etravirine (etravirine tablet 25 mg) Dailymed
Generic: etravirine is used for the treatment of HIV Infections
IMPRINT: A56
SHAPE: oval
COLOR: white
All Imprints
etravirine tablet 200 mg - ac76 oval white
etravirine tablet 100 mg - ac75 oval white
etravirine tablet 25 mg - a56 oval white
Go PRO for all pill images
1 Indications And Usage
Etravirine tablets, in combination with other antiretroviral agents, are indicated for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in antiretroviral treatment-experienced adult patients and pediatric patients 6 years of age and older [see Microbiology (12.4) and Clinical Studies (14)].
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ (etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Etravirine is a human immunodeficiency virus type 1 (HIV-1) non-nucleoside reverse transcriptase inhibitor (NNRTI) indicated for treatment of HIV-1 infection in treatment-experienced patients 6 years of age and older.(1)
2 Dosage And Administration
- Adult patients: 200 mg (one 200 mg tablet or two 100 mg tablets) taken twice daily following a meal.
(2.1 ,2.2 ,2.4) - Pregnant patients: 200 mg (one 200 mg tablet or two 100 mg tablets) taken twice daily following a meal.
(2.2) - Pediatric patients (6 years to less than 18 years of age and weighing at least 16 kg): dosage of etravirine tablets are based on body weight and should not exceed the recommended adult dose. Etravirine tablets should be taken following a meal.
(2.3) 2.1 RecommendedDosage in Adult Patients
The recommended oral dosage of etravirine tablets for adult patients is 200 mg (one 200 mg tablet or two 100 mg tablets) taken twice daily following a meal. The type of food does not affect the exposure to etravirine [see Clinical Pharmacology (12.3)].
2.2 RecommendedDosage During Pregnancy
The recommended oral dosage of etravirine tablets for pregnant individuals is 200 mg (one 200 mg tablet or two 100 mg tablets) taken twice daily following a meal [see Use in Specific Populations (8.1)].
2.3 RecommendedDosage in Pediatric Patients (6 Years to Less Than 18 Years of Age)
The recommended dosage of etravirine tablets for pediatric patients 6 years to less than 18 years of age and weighing at least 16 kg is based on body weight (see Table 1) not exceeding the recommended adult dosage. Etravirine tablets should be taken orally, following a meal. The type of food does not affect the exposure to etravirine tablets [see Clinical Pharmacology (12.3)].
Table 1: Recommended Dosage of Etravirine Tablets for Pediatric Patients 6 Years to Less Than 18 Years of Age
Body Weight
kilograms (kg)
Dose
greater than or equal to 16 kg to less than 20 kg
100 mg twice daily
greater than or equal to 20 kg to less than 25 kg
125 mg twice daily
greater than or equal to 25 kg to less than 30 kg
150 mg twice daily
greater than or equal to 30 kg
200 mg twice daily
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ (etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
2.4 Method ofAdministration
Instruct patients to swallow the etravirine tablet(s) whole with liquid such as water. Patients who are unable to swallow the etravirine tablet(s) whole may disperse the tablet(s) in water. Instruct the patient to do the following:
- place the tablet(s) in 5 mL (1 teaspoon) of water, or at least enough liquid to cover the medication,
- stir well until the water looks milky,
- add approximately 15 mL (1 tablespoon) of liquid. Water may be used but other liquids, such as orange juice or milk, may improve taste. Patients should not place the tablets in orange juice or milk without first adding water. The use of warm (temperature greater than 104¬įF [greater than 40¬įC]) or carbonated beverages should be avoided.
- drink the mixture immediately,
- rinse the glass several times with orange juice, milk or water and completely swallow the rinse each time to make sure the patient takes the entire dose.
3 Dosage Forms And Strengths
- 25 mg white to off-white, oval shaped, uncoated tablets debossed with ‚ÄúA56‚ÄĚ on one side and score on the other side.
- 100 mg white to off-white oval shaped, uncoated tablets debossed with ‚ÄúAC75‚ÄĚ on one side and plain on the other side.
- 200 mg white to off-white, oval shaped, uncoated tablets debossed with ‚ÄúAC76‚ÄĚ on one side and plain on the other side.
- Tablets: 25 mg, 100 mg, and 200 mg
(3)
4 Contraindications
None.
None.(4)
5 Warnings And Precautions
- Severe, potentially life threatening and fatal skin reactions have been reported. This includes cases of Stevens-Johnson syndrome, hypersensitivity reaction, toxic epidermal necrolysis and erythema multiforme. Immediately discontinue treatment if severe hypersensitivity, severe rash or rash with systemic symptoms or liver transaminase elevations develops and monitor clinical status, including liver transaminases closely.
(5.1) - Monitor for immune reconstitution syndrome and fat redistribution.
(5.3 ,5.4) 5.1 Severe Skinand Hypersensitivity Reactions
Severe, potentially life-threatening and fatal skin reactions have been reported. In clinical trials, these include cases of Stevens-Johnson syndrome, toxic epidermal necrolysis and erythema multiforme. Hypersensitivity reactions including Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) have also been reported and were characterized by rash, constitutional findings, and sometimes organ dysfunction, including hepatic failure. In Phase 3 clinical trials, Grade 3 and 4 rashes were reported in 1.3% of subjects receiving etravirine compared to 0.2% of placebo subjects. A total of 2.2% of HIV-1-infected subjects receiving etravirine discontinued from Phase 3 trials due to rash [see Adverse Reactions (6.1)]. Rash occurred most commonly during the first 6 weeks of therapy. The incidence of rash was higher in females [see Adverse Reactions (6.1)]. Stevens-Johnson syndrome was reported in 1.1% (2/177) of pediatric patients less than 18 years of age receiving etravirine in combination with other HIV-1 antiretroviral agents in an observational study.
Discontinue etravirine immediately if signs or symptoms of severe skin reactions or hypersensitivity reactions develop (including, but not limited to, severe rash or rash accompanied by fever, general malaise, fatigue, muscle or joint aches, bulers, oral lesions, conjunctivitis, facial edema, hepatitis, eosinophilia, angioedema). Clinical status including liver transaminases should be monitored and appropriate therapy initiated. Delay in stopping etravirine treatment after the onset of severe rash may result in a life-threatening reaction.
5.2 Risk ofAdverse Reactions or Loss of Virologic Response Due to Drug Interactions
The concomitant use of etravirine and other drugs may result in potentially significant drug interactions, some of which may lead to [see Drug Interactions (7.3)]:
- Loss of therapeutic effect of concomitant drug or etravirine and possible development of resistance.
- Possible clinically significant adverse reactions from greater exposures of etravirine or other concomitant drugs.
See Table 4 for steps to prevent or manage these possible and known significant drug interactions, including dosing recommendations. Consider the potential for drug interactions prior to and during etravirine therapy and review concomitant medications during etravirine therapy.
5.3 ImmuneReconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including etravirine. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jiroveci pneumonia (PCP) or tuberculosis), which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves’ disease, polymyositis, Guillain-Barré syndrome, and autoimmune hepatitis) have also been reported to occur in the setting of immune reconstitution; however, the time to onset is more variable, and can occur many months after initiation of treatment.
5.4 FatRedistribution
Redistribution/accumulation of body fat, including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and ‚Äúcushingoid appearance‚ÄĚ have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
6 Adverse Reactions
The following adverse reactions are described in greater detail in other sections:
- Severe skin and hypersensitivity reactions [see Warnings and Precautions (5.1)].
- Immune reconstitution syndrome [see Warnings and Precautions (5.3)].
The most common adverse drug reactions of moderate to severe intensity (at least 2%) which occurred at a higher rate than placebo in adults are rash and peripheral neuropathy.(6.1)
The most common adverse drug reactions in at least 2% of pediatric patients are rash and diarrhea.(6.1) To report SUSPECTED ADVERSE REACTIONS, contact Amneal Pharmaceuticals at 1-877-835-5472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 ClinicalTrials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trials Experience in Adults
The safety assessment is based on all data from 1,203 subjects in the Phase 3 placebo-controlled trials, TMC125-C206 and TMC125-C216, conducted in antiretroviral treatment-experienced HIV-1-infected adult subjects, 599 of whom received etravirine (200 mg twice daily). In these pooled trials, the median exposure for subjects in the etravirine arm and placebo arm was 52.3 and 51.0 weeks, respectively. Discontinuations due to adverse drug reactions (ADRs) were 5.2% in the etravirine arm and 2.6% in the placebo arm.
The most frequently reported ADR at least Grade 2 in severity was rash (10.0%). Stevens-Johnson syndrome, drug hypersensitivity reaction and erythema multiforme were reported in less than 0.1% of subjects during clinical development with etravirine [see Warnings and Precautions (5.1)]. A total of 2.2% of HIV-1-infected subjects in Phase 3 trials receiving etravirine discontinued due to rash. In general, in clinical trials, rash was mild to moderate, occurred primarily in the second week of therapy, and was infrequent after Week 4. Rash generally resolved within 1 to 2 weeks on continued therapy. The incidence of rash was higher in women compared to men in the etravirine arm in the Phase 3 trials (rash ‚Č• Grade 2 was reported in 9/60 [15.0%] women versus 51/539 [9.5%] men; discontinuations due to rash were reported in 3/60 [5.0%] women versus 10/539 [1.9%] men) [see Warnings and Precautions (5.1)]. Patients with a history of NNRTI-related rash did not appear to be at increased risk for the development of etravirine-related rash compared to patients without a history of NNRTI-related rash.
Common Adverse Reactions
Clinical ADRs of moderate intensity or greater (greater than or equal to Grade 2) and reported in at least 2% of subjects treated with etravirine and occurring at a higher rate compared to placebo (excess of 1%) are presented in Table 2. Laboratory abnormalities considered ADRs are included in Table 3.
Table 2: Adverse Drug Reactions (Grades 2 to 4) in at Least 2% of Adult Subjects (Pooled TMC125-C206 and TMC125-C216 Trials)
Preferred Term
Etravirine + BR
N=599
%
Placebo + BR
N=604
%
Rash
10%
3%
Peripheral neuropathy
4%
2%
N=total number of subjects per treatment group; BR=background regimen
Less Common Adverse Reactions
Treatment-emergent ADRs occurring in less than 2% of subjects (599 subjects) receiving etravirine and of at least moderate intensity (greater than or equal to Grade 2) are uled below by body system:
Cardiac Disorders: myocardial infarction, angina pectoris, atrial fibrillation
Ear and Labyrinth Disorders: vertigo
Eye Disorders: blurred vision
Gastrointestinal Disorders: gastroesophageal reflux disease, flatulence, gastritis, abdominal distension, pancreatitis, constipation, dry mouth, hematemesis, retching, stomatitis
General Disorders and Administration Site Conditions: sluggishness
Hematologic Disorders: hemolytic anemia
Hepatobiliary Disorders: hepatic failure, hepatomegaly, cytolytic hepatitis, hepatic steatosis, hepatitis
Immune System Disorders: drug hypersensitivity, immune reconstitution syndrome
Metabolism and Nutrition Disorders: diabetes mellitus, anorexia, dyslipidemia
Nervous System Disorders: paresthesia, somnolence, convulsion, hypoesthesia, amnesia, syncope, disturbance in attention, hypersomnia, tremor
Psychiatric Disorders: anxiety, sleep disorders, abnormal dreams, confusional state, disorientation, nervousness, nightmares
Renal and Urinary Disorders: acute renal failure
Reproductive System and Breast Disorders: gynecomastia
Respiratory, Thoracic and Mediastinal Disorders: exertional dyspnea, bronchospasm
Skin and Subcutaneous Tissue Disorders: night sweats, lipohypertrophy, prurigo, hyperhidrosis, dry skin, swelling face
Additional ADRs of at least moderate intensity observed in other trials were acquired lipodystrophy, angioneurotic edema, erythema multiforme and hemorrhagic stroke, each reported in no more than 0.5% of subjects.
Laboratory Abnormalities in Treatment-Experienced Patients
Selected Grade 2 to Grade 4 laboratory abnormalities that represent a worsening from baseline observed in adult subjects treated with etravirine are presented in Table 3.
Table 3: Selected Grade 2 to 4 Laboratory Abnormalities Observed in Treatment-Experienced Subjects (Pooled TMC125-C206 and TMC125-C216 Trials)
Laboratory Parameter
DAIDS Toxicity
Range
Etravirine + BR
N=599
%
Placebo + BR
N=604
%
GENERAL BIOCHEMISTRY
Pancreatic amylase
Grade 2
> 1.5 to 2 x ULN
7%
8%
Grade 3
> 2 to 5 x ULN
7%
8%
Grade 4
> 5 x ULN
2%
1%
Lipase
Grade 2
> 1.5 to 3 x ULN
4%
6%
Grade 3
> 3 to 5 x ULN
2%
2%
Grade 4
> 5 x ULN
1%
< 1%
Creatinine
Grade 2
> 1.4 to 1.8 x ULN
6%
5%
Grade 3
> 1.9 to 3.4 x ULN
2%
1%
Grade 4
> 3.4 x ULN
0%
< 1%
HEMATOLOGY
Decreased hemoglobin
Grade 2
90 g/L to 99 g/L
2%
4%
Grade 3
70 g/L to 89 g/L
< 1%
< 1%
Grade 4
< 70 g/L
< 1%
< 1%
White blood cell count
Grade 2
1,500 to 1,999/mm3
2%
3%
Grade 3
1,000 to 1,499/mm3
1%
4%
Grade 4
< 1,000/mm3
1%
< 1%
Neutrophils
Grade 2
750 to 999/mm3
5%
6%
Grade 3
500 to 749/mm3
4%
4%
Grade 4
< 500/mm3
2%
3%
Platelet count
Grade 2
50,000 to 99,999/mm3
3%
5%
Grade 3
25,000 to 49,999/mm3
1%
1%
Grade 4
< 25,000/mm3
< 1%
< 1%
LIPIDS AND GLUCOSE
Total cholesterol
Grade 2
> 6.20 to 7.77 mmol/L
240 to 300 mg/dL
20%
17%
Grade 3
> 7.77 mmol/L
> 300 mg/dL
8%
5%
Low density lipoprotein
Grade 2
4.13 to 4.9 mmol/L
160 to 190 mg/dL
13%
12%
Grade 3
> 4.9 mmol/L
> 190 mg/dL
7%
7%
Triglycerides
Grade 2
5.65 to 8.48 mmol/L
500 to 750 mg/dL
9%
7%
Grade 3
8.49 to 13.56 mmol/L
751 to 1,200 mg/dL
6%
4%
Grade 4
> 13.56 mmol/L
> 1200 mg/dL
4%
2%
Elevated glucose levels
Grade 2
6.95 to 13.88 mmol/L
161 to 250 mg/dL
15%
13%
Grade 3
13.89 to 27.75 mmol/L
251 to 500 mg/dL
4%
2%
Grade 4
> 27.75 mmol/L
> 500 mg/dL
0%
< 1%
HEPATIC PARAMETERS
Alanine amino transferase
Grade 2
2.6 to 5 x ULN
6%
5%
Grade 3
5.1 to 10 x ULN
3%
2%
Grade 4
> 10 x ULN
1%
< 1%
Aspartate amino transferase
Grade 2
2.6 to 5 x ULN
6%
8%
Grade 3
5.1 to 10 x ULN
3%
2%
Grade 4
> 10 x ULN
< 1%
< 1%
ULN=Upper Limit of Normal; BR=background regimen
Patients Co-Infected With Hepatitis B and/or Hepatitis C Virus
In Phase 3 trials TMC125-C206 and TMC125-C216, 139 subjects (12.3%) with chronic hepatitis B and/or hepatitis C virus co-infection out of 1,129 subjects were permitted to enroll. AST and ALT abnormalities occurred more frequently in hepatitis B and/or hepatitis C virus co-infected subjects for both treatment groups. Grade 2 or higher laboratory abnormalities that represent a worsening from baseline of AST, ALT or total bilirubin occurred in 27.8%, 25.0% and 7.1% respectively, of etravirine-treated co-infected subjects as compared to 6.7%, 7.5% and 1.8% of non-co-infected etravirine-treated subjects. In general, adverse events reported by etravirine-treated subjects with hepatitis B and/or hepatitis C virus co-infection were similar to etravirine-treated subjects without hepatitis B and/or hepatitis C virus co-infection.
Clinical Trials Experience in Pediatric Subjects (6 Years to Less Than 18 years of age)
The safety assessment in pediatric subjects is based on a single-arm trial. TMC125-C213 is a Phase 2 trial in which 101 antiretroviral treatment-experienced HIV-1 infected pediatric subjects 6 years to less than 18 years of age received etravirine in combination with other antiretroviral agents (Week 24 analysis) [see Clinical Studies (14.2)].
In TMC125-C213, the frequency, type and severity of adverse drug reactions in pediatric subjects 6 years to less than 18 years of age were comparable to those observed in adult subjects, except for rash which was observed more frequently in pediatric subjects. The most common adverse drug reactions in at least 2% of pediatric subjects were rash and diarrhea. Rash was reported more frequently in female subjects than in male subjects (rash ‚Č• Grade 2 was reported in 13/64 [20.3%] females versus 2/37 [5.4%] males; discontinuations due to rash were reported in 4/64 [6.3%] females versus 0/37 [0%] males). Rash (greater than or equal to Grade 2) occurred in 15% of pediatric subjects from 6 years to less than 18 years of age. In the majority of cases, rash was mild to moderate, of macular/papular type, and occurred in the second week of therapy. Rash was self-limiting and generally resolved within 1 week on continued therapy. The safety profile for subjects who completed 48 weeks of treatment was similar to the safety profile for subjects who completed 24 weeks of treatment.
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ (etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
6.2 PostmarketingExperience
The following events have been identified during postmarketing use of etravirine. Because these events are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System Disorders: Severe hypersensitivity reactions including DRESS and cases of hepatic failure have been reported [see Warnings and Precautions (5.1)].
Musculoskeletal and Connective Tissue Disorders: rhabdomyolysis
Skin and Subcutaneous Tissue Disorders: Fatal cases of toxic epidermal necrolysis and Stevens-Johnson syndrome have been reported [see Warnings and Precautions (5.1)].
7 Drug Interactions
Co-administration of etravirine with other drugs can alter the concentrations of other drugs and other drugs may alter the concentrations of etravirine. The potential drug-drug interactions must be considered prior to and during therapy.(7 ,12.3)
7.1 Potentialfor Other Drugs to Affect Etravirine
Etravirine is a substrate of CYP3A, CYP2C9, and CYP2C19. Therefore, co-administration of etravirine with drugs that induce or inhibit CYP3A, CYP2C9, and CYP2C19 may alter the therapeutic effect or adverse reaction profile of etravirine (see Table 4) [see Clinical Pharmacology (12.3)].
7.2 Potentialfor Etravirine to Affect Other Drugs
Etravirine is an inducer of CYP3A and inhibitor of CYP2C9, CYP2C19 and P-glycoprotein (P-gp). Therefore, co-administration of drugs that are substrates of CYP3A, CYP2C9 and CYP2C19 or are transported by P-gp with etravirine may alter the therapeutic effect or adverse reaction profile of the co-administered drug(s) (see Table 4) [see Clinical Pharmacology (12.3)].
7.3 SignificantDrug Interactions
Table 4 shows significant drug interactions based on which, alterations in dose or regimen of etravirine and/or co-administered drug may be recommended. Drugs that are not recommended for co-administration with etravirine are also included in Table 4 [see Clinical Pharmacology (12.3)].
Table 4: Significant Drug Interactions
Concomitant Drug Class:
Drug Name
Effect on Concentration of Etravirine or Concomitant Drug
Clinical Comment
HIV-antiviral agents: integrase strand inhibitors
dolutegravir*
‚Üď dolutegravir
‚ÜĒ etravirine
Etravirine significantly reduced plasma concentrations of dolutegravir. Using cross-study comparisons to historical pharmacokinetic data for etravirine, dolutegravir did not appear to affect the pharmacokinetics of etravirine.
dolutegravir/darunavir/ritonavir*
‚Üď dolutegravir
‚ÜĒ etravirine
The effect of etravirine on dolutegravir plasma concentrations was mitigated by co-administration of darunavir/ritonavir or lopinavir/ritonavir, and is expected to be mitigated by atazanavir/ritonavir.
dolutegravir/lopinavir/ritonavir*
‚ÜĒ dolutegravir
‚ÜĒ etravirine
Dolutegravir should only be used with etravirine when co-administered with atazanavir/ritonavir, darunavir/ritonavir, or lopinavir/ritonavir.
HIV-antiviral agents: non-nucleoside reverse transcriptase inhibitors (NNRTIs)
efavirenz*
nevirapine*
‚Üď etravirine
Combining two NNRTIs has not been shown to be beneficial. Concomitant use of etravirine with efavirenz or nevirapine may cause a significant decrease in the plasma concentrations of etravirine and loss of therapeutic effect of etravirine. Co-administration of etravirine and other NNRTIs is not recommended.
delavirdine
‚ÜĎ etravirine
Combining two NNRTIs has not been shown to be beneficial. Etravirine and delavirdine should not be co-administered.
rilpivirine
‚Üď rilpivirine
‚ÜĒ etravirine
Combining two NNRTIs has not been shown to be beneficial. Co-administration of etravirine and rilpivirine is not recommended.
HIV-antiviral agents: protease inhibitors (PIs)
atazanavir*
(without ritonavir)
‚Üď atazanavir
Co-administration of etravirine and atazanavir without low-dose ritonavir is not recommended.
atazanavir/ritonavir*
‚Üď atazanavir
‚ÜĒ etravirine
Concomitant use of etravirine with atazanavir/ritonavir decreased atazanavir Cmin but it is not considered clinically relevant. The mean systemic exposure (AUC) of etravirine after co-administration of etravirine with atazanavir/ritonavir in HIV-infected subjects was similar to the mean systemic exposure of etravirine observed in the Phase 3 trials after co-administration of etravirine and darunavir/ritonavir (as part of the background regimen). Etravirine and atazanavir/ritonavir can be co-administered without dose adjustments.
atazanavir/cobicistat
‚Üď atazanavir
‚Üď cobicistat
Co-administration of etravirine with atazanavir/cobicistat is not recommended because it may result in loss of therapeutic effect and development of resistance to atazanavir.
darunavir/ritonavir*
‚Üď etravirine
The mean systemic exposure (AUC) of etravirine was reduced when etravirine was co-administered with darunavir/ritonavir. Because all subjects in the Phase 3 trials received darunavir/ritonavir as part of the background regimen and etravirine exposures from these trials were determined to be safe and effective, etravirine and darunavir/ritonavir can be co-administered without dose adjustments.
darunavir/cobicistat
‚Üď cobicistat
darunavir: effect unknown
Co-administration of etravirine with darunavir/cobicistat is not recommended because it may result in loss of therapeutic effect and development of resistance to darunavir.
fosamprenavir
(without ritonavir)
‚ÜĎ amprenavir
Concomitant use of etravirine with fosamprenavir without low-dose ritonavir may cause a significant alteration in the plasma concentration of amprenavir. Co-administration of etravirine and fosamprenavir without low-dose ritonavir is not recommended.
fosamprenavir/ritonavir*
‚ÜĎ amprenavir
Due to a significant increase in the systemic exposure of amprenavir, the appropriate doses of the combination of etravirine and fosamprenavir/ritonavir have not been established. Co-administration of etravirine and fosamprenavir/ritonavir is not recommended.
indinavir*
(without ritonavir)
‚Üď indinavir
Concomitant use of etravirine with indinavir without low-dose ritonavir may cause a significant alteration in the plasma concentration of indinavir. Co-administration of etravirine and indinavir without low-dose ritonavir is not recommended.
lopinavir/ritonavir*
‚Üď etravirine
The mean systemic exposure (AUC) of etravirine was reduced after co-administration of etravirine with lopinavir/ritonavir (tablet). Because the reduction in the mean systemic exposures of etravirine in the presence of lopinavir/ritonavir is similar to the reduction in mean systemic exposures of etravirine in the presence of darunavir/ritonavir, etravirine and lopinavir/ritonavir can be co-administered without dose adjustments.
nelfinavir
(without ritonavir)
‚ÜĎ nelfinavir
Concomitant use of etravirine with nelfinavir without low-dose ritonavir may cause a significant alteration in the plasma concentration of nelfinavir. Co-administration of etravirine and nelfinavir without low-dose ritonavir is not recommended.
ritonavir*
‚Üď etravirine
Concomitant use of etravirine with ritonavir 600 mg twice daily may cause a significant decrease in the plasma concentration of etravirine and loss of therapeutic effect of etravirine. Co-administration of etravirine and ritonavir 600 mg twice daily is not recommended.
saquinavir/ritonavir*
‚Üď etravirine
The mean systemic exposure (AUC) of etravirine was reduced when etravirine was co-administered with saquinavir/ritonavir. Because the reduction in the mean systemic exposures of etravirine in the presence of saquinavir/ritonavir is similar to the reduction in mean systemic exposures of etravirine in the presence of darunavir/ritonavir, etravirine and saquinavir/ritonavir can be co-administered without dose adjustments.
tipranavir/ritonavir*
‚Üď etravirine
Concomitant use of etravirine with tipranavir/ritonavir may cause a significant decrease in the plasma concentrations of etravirine and loss of therapeutic effect of etravirine. Co-administration of etravirine and tipranavir/ritonavir is not recommended.
CCR5 antagonists
maraviroc*
‚ÜĒ etravirine
‚Üď maraviroc
When etravirine is co-administered with maraviroc in the absence of a potent CYP3A inhibitor (e.g., ritonavir boosted protease inhibitor), the recommended dose of maraviroc is 600 mg twice daily. No dose adjustment of etravirine is needed.
maraviroc/darunavir/ritonavir*†
‚ÜĒ etravirine
‚ÜĎ maraviroc
When etravirine etravirine is co-administered with maraviroc in the presence of a potent CYP3A inhibitor (e.g., ritonavir boosted protease inhibitor), the recommended dose of maraviroc is 150 mg twice daily. No dose adjustment of etravirine is needed.
Other agents
Antiarrhythmics:
digoxin*
‚ÜĒ etravirine
‚ÜĎ digoxin
For patients who are initiating a combination of etravirine and digoxin, the lowest dose of digoxin should initially be prescribed.
For patients on a stable digoxin regimen and initiating etravirine, no dose adjustment of either etravirine or digoxin is needed. The serum digoxin concentrations should be monitored and used for titration of the digoxin dose to obtain the desired clinical effect.
amiodarone
bepridil
disopyramide
flecainide
lidocaine (systemic)
mexiletine
propafenone
quinidine
‚Üď antiarrhythmics
Concentrations of these antiarrhythmics may be decreased when co-administered with etravirine.
Etravirine and antiarrhythmics should be co-administered with caution. Drug concentration monitoring is recommended, if available.
Anticoagulant:
warfarin
‚ÜĎ anticoagulants
Warfarin concentrations may be increased when co-administered with etravirine. The international normalized ratio (INR) should be monitored when warfarin is combined with etravirine.
Anticonvulsants:
carbamazepine
phenobarbital
phenytoin
‚Üď etravirine
Carbamazepine, phenobarbital and phenytoin are inducers of CYP450 enzymes.
Etravirine should not be used in combination with carbamazepine, phenobarbital, or phenytoin as co-administration may cause significant decreases in etravirine plasma concentrations and loss of therapeutic effect of etravirine.
Antifungals:
fluconazole*
‚ÜĎ etravirine
‚ÜĒ fluconazole
Co-administration of etravirine and fluconazole significantly increased etravirine exposures. The amount of safety data at these increased etravirine exposures is limited, therefore, etravirine and fluconazole should be co-administered with caution. No dose adjustment of etravirine or fluconazole is needed.
voriconazole*
‚ÜĎ voriconazole
Co-administration of etravirine and voriconazole significantly increased etravirine exposures.
The amount of safety data at these increased etravirine exposures is limited, therefore, etravirine and voriconazole should be co-administered with caution. No dose adjustment of etravirine or voriconazole is needed.
Antifungals:
itraconazole
ketoconazole
posaconazole
‚ÜĎ etravirine
‚Üď itraconazole
‚Üď ketoconazole
‚ÜĒ posaconazole
Posaconazole, a potent inhibitor of CYP3A4, may increase plasma concentrations of etravirine. Itraconazole and ketoconazole are potent inhibitors as well as substrates of CYP3A4. Concomitant systemic use of itraconazole or ketoconazole and etravirine may increase plasma concentrations of etravirine.
Simultaneously, plasma concentrations of itraconazole or ketoconazole may be decreased by etravirine. Dose adjustments for itraconazole, ketoconazole or posaconazole may be necessary depending on the other co-administered drugs.
Antiinfective:
clarithromycin*
‚ÜĎ etravirine
‚Üď clarithromycin
‚ÜĎ 14-OH-clarithromycin
Clarithromycin exposure was decreased by etravirine; however, concentrations of the active metabolite, 14-hydroxy-clarithromycin, were increased. Because 14-hydroxy-clarithromycin has reduced activity against Mycobacterium avium complex (MAC), overall activity against this pathogen may be altered.
Alternatives to clarithromycin, such as azithromycin, should be considered for the treatment of MAC.
Antimalarial:
artemether/lumefantrine*
‚ÜĒ etravirine
‚Üď artemether
‚Üď dihydroartemisinin
‚Üď lumefantrine
Caution is warranted when co-administering etravirine and artemether/lumefantrine as it is unknown whether the decrease in exposure of artemether or its active metabolite, dihydroartemisinin, could result in decreased antimalarial efficacy. No dose adjustment is needed for etravirine.
Antimycobacterials:
rifampin
rifapentine
‚Üď etravirine
Rifampin and rifapentine are potent inducers of CYP450 enzymes. Etravirine should not be used with rifampin or rifapentine as co-administration may cause significant decreases in etravirine plasma concentrations and loss of therapeutic effect of etravirine.
Antimycobacterial:
rifabutin*
‚Üď etravirine
‚Üď rifabutin
‚Üď 25-O-desacetylrifabutin
If etravirine is NOT co-administered with a protease inhibitor/ritonavir, then rifabutin at a dose of 300 mg once daily is recommended.
If etravirine is co-administered with darunavir/ritonavir, lopinavir/ritonavir or saquinavir/ritonavir, then rifabutin should not be co-administered due to the potential for significant reductions in etravirine exposure.
Benzodiazepine:
diazepam
‚ÜĎ diazepam
Concomitant use of etravirine with diazepam may increase plasma concentrations of diazepam. A decrease in diazepam dose may be needed.
Corticosteroid:
dexamethasone (systemic)
‚Üď etravirine
Systemic dexamethasone induces CYP3A and can decrease etravirine plasma concentrations. This may result in loss of therapeutic effect of etravirine. Systemic dexamethasone should be used with caution or alternatives should be considered, particularly for long-term use.
Herbal products:
St. John's wort (Hypericum perforatum)
‚Üď etravirine
Concomitant use of etravirine with products containing St. John’s wort may cause significant decreases in etravirine plasma concentrations and loss of therapeutic effect of etravirine. Etravirine and products containing St. John’s wort should not be co-administered.
Hepatitis C virus (HCV) direct-acting antivirals:
daclatasvir
‚Üď daclatasvir
Co-administration of etravirine with daclatasvir may decrease daclatasvir concentrations. Increase the daclatasvir dose to 90 mg once daily.
elbasvir/grazoprevir
‚Üď elbasvir
‚Üď grazoprevir
Co-administration of etravirine with elbasvir/grazoprevir may decrease elbasvir and grazoprevir concentrations, leading to reduced therapeutic effect of elbasvir/grazoprevir.
Co-administration is not recommended.
simeprevir
‚Üď simeprevir
Co-administration of etravirine with simeprevir may decrease simeprevir concentrations. Co-administration is not recommended.
HMG-CoA reductase inhibitors:
atorvastatin*
‚ÜĒ etravirine
‚Üď atorvastatin
‚ÜĎ 2-OH-atorvastatin
The combination of etravirine and atorvastatin can be given without dose adjustments, however, the dose of atorvastatin may need to be altered based on clinical response.
pravastatin
rosuvastatin
‚ÜĒ etravirine
‚ÜĒ pravastatin
‚ÜĒ rosuvastatin
No interaction between pravastatin, rosuvastatin and etravirine is expected.
lovastatin
simvastatin
‚Üď lovastatin
‚Üď simvastatin
Lovastatin and simvastatin are CYP3A substrates and co-administration with etravirine may result in lower plasma concentrations of the HMG-CoA reductase inhibitor.
fluvastatin
pitavastatin
‚ÜĎ fluvastatin
‚ÜĎ pitavastatin
Fluvastatin and pitavastatin are metabolized by CYP2C9 and co-administration with etravirine may result in higher plasma concentrations of the HMG-CoA reductase inhibitor. Dose adjustments for these HMG-CoA reductase inhibitors may be necessary.
Immunosuppressants:
cyclosporine
sirolimus
tacrolimus
‚Üď immunosuppressant
Etravirine and systemic immunosuppressants should be co-administered with caution because plasma concentrations of cyclosporine, sirolimus, or tacrolimus may be affected.
Narcotic analgesics/treatment of opioid dependence:
buprenorphine
buprenorphine/naloxone*
methadone*
‚ÜĒ etravirine
‚Üď buprenorphine
‚ÜĒ norbuprenorphine
‚ÜĒ methadone
Etravirine and buprenorphine (or buprenorphine/naloxone) can be co-administered without dose adjustments, however, clinical monitoring for withdrawal symptoms is recommended as buprenorphine (or buprenorphine/naloxone) maintenance therapy may need to be adjusted in some patients. Etravirine and methadone can be co-administered without dose adjustments, however, clinical monitoring for withdrawal symptoms is recommended as methadone maintenance therapy may need to be adjusted in some patients.
Phosphodiesterase type 5 (PDE-5) inhibitors:
sildenafil*
tadalafil
vardenafil
‚Üď sildenafil
‚Üď N-desmethyl-sildenafil
Etravirine and sildenafil can be co-administered without dose adjustments, however, the dose of sildenafil may need to be altered based on clinical effect.
Platelet aggregation inhibitors:
clopidogrel
‚Üď clopidogrel
(active) metabolite
Activation of clopidogrel to its active metabolite may be decreased when clopidogrel is co-administered with etravirine. Alternatives to clopidogrel should be considered.
‚ÜĎ = increase; ‚Üď = decrease; ‚ÜĒ = no change
* The interaction between etravirine and the drug was evaluated in a clinical study. All other drug interactions shown are predicted.
† The reference for etravirine exposure is the pharmacokinetic parameters of etravirine in the presence of darunavir/ritonavir.
7.4 Drugs Without Clinically SignificantInteractions with Etravirine
In addition to the drugs included in Table 4, the interaction between etravirine and the following drugs were evaluated in clinical studies and no dose adjustment is needed for either drug [see Clinical Pharmacology (12.3)]: didanosine, enfuvirtide (ENF), ethinylestradiol/norethindrone, omeprazole, paroxetine, raltegravir, ranitidine, and tenofovir disoproxil fumarate.
8 Use In Specific Populations
- Lactation: Breastfeeding is not recommended due to the potential for HIV-1 transmission.
(8.2)
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ (etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to etravirine during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
Prospective pregnancy data from clinical trials and the APR are not sufficient to adequately assess the risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Etravirine use during pregnancy has been evaluated in a limited number of individuals as reported by the APR, and available data show 1 birth defect in 66 first trimester exposures to etravirine-containing regimens (see Data).
The estimated background rate for major birth defects is 2.7% in the U.S. reference population of the Metropolitan Atlanta Congenital Defects Program (MACDP). The rate of miscarriage is not reported in the APR. The estimated background rate of miscarriage in clinically recognized pregnancies in the U.S. general population is 15% to 20%. The background risk of major birth defects and miscarriage for the indicated population is unknown.
In animal reproduction studies, no adverse developmental effects were observed with orally administered etravirine at exposures equivalent to those at the maximum recommended human dose (MRHD) of 400 mg daily (see Data).
Data
Human Data
Based on prospective reports to the APR of 116 live births following exposure to etravirine-containing regimens during pregnancy (including 66 exposed in the first trimester and 38 exposed in the second/third trimester), the number of birth defects in live births for etravirine was 1 out of 66 with first trimester exposure and 0 out of 38 with second/third trimester exposure. Prospective reports from the APR of overall major birth defects in pregnancies exposed to etravirine are compared with a U.S. background major birth defect rate. Methodological limitations of the APR include the use of MACDP as the external comparator group. Limitations of using an external comparator include differences in methodology and populations, as well as confounding due to the underlying disease; these limitations preclude an accurate comparison of outcomes.
Etravirine (200 mg twice daily) in combination with other antiretroviral agents was evaluated in a clinical trial enrolling 15 pregnant subjects during the second and third trimesters of pregnancy and postpartum. Thirteen subjects completed the trial through postpartum period (6 to 12 weeks after delivery). The pharmacokinetic data demonstrated that exposure to total etravirine was generally higher during pregnancy compared with postpartum [see Clinical Pharmacology (12.3)].
Among subjects who were virologically suppressed (HIV-1 RNA less than 50 copies/mL) at baseline (9/13), virologic suppression was maintained through the third trimester and postpartum period. Among subjects with HIV-1 RNA greater than 50 copies/mL and less than 400 copies/mL at baseline (3/13), viral loads remained less than 400 copies/mL. In one subject with HIV-1 RNA greater than 1,000 copies/mL at baseline (1/13), HIV-1 RNA remained greater than 1,000 copies/mL during the study period. Thirteen infants were born to 13 HIV-infected pregnant individuals in this study. HIV-1 test results were not available for 2 infants. Among the eleven infants with HIV-1 test results available, who were born to 11 HIV-infected pregnant individuals who completed the study, all had test results that were negative for HIV-1 at the time of delivery. No unexpected safety findings were observed compared with the known safety profile of etravirine in non-pregnant adults.
Animal Data
Reproductive and developmental toxicity studies were performed in rats (at 250, 500 and 1,000 mg/kg/day) and rabbits (at 125, 250 and 375 mg/kg/day) administered etravirine on gestation days 6 through 16, and 6 through 19, respectively. In both species, no treatment-related embryo-fetal effects were observed. In addition, no treatment-related effects were observed in a pre- and postnatal development study performed in rats administered oral doses up to 500 mg/kg/day on gestation days 7 through lactation day 7. The systemic drug exposures achieved at the high dose in these animal studies were equivalent to those at the MRHD.
8.2 Lactation
Risk Summary
The Centers for Disease Control and Prevention recommend that HIV-1-infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV.
Based on limited data, etravirine has been shown to be present in human breast milk. There are no data on the effects of etravirine on the breastfed infant, or the effects of etravirine on milk production.
Because of the potential for (1) HIV-1 transmission (in HIV-negative infants), (2) developing viral resistance (in HIV-positive infants) and (3) adverse reactions in breastfed infants similar to those seen in adults, instruct mothers not to breastfeed if they are receiving etravirine.
8.4 Pediatric Use
The safety and effectiveness of etravirine have been established for the treatment of HIV-infected pediatric patients from 6 years of age to less than 18 years [see Indications and Usage (1) and Dosage and Administration (2.3)]. Use of etravirine in pediatric patients 6 years to less than 18 years of age is supported by evidence from adequate and well-controlled studies of etravirine in adults with additional data from a Phase 2 trial in treatment-experienced pediatric subjects, TMC125-C213, 6 years to less than 18 years of age (N=101). The study was an open-label, single arm trial of etravirine plus an optimized background regimen. In the clinical trial, the safety, pharmacokinetics, and efficacy were comparable to that observed in adults except for rash (greater than or equal to Grade 2) which was observed more frequently in pediatric subjects [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14.2)]. Postmarketing reports of Stevens-Johnson syndrome in pediatric patients receiving etravirine have been reported [see Warnings and Precautions (5.1), and Adverse Reactions (6.2) ].
Treatment with etravirine is not recommended in pediatric patients less than 2 years of age [see Clinical Pharmacology (12.3)].
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ (etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
8.5 Geriatric Use
Clinical studies of etravirine did not include sufficient numbers of subjects aged 65 years of age and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger subjects. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy [see Clinical Pharmacology (12.3)].
8.6 HepaticImpairment
No dose adjustment of etravirine is required in patients with mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment. The pharmacokinetics of etravirine have not been evaluated in patients with severe hepatic impairment (Child-Pugh Class C) [see Clinical Pharmacology (12.3)].
8.7 RenalImpairment
Since the renal clearance of etravirine is negligible (less than 1.2%), a decrease in total body clearance is not expected in patients with renal impairment. No dose adjustments are required in patients with renal impairment. As etravirine is highly bound to plasma proteins, it is unlikely that it will be significantly removed by hemodialysis or peritoneal dialysis [see Clinical Pharmacology (12.3)].
10 Overdosage
There is no specific antidote for overdose with etravirine. Human experience of overdose with etravirine is limited. The highest dose studied in healthy volunteers was 400 mg once daily. Treatment of overdose with etravirine consists of general supportive measures including monitoring of vital signs and observation of the clinical status of the patient. Because etravirine is highly protein bound, dialysis is unlikely to result in significant removal of the active substance.
11 Description
Etravirine is a non-nucleoside reverse transcriptase inhibitor (NNRTI) of human immunodeficiency virus type 1 (HIV-1).
The chemical name for etravirine is 4-[[6-amino-5-bromo-2-[(4-cyanophenyl) amino]-4-pyrimidinyl] oxy]-3,5-dimethylbenzonitrile. Its molecular formula is C20H15BrN6O and its molecular weight is 435.28 g/mol. Etravirine has the following structural formula:
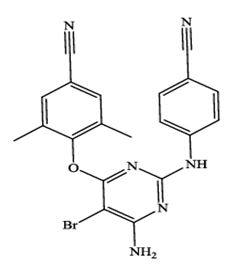
Etravirine is a white to slightly yellowish-brown powder. Etravirine is practically insoluble in water and freely soluble in some organic solvents like N,N-dimethylformamide and tetrahydrofuran.
Etravirine tablets are for oral administration. Each etravirine tablet contains 25 mg, 100 mg or 200 mg of etravirine. It also contains the inactive ingredients: croscarmellose sodium, crospovidone (type A), colloidal silicon dioxide, hypromellose, low-substituted hydroxy propyl cellulose, magnesium stearate and microcrystalline cellulose.
12 Clinical Pharmacology
12.1 Mechanism of Action
Etravirine is an antiretroviral drug [see Microbiology (12.4)].
12.2 Pharmacodynamics
Cardiac Electrophysiology
In a thorough QT/QTc study in 41 healthy subjects, etravirine 200 mg twice daily or 400 mg once daily did not affect the QT/QTc interval.
12.3 Pharmacokinetics
The pharmacokinetic properties of etravirine were determined in healthy adult subjects and in treatment-experienced HIV-1-infected adult and pediatric subjects. The systemic exposures (AUC) to etravirine were lower in HIV-1-infected subjects (Table 5) than in healthy subjects.
Table 5: Population Pharmacokinetic Estimates of Etravirine 200 mg Twice Daily in HIV-1-Infected Adult Subjects (Integrated Data from Phase 3 Trials at Week 48)*
Parameter
Etravirine
N=575
AUC12h (ng‚ÄĘh/mL)
Geometric mean ¬Ī standard deviation
4,522 ¬Ī 4,710
Median (range)
4,380 (458 to 59,084)
C0h (ng/mL)
Geometric mean ¬Ī standard deviation
297 ¬Ī 391
Median (range)
298 (2 to 4,852)
* All HIV-1-infected subjects enrolled in Phase 3 clinical trials received darunavir/ritonavir 600/100 mg twice daily as part of their background regimen. Therefore, the pharmacokinetic parameter estimates shown in Table 5 account for reductions in the pharmacokinetic parameters of etravirine due to co-administration of etravirine with darunavir/ritonavir.
Note: The median protein binding adjusted EC50 for MT4 cells infected with HIV-1/IIIB in vitro equals 4 ng/mL.
Absorption and Bioavailability
Following oral administration, etravirine was absorbed with a Tmax of about 2.5 to 4 hours. The absolute oral bioavailability of etravirine is unknown.
In healthy subjects, the absorption of etravirine is not affected by co-administration of oral ranitidine or omeprazole, drugs that increase gastric pH.
Effects of Food on Oral Absorption
The systemic exposure (AUC) to etravirine was decreased by about 50% when etravirine tablet was administered under fasting conditions, as compared to when etravirine tablet was administered following a meal. Within the range of meals studied, the systemic exposures to etravirine were similar. The total caloric content of the various meals evaluated ranged from 345 kilocalories (17 grams fat) to 1,160 kilocalories (70 grams fat).
Distribution
Etravirine is about 99.9% bound to plasma proteins, primarily to albumin (99.6%) and alpha 1-acid glycoprotein (97.66% to 99.02%) in vitro. The distribution of etravirine into compartments other than plasma (e.g., cerebrospinal fluid, genital tract secretions) has not been evaluated in humans.
Metabolism
In vitro experiments with human liver microsomes (HLMs) indicate that etravirine primarily undergoes metabolism by CYP3A, CYP2C9, and CYP2C19 enzymes. The major metabolites, formed by methyl hydroxylation of the dimethylbenzonitrile moiety, were at least 90% less active than etravirine against wild-type HIV in cell culture.
Elimination
After single dose oral administration of 800 mg 14C-etravirine, 93.7% and 1.2% of the administered dose of 14C-etravirine was recovered in the feces and urine, respectively. Unchanged etravirine accounted for 81.2% to 86.4% of the administered dose in feces. Unchanged etravirine was not detected in urine. The mean (¬Ī standard deviation) terminal elimination half-life of etravirine was about 41 (¬Ī 20) hours.
Specific Populations
Geriatric Patients
Population pharmacokinetic analysis in HIV-infected subjects showed that etravirine pharmacokinetics are not considerably different within the age range (18 to 77 years) evaluated [see Use in Specific Populations (8.5)].
Pediatric Patients
The pharmacokinetics of etravirine in 101 treatment-experienced HIV-1-infected pediatric subjects, 6 years to less than 18 years of age showed that the administered weight-based dosages resulted in etravirine exposure comparable to that in adults receiving etravirine 200 mg twice daily [see Dosage and Administration (2.3)]. The pharmacokinetic parameters for etravirine (AUC12h and C0h) are summarized in Table 6.
Table 6: Pharmacokinetic Parameters for Etravirine in Treatment-Experienced HIV-1-Infected Pediatric Subjects 6 Years to Less Than 18 Years of Age (TMC125-C213 [Population PK])
Study
TMC125-C213
Age Range (years)
(6 years to less than 18 years)
Parameter
N=101
AUC12h (ng‚ÄĘh/mL)
Geometric mean ¬Ī standard deviation
3,742 ¬Ī 4,314
Median (range)
4,499 (62 to 28,865)
C0h (ng/mL)
Geometric mean ¬Ī standard deviation
205 ¬Ī 342
Median (range)
287 (2 to 2,276)
The pharmacokinetics and dose of etravirine in pediatric subjects less than 2 years of age have not been established [see Use in Specific Populations (8.4)].
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ (etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Male and Female Patients
No significant pharmacokinetic differences have been observed between males and females.
Racial or Ethnic Groups
Population pharmacokinetic analysis of etravirine in HIV-infected subjects did not show an effect of race on exposure to etravirine.
Patients with Renal Impairment
The pharmacokinetics of etravirine have not been studied in patients with renal impairment. The results from a mass balance study with 14C-etravirine showed that less than 1.2% of the administered dose of etravirine is excreted in the urine as metabolites. No unchanged drug was detected in the urine. As etravirine is highly bound to plasma proteins, it is unlikely that it will be significantly removed by hemodialysis or peritoneal dialysis [see Use in Specific Populations (8.7)].
Patients with Hepatic Impairment
Etravirine is primarily metabolized by the liver. The steady-state pharmacokinetic parameters of etravirine were similar after multiple dose administration of etravirine to subjects with normal hepatic function (16 subjects), mild hepatic impairment (Child-Pugh Class A, 8 subjects), and moderate hepatic impairment (Child-Pugh Class B, 8 subjects). The effect of severe hepatic impairment on the pharmacokinetics of etravirine has not been evaluated [see Use in Specific Populations (8.6)].
Pregnancy and Postpartum
After intake of etravirine 200 mg twice daily in combination with other antiretroviral agents (13 subjects with 2 NRTIs, 1 subject with 2 NRTIs + lopinavir + ritonavir, 1 subject with 2 NRTIs + raltegravir), based on intra-individual comparison, the Cmax and AUC12h of total etravirine were 23% to 42% higher during pregnancy compared with postpartum (6 to 12 weeks). The Cmin of total etravirine was 78 to 125% higher during pregnancy compared with postpartum (6 to 12 weeks), while two subjects had Cmin < 10 ng/mL in the postpartum period (6 to 12 weeks) [Cmin of total etravirine was 11% to 16% higher when these 2 subjects are excluded] (see Table 7) [see Use in Specific Populations (8.1)]. Increased etravirine exposures during pregnancy are not considered clinically significant. The protein binding of etravirine was similar (> 99%) during the second trimester, third trimester, and postpartum period.
Table 7: Pharmacokinetic Results of Total Etravirine After Administration of Etravirine 200 mg Twice Daily as Part of an Antiretroviral Regimen, During the 2nd Trimester of Pregnancy, the 3rd Trimester of Pregnancy, and Postpartum.
Parameter
Mean ¬Ī SD (median)
Postpartum
N=10
2nd Trimester
N=13
3rd Trimester
N=10*
Cmin, ng/mL
269 ¬Ī 182 (284)‚Ć
383 ¬Ī 210 (346)
349 ¬Ī 103 (371)
Cmax, ng/mL
569 ¬Ī 261 (528)
774 ¬Ī 300 (828)
785 ¬Ī 238 (694)
AUC12h, ng‚ÄĘh/mL
5,004 ¬Ī 2521
(5,246)
6,617 ¬Ī 2766
(6,836)
6,846 ¬Ī 1482
(6,028)
*n=9 for AUC12h
‚Ć Two subjects had Cmin <10 ng/mL, Cmin was 334 ¬Ī 135 (315) in the postpartum period when these subjects were excluded from the descriptive analysis (N=8).
Patients with Hepatitis B and/or Hepatitis C Virus Co-Infection
Population pharmacokinetic analysis of the TMC125-C206 and TMC125-C216 trials showed reduced clearance for etravirine in HIV-1-infected subjects with hepatitis B and/or C virus co-infection. Based upon the safety profile of etravirine [see Adverse Reactions (6)], no dose adjustment is necessary in patients co-infected with hepatitis B and/or C virus.
Drug Interactions
Etravirine is a substrate of CYP3A, CYP2C9, and CYP2C19. Therefore, co-administration of etravirine with drugs that induce or inhibit CYP3A, CYP2C9, and CYP2C19 may alter the therapeutic effect or adverse reaction profile of etravirine.
Etravirine is an inducer of CYP3A and inhibitor of CYP2C9, CYP2C19 and P-gp. Therefore, co-administration of drugs that are substrates of CYP3A, CYP2C9 and CYP2C19 or are transported by P-gp with etravirine may alter the therapeutic effect or adverse reaction profile of the co-administered drug(s).
Drug interaction studies were performed with etravirine and other drugs likely to be co-administered and some drugs commonly used as probes for pharmacokinetic interactions. The effects of co-administration of other drugs on the AUC, Cmax, and Cmin values of etravirine are summarized in Table 8 (effect of other drugs on etravirine). The effect of co-administration of etravirine on the AUC, Cmax, and Cmin values of other drugs are summarized in Table 9 (effect of etravirine on other drugs). For information regarding clinical recommendations, [see Drug Interactions (7)].
Table 8: Drug Interactions: Pharmacokinetic Parameters for Etravirine in the Presence of Co-administered Drugs
Co-administered Drug
Dose/Schedule of Co-administered Drug
N
Exposure
Mean Ratio of Etravirine
Pharmacokinetic Parameters
90% CI; No Effect = 1.00
Cmax
AUC
Cmin
Co-administration with HIV protease inhibitors (PIs)
Atazanavir
400 mg once daily
14
‚ÜĎ
1.47
(1.36 to 1.59)
1.50
(1.41 to 1.59)
1.58
(1.46 to 1.70)
Atazanavir/ritonavir*
300 mg/100 mg once daily
14
‚ÜĎ
1.30
(1.17 to 1.44)
1.30
(1.18 to 1.44)
1.26
(1.12 to 1.42)
Darunavir/ritonavir
600 mg/100 mg twice daily
14
‚Üď
0.68
(0.57 to 0.82)
0.63
(0.54 to 0.73)
0.51
(0.44 to 0.61)
Lopinavir/ritonavir
(tablet)
400 mg/100 mg twice daily
16
‚Üď
0.70
(0.64 to 0.78)
0.65
(0.59 to 0.71)
0.55
(0.49 to 0.62)
Ritonavir
600 mg twice daily
11
‚Üď
0.68
(0.55 to 0.85)
0.54
(0.41 to 0.73)
N.A.
Saquinavir/ritonavir
1,000 mg/100 mg twice daily
14
‚Üď
0.63
(0.53 to 0.75)
0.67
(0.56 to 0.80)
0.71
(0.58 to 0.87)
Tipranavir/ritonavir
500 mg/200 mg twice daily
19
‚Üď
0.29
(0.22 to 0.40)
0.24
(0.18 to 0.33)
0.18
(0.13 to 0.25)
Co-administration with nucleoside reverse transcriptase inhibitors (NRTIs)
Didanosine
400 mg once daily
15
‚ÜĒ
1.16
(1.02 to 1.32)
1.11
(0.99 to 1.25)
1.05
(0.93 to 1.18)
Tenofovir disoproxil fumarate
300 mg once daily
23
‚Üď
0.81
(0.75 to 0.88)
0.81
(0.75 to 0.88)
0.82
(0.73 to 0.91)
Co-administration with CCR5 antagonists
Maraviroc
300 mg twice daily
14
‚ÜĒ
1.05
(0.95 to 1.17)
1.06
(0.99 to 1.14)
1.08
(0.98 to 1.19)
Maraviroc (when co-administered with darunavir/ritonavir)†
150 mg/600 mg/100 mg twice daily
10
‚ÜĒ
1.08
(0.98 to 1.20)
1.00
(0.86 to 1.15)
0.81
(0.65 to 1.01)
Co-administration with integrase strand transfer inhibitors
Raltegravir
400 mg twice daily
19
‚ÜĒ
1.04
(0.97 to 1.12)
1.10
(1.03 to 1.16)
1.17
(1.10 to 1.26)
Co-administration with other drugs
Artemether/lumefantrine
80 mg/480 mg, 6 doses at 0, 8, 24, 36, 48, and 60 hours
14
‚ÜĒ
1.11
(1.06 to 1.17)
1.10
(1.06 to 1.15)
1.08
(1.04 to 1.14)
Atorvastatin
40 mg once daily
16
‚ÜĒ
0.97
(0.93 to 1.02)
1.02
(0.97 to 1.07)
1.10
(1.02 to 1.19)
Clarithromycin
500 mg twice daily
15
‚ÜĎ
1.46
(1.38 to 1.56)
1.42
(1.34 to 1.50)
1.46
(1.36 to 1.58)
Fluconazole
200 mg once daily in the morning
16
‚ÜĎ
1.75
(1.60 to 1.91)
1.86
(1.73 to 2.00)
2.09
(1.90 to 2.31)
Omeprazole
40 mg once daily
18
‚ÜĎ
1.17
(0.96 to 1.43)
1.41
(1.22 to 1.62)
N.A.
Paroxetine
20 mg once daily
16
‚ÜĒ
1.05
(0.96 to 1.15)
1.01
(0.93 to 1.10)
1.07
(0.98 to 1.17)
Ranitidine
150 mg twice daily
18
‚Üď
0.94
(0.75 to 1.17)
0.86
(0.76 to 0.97)
N.A.
Rifabutin
300 mg once daily
12
‚Üď
0.63
(0.53 to 0.74)
0.63
(0.54 to 0.74)
0.65
(0.56 to 0.74)
Voriconazole
200 mg twice daily
16
‚ÜĎ
1.26
(1.16 to 1.38)
1.36
(1.25 to 1.47)
1.52
(1.41 to 1.64)
CI = Confidence Interval; N = number of subjects with data; N.A. = not available; ‚ÜĎ = increase; ‚Üď = decrease; ‚ÜĒ = no change
* The systemic exposure of etravirine when co-administered with atazanavir/ritonavir in HIV infected subjects is similar to exposures of etravirine observed in the Phase 3 trials after co-administration of etravirine and darunavir/ritonavir (as part of the background regimen).
† The reference for etravirine exposure is the pharmacokinetic parameters of etravirine in the presence of darunavir/ritonavir.
Table 9: Drug Interactions: Pharmacokinetic Parameters for Co-administered Drugs in the Presence of Etravirine
Co-administered Drug
Dose/Schedule of Co-administered Drug
N
Exposure
Mean Ratio of Co-administered Drug
Pharmacokinetic Parameters
90% CI; No effect = 1.00
Cmax
AUC
Cmin
Co-administration with HIV protease inhibitors (PIs)
Atazanavir
400 mg once daily
14
‚Üď
0.97
(0.73 to 1.29)
0.83
(0.63 to 1.09)
0.53
(0.38 to 0.73)
Atazanavir/ritonavir
300 mg/100 mg once daily
13
‚Üď
0.97
(0.89 to 1.05)
0.86
(0.79 to 0.93)
0.62
(0.55 to 0.71)
Atazanavir/ritonavir*
300 mg/100 mg once daily
20
‚Üď
0.96
(0.80 to 1.16)
0.96
(0.76 to 1.22)
0.82
(0.55 to 1.22)
Darunavir/ritonavir
600 mg/100 mg twice daily
15
‚ÜĒ
1.11
(1.01 to 1.22)
1.15
(1.05 to 1.26)
1.02
(0.90 to 1.17)
Fosamprenavir/ritonavir
700 mg/100 mg twice daily
8
‚ÜĎ
1.62
(1.47 to 1.79)
1.69
(1.53 to 1.86)
1.77
(1.39 to 2.25)
Lopinavir/ritonavir
(tablet)
400 mg/100 mg twice daily
16
‚ÜĒ
0.89
(0.82 to 0.96)
0.87
(0.83 to 0.92)
0.80
(0.73 to 0.88)
Saquinavir/ritonavir
1,000 mg/100 mg twice daily
15
‚ÜĒ
1.00
(0.70 to 1.42)
0.95
(0.64 to 1.42)
0.80
(0.46 to 1.38)
Tipranavir/ritonavir
500 mg/200 mg twice daily
19
‚ÜĎ
1.14
(1.02 to 1.27)
1.18
(1.03 to 1.36)
1.24
(0.96 to 1.59)
Co-administration with nucleoside reverse transcriptase inhibitors (NRTIs)
Didanosine
400 mg once daily
14
‚ÜĒ
0.91
(0.58 to 1.42)
0.99
(0.79 to 1.25)
N.A.
Tenofovir disoproxil fumarate
300 mg once daily
19
‚ÜĒ
1.15
(1.04 to 1.27)
1.15
(1.09 to 1.21)
1.19
(1.13 to 1.26)
Co-administration with CCR5 antagonists
Maraviroc
300 mg twice daily
14
‚Üď
0.40
(0.28 to 0.57)
0.47
(0.38 to 0.58)
0.61
(0.53 to 0.71)
Maraviroc (when co-administered with darunavir/ritonavir)†
150 mg/600 mg/100 mg twice daily
10
‚ÜĎ
1.77
(1.20 to 2.60)
3.10
(2.57 to 3.74)
5.27
(4.51 to 6.15)
Co-administration with integrase strand transfer inhibitors
Dolutegravir
50 mg once daily
16
‚Üď
0.48
(0.43 to 0.54)
0.29
(0.26 to 0.34)
0.12
(0.09 to 0.16)
Dolutegravir (when co-administered with darunavir/ritonavir)
50 mg once daily + 600/100 mg twice daily
9
‚Üď
0.88
(0.78 to 1.00)
0.75
(0.69 to 0.81)
0.63
(0.52 to 0.76)
Dolutegravir (when co-administered with lopinavir/ritonavir
50 mg once daily + 400/100 mg twice daily
8
‚ÜĒ
1.07
(1.02 to 1.13)
1.11
(1.02 to 1.20)
1.28
(1.13 to 1.45)
Raltegravir
400 mg twice daily
19
‚Üď
0.89
(0.68 to 1.15)
0.90
(0.68 to 1.18)
0.66
(0.34 to 1.26)
Co-administration with other drugs
Artemether
80 mg/480 mg, 6 doses at 0, 8, 24, 36, 48, and 60 hours
15
‚Üď
0.72
(0.55 to 0.94)
0.62
(0.48 to 0.80)
0.82
(0.67 to 1.01)
Dihydroartemisinin
15
‚Üď
0.84
(0.71 to 0.99)
0.85
(0.75 to 0.97)
0.83
(0.71 to 0.97)
Lumefantrine
15
‚Üď
1.07
(0.94 to 1.23)
0.87
(0.77 to 0.98)
0.97
(0.83 to 1.15)
Atorvastatin
40 mg once daily
16
‚Üď
1.04
(0.84 to 1.30)
0.63
(0.58 to 0.68)
N.A.
2-hydroxy-atorvastatin
16
‚ÜĎ
1.76
(1.60 to 1.94)
1.27
(1.19 to 1.36)
N.A.
Buprenorphine
Individual dose regimen ranging from 4/1 mg to 16/4 mg once daily
16
‚Üď
0.89
(0.76 to 1.05)
0.75
(0.66 to 0.84)
0.60
(0.52 to 0.68)
Norbuprenorphine
16
‚ÜĒ
1.08
(0.95 to 1.23)
0.88
(0.81 to 0.96)
0.76
(0.67 to 0.87)
Clarithromycin
500 mg twice daily
15
‚Üď
0.66
(0.57 to 0.77)
0.61
(0.53 to 0.69)
0.47
(0.38 to 0.57)
14-hydroxy-clarithromycin
15
‚ÜĎ
1.33
(1.13 to 1.56)
1.21
(1.05 to 1.39)
1.05
(0.90 to 1.22)
Digoxin
0.5 mg single-dose
16
‚ÜĎ
1.19
(0.96 to 1.49)
1.18
(0.90 to 1.56)
N.A.
Ethinylestradiol
0.035 mg once daily
16
‚ÜĎ
1.33
(1.21 to 1.46)
1.22
(1.13 to 1.31)
1.09
(1.01 to 1.18)
Norethindrone
1 mg once daily
16
‚ÜĒ
1.05
(0.98 to 1.12)
0.95
(0.90 to 0.99)
0.78
(0.68 to 0.90)
Fluconazole
200 mg once daily in the morning
15
‚ÜĒ
0.92
(0.85 to 1.00)
0.94
(0.88 to 1.01)
0.91
(0.84 to 0.98)
R(-) Methadone
Individual dose regimen ranging from 60 to 130 mg/day
16
‚ÜĒ
1.02
(0.96 to 1.09)
1.06
(0.99 to 1.13)
1.10
(1.02 to 1.19)
S(+) Methadone
16
‚ÜĒ
0.89
(0.83 to 0.97)
0.89
(0.82 to 0.96)
0.89
(0.81 to 0.98)
Paroxetine
20 mg once daily
16
‚ÜĒ
1.06
(0.95 to 1.20)
1.03
(0.90 to 1.18)
0.87
(0.75 to 1.02)
Rifabutin
300 mg once daily
12
‚Üď
0.90
(0.78 to 1.03)
0.83
(0.75 to 0.94)
0.76
(0.66 to 0.87)
25-O-desacetylrifabutin
300 mg once daily
12
‚Üď
0.85
(0.72 to 1.00)
0.83
(0.74 to 0.92)
0.78
(0.70 to 0.87)
Sildenafil
50 mg single-dose
15
‚Üď
0.55
(0.40 to 0.75)
0.43
(0.36 to 0.51)
N.A.
N-desmethyl-sildenafil
15
‚Üď
0.75
(0.59 to 0.96)
0.59
(0.52 to 0.68)
N.A.
Voriconazole
200 mg twice daily
14
‚ÜĎ
0.95
(0.75 to 1.21)
1.14
(0.88 to 1.47)
1.23
(0.87 to 1.75)
CI = Confidence Interval; N = number of subjects with data; N.A. = not available; ‚ÜĎ = increase; ‚Üď = decrease; ‚ÜĒ = no change
* HIV-infected subjects
† compared to maraviroc 150 mg twice daily
12.4 Microbiology
Mechanism of Action
Etravirine is an NNRTI of HIV-1. Etravirine binds directly to reverse transcriptase (RT) and blocks the RNA-dependent and DNA-dependent DNA polymerase activities by causing a disruption of the enzyme's catalytic site. Etravirine does not inhibit the human DNA polymerases őĪ, ő≤, and ő≥.
Antiviral Activity in Cell Culture
Etravirine exhibited activity against laboratory strains and clinical isolates of wild-type HIV-1 in acutely infected T-cell lines, human peripheral blood mononuclear cells, and human monocytes/macrophages with median EC50 values ranging from 0.9 nM to 5.5 nM (i.e. 0.4 ng/mL to 2.4 ng/mL). Etravirine demonstrated antiviral activity in cell culture against a broad panel of HIV-1 group M isolates (subtype A, B, C, D, E, F, G) with EC50 values ranging from 0.29 nM to 1.65 nM and EC50 values ranging from 11.5 nM to 21.7 nM against group O primary isolates. Etravirine did not show antagonism when studied in combination with the following antiretroviral drugs‚ÄĒthe NNRTIs delavirdine, efavirenz, and nevirapine; the N(t)RTIs abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir, and zidovudine; the PIs amprenavir, atazanavir, darunavir, indinavir, lopinavir, nelfinavir, ritonavir, saquinavir, and tipranavir; the gp41 fusion inhibitor ENF; the integrase strand transfer inhibitor raltegravir and the CCR5 co-receptor antagonist maraviroc.
Resistance
In Cell Culture
Etravirine-resistant strains were selected in cell culture originating from wild-type HIV-1 of different origins and subtypes, as well as NNRTI resistant HIV-1. Development of reduced susceptibility to etravirine typically required more than one substitution in reverse transcriptase of which the following were observed most frequently: L100I, E138K, E138G, V179I, Y181C, and M230I.
In Treatment-Experienced Subjects
In the Phase 3 trials TMC125-C206 and TMC125-C216, substitutions that developed most commonly in subjects with virologic failure at Week 48 to the etravirine-containing regimen were V179F, V179I, and Y181C which usually emerged in a background of multiple other NNRTI resistance-associated substitutions. In all the trials conducted with etravirine in HIV-1 infected subjects, the following substitutions emerged most commonly: L100I, E138G, V179F, V179I, Y181C and H221Y. Other NNRTI-resistance-associated substitutions which emerged on etravirine treatment in less than 10% of the virologic failure isolates included K101E/H/P, K103N/R, V106I/M, V108I, Y181I, Y188L, V189I, G190S/C, N348I and R356K. The emergence of NNRTI substitutions on etravirine treatment contributed to decreased susceptibility to etravirine with a median fold-change in etravirine susceptibility of 40-fold from reference and a median fold-change of 6-fold from baseline.
Cross-Resistance
Cross-resistance among NNRTIs has been observed. Cross-resistance to delavirdine, efavirenz, and/or nevirapine is expected after virologic failure with an etravirine-containing regimen. Virologic failure on a rilpivirine-containing regimen with development of rilpivirine resistance is likely to result in cross-resistance to etravirine (see Treatment-Na√Įve HIV-1-Infected Subjects in the Phase 3 Trials for EDURANT (rilpivirine) below). Cross-resistance to etravirine has been observed after virologic failure on a doravirine-containing regimen with development of doravirine resistance. Some NNRTI-resistant viruses are susceptible to etravirine, but genotypic and phenotypic testing should guide the use of etravirine (see Baseline Genotype/Phenotype and Virologic Outcome Analyses below).
Site-Directed NNRTI Mutant Virus
Etravirine showed antiviral activity against 55 of 65 HIV-1 strains (85%) with single amino acid substitutions at RT positions associated with NNRTI resistance, including the most commonly found K103N. The single amino acid substitutions associated with an etravirine reduction in susceptibility greater than 3-fold were K101A, K101P, K101Q, E138G, E138Q, Y181C, Y181I, Y181T, Y181V, and M230L, and of these, the greatest reductions were Y181I (13-fold change in EC50 value) and Y181V (17-fold change in EC50 value). Mutant strains containing a single NNRTI resistance-associated substitution (K101P, K101Q, E138Q, or M230L) had cross-resistance between etravirine and efavirenz.
The majority (39 of 61; 64%) of the NNRTI mutant viruses with 2 or 3 amino acid substitutions associated with NNRTI resistance had decreased susceptibility to etravirine (fold-change greater than 3). The highest levels of resistance to etravirine were observed for HIV-1 harboring a combination of substitutions V179F + Y181C (187 fold-change), V179F + Y181I (123 fold-change), or V179F + Y181C + F227C (888 fold-change).
Clinical Isolates
Etravirine retained a fold-change less than or equal to 3 against 60% of 6171 NNRTI-resistant clinical isolates. In the same panel, the proportion of clinical isolates resistant to delavirdine, efavirenz and/or nevirapine (defined as a fold-change above their respective biological cutoff values in the assay) was 79%, 87%, and 95%, respectively. In TMC125-C206 and TMC125-C216, 34% of the baseline isolates had decreased susceptibility to etravirine (fold-change greater than 3) and 60%, 69%, and 78% of all baseline isolates were resistant to delavirdine, efavirenz, and nevirapine, respectively. Of subjects who received etravirine and were virologic failures in TMC125-C206 and TMC125-C216, 90%, 84%, and 96% of viral isolates obtained at the time of treatment failure were resistant to delavirdine, efavirenz, and nevirapine, respectively.
Treatment-Na√Įve HIV-1-Infected Subjects in the Phase 3 Trials for EDURANT (Rilpivirine)
There are currently no clinical data available on the use of etravirine in subjects who experienced virologic failure on a rilpivirine-containing regimen. However, in the rilpivirine adult clinical development program, there was evidence of phenotypic cross-resistance between rilpivirine and etravirine. In the pooled analyses of the Phase 3 clinical trials for rilpivirine, 38 rilpivirine virologic failure subjects had evidence of HIV-1 strains with genotypic and phenotypic resistance to rilpivirine. Of these subjects, 89% (34 subjects) of virologic failure isolates were cross-resistant to etravirine based on phenotype data. Consequently, it can be inferred that cross-resistance to etravirine is likely after virologic failure and development of rilpivirine resistance. Refer to the prescribing information for EDURANT (rilpivirine) for further information.
Baseline Genotype/Phenotype and Virologic Outcome Analyses
In TMC125-C206 and TMC125-C216, the presence at baseline of the substitutions L100I, E138A, I167V, V179D, V179F, Y181I, Y181V, or G190S was associated with a decreased virologic response to etravirine. Additional substitutions associated with a decreased virologic response to etravirine when in the presence of 3 or more additional 2008 IAS-USA defined NNRTI substitutions include A98G, K101H, K103R, V106I, V179T, and Y181C. The presence of K103N, which was the most prevalent NNRTI substitution in TMC125-C206 and TMC125-C216 at baseline, did not affect the response in the etravirine arm. Overall, response rates to etravirine decreased as the number of baseline NNRTI substitutions increased (shown as the proportion of subjects achieving viral load less than 50 plasma HIV RNA copies/mL at Week 48) (Table 10).
Table 10: Proportion of Subjects With Less Than 50 HIV-1 RNA Copies/mL at Week 48 by Baseline Number of IAS-USA-Defined NNRTI Substitutions* in the Non-VF Excluded Population of the Pooled TMC125-C206 and TMC125-C216
# IAS-USA-Defined NNRTI substitutions*
Etravirine
N=561
Re-used/not used
ENF
de novo ENF
All ranges
61% (254/418)
76% (109/143)
0
68% (52/76)
95% (20/21)
1
67% (72/107)
77% (24/31)
2
64% (75/118)
86% (38/44)
3
55% (36/65)
62% (16/26)
‚Č• 4
37% (19/52)
52% (11/21)
Placebo
N=592
All ranges
34% (147/435)
59% (93/157)
ENF: enfuvirtide
* 2008 IAS-USA defined substitutions = V90I, A98G, L100I, K101E/H/P, K103N, V106A/I/M, V108I, E138A, V179D/F/T, Y181C/I/V, Y188C/H/L, G190A/S, P225H, M230L
Response rates assessed by baseline etravirine phenotype are shown in Table 11. These baseline phenotype groups are based on the select subject populations in TMC125-C206 and TMC125-C216 and are not meant to represent definitive clinical susceptibility breakpoints for etravirine. The data are provided to give clinicians information on the likelihood of virologic success based on pre-treatment susceptibility to etravirine in treatment-experienced patients.
Table 11: Proportion of Subjects With Less Than 50 HIV-1 RNA Copies/mL at Week 48 by Baseline Phenotype and ENF Use in the Pooled TMC125-C206 and TMC125-C216*
Fold Change
Etravirine
N=559
Re-used/not used ENF
de novo ENF
Clinical response range
All ranges
61% (253/416)
76% (109/143)
Overall Response
0 to 3
69% (188/274)
83% (75/90)
Higher than Overall Response
> 3 to 13
50% (39/78)
66% (25/38)
Lower than Overall Response
> 13
41% (26/64)
60% (9/15)
Lower than Overall Response
Placebo
N=583
All ranges
34% (145/429)
60% (92/154)
ENF: enfuvirtide
* Non-VF excluded analysis
The proportion of virologic responders (viral load less than 50 HIV-1 RNA copies/mL) by the phenotypic susceptibility score (PSS) of the background therapy, including ENF, is shown in Table 12.
Table 12: Virologic Response (Viral Load Less Than 50 HIV-1 RNA Copies/mL) at Week 48 by Phenotypic Susceptibility Score (PSS) in the Non-VF Excluded Population of TMC125-C206 and TMC125-C216
PSS*
Etravirine + BR
N=559
Placebo + BR
N=586
0
43% (40/93)
5% (5/95)
1
61% (125/206)
28% (64/226)
2
77% (114/149)
59% (97/165)
‚Č• 3
75% (83/111)
72% (72/100)
* The phenotypic susceptibility score (PSS) was defined as the total number of active antiretroviral drugs in the background therapy to which a subject‚Äôs baseline viral isolate showed sensitivity in phenotypic resistance tests. Each drug in the background therapy was scored as a ‚Äė1‚Äô or ‚Äė0‚Äô based on whether the viral isolate was considered susceptible or resistant to that drug, respectively. In the calculation of the PSS, darunavir was counted as a sensitive antiretroviral if the FC was less than or equal to 10; ENF was counted as a sensitive antiretroviral if it had not been used previously. Etravirine was not included in this calculation.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Etravirine was evaluated for carcinogenic potential by oral gavage administration to mice and rats for up to approximately 104 weeks. Daily doses of 50 mg/kg, 200 mg/kg and 400 mg/kg were administered to mice and doses of 70 mg/kg, 200 mg/kg and 600 mg/kg were administered to rats in the initial period of approximately 41 to 52 weeks. The high and middle doses were subsequently adjusted due to tolerability and reduced by 50% in mice and by 50% to 66% in rats to allow for completion of the studies. In the mouse study, statistically significant increases in the incidences of hepatocellular carcinoma and incidences of hepatocellular adenomas or carcinomas combined were observed in treated females. In the rat study, no statistically significant increases in tumor findings were observed in either sex. The relevance of these liver tumor findings in mice to humans is not known. Because of tolerability of the formulation in these rodent studies, maximum systemic drug exposures achieved at the doses tested were lower than those in humans at the clinical dose (400 mg/day), with animal vs. human AUC ratios being 0.6-fold (mice) and 0.2-to-0.7-fold (rats).
Mutagenesis
Etravirine tested negative in the in vitro Ames reverse mutation assay, in vitro chromosomal aberration assay in human lymphocyte, and in vitro clastogenicity mouse lymphoma assay, tested in the absence and presence of a metabolic activation system. Etravirine did not induce chromosomal damage in the in vivo micronucleus test in mice.
Impairment of Fertility
No effects on fertility and early embryonic development were observed when etravirine was tested in rats at maternal doses up to 500 mg/day, resulting in systemic drug exposure up to the recommended human dose (400 mg/day).
14 Clinical Studies
14.1 Treatment-ExperiencedAdult Subjects
The clinical efficacy of etravirine is derived from the analyses of 48-week data from 2 ongoing, randomized, double-blinded, placebo-controlled, Phase 3 trials, TMC125-C206 and TMC125-C216 (DUET-1 and DUET-2) in subjects with 1 or more NNRTI resistance-associated substitutions. These trials are identical in design and the results below are pooled data from the two trials.
TMC125-C206 and TMC125-C216 are Phase 3 studies designed to evaluate the safety and antiretroviral activity of etravirine in combination with a background regimen (BR) as compared to placebo in combination with a BR. Eligible subjects were treatment-experienced HIV-1-infected subjects with plasma HIV-1 RNA greater than 5,000 copies/mL while on an antiretroviral regimen for at least 8 weeks. In addition, subjects had 1 or more NNRTI resistance-associated substitutions at screening or from prior genotypic analysis, and 3 or more of the following primary PI substitutions at screening: D30N, V32I, L33F, M46I/L, I47A/V, G48V, I50L/V, V82A/F/L/S/T, I84V, N88S, or L90M. Randomization was stratified by the intended use of ENF in the BR, previous use of darunavir/ritonavir, and screening viral load. Virologic response was defined as HIV-1 RNA less than 50 copies/mL at Week 48.
All study subjects received darunavir/ritonavir as part of their BR, and at least 2 other investigator-selected antiretroviral drugs (N[t]RTIs with or without ENF). Of etravirine-treated subjects, 25.5% used ENF for the first time (de novo) and 20.0% re-used ENF. Of placebo-treated subjects, 26.5% used de novo ENF and 20.4% re-used ENF.
In the pooled analysis for TMC125-C206 and TMC125-C216, demographics and baseline characteristics were balanced between the etravirine arm and the placebo arm (Table 13). Table 13 displays selected demographic and baseline disease characteristics of the subjects in the etravirine and placebo arms.
Table 13: Demographic and Baseline Disease Characteristics of Subjects (Pooled Analysis TMC125-C206 and TMC125-C216)‚ÄĒ
Etravirine + BR
N=599
Placebo + BR
N=604
Demographic characteristics
Median age, years (range)
46
(18 to 77)
45
(18 to 72)
Sex
Male
90.0%
88.6%
Female
10.0%
11.4%
Race
White
70.1%
69.8%
Black
13.2%
13.0%
Hispanic
11.3%
12.2%
Asian
1.3%
0.6%
Other
4.1%
4.5%
Baseline disease characteristics
Median baseline plasma HIV-1 RNA (range), log10 copies/mL
4.8
(2.7 to 6.8)
4.8
(2.2 to 6.5)
Percentage of subjects with baseline viral load:
< 30,000 copies/mL
‚Č• 30,000 copies/mL and < 100,000 copies/mL
‚Č• 100,000 copies/mL
27.5%
34.4%
38.1%
28.8%
35.3%
35.9%
Median baseline CD4+ cell count (range), cells/mm3
99
(1 to 789)
109
(0 to 912)
Percentage of subjects with baseline CD4+ cell count:
< 50 cells/mm3
‚Č• 50 cells/mm3 and < 200 cells/mm3
‚Č• 200 cells/mm3
35.6%
34.8%
29.6%
34.7%
34.5%
30.8%
Median (range) number of primary PI substitutions*
4
(0 to 7)
4
(0 to 8)
Percentage of subjects with previous use of NNRTIs:
0
1
> 1
8.2%
46.9%
44.9%
7.9%
46.7%
45.4%
Percentage of subjects with previous use of the following NNRTIs:
Efavirenz
Nevirapine
Delavirdine
70.3%
57.1%
13.7%
72.5%
58.6%
12.6%
Median (range) number of NNRTI RASs†
2
(0 to 8)
2
(0 to 7)
Median fold change of the virus for the following NNRTIs: Delavirdine
Efavirenz
Etravirine
Nevirapine
27.3
63.9
1.6
74.3
26.1
45.4
1.5
74.0
Percentage of subjects with previous use of a fusion inhibitor
39.6%
42.2%
Percentage of subjects with a Phenotypic Sensitivity Score (PSS) for the background therapy ‡ of:
0
1
2
‚Č• 3
17.0%
36.5%
26.9%
19.7%
16.2%
38.7%
27.8%
17.3%
RASs = Resistance-Associated Substitutions, BR=background regimen, FC = fold change in EC50
* IAS-USA primary PI substitutions [August/September 2007]: D30N, V32I, L33F, M46I/L, I47A/V, G48V, I50L/V, I54L/M, L76V, V82A/F/L/S/T, I84V, N88S, L90M
† Tibotec NNRTI RASs [June 2008]: A98G, V90I, L100I, K101E/H/P/Q, K103H/N/S/T, V106A/M/I, V108I, E138A/G/K/Q, V179D/E/F/G/I/T, Y181C/I/V, Y188C/H/L, V189I, G190A/C/E/Q/S, H221Y, P255H, F227C/L, M230I/L, P236L, K238N/T, Y318F
‡ The PSS was calculated for the background therapy (as determined on Day 7). Percentages are based on the number of subjects with available phenotype data. For fusion inhibitors (enfuvirtide), subjects were considered resistant if the drug was used in previous therapy up to baseline. Etravirine is not included in this calculation.
Efficacy at Week 48 for subjects in the etravirine and placebo arms for the pooled TMC125-C206 and TMC125-C216 study populations are shown in Table 14.
Table 14: Treatment Outcomes at Week 48 (Pooled Analysis TMC125-C206 and TMC125-C216)
Etravirine + BR
N=599
Placebo + BR
N=604
Virologic responders at Week 48
Viral Load < 50 HIV-1 RNA copies/mL
359 (60%)
232 (38%)
Virologic failures at Week 48
Viral Load ‚Č• 50 HIV-1 RNA copies/mL
123 (21%)
201 (33%)
Death
11 (2%)
19 (3%)
Discontinuations before Week 48:
due to virologic failures
58 (10%)
110 (18%)
due to adverse events
31 (5%)
14 (2%)
due to other reasons
17 (3%)
28 (5%)
BR=background regimen
At Week 48, 70.8% of etravirine-treated subjects achieved HIV-1 RNA less than 400 copies/mL as compared to 46.4% of placebo-treated subjects. The mean decrease in plasma HIV-1 RNA from baseline to Week 48 was -2.23 log10 copies/mL for etravirine-treated subjects and -1.46 log10 copies/mL for placebo-treated subjects. The mean CD4+ cell count increase from baseline for etravirine-treated subjects was 96 cells/mm3 and 68 cells/mm3 for placebo-treated subjects.
Of the study population who either re-used or did not use ENF, 57.4% of etravirine-treated subjects and 31.7% of placebo-treated subjects achieved HIV-1 RNA less than 50 copies/mL. Of the study population using ENF de novo, 67.3% of etravirine-treated subjects and 57.2% of placebo-treated subjects achieved HIV-1 RNA less than 50 copies/mL.
Treatment-emergent CDC category C events occurred in 4% of etravirine-treated subjects and 8.4% of placebo-treated subjects.
Study TMC125-C227 was a randomized, exploratory, active-controlled, open-label, Phase 2b trial. Eligible subjects were treatment-experienced, PI-na√Įve HIV-1-infected subjects with genotypic evidence of NNRTI resistance at screening or from prior genotypic analysis. The virologic response was evaluated in 116 subjects who were randomized to etravirine (59 subjects) or an investigator-selected PI (57 subjects), each given with 2 investigator-selected N(t)RTIs. Etravirine-treated subjects had lower antiviral responses associated with reduced susceptibility to the N(t)RTIs and to etravirine as compared to the control PI-treated subjects.
14.2 Treatment-ExperiencedPediatric Subjects (6 Years to Less Than 18 Years of Age)
The efficacy of etravirine for treatment-experienced pediatric subjects is based on one Phase 2 trial, TMC125-C213.
Pediatric Subjects (6 Years to Less Than 18 Years of Age [TMC125-C213])
TMC125-C213, a single-arm, Phase 2 trial evaluating the pharmacokinetics, safety, tolerability, and efficacy of etravirine enrolled 101 antiretroviral treatment-experienced HIV-1 infected pediatric subjects 6 years to less than 18 years of age and weighing at least 16 kg. Subjects eligible for this trial were on an antiretroviral regimen with confirmed plasma HIV-1 RNA of at least 500 copies/mL and viral susceptibility to etravirine at screening.
The median baseline plasma HIV-1 RNA was 3.9 log10 copies/mL, and the median baseline CD4+ cell count was 385 x 106 cells/mm3.
At Week 24, 52% of subjects had HIV-1 RNA less than 50 copies per mL. The proportion of subjects with HIV-1 RNA less than 400 copies/mL was 67%. The mean CD4+ cell count increase from baseline was 112 x 106 cells/mm3.
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ (etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
16 How Supplied/storage Andhandling
Etravirine Tablets, 25 mg are supplied as white to off-white, oval shaped, uncoated tablets containing 25 mg of etravirine. Each tablet is debossed with ‚ÄúA56‚ÄĚ on one side and score on the other side.They are available as follows:
Bottles of 120 with child-resistant closure:                NDC 60219-1720-7Each bottle contains 2 desiccant pouches.
Etravirine Tablets, 100 mg are supplied as white to off-white, oval shaped, uncoated tablets containing 100 mg of etravirine. Each tablet is debossed with ‚ÄúAC75‚ÄĚ on one side and plain on the other side.They are available as follows:
Bottles of 120 with child-resistant closure:                NDC 60219-1721-7Each bottle contains 3 desiccant pouches.
Etravirine Tablets, 200 mg are supplied as white to off-white, oval shaped, uncoated tablets containing 200 mg of etravirine. Each tablet is debossed with ‚ÄúAC76‚ÄĚ on one side and plain on the other side.They are available as follows:
Bottles of 60 with child-resistant closure:                  NDC 60219-1722-6Each bottle contains 3 desiccant pouches.
Store etravirine tablets at 20¬į to 25¬įC (68¬į to 77¬įF); excursions permitted between 15¬į to 30¬įC (59¬į to 86¬įF) [see USP controlled room temperature]. Store in the original bottle. Keep the bottle tightly closed in order to protect from moisture. Do not remove the desiccant pouches.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Administration
Advise patients to take etravirine tablets following a meal twice a day on a regular dosing schedule, as missed doses can result in development of resistance. The type of food does not affect the exposure to etravirine. Inform patients not to take more or less than the prescribed dose of etravirine or discontinue therapy with etravirine without consulting their physician. Etravirine must always be used in combination with other antiretroviral drugs [see Dosage and Administration (2.4)].
Advise patients to swallow the etravirine tablet(s) whole with a liquid such as water. Instruct patients not to chew the tablets. Patients who are unable to swallow the etravirine tablet(s) whole may disperse the tablet(s) in water. The patient should be instructed to do the following:
- place the tablet(s) in 5 mL (1 teaspoon) of water, or at least enough liquid to cover the medication,
- stir well until the water looks milky,
- add approximately 15 mL (1 tablespoon) of liquid. Water may be used, but orange juice or milk may improve taste. Patients should not place the tablets in orange juice or milk without first adding water. The use of warm (temperature greater than 104¬įF [greater than 40¬įC]) or carbonated beverages should be avoided.
- drink the mixture immediately,
- rinse the glass several times with orange juice, milk or water and completely swallow the rinse each time to make sure the patient takes the entire dose.
Severe Skin Reactions
Inform patients that severe and potentially life-threatening rash has been reported with etravirine. Rash has been reported most commonly in the first 6 weeks of therapy. Advise patients to immediately contact their healthcare provider if they develop rash. Instruct patients to immediately stop taking etravirine and seek medical attention if they develop a rash associated with any of the following symptoms as it may be a sign of a more serious reaction such as Stevens-Johnson syndrome, toxic epidermal necrolysis or severe hypersensitivity: fever, generally ill feeling, extreme tiredness, muscle or joint aches, bulers, oral lesions, eye inflammation, facial swelling, swelling of the eyes, lips, mouth, breathing difficulty, and/or signs and symptoms of liver problems (e.g., yellowing of your skin or whites of your eyes, dark or tea colored urine, pale colored stools/bowel movements, nausea, vomiting, loss of appetite, or pain, aching or sensitivity on your right side below your ribs). Patients should understand that if severe rash occurs, they will be closely monitored, laboratory tests will be ordered and appropriate therapy will be initiated [see Warnings and Precautions (5.1)].
Drug Interactions
Etravirine may interact with many drugs; therefore, advise patients to report to their healthcare provider the use of any other prescription or nonprescription medication or herbal products, including St. John's wort [see Warnings and Precautions (5.2)].
Immune Reconstitution Syndrome
Advise patients to inform their healthcare provider immediately of any symptoms of infection, as in some patients with advanced HIV infection (AIDS), signs and symptoms of inflammation from previous infections may occur soon after anti-HIV treatment is started [see Warnings and Precautions (5.3)].
Fat Redistribution
Inform patients that redistribution or accumulation of body fat may occur in patients receiving antiretroviral therapy, including etravirine, and that the cause and long-term health effects of these conditions are not known at this time [see Warnings and Precautions (5.4)].
Pregnancy Registry
Inform patients that there is an antiretroviral pregnancy registry to monitor fetal outcomes of pregnant individuals exposed to etravirine [see Use in Specific Populations (8.1)].
Lactation
Instruct mothers with HIV-1 infection not to breastfeed because HIV-1 can be passed to the baby in breast milk [see Use in Specific Populations (8.2)].
All brands uled are trademark of their respective owner.
Manufactured by: Amneal Pharmaceuticals Pvt. Ltd. Oral Solid Dosage Unit Ahmedabad 382213, INDIA
Distributed by: Amneal Pharmaceuticals LLC Bridgewater, NJ 08807
Rev. 09-2023-02
Patient Information
¬†Etravirine¬†(e‚ÄĚ tra vir‚Äô een)¬†Tablets Important: Ask your healthcare provider or pharmacist about medicines that should not be taken with etravirine tablets. For more information, see the section ‚ÄúWhat should I tell my healthcare provider before taking etravirine tablets?‚ÄĚ
What are etravirine tablets?
Etravirine tablet is a prescription medicine that is used to treat human immunodeficiency virus-1 (HIV-1) infection in combination with other HIV-1 medicines, in adults and children 6 years of age and older who have taken HIV-1 medicines in the past.
HIV-1 is the virus that causes AIDS (Acquired Immune Deficiency Syndrome).
Etravirine tablets are not recommended for use in children less than 2 years of age.
What should I tell my healthcare provider before taking etravirine tablets?
Before taking etravirine tablets tell your healthcare provider about all of your medical conditions, including if you:
- have liver problems, including hepatitis B or C.
- are pregnant or plan to become pregnant. Tell your healthcare provider if you become pregnant during treatment with etravirine tablets.
Pregnancy Registry: There is a pregnancy registry for people who take etravirine tablets during pregnancy. The purpose of this registry is to collect information about the health of you and your baby. Talk to your healthcare provider about how you can take part in this registry.
- are breastfeeding or plan to breastfeed. Do not breastfeed if you take etravirine tablets.
- You should not breastfeed if you have HIV-1 because of the risk of passing HIV-1 to your baby.
- Etravirine can pass to your baby in your breast milk.
- Talk with your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Some medicines may interact with etravirine tablets. Keep a ul of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.
- You can ask your healthcare provider or pharmacist for a ul of medicines that interact with etravirine tablets.
- Do not start a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take etravirine tablets with other medicines.
How should I take etravirine tablets?
- Stay under the care of your healthcare provider during treatment with etravirine tablets.
- Take etravirine tablets every day exactly as prescribed by your healthcare provider.
- Your healthcare provider will tell you how many etravirine tablets to take and when to take them. Talk to your healthcare provider if you have questions about when to take etravirine tablets.
- Take etravirine tablets 2 times each day.
- If your child takes etravirine tablets, your healthcare provider will prescribe the right dose based on your child’s weight.
- Always take etravirine tablets following a meal. Do not take etravirine tablets on an empty stomach. Etravirine tablets may not work as well if you take it on an empty stomach.
- Do not change your dose or stop taking etravirine tablets without first talking with your healthcare provider.
- Swallow etravirine tablets whole, with liquid, such as water. Do not chew the tablet(s).
- If you are unable to swallow etravirine tablets whole, you may take your dose of etravirine tablets as follows:
Step 1: Measure approximately 5 mL (1 teaspoon) of water and pour into a cup.
Step 2: Place the tablets in the cup containing 5 mL of water. If needed, add more water to cover the tablets. Do not put the tablets in other liquids.
Step 3: Stir well until the water looks milky.
Step 4: Add a small amount (approximately 15 mL or 1 tablespoon) of liquid. Water may be used but adding orange juice or milk rather than water may make it easier to take. Do not use warm (temperature more than 104¬įF or 40¬įC) or carbonated beverages.
Step 5: Drink the mixture right away.
Step 6: Add more orange juice, milk, or water to the cup to rinse the cup several times and completely swallow each time to make sure you take your entire dose of etravirine tablets.
- It is important that you do not miss or skip doses of etravirine tablets during treatment.
- When your supply of etravirine tablets starts to run low, get more from your healthcare provider or pharmacy. It is important not to run out of etravirine tablets. The amount of HIV in your blood may increase if the medicine is stopped even for a short time.
- If you take too much etravirine tablets, call your healthcare provider or go to the nearest emergency room right away.
What are the possible side effects of etravirine tablets?
Etravirine tablets can cause serious side effects including:
- Severe skin rash and allergic reactions. Skin rash is a common side effect of etravirine tablets. The risk of getting a skin rash is higher in females. Rarely, rash can be severe and may lead to death. Severe skin rash with bulers or peeling skin, including the area around the mouth or eyes, may happen more frequently in children less than 18 years of age who take etravirine tablets in combination with other HIV-1 medicines than in adults. Call your healthcare provider right away if a rash develops; severe cases may need to be treated in a hospital.
If you get a rash with any of the following symptoms, stop taking etravirine tablets and call your healthcare provider or get medical help right away:
 
- fever
- muscle or joint aches
- redness or swelling of the eyes
- generally ill feeling
- bulers or sores in mouth
- swelling of the mouth, lips, or face
- extreme tiredness
- bulers or peeling of the skin
- problems breathing
Sometimes allergic reactions can affect body organs, such as your liver. Call your healthcare provider right away if you have any of the following signs or symptoms of liver problems:
- yellowing of your skin or whites of your eyes
- dark or tea colored urine
- pale colored stools (bowel movements)
- nausea or vomiting
- loss of appetite
- pain, aching, or tenderness on the right side of your stomach area
- Changes in your immune system (Immune Reconstitution Syndrome) can happen when you start taking HIV-1 medicines. Your immune system may get stronger and begin to fight infections that have been hidden in your body for a long time. Call your healthcare provider right away if you start having any new symptoms after starting your HIV-1 medicines.
- Changes in body fat¬†can happen in people taking HIV-1 medicines. These changes may include an increased amount of fat in the upper back and neck (‚Äúbuffalo hump‚ÄĚ), breast, and around the middle of your body (trunk). Loss of fat from the legs, arms, and face may also happen. The exact cause and long-term health effects of these problems are not known.
The most common side effects of etravirine tablets in adults include rash as well as numbness, tingling or pain in the hands or feet.
The most common side effects of etravirine tablets in children include rash and diarrhea.
These are not all the possible side effects of etravirine tablets.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store etravirine tablets?
- Store etravirine tablets at room temperature between 68¬į to 77¬įF (20¬į to 25¬įC).
- Keep etravirine tablets in the original bottle. Etravirine tablets come in a child-resistant package.
- Keep the bottle tightly closed to protect etravirine tablets from moisture.
- The etravirine tablets bottle contains a desiccant packet to help keep your medicine dry (protect it from moisture). The bottle of 25 mg tablets contains 2 desiccant packets. The bottles of 100 mg and 200 mg tablets contain 3 desiccant packets. Keep the desiccant packets in the bottle. Do not eat the desiccant packets.
Keep etravirine tablets and all medicines out of the reach of children.
General information about the safe and effective use of etravirine tablets
Medicines are sometimes prescribed for purposes other than those uled in a Patient Information leaflet. Do not use etravirine tablets for a condition for which it was not prescribed. Do not give etravirine tablets to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about etravirine tablets that is written for health professionals.
What are the ingredients in etravirine tablets?
Active ingredient: etravirine.
25 mg, 100 mg and 200 mg tablets contain the following inactive ingredients: croscarmellose sodium, crospovidone (type A), colloidal silicon dioxide, hypromellose, low-substituted hydroxy propyl cellulose, magnesium stearate and microcrystalline cellulose.
Additional pediatric use information is approved for Janssen Products, LP‚Äôs INTELENCE¬ģ¬†(etravirine) tablets. However, due to Janssen Products, LP‚Äôs marketing exclusivity rights, this drug product is not labeled with that pediatric information.
For more information, go to www.amneal.com or call toll-free 1-877-835-5472.
This Patient Information has been approved by the U.S. Food and Drug Administration.
All brands uled are trademark of their respective owner.
Manufactured by: Amneal Pharmaceuticals Pvt. Ltd. Oral Solid Dosage Unit Ahmedabad 382213, INDIA
Distributed by: Amneal Pharmaceuticals LLC Bridgewater, NJ 08807
Rev. 09-2023-01
Dispense with Patient Information available at:
documents.amneal.com/mg/ppi-etravirine-tab.pdf
Principal Display Panel
NDC 60219-1720-7 Etravirine Tablets, 25 mg 120 Tablets Rx Only Amneal Pharmaceuticals LLC
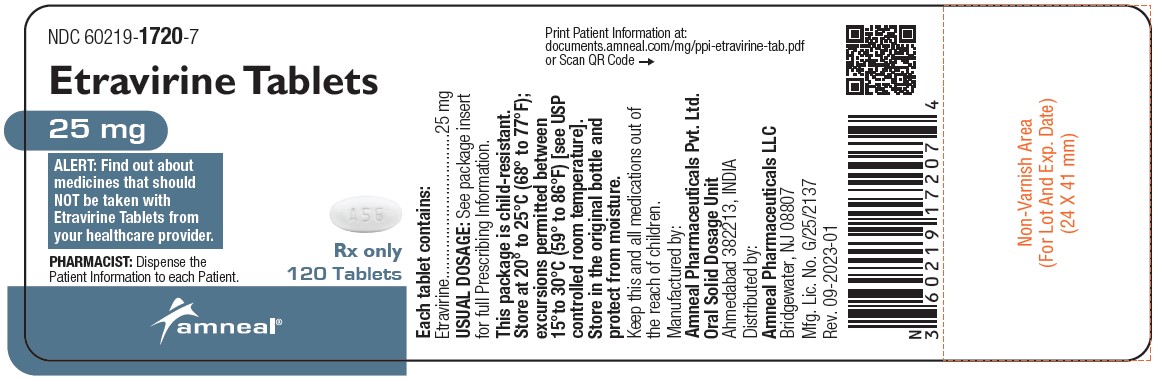
NDC 60219-1721-7 Etravirine Tablets, 100 mg 120 Tablets Rx Only Amneal Pharmaceuticals LLC
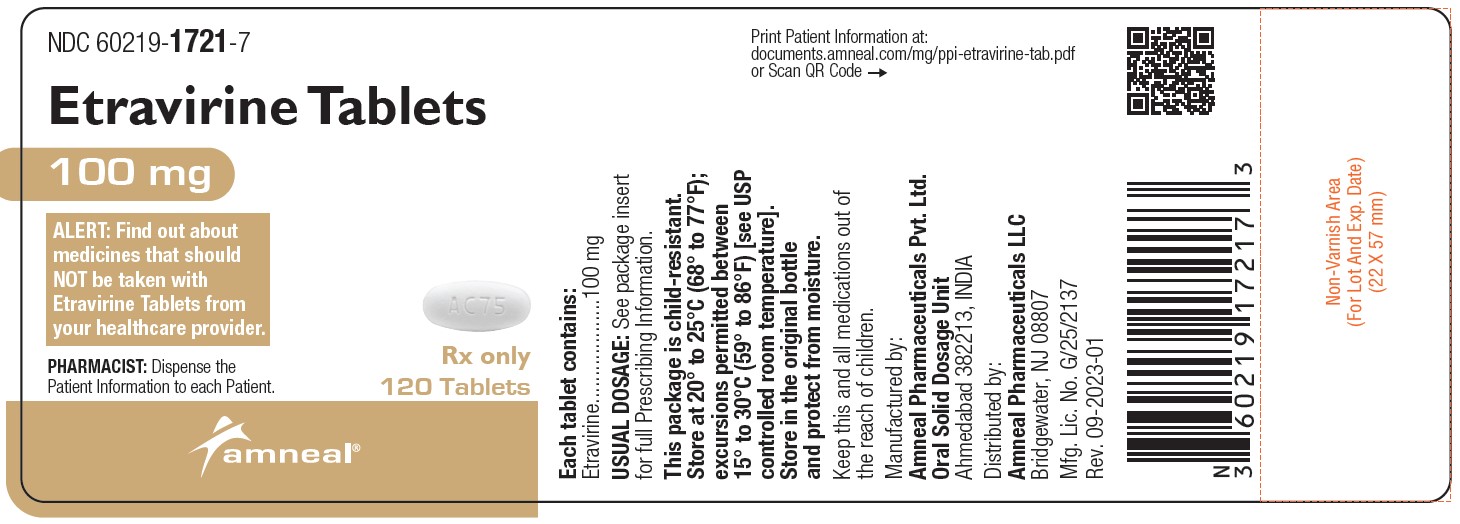
NDC 60219-1722-6 Etravirine Tablets, 200 mg 60 Tablets Rx Only Amneal Pharmaceuticals LLC
 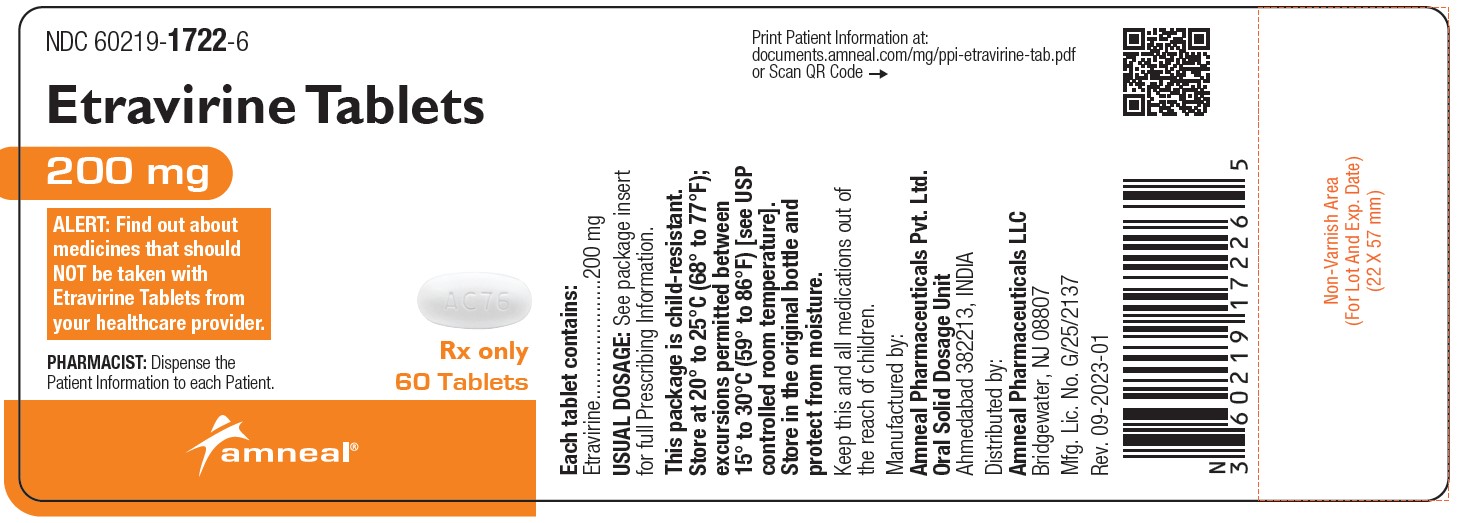
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


