by certain x-ray tests that use injectable dye.
- have liver problems.
- drink alcohol very often or drink a lot of alcohol in the short term ("binge") drinking.
- get dehydrated (lose a large amount of body fluids). This can happen if you are sick with a fever, vomiting, or diarrhea. Dehydration can also happen when you sweat a lot with activity or exercise and do not drink enough fluids.
- have surgery.
- have a heart attack, severe infection, or stroke.
- Diabetic ketoacidosis (increased ketones in your blood or urine) in people with type 1 diabetes and other ketoacidosis. SEGLUROMET can cause ketoacidosis that can be life-threatening and may lead to death. Ketoacidosis is a serious condition which needs to be treated in a hospital. People with type 1 diabetes have a high risk of getting ketoacidosis. People with type 2 diabetes or pancreas problems also have an increased risk of getting ketoacidosis. Ketoacidosis can also happen in people who are sick, cannot eat or drink as usual, skip meals, are on a diet high in fat and low in carbohydrates (ketogenic diet), take less than the usual amount of insulin or miss insulin doses, drink too much alcohol, have a loss of too much fluid from the body (volume depletion), or who have surgery. Ketoacidosis can happen even if your blood sugar is less than 250 mg/dL. Your healthcare provider may ask you to periodically check ketones in your urine or blood. Stop taking SEGLUROMET and call your healthcare provider or get medical help right away if you get any of the following. If possible, check for ketones in your urine or blood, even if your blood sugar is less than 250 mg/dL:
- nausea
- vomiting
- stomach-area (abdominal) pain
- tiredness
- trouble breathing
- ketones in your urine or blood
SEGLUROMET can have other serious side effects. See "What are the possible side effects of SEGLUROMET?" What is SEGLUROMET?
- SEGLUROMET contains 2 prescription medicines called ertugliflozin (STEGLATRO¬ģ) and metformin hydrochloride. SEGLUROMET is used in adults with type 2 diabetes to improve blood sugar (glucose) along with diet and exercise.
- SEGLUROMET is not recommended to decrease blood sugar (glucose) in people with type 1 diabetes. It is not known if SEGLUROMET is safe and effective in children under 18 years of age.
Who should not take SEGLUROMET? Do not take SEGLUROMET if you:
If you have any of these symptoms, stop taking SEGLUROMET and call your healthcare provider right away or go to the nearest hospital emergency room.
- have severe kidney problems, have end stage renal disease (ESRD) or are on dialysis.
- have a condition called metabolic acidosis or diabetic ketoacidosis (increased ketones in the blood or urine).
- are allergic to ertugliflozin, metformin, or any of the ingredients in SEGLUROMET. See the end of this Medication Guide for a ul of ingredients in SEGLUROMET. Symptoms of a serious allergic reaction to SEGLUROMET may include:
- skin rash
- raised red patches on your skin (hives)
- swelling of the face, lips, tongue, and throat that may cause difficulty in breathing or swallowing
Before you take SEGLUROMET, tell your healthcare provider about all of your medical conditions, including if you:
- have type 1 diabetes or have had diabetic ketoacidosis.
- have a decrease in your insulin dose.
- have a serious infection.
- have a history of infection of the vagina or penis.
- have a history of amputation.
- have had blocked or narrowed blood vessels, usually in the leg.
- have damage to the nerves (neuropathy) in your leg.
- have had diabetic foot ulcers or sores.
- have kidney problems.
- have liver problems.
- have a history of urinary tract infections or problems with urination.
- are on a low sodium (salt) diet. Your healthcare provider may change your diet or your dose.
- have heart problems, including congestive heart failure.
- are going to have surgery. Your healthcare provider may stop your SEGLUROMET before you have surgery. Talk to your healthcare provider if you are having surgery about when to stop taking SEGLUROMET and when to start it again.
- are eating less or there is a change in your diet.
- are dehydrated.
- have or have had problems with your pancreas, including pancreatitis or surgery on your pancreas.
- drink alcohol very often or drink a lot of alcohol in the short term (‚Äúbinge‚ÄĚ drinking).
- have ever had an allergic reaction to SEGLUROMET.
- are going to get an injection of dye or contrast agents for an x-ray procedure. SEGLUROMET may need to be stopped for a short time. Talk to your healthcare provider about when you should stop SEGLUROMET and when you should start SEGLUROMET again. See
"What is the most important information I should know about SEGLUROMET?" - are pregnant or plan to become pregnant. SEGLUROMET may harm your unborn baby. If you become pregnant while taking SEGLUROMET, your healthcare provider may switch you to a different medicine to control your blood sugar. Talk to your healthcare provider about the best way to control your blood sugar if you plan to become pregnant or while you are pregnant.
- are a premenopausal woman (before the ‚Äúchange of life‚ÄĚ), who does not have periods regularly or at all. Talk to your healthcare provider about birth control choices while taking SEGLUROMET if you are not planning to become pregnant since SEGLUROMET may increase your chance of becoming pregnant. Tell your healthcare provider right away if you become pregnant while taking SEGLUROMET.
- are breastfeeding or plan to breastfeed. It is not known if SEGLUROMET passes into your breast milk. You should not breastfeed if you take SEGLUROMET.
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. SEGLUROMET may affect the way other medicines work, and other medicines may affect how SEGLUROMET works. Know the medicines you take. Keep a ul of them to show your healthcare provider and pharmacist when you get a new medicine. How should I take SEGLUROMET?
- Take SEGLUROMET by mouth 2 times a day with meals, exactly as your healthcare provider tells you to take it. Taking SEGLUROMET with meals may lower your chance of having an upset stomach.
- Your healthcare provider may tell you to take SEGLUROMET along with other diabetes medicines. Low blood sugar can happen more often when SEGLUROMET is taken with certain other diabetes medicines. See "
What are the possible side effects of SEGLUROMET? " - If you miss a dose, take it as soon as you remember. If it is almost time for your next dose, skip the missed dose and take the medicine at the next regularly scheduled time. Do not take 2 doses of SEGLUROMET at the same time. Talk with your healthcare provider if you have questions about a missed dose.
- If you take too much SEGLUROMET, call your healthcare provider or go to the nearest hospital emergency room right away.
- When your body is under some types of stress, such as fever, trauma (such as a car accident), infection, or surgery, the amount of diabetes medicine you need may change. Tell your healthcare provider right away if you have any of these conditions and follow your healthcare provider’s instructions.
- SEGLUROMET will cause your urine to test positive for glucose.
- Your healthcare provider may do certain blood tests before you start SEGLUROMET and during treatment as needed. Your healthcare provider may change your dose of SEGLUROMET based on the results of your blood tests.
What should I avoid while taking SEGLUROMET?
- Avoid drinking alcohol very often or drinking a lot of alcohol in a short period of time ("binge" drinking). It can increase your chances of getting serious side effects.
What are the possible side effects of SEGLUROMET? SEGLUROMET may cause serious side effects, including: See " What is the most important information I should know about SEGLUROMET? "
Amputations. SEGLUROMET may increase your risk of lower limb amputations. You may be at a higher risk of lower limb amputation if you:
- have a history of amputation
- have had blocked or narrowed blood vessels, usually in your leg
- have damage to the nerves (neuropathy) in your leg
- have had diabetic foot ulcers or sores
Call your healthcare provider right away if you have new pain or tenderness, any sores, ulcers, or infections in your leg or foot. Your healthcare provider may decide to stop your SEGLUROMET for a while if you have any of these signs or symptoms. Talk to your healthcare provider about proper foot care.
Talk to your healthcare provider about what you can do to prevent dehydration including how much fluid you should drink on a daily basis. Call your healthcare provider right away if you reduce the amount of food or liquid you drink, for example if you are sick or cannot eat, or you start to lose liquids from your body, for example from vomiting, diarrhea or being in the sun too long.
Dehydration. SEGLUROMET can cause some people to become dehydrated (the loss of body water and salt). Dehydration may cause you to feel dizzy, faint, lightheaded, or weak, especially when you stand up (orthostatic hypotension). There have been reports of sudden worsening of kidney function in people who are taking SEGLUROMET. You may be at risk of dehydration if you:
- take medicines to lower your blood pressure, including water pills (diuretics)
- are on a low sodium (salt) diet
- have kidney problems
- are 65 years of age or older
Serious urinary tract infections. Serious urinary tract infections that may lead to hospitalization have happened in people who are taking SEGLUROMET. Tell your healthcare provider if you have any signs or symptoms of a urinary tract infection such as a burning feeling when passing urine, a need to urinate often, the need to urinate right away, pain in the lower part of your stomach (pelvis), or blood in the urine. Sometimes people may also have a fever, back pain, nausea, or vomiting.
Low blood sugar (hypoglycemia). If you take SEGLUROMET with another medicine that can cause low blood sugar such as a sulfonylurea or insulin, your risk of getting low blood sugar is higher. The dose of your sulfonylurea or insulin may need to be lowered while you take SEGLUROMET. Signs and symptoms of low blood sugar may include:
- headache
- confusion
- hunger
- shaking or feeling jittery
- drowsiness
- dizziness
- fast heartbeat
- weakness
- sweating
- irritability
- A rare but serious bacterial infection that causes damage to the tissue under the skin (necrotizing fasciitis) in the area between and around the anus and genitals (perineum). Necrotizing fasciitis of the perineum has happened in women and men who take medicines that lower blood sugar in the same way as one of the medicines in SEGLUROMET. Necrotizing fasciitis of the perineum may lead to hospitalization, may require multiple surgeries, and may lead to death. Seek medical attention immediately if you have fever above 100.4¬įF or you are feeling very weak, tired or uncomfortable (malaise) and you develop any of the following symptoms in the area between and around your anus and genitals:
- pain or tenderness
- swelling
- redness of skin (erythema)
Vaginal yeast infection. Symptoms of a vaginal yeast infection include:
- vaginal odor
- white or yellowish vaginal discharge (discharge may be lumpy or look like cottage cheese)
- vaginal itching
Yeast infection of the penis (balanitis or balanoposthitis). Swelling of an uncircumcised penis may develop that makes it difficult to pull back the skin around the tip of the penis. Other symptoms of yeast infection of the penis include:
- redness, itching, or swelling of the penis
- foul smelling discharge from the penis
- rash of the penis
- pain in the skin around your penis
Talk to your healthcare provider about what to do if you get symptoms of a yeast infection of the vagina or penis. Your healthcare provider may suggest you use an over-the-counter antifungal medicine. Talk to your healthcare provider right away if you use an over-the-counter antifungal medicine and your symptoms do not go away.
Low vitamin B12 (vitamin B12 deficiency). Using metformin for long periods of time may cause a decrease in the amount of vitamin B12 in your blood, especially if you have had low vitamin B12 blood levels before. Your healthcare provider may do blood tests to check your vitamin B12 levels. Serious allergic reaction. If you have any symptoms of a serious allergic reaction, stop taking SEGLUROMET and call your healthcare provider right away or go to the nearest hospital emergency room. See ‚Äú Who should not take SEGLUROMET? ‚ÄĚ. Your healthcare provider may give you a medicine for your allergic reaction and prescribe a different medicine for your diabetes The most common side effects of ertugliflozin include:
- vaginal yeast infections and yeast infections of the penis
(See "What is the most important information I should know about SEGLUROMET?") - changes in urination, including urgent need to urinate more often, in larger amounts, or at night
The most common side effects of metformin hydrochloride include:
- diarrhea
- nausea
- stomach discomfort
- vomiting
- gas
- headache
- indigestion
- weakness
These are not all the possible side effects of SEGLUROMET.Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store SEGLUROMET?
- Store SEGLUROMET at room temperature between 68¬įF to 77¬įF (20¬įC to 25¬įC).
- Keep SEGLUROMET dry.
Keep SEGLUROMET and all medicines out of the reach of children. General information about the safe and effective use of SEGLUROMET. Medicines are sometimes prescribed for purposes other than those uled in a Medication Guide. Do not use SEGLUROMET for a condition for which it was not prescribed. Do not give SEGLUROMET to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about SEGLUROMET that is written for health professionals. For more information about SEGLUROMET, go to www.segluromet.com or call 1-800-622-4477. What are the ingredients in SEGLUROMET? Active ingredients: ertugliflozin and metformin hydrochloride. Inactive ingredients: povidone, microcrystalline cellulose, crospovidone, sodium lauryl sulfate, and magnesium stearate. The tablet film coating contains the following inactive ingredients: hydroxypropyl methylcellulose, hydroxypropyl cellulose, titanium dioxide, iron oxide red, and carnauba wax. Manufactured for: Merck Sharp & Dohme LLC Rahway, NJ 07065, USAFor patent information, go to: www.msd.com/research/patent Copyright © 2017-2023 Merck & Co., Inc., Rahway, NJ, USA, and its affiliates. All rights reserved. usmg-mk8835b-t-2309r007
Principal Display Panel - 2.5 Mg/500 Mg Tablet Bottle Label
NDC 0006-5369-03
Segluromet¬ģ
(ertugliflozin andmetformin HCl) tablets
2.5 mg / 500 mg
Dispense the accompanying Medication Guideto each patient.
Each tablet contains 3.24 mg ertugliflozin L-pyroglutamicacid (equivalent to 2.5 mg ertugliflozin) and500 mg of metformin hydrochloride.
Rx only
60 Tablets
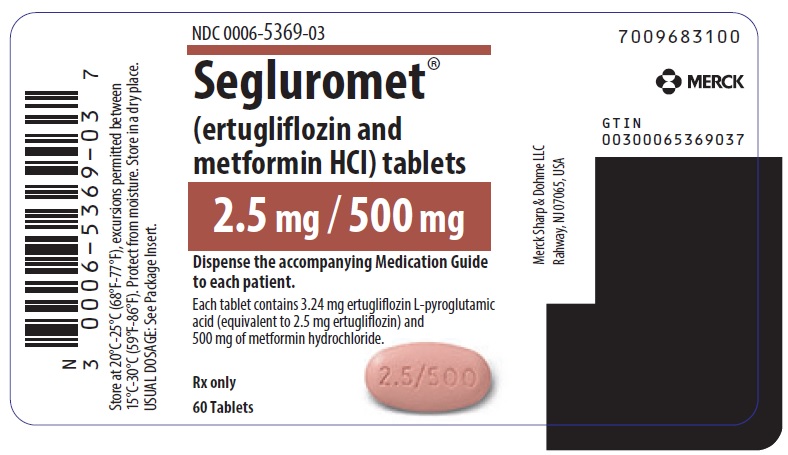
Principal Display Panel - 2.5 Mg/1,000 Mg Tablet Bottle Label
NDC 0006-5373-03
Segluromet¬ģ (ertugliflozin andmetformin HCl) tablets
2.5 mg / 1,000 mg
Dispense the accompanying Medication Guideto each patient.
Each tablet contains 3.24 mg ertugliflozinL-pyroglutamic acid (equivalentto 2.5 mg ertugliflozin) and1,000 mg of metforminhydrochloride.
60 TabletsRx only
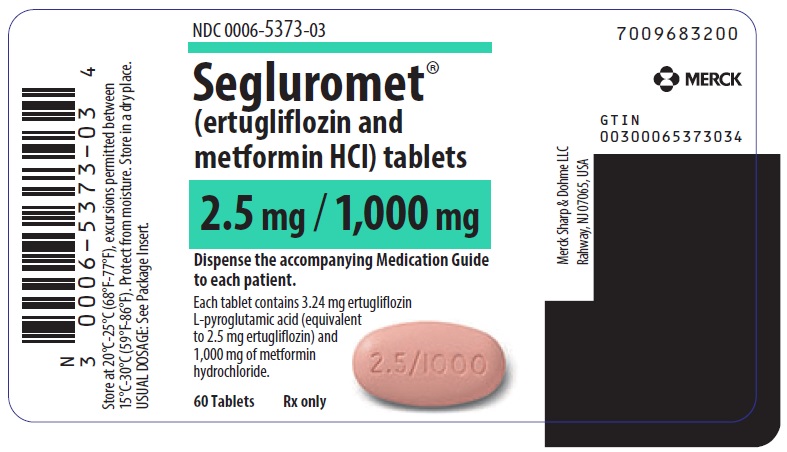
Principal Display Panel - 7.5 Mg/500 Mg Tablet Bottle Label
NDC 0006-5370-03
Segluromet¬ģ
(ertugliflozin andmetformin HCl) tablets
7.5 mg / 500 mg
Dispense the accompanying Medication Guideto each patient.
Each tablet contains 9.71 mg ertugliflozin L-pyroglutamicacid (equivalent to 7.5 mg ertugliflozin)and 500 mg of metforminhydrochloride.
Rx only
60 Tablets
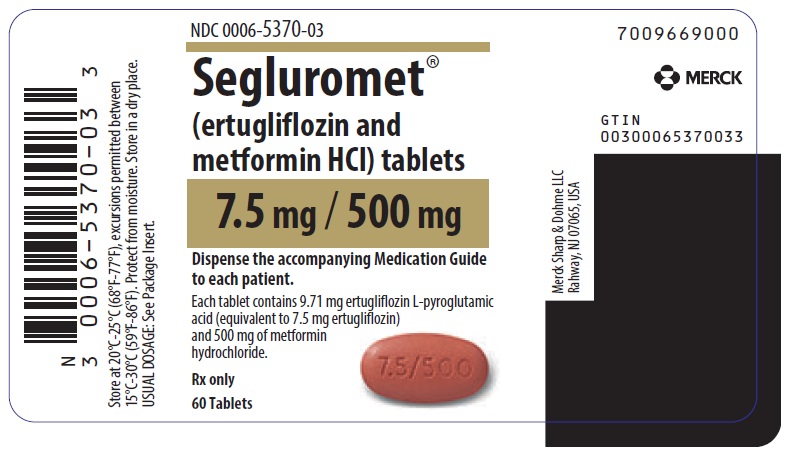
Principal Display Panel - 7.5 Mg/1,000 Mg Tablet Bottle Label
NDC 0006-5374-03
Segluromet¬ģ (ertugliflozin andmetformin HCl) tablets
7.5 mg / 1,000 mg
Dispense the accompanying Medication Guideto each patient.
Each tablet contains 9.71 mg ertugliflozin L-pyroglutamicacid (equivalent to 7.5 mgertugliflozin) and 1,000 mgof metformin hydrochloride.
Rx only
60 Tablets
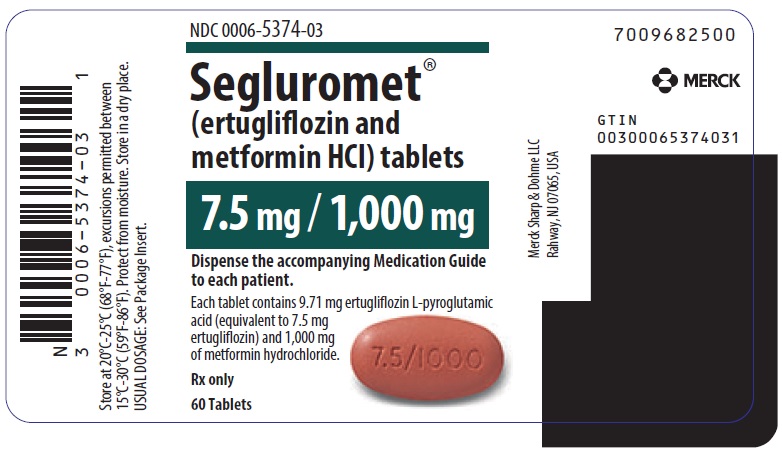
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


