Meropenem and Sodium Chloride Dailymed
Generic: meropenem and sodium chloride is used for the treatment of Appendicitis Bacteroides Infections Escherichia coli Infections Fever Hypersensitivity Klebsiella Infections Meningitis, Haemophilus Meningitis, Meningococcal Meningitis, Pneumococcal Neutropenia Peritonitis Pseudomonas Infections Respiratory Tract Infections Urinary Tract Infections Soft Tissue Infections
Go PRO for all pill images
Recent Major Changes
Warnings and Precautions, Severe Cutaneous Adverse Reactions (5.2 ) 1/2020
1 Indications And Usage
Meropenem for Injection and Sodium Chloride Injection is a penem antibacterial indicated for the treatment of:
- Complicated skin and skin structure infections (adult patients and pediatric patients 3 months of age and older requiring the full adult dose only). (
1.1 ) - Complicated intra-abdominal infections (adult patients and pediatric patients 3 months of age and older requiring the full adult dose only). (
1.2 ) - Bacterial meningitis (pediatric patients 3 months of age and older requiring the full adult dose only). (
1.3 )
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Meropenem for Injection USP and Sodium Chloride Injection USP and other antibacterial drugs, Meropenem for Injection USP and Sodium Chloride Injection USP should only be used to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
1.1 Complicated Skin and Skin Structure Infections (Adult Patients and Pediatric Patients 3 Months of ageand older requiring the full adult dose only)
Meropenem for Injection and Sodium Chloride Injection is indicated for the treatment of complicated skin and skin structure infections (cSSSI) due to Staphylococcus aureus (methicillin-susceptible isolates only), Streptococcus pyogenes, Streptococcus agalactiae, viridans group streptococci, Enterococcus faecalis (vancomycin-susceptible isolates only), Pseudomonas aeruginosa, Escherichia coli, Proteus mirabilis, Bacteroides fragilis, and Peptostreptococcus species.
1.2 Complicated Intra-abdominal Infections (Adult Patients and Pediatric Patients 3 Months of age and older requiring the full adult dose only)
Meropenem for Injection and Sodium Chloride Injection is indicated for the treatment of complicated appendicitis and peritonitis caused by viridans group streptococci, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Bacteroides fragilis, B. thetaiotaomicron, and Peptostreptococcus species.
1.3 Bacterial Meningitis (Pediatric Patients 3 Months of age and older requiring the full adult dose only)
Meropenem for Injection and Sodium Chloride Injection is indicated for the treatment of bacterial meningitis caused by Haemophilus influenzae, Neisseria meningitidis and penicillin-susceptible isolates of Streptococcus pneumoniae.
Meropenem has been found to be effective in eliminating concurrent bacteremia in association with bacterial meningitis.
For information regarding use in pediatric patients (3 months of age and older) [see Indications and Usage (1.1), (1.2) or (1.3); Dosage and Administration (2.3), and Adverse Reactions (6.1)].
1.4 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Meropenem for Injection and Sodium Chloride Injection and other antibacterial drugs, Meropenem for Injection and Sodium Chloride Injection should only be used to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
2 Dosage And Administration
Use this formulation of meropenem only in patients who require the entire 500 mg or 1 gram dose and not any fraction thereof. (2.1 )
500 mg every 8 hours by intravenous infusion over 15 to 30 minutes for complicated skin and skin structure infections (cSSSI) for adult patients. When treating infections caused by Pseudomonas aeruginosa, a dose of 1 gram every 8 hours is recommended (2.1 ).
1 gram every 8 hours by intravenous infusion over 15 to 30 minutes for intra-abdominal infections for adult patients. (2.1 )
Dosage should be reduced in adult patients with renal impairment. If less than a full dose (1 gram or 500 mg) is required, an alternative formulation should be used to avoid risk of overdose. (2.2 )
 Recommended Meropenem for Injection Dosage Schedule for Adult Patients with Renal Impairment
Creatinine Clearance (mL/min)
 Dose (dependent on type of infection)  Dosing Interval  greater than 50  Recommended dose (500 mg cSSSI and 1 gram Intra-abdominal infection)  Every 8 hours 26-50   Recommended dose  Every 12 hours  10-25  One-half recommended dose  Every 12 hours  less than 10  One-half recommended dose  Every 24 hours
Meropenem for Injection and Sodium Chloride Injection in the DUPLEX¬ģ Container is designed to deliver a 500 mg or 1 gram dose of Meropenem. To prevent unintentional overdose, this product should not be used in pediatric patients who require less than the full adult dose of Meropenem. Meropenem is not to be used in pediatric patients aged less than three months. There is no experience in pediatric patients with renal impairment.
- Pediatric patients 3 months of age and older. (
2.3 )
Recommended Meropenem for Injection Dosage Schedule for Pediatric Patients with Normal Renal Function 
 Type of Infection  Dose (mg/kg)  Up to a Maximum Dose Dosing Interval   Complicated skin and skin structure 20 mg/kg (or 1 gram for pediatric patients weighing over 50 kg) every 8 hours is recommended when treating complicated skin and skin structure infections caused by P. aeruginosa (2.3).   10  500 mg  Every 8 hours  Intra-abdominal  20  1 gram  Every 8 hours  Meningitis  40  2 grams Every 8 hours 
- Intravenous infusion is to be given over approximately 15 to 30 minutes.
- There is no experience in pediatric patients with renal impairment.2.1 Adult Patients
Meropenem for Injection and Sodium Chloride Injection in the DUPLEX¬ģ Container should be used only in patients who require the entire 500 mg or 1 gram dose and not any fraction thereof. The recommended dose of Meropenem for Injection and Sodium Chloride Injection is 500 mg given every 8 hours for skin and skin structure infections and 1 gram given every 8 hours for intra-abdominal infections. When treating complicated skin and skin structure infections caused by P. aeruginosa, a dose of 1 gram every 8 hours is recommended.
Meropenem for Injection and Sodium Chloride Injection should be administered by intravenous infusion over approximately 15 to 30 minutes.
2.2 Use in Adult Patients with Renal Impairment
Dosage should be reduced in patients with creatinine clearance of 50 mL/min or less. (See dosing table below.)
Dosage should be reduced in renal failure if less than a full dose (1 gram or 500 mg) is required and an alternative formulation should be used to avoid risk of overdose.
When only serum creatinine is available, the following formula (Cockcroft and Gault equation)1 may be used to estimate creatinine clearance.
Males: Creatinine Clearance (mL/min) =
Weight (kg) x (140 - age)   72 x serum creatinine (mg/dL)
Females: 0.85 x above value
Table 1: Recommended Meropenem for Injection Dosage Schedule for Adult Patients With Renal Impairment
Creatinine Clearance (mL/min)   Dose (dependent on type of infection)  Dosing Interval greater than 50  Recommended dose (500 mg cSSSI and 1 gram Intra-abdominal infection)  Every 8 hours  26-50  Recommended dose  Every 12 hours  10-25  One-half recommended dose  Every 12 hours less than 10  One-half recommended dose  Every 24 hours
There is inadequate information regarding the use of meropenem for injection in patients on hemodialysis or peritoneal dialysis.
2.3 Use in Pediatric Patients (3 Months of age and older only)
- Meropenem for Injection and Sodium Chloride Injection in the DUPLEX¬ģ Container is designed to deliver a 500 mg or 1 gram dose of meropenem. To prevent unintentional overdose, this product should not be used in pediatric patients who require less than the full adult dose of meropenem.¬† Meropenem is not to be used in pediatric patients aged less than three months. For pediatric patients 3 months of age and older, the Meropenem for Injection and Sodium Chloride Injection dose is 10 mg/kg, 20 mg/kg or 40 mg/kg every 8 hours (maximum dose is 2 grams every 8 hours), depending on the type of infection (cSSSI, cIAI, intra-abdominal infection or meningitis). See dosing table 2 below. [see Use in Specific Populations (8.4)].¬†¬†
- For pediatric patients weighing over 50 kg administer Meropenem for Injection and Sodium Chloride Injection at a dose of 500 mg every 8 hours for cSSSI, 1 gram every 8 hours for cIAI and 2 grams every 8 hours for meningitis.
- Administer Meropenem for Injection and Sodium Chloride Injection as an intravenous infusion over approximately 15 minutes to 30 minutes.
Table 2: Recommended Meropenem for Injection Dosage Schedule for Pediatric Patients With Normal Renal Function
 Type of Infection  Dose (mg/kg)  Up to a Maximum Dose  Dosing Interval  Complicated Skin and Skin Structure Infections  10  500 mg  Every 8 hours  Complicated Intra-abdominal Infections  20  1 gram  Every 8 hours  Meningitis  40  2 grams Every 8 hours 
There is no experience in pediatric patients with renal impairment.
When treating cSSSI caused by P. aeruginosa, a dose of 20 mg/kg (or 1 gram for pediatric patients weighing over 50 kg) every 8 hours is recommended.
2.4 Preparation and Administration of Meropenem for Injection and Sodium Chloride Injection in DUPLEX Container
Important Administration Instructions
- Do not use in series connections. Such use would result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is complete. If administration is controlled by a pumping device, care must be taken to discontinue pumping action before the container runs dry or air embolism may result.
- Do not introduce additives into the DUPLEX¬ģ Container.
- Administer Meropenem for Injection and Sodium Chloride Injection intravenously over approximately 15 to 30 minutes.
This reconstituted solution is for intravenous use only.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
Use only if solution is clear and container and seals are intact.
DUPLEX¬ģ Container Storage
- To avoid inadvertent activation, the DUPLEX¬ģ Container should remain in the folded position until activation is intended.
Patient Labeling and Drug Powder/Diluent Inspection
- Apply patient-specific label on foil side of container. Use care to avoid activation. Do not cover any portion of foil strip with patient label.
- Unlatch side tab and unfold DUPLEX¬ģ Container (see Diagram 1).

- Visually inspect diluent chamber for particulate matter.
- Use only if container and seals are intact.
- To inspect the drug powder for foreign matter or discoloration, peel foil strip from drug chamber (see Diagram 2).
- Protect from light after removal of foil strip.
Note: If foil strip is removed, the container should be re-folded and the side tab latched until ready to activate. The product must then be used within 7 days at room temperature, but not beyond the labeled expiration date.
Reconstitution (Activation)
- Do not use directly after storage by refrigeration, allow the product to equilibrate to room temperature before patient use.
- Unfold the DUPLEX¬ģ Container and point the set port in a downward direction. Starting at the hanger tab end, fold the DUPLEX¬ģ Container just below the diluent meniscus trapping all air above the fold. To activate, squeeze the folded diluent chamber until the seal between the diluent and powder opens, releasing diluent into the drug powder chamber (see Diagram 3).
- Agitate the liquid-powder mixture until the drug powder is completely dissolved.
Note: Following reconstitution (activation), product must be used within 1 hour if stored at room temperature or within 15 hours if stored under refrigeration.
Administration
- Visually inspect the reconstituted solution for particulate matter.
- Point the set port in a downwards direction. Starting at the hanger tab end, fold the DUPLEX¬ģ Container just below the solution meniscus trapping all air above the fold. Squeeze the folded DUPLEX¬ģ Container until the seal between reconstituted drug solution and set port opens, releasing liquid to set port (see Diagram 4).
- Prior to attaching the IV set, check for minute leaks by squeezing container firmly. If leaks are found, discard container and solution as sterility may be compromised.
- Using aseptic technique, peel foil cover from the set port and attach sterile administration set (see Diagram 5).
- Refer to directions for use accompanying the administration set.
- Discard unused portion.
2.5 Compatibility
Compatibility of Meropenem for Injection and Sodium Chloride Injection with other drugs has not been established. Meropenem for Injection and Sodium Chloride Injection should not be mixed with or physically added to solutions containing other drugs.
2.6 Stability and Storage
Freshly prepared solutions of Meropenem for Injection and Sodium Chloride Injection should be used. Following reconstitution (activation) in the DUPLEX¬ģ Container, the product maintains satisfactory potency for 1 hour at up to 25¬ļC (77¬ļF) or for 15 hours at up to 5¬ļC (41¬ļF). Solutions of intravenous Meropenem for Injection and Sodium Chloride Injection should not be frozen.
3 Dosage Forms And Strengths
Single-dose DUPLEX¬ģ (Dual-chamber) container:
- 500 mg meropenem for injection USP (as a blend of sterile meropenem trihydrate USP and sterile sodium carbonate USP/NF) and 50 mL of sodium chloride injection USP
- 1 gram meropenem for injection USP (as a blend of sterile meropenem trihydrate USP and sterile sodium carbonate USP/NF) and 50 mL of sodium chloride injection USP
Single-dose DUPLEX¬ģ Container consisting of:
- 500 mg Meropenem for Injection and 50 mL Sodium Chloride Injection 0.9% (
3 )- 1 gram Meropenem for Injection and 50 mL Sodium Chloride Injection 0.9% (
3 )
4 Contraindications
Meropenem for Injection and Sodium Chloride Injection is contraindicated in patients with known hypersensitivity to any component of this product or to other drugs in the same class or in patients who have demonstrated anaphylactic reactions to beta-lactams.
- Known hypersensitivity to product components or anaphylactic reactions to beta-lactams. (
4 )- Contraindicated where the administration of sodium or chloride could be clinically detrimental. (
4 )
5 Warnings And Precautions
- Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients receiving beta-lactams. (
5.1 )
Severe cutaneous adverse reactions have been reported in patients receiving meropenem intravenous. Discontinue meropenem immediately if patients experience these signs and symptoms and consider alternative treatment. (5.2 )
- Seizures and other adverse CNS experiences have been reported during treatment. (
5.3 )- Co-administration of Meropenem for Injection with valproic acid or divalproex sodium reduces the serum concentration of valproic acid potentially increasing the risk of breakthrough seizures. (
5.4 ,7.2 )
Clostridioides difficile-associated diarrhea (ranging from mild diarrhea to fatal colitis) has been reported. Evaluate if diarrhea occurs. (5.5 )
- In patients with renal dysfunction, thrombocytopenia has been observed. (
5.8 )- Solutions containing sodium ions should be used with great care, if at all, in patients where the administration of sodium could be detrimental. (
5.10 ).5.1 Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients receiving therapy with beta-lactams. These reactions are more likely to occur in individuals with a history of sensitivity to multiple allergens.
There have been reports of individuals with a history of penicillin hypersensitivity who have experienced severe hypersensitivity reactions when treated with another beta-lactam. Before initiating therapy with Meropenem for Injection and Sodium Chloride Injection, it is important to inquire about previous hypersensitivity reactions to penicillins, cephalosporins, other beta-lactams, and other allergens. If an allergic reaction to Meropenem for Injection and Sodium Chloride Injection occurs, discontinue the drug immediately.
5.2 Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions (SCAR) such as Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), erythema multiforme (EM) and acute generalized exanthematous pustulosis (AGEP) have been reported in patients receiving meropenem [see Adverse Reactions (6.2) ]. If signs and symptoms suggestive of these reactions appear, Meropenem for Injection and Sodium Chloride Injection should be withdrawn immediately and an alternative treatment should be considered.
5.3 Seizure Potential
Seizures and other adverse CNS experiences have been reported during treatment with meropenem for injection. These experiences have occurred most commonly in patients with CNS disorders (e.g., brain lesions or history of seizures) or with bacterial meningitis and/or compromised renal function [see Adverse Reactions (6.1)  and Drug Interactions (7.2)].
During clinical investigations, 2904 immunocompetent adult patients were treated for non-CNS infections with the overall seizure rate being 0.7% (based on 20 patients with this adverse event). All meropenem-treated patients with seizures had pre-existing contributing factors. Among these are included prior history of seizures or CNS abnormality and concomitant medications with seizure potential. Dosage adjustment is recommended in patients with advanced age and/or adult patients with creatinine clearance of 50 mL/min or less [see Dosage and Administration (2.2)].
Close adherence to the recommended dosage regimens is urged, especially in patients with known factors that predispose to convulsive activity. Anti-convulsant therapy should be continued in patients with known seizure disorders. If focal tremors, myoclonus, or seizures occur, evaluate neurologically, place on anti-convulsant therapy if not already instituted, and re-examine the dosage of Meropenem for Injection and Sodium Chloride Injection to determine whether it should be decreased or discontinued.
5.4 Risk of Breakthrough Seizures Due to Drug Interaction with Valproic Acid
The concomitant use of meropenem and valproic acid or divalproex sodium is generally not recommended. Case reports in the literature have shown that co-administration of carbapenems, including meropenem, to patients receiving valproic acid or divalproex sodium results in a reduction in valproic acid concentrations. The valproic acid concentrations may drop below the therapeutic range as a result of this interaction, therefore increasing the risk of breakthrough seizures. Increasing the dose of valproic acid or divalproex sodium may not be sufficient to overcome this interaction. Consider administration of antibacterial drugs other than carbapenems to treat infections in patients whose seizures are well controlled on valproic acid or divalproex sodium. If administration of Meropenem for Injection and Sodium Chloride Injection is necessary, consider supplemental anti-convulsant therapy [see Drug Interactions (7.2)].
5.5 Associated Diarrhea
Clostridioides difficile- associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including meropenem for injection, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing isolates of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial drug use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial drug treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.6 Development of Drug-Resistant Bacteria
Prescribing Meropenem for Injection and Sodium Chloride Injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
5.7 Overgrowth of Nonsusceptible Organisms
As with other broad-spectrum antibacterial drugs, prolonged use of meropenem may result in overgrowth of nonsusceptible organisms. Repeated evaluation of the patient is essential. If superinfection does occur during therapy, appropriate measures should be taken.
5.8 Thrombocytopenia
In patients with renal impairment, thrombocytopenia has been observed but no clinical bleeding reported [see Dosage and Administration (2.2), Adverse Reactions (6.1), Use In Specific Populations (8.5) and (8.6), and Clinical Pharmacology (12.3)].
5.9 Potential for Neuromotor Impairment
Alert patients receiving meropenem for injection on an outpatient basis regarding adverse events such as seizures, delirium, headaches and/or paresthesias that could interfere with mental alertness and/or cause motor impairment. Until it is reasonably well established that meropenem for injection is well tolerated, advise patients not to operate machinery or motorized vehicles [see Adverse Reactions (6.1)].
5.10 High Sodium Load
Each 500 mg of Meropenem for Injection and Sodium Chloride Injection delivers 245.1 mg (10.7 mEq) of sodium and each 1 gram of Meropenem for Injection and Sodium Chloride Injection delivers 290.2 mg (12.6 mEq) of sodium. Avoid use of Meropenem for Injection and Sodium Chloride Injection in patients with congestive heart failure, elderly patients and patients requiring restricted sodium intake.
6 Adverse Reactions
 The following are discussed in greater detail in other sections of labeling:
- Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
- Severe Cutaneous Adverse Reactions [see Warnings and Precautions (5.2)]
- Seizure Potential [see Warnings and Precautions (5.3)]
- Risk of Breakthrough Seizures Due to Drug Interaction with Valproic Acid [see Warnings and Precautions (5.4)]
- Clostridioides difficile ‚Äď Associated Diarrhea [see Warnings and Precautions (5.5)]
- Development of Drug-Resistant Bacteria [see Warnings and Precautions (5.6)]
- Overgrowth of Nonsusceptible Organisms [see Warnings and Precautions (5.7)]
- Thrombocytopenia [see Warnings and Precautions (5.8)]
- Potential for Neuromotor Impairment [see Warnings and Precautions (5.9)]
- High Sodium Load [see Warnings and Precautions (5.10)]
 Most common adverse reactions (greater than or equal to 2%) are: headache, nausea, constipation, diarrhea, anemia, vomiting, and rash (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact B. Braun Medical Inc. at 1-800-854-6851 or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch .
6.1 Adverse Reactions from Clinical Trials
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Patients:
During clinical investigations, 2904 immunocompetent adult patients were treated for non-CNS infections with meropenem for injection (500 mg or 1000 mg every 8 hours). Deaths in 5 patients were assessed as possibly related to meropenem; 36 (1.2%) patients had meropenem discontinued because of adverse events. Many patients in these trials were severely ill and had multiple background diseases, physiological impairments and were receiving multiple other drug therapies.
In the seriously ill patient population, it was not possible to determine the relationship between observed adverse events and therapy with meropenem for injection.
The following adverse reaction frequencies were derived from the clinical trials in the 2904 patients treated with meropenem for injection.
Local Adverse Reactions
Local adverse reactions that were reported with meropenem for injection were as follows:
 Inflammation at the injection site  2.4%  Injection site reaction  0.9%  Phlebitis/thrombophlebitis  0.8%  Pain at the injection site  0.4%  Edema at the injection site  0.2%
Systemic Adverse Reactions
Systemic adverse events that were reported with meropenem for injection occurring in greater than 1.0% of the patients were diarrhea (4.8%), nausea/vomiting (3.6%), headache (2.3%), rash (1.9%), sepsis (1.6%), constipation (1.4%), apnea (1.3%), shock (1.2%), and pruritus (1.2%).
Additional systemic adverse reactions that were reported with meropenem for injection and occurring in less than or equal to 1.0% but greater than 0.1% of the patients are uled below within each body system in order of decreasing frequency:
Bleeding events were seen as follows: gastrointestinal hemorrhage (0.5%), melena (0.3%), epistaxis (0.2%), hemoperitoneum (0.2%).
Body as a Whole: pain, abdominal pain, chest pain, fever, back pain, abdominal enlargement, chills, pelvic pain
Cardiovascular: heart failure, heart arrest, tachycardia, hypertension, myocardial infarction, pulmonary embolus, bradycardia, hypotension, syncope
Digestive System: oral moniliasis, anorexia, cholestatic jaundice/jaundice, flatulence, ileus, hepatic failure, dyspepsia, intestinal obstruction
Hemic/Lymphatic: anemia, hypochromic anemia, hypervolemia
Metabolic/Nutritional: peripheral edema, hypoxia
Nervous System: insomnia, agitation, delirium, confusion, dizziness, seizure, nervousness, paresthesia, hallucinations, somnolence, anxiety, depression, asthenia [see Warnings and Precautions (5.3) and (5.9)]
Respiratory: respiratory disorder, dyspnea, pleural effusion, asthma, cough increased, lung edema
Skin and Appendages: urticaria, sweating, skin ulcer
Urogenital System: dysuria, kidney failure, vaginal moniliasis, urinary incontinence
Adverse Laboratory Changes
Adverse laboratory changes that were reported and occurring in greater than 0.2% of the patients were as follows:
Hepatic: increased alanine transaminase (ALT), aspartate transaminase (AST), alkaline phosphatase, lactate dehydrogenase (LDH), and bilirubin
Hematologic: increased platelets, increased eosinophils, decreased platelets, decreased hemoglobin, decreased hematocrit, decreased white blood cell (WBC), shortened prothrombin time and shortened partial thromboplastin time, leukocytosis, hypokalemia
Renal: increased creatinine and increased blood urea nitrogen (BUN)
Urinalysis: presence of red blood cells
Complicated Skin and Skin Structure Infections
In a study of complicated skin and skin structure infections, the adverse reactions were similar to those uled above. The most common adverse events occurring in greater than 5% of the patients were: headache (7.8%), nausea (7.8%), constipation (7.0%), diarrhea (7.0%), anemia (5.5%), and pain (5.1%). Adverse events with an incidence of greater than 1%, and not uled above, include: pharyngitis, accidental injury, gastrointestinal disorder, hypoglycemia, peripheral vascular disorder, and pneumonia.
Patients with Renal Impairment:
For patients with varying degrees of renal impairment, the incidence of heart failure, kidney failure, seizure and shock reported irrespective of relationship to meropenem for injection, increased in patients with moderately severe renal impairment (creatinine clearance greater than 10 to 26 mL/min) [see Dosage and Administration (2.2), Warnings and Precautions (5.8), Use in Specific Populations (8.5) and (8.6) and Clinical Pharmacology (12.3)].
Pediatric Patients
Systemic and Local Adverse Reactions
Pediatric Patients with Serious Bacterial Infections (excluding Bacterial Meningitis):
Meropenem for injection was studied in 515 pediatric patients (3 months of age and older to below 13 years of age) with serious bacterial infections (excluding meningitis, see next section) at dosages of 10 to 20 mg/kg every 8 hours. The types of systemic and local adverse events seen in these patients are similar to the adults, with the most common adverse events reported as possibly, probably, or definitely related to meropenem for injection and their rates of occurrence as follows:
Diarrhea  3.5% Rash  1.6% Nausea and Vomiting  0.8%
Pediatric Patients with Bacterial Meningitis:
Meropenem for injection was studied in 321 pediatric patients (3 months of age and older to below 17 years of age) with meningitis at a dosage of 40 mg/kg every 8 hours. The types of systemic and local adverse events seen in these patients are similar to the adults, with the most common adverse events reported as possibly, probably, or definitely related to meropenem for injection and their rates of occurrence as follows:
Diarrhea   4.7% Rash (mostly diaper area moniliasis)  3.1% Oral Moniliasis  1.9% Glossitis  1.0%
In the meningitis studies, the rates of seizure activity during therapy were comparable between patients with no CNS abnormalities who received meropenem and those who received comparator agents (either cefotaxime or ceftriaxone). In the meropenem for injection treated group, 12/15 patients with seizures had late onset seizures (defined as occurring on day 3 or later) versus 7/20 in the comparator arm. The meropenem group had a statistically higher number of patients with transient elevation of liver enzymes.
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post-approval use of meropenem for injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Worldwide post-marketing adverse reactions not otherwise uled in the Adverse Reactions from Clinical Trials section of this prescribing information and reported as possibly, probably, or definitely drug related are uled within each body system in order of decreasing severity.
Blood and Lymphatic System Disorders: agranulocytosis, neutropenia, and leukopenia; a positive direct or indirect Coombs test, and hemolytic anemia.
Immune System Disorders: angioedema.
Skin and Subcutaneous Disorders: toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), erythema multiforme (EM) and acute generalized exanthematous pustulosis (AGEP).
7 Drug Interactions
- Co-administration of Meropenem for Injection with probenecid inhibits renal excretion of meropenem and is therefore not recommended. (
7.1 )- The concomitant use of Meropenem and valproic acid or divalproex sodium is generally not recommended. Antibacterial drugs other than carbapenems should be considered to treat infections in patients whose seizures are well controlled on valproic acid or divalproex sodium. (
5.4 ,7.2 )7.1 Probenecid
Probenecid competes with meropenem for active tubular secretion, resulting in increased plasma concentrations of meropenem. Coadministration of probenecid with meropenem is not recommended.
7.2 Valproic Acid
Case reports in the literature have shown that co-administration of carbapenems, including meropenem, to patients receiving valproic acid or divalproex sodium results in a reduction in valproic acid concentrations. The valproic acid concentrations may drop below the therapeutic range as a result of this interaction, therefore increasing the risk of breakthrough seizures. Although the mechanism of this interaction is unknown, data from in vitro and animal studies suggest that carbapenems may inhibit the hydrolysis of valproic acid’s glucuronide metabolite (VPA-g) back to valproic acid, thus decreasing the serum concentrations of valproic acid. If administration of meropenem for injection is necessary, then supplemental anti-convulsant therapy should be considered [see Warnings and Precautions (5.4)].
8 Use In Specific Populations
- Pediatric use: Meropenem for Injection and Sodium Chloride Injection should not be used in pediatric patients who require less than the full adult dose of meropenem. (
8.4 )- Renal Impairment: Dose adjustment is necessary, if creatinine clearance is 50 mL/min or less. (
2.2 ,8.6 )8.1 Pregnancy
There are insufficient human data to establish whether there is a drug-associated risk of major birth defects or miscarriages with meropenem in pregnant women.
No fetal toxicity or malformations were observed in pregnant rats and cynomolgus macaques administered intravenous meropenem during organogenesis at doses up to 3.2 and 2.3 times the maximum recommended human dose based on body surface area comparison, respectively. In rats administered intravenous meropenem in late pregnancy and during the lactation period, there were no adverse effects on offspring at doses equivalent to approximately 3.2 times the maximum recommended human dose based on body surface area comparison  [see Data].
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4 % and 15-20%, respectively.
Animal Data
Reproductive studies have been performed with meropenem in rats at doses of up to 1000 mg/kg/day and in cynomolgus monkeys at doses of up to 360 mg/kg/day (on the basis of body surface area comparisons, approximately 3.2 times and 2.3 times higher, respectively, than the maximum recommended human dose of 1 gram every 8 hours). These studies revealed no evidence of harm to the fetus due to meropenem, although there were slight changes in fetal body weight at doses of 250 mg/kg/day (equivalent to approximately 0.8 times the maximum recommended human dose of 1 gram every 8 hours based on body surface area comparison) and above in rats. In a published study2, meropenem administered to pregnant rats from Gestation Day 6  to Gestation Day 17, was associated with mild maternal weight loss at all doses, but did not produce malformations or fetal toxicity. The no-observed-adverse-effect-level (NOAEL) for fetal toxicity in this study was considered to be the high dose of 750 mg/kg/day (equivalent to approximately 2.4 times the highest recommended human dose based on body surface area comparison).
In a peri-postnatal study in rats described in the published literature1, intravenous meropenem was administered to dams from Gestation Day 17 until Postpartum Day 21. There were no adverse effects in the dams and no adverse effects in the first generation offspring (including developmental, behavioral, and functional assessments and reproductive parameters) except that female offspring exhibited lowered body weights which continued during gestation and nursing of the second generation offspring. Second generation offspring showed no meropenem-related effects. The NOAEL value was considered to be 1000 mg/kg/day (approximately 3.2 times the highest recommended clinical dose based on body surface area comparisons).
8.2Lactation
Risk Summary
Meropenem has been reported to be excreted in human milk. No information is available on the effects of meropenem on the breastfed ‚Äďchild or on milk production.¬† The developmental and health benefits of breastfeeding should be considered along with the mother‚Äôs clinical need for Meropenem for Injection and Sodium Chloride Injection in the DUPLEX¬ģ Container and any potential adverse effects on the breastfed-child from Meropenem for Injection and Sodium Chloride Injection in the DUPLEX¬ģ Container or from the underlying maternal conditions.
8.4 Pediatric Use
Meropenem for Injection and Sodium Chloride Injection in the DUPLEX¬ģ Container is designed to deliver a 500 mg or 1 gram dose of meropenem. To prevent unintentional overdose, this product should not be used in pediatric patients who require less than the full adult dose of meropenem. Meropenem is not to be used in pediatric patients aged less than three months. [see Dosage and Administration (2.3)].¬†¬†¬†
Use of meropenem for injection in pediatric patients with bacterial meningitis is supported by evidence from adequate and well-controlled studies in the pediatric population. Use of meropenem for injection in pediatric patients with intra-abdominal infections is supported by evidence from adequate and well-controlled studies with adults with additional data from pediatric pharmacokinetics studies and controlled clinical trials in pediatric patients. Use of meropenem for injection in pediatric patients with complicated skin and skin structure infections is supported by evidence from an adequate and well-controlled study with adults and additional data from pediatric pharmacokinetics studies [see Indications and Usage (1), Dosage and Administration (2.3), Adverse Reactions (6.1),  Clinical Pharmacology (12.3) and Clinical Studies (14)].
8.5 Geriatric Use
Of the total number of subjects in clinical studies of meropenem for injection, approximately 1100 (30%) were 65 years of age and older, while 400 (11%) were 75 years and older. Additionally, in a study of 511 patients with complicated skin and skin structure infections, 93 (18%) were 65 years of age and older, while 38 (7%) were 75 years and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects; spontaneous reports and other reported clinical experience have not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Meropenem is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with renal impairment. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
A pharmacokinetic study with meropenem for injection in elderly patients has shown a reduction in the plasma clearance of meropenem that correlates with age-associated reduction in creatinine clearance [see Clinical Pharmacology (12.3)].
Each 500 mg of Meropenem for Injection and Sodium Chloride Injection delivers 245.1 mg (10.7 mEq) of sodium and each 1 gram of Meropenem for Injection and Sodium Chloride Injection delivers 290.2 mg (12.6 mEq) of sodium. At the usual recommended doses of 500 mg or 1000 mg every 8 hours, patients would receive between 735 mg/day and 870 mg/day (32 mEq and 38 mEq) of sodium. The geriatric population may respond with a blunted natriuresis to salt loading. This may be clinically important with regard to such diseases as congestive heart failure [see C ontraindications (4)  and  Warnings and Precautions (5.10)].
8.6 Patients with Renal Impairment
Dosage adjustment is necessary in patients with creatinine clearance 50 mL/min or less [see Dosage and Administration (2.2), Warnings and Precautions (5.8), and Clinical Pharmacology (12.3)].
10 Overdosage
In mice and rats, large intravenous doses of meropenem (2200-4000 mg/kg) have been associated with ataxia, dyspnea, convulsions, and mortalities.
Intentional overdosing of Meropenem for Injection and Sodium Chloride Injection is unlikely, although accidental overdosing might occur if large doses are given to patients with reduced renal function. The largest dose of meropenem administered in clinical trials has been 2 grams given intravenously every 8 hours. At this dosage, no adverse pharmacological effects or increased safety risks have been observed.
Limited post-marketing experience indicates that if adverse events occur following overdosage, they are consistent with the adverse event profile described in the Adverse Reactions section and are generally mild in severity and resolve on withdrawal or dose reduction. Symptomatic treatments should be considered. In individuals with normal renal function, rapid renal elimination takes place. Meropenem and its metabolite are readily dialyzable and effectively removed by hemodialysis; however, no information is available on the use of hemodialysis to treat overdosage.
11 Description
Meropenem for injection is a sterile, pyrogen-free, synthetic, carbapenem¬†antibacterial drug for intravenous administration.¬†Meropenem is (4R,5S,6S)-3- [[(3S,5S)-5-(Dimethylcarbamoyl)-3-pyrrolidinyl]thio]-6-[(1R)-1-hydroxyethyl]-4-methyl-7-oxo-1-azabicyclo[3.2.0]hept-2-ene-2-carboxylic acid trihydrate. Its empirical formula is C17H25N3O5S‚ÄĘ3H2O with a molecular weight of 437.52.
Its structural formula is:

Meropenem for injection is a white to pale yellow crystalline powder containing meropenem trihydrate and sodium carbonate. The constituted solution varies from colorless to yellow depending on the concentration. The pH of freshly constituted solutions is between 7.3 and 8.3. Meropenem is soluble in 5% monobasic potassium phosphate solution, sparingly soluble in water, very slightly soluble in hydrated ethanol, and practically insoluble in acetone or ether.
Meropenem for Injection USP and Sodium Chloride Injection USP is supplied as a sterile, nonpyrogenic, single-dose packaged combination of meropenem (drug chamber) and 50 mL of sodium chloride (diluent) in the DUPLEX¬ģ sterile container. When reconstituted as instructed, each 1 gram Meropenem for injection in the DUPLEX¬ģ Container will deliver 1 gram of meropenem and a total sodium content of 290.2 mg (12.6 mEq). Each 500 mg Meropenem for injection in the DUPLEX¬ģ Container will deliver 500 mg of meropenem and a total sodium content of 245.1 mg (10.7 mEq)¬†[see Dosage and Administration (2.4)]. The osmolality of the reconstituted solution of Meropenem for Injection USP and Sodium Chloride Injection USP is approximately 356 mOsmol/kg for the 500 mg dose and approximately 417 mOsmol/kg for the 1 gram dose.
The DUPLEX¬ģ Container is a flexible dual chamber container. After removing the peelable foil strip, activating the seals, and thoroughly mixing, the reconstituted drug product is hyperosmotic and is intended for single intravenous use. The product (diluent and drug) contact layer is a mixture of thermoplastic rubber and a polypropylene ethylene copolymer that contains no plasticizers.
Not made with natural rubber latex, PVC or Di(2-ethylhexyl)phthalate (DEHP).
12 Clinical Pharmacology
12.1 Mechanism of Action
Meropenem is an antibacterial drug [see Microbiology  (12.4)].
12.2Pharmacodynamics
The percentage of time of a dosing interval that unbound plasma concentration of meropenem exceeds the meropenem minimum inhibitory concentration (MIC) against the infecting organism has been shown to best correlate with efficacy in animal and in vitro models of infection.
12.3 Pharmacokinetics
Plasma Concentrations
At the end of a 30-minute intravenous infusion of a single dose of meropenem for injection in healthy volunteers, mean peak plasma concentrations of meropenem are approximately 23 mcg/mL (range 14-26) for the 500 mg dose and 49 mcg/mL (range 39-58) for the 1 gram dose. A 5-minute intravenous bolus injection of meropenem in healthy volunteers results in mean peak plasma concentrations of approximately 45 mcg/mL (range 18-65) for the 500 mg dose and 112 mcg/mL (range 83-140) for the 1 gram dose.
Following intravenous doses of 500 mg, mean plasma concentrations of meropenem usually decline to approximately 1 mcg/mL at 6 hours after administration.
No accumulation of meropenem in plasma was observed with regimens using 500 mg administered every 8 hours or 1 gram administered every 6 hours in healthy volunteers with normal renal function.
Distribution
The plasma protein binding of meropenem is approximately 2%.
After a single intravenous dose of meropenem for injection, the highest mean concentrations of meropenem were found in tissues and fluids at 1 hour (0.5 to 1.5 hours) after the start of infusion, except where indicated in the tissues and fluids uled in table 3 below.
Table 3: Meropenem Concentrations in Selected Tissues (Highest Concentrations Reported)
Tissue Intravenous Dose (gram) ¬†Number of Samples ¬†Mean [mcg/mL or mcg/(g)] at 1 hour unless otherwise noted ¬†¬†¬†Range [mcg/mL or mcg/(g)] Endometrium 0.5¬† ¬†7 ¬†4.2 1.7‚Äď10.2¬† Myometrium¬† ¬†0.5 ¬†15 ¬†3.8 ¬†0.4‚Äď8.1 Ovary¬† ¬†0.5 ¬†8 ¬†2.8 ¬†0.8‚Äď4.8 Cervix¬† ¬†0.5 2¬† ¬†7 ¬†5.4‚Äď8.5 Fallopian tube ¬†0.5 9¬† ¬†1.7 ¬†0.3-3.4 Skin¬† ¬†0.5 22¬† ¬†3.3 ¬†0.5‚Äď12.6 Interstitial fluid obtained from buler fluid ¬†¬†¬†0.5 ¬†9 ¬†5.5 3.2-8.6¬† Skin¬† ¬†1 ¬†10 5.3¬† ¬†1.3‚Äď16.7 Interstitial fluid ¬† 1 ¬†5 26.3¬† 20.9‚Äď37.4¬† Colon¬† 1 2¬† ¬†2.6 ¬†2.5‚Äď2.7 Bile¬† ¬†1 ¬†7 ¬†14.6 (3 hours) 4.0‚Äď25.7¬† Gall bladder¬† 1 ¬†1 ‚ÄĒ¬† ¬†3.9 Peritoneal fluid 1 ¬†9 ¬†30.2 ¬†7.4‚Äď54.6 Lung¬† 1 ¬†2 ¬†4.8 (2 hours) ¬†1.4‚Äď8.2 Bronchial mucosa¬† ¬†1 ¬†7 4.5¬† ¬†1.3‚Äď11.1 Muscle ¬†1 2¬† 6.1 (2 hours)¬† 5.3‚Äď6.9¬† Fascia ¬†1 ¬†9 8.8¬† ¬†1.5‚Äď20 Heart valves¬† ¬†1 ¬†7 ¬†9.7 ¬†6.4‚Äď12.1 Myocardium ¬†1 10¬† ¬†15.5 ¬†5.2‚Äď25.5 CSF (inflamed) 20 mg/kg in pediatric patients of age 5 months to 8 years ¬†¬†8 ¬†1.1 (2 hours) ¬†0.2-2.8 ¬†40 mg/kg in pediatric patients of age 1 month to 15 years ¬†¬†5 ¬†3.3 (3 hours) ¬†0.9-6.5 CSF (uninflamed)¬† ¬†1 4¬† ¬†0.2 (2 hours) 0.1‚Äď0.3¬†
Elimination
In subjects with normal renal function, the elimination half-life of meropenem is approximately 1 hour.
Metabolism
There is one metabolite of meropenem that is microbiologically inactive.
Excretion
Meropenem is primarily excreted unchanged by the kidneys. Approximately 70% (50 ‚Äď 75%) of the dose is excreted unchanged within 12 hours. A further 28% is recovered as the microbiologically inactive metabolite. Fecal elimination represents only approximately 2% of the dose. The measured renal clearance and the effect of probenecid show that meropenem undergoes both filtration and tubular secretion.
Urinary concentrations of meropenem in excess of 10 mcg/mL are maintained for up to 5 hours after a 500 mg dose.
Specific Populations
Patients with Renal Impairment
Pharmacokinetic studies with meropenem for injection in patients with renal impairment have shown that the plasma clearance of meropenem correlates with creatinine clearance. Dosage adjustments are necessary in subjects with renal impairment (creatinine clearance 50 mL/min or less) [see Dosage and Administration (2.2 )  and Use In Specific Populations (8.6)].
Meropenem is hemodialyzable. However, there is no information on the usefulness of hemodialysis to treat overdosage [see Overdosage (10)].
Patients with Hepatic Impairment
A pharmacokinetic study with meropenem for injection in patients with hepatic impairment has shown no effects of liver disease on the pharmacokinetics of meropenem.
Geriatric Patients
A pharmacokinetic study with meropenem for injection in elderly patients with renal impairment showed a reduction in plasma clearance of meropenem that correlates with age-associated reduction in creatinine clearance.
Pediatric Patients
The pharmacokinetics of meropenem in pediatric patients 2 years of age or older are similar to those in adults. The elimination half-life for meropenem was approximately 1.5 hours in pediatric patients of age 3 months to 2 years.
The pharmacokinetics of meropenem in patients less than 3 months of age receiving combination antibacterial drug therapy are given below.
Table 4: Meropenem Pharmacokinetic Parameters in Patients Less Than 3 Months of AgeValues are derived from a population pharmacokinetic analysis of sparse data  
  GA less than 32 weeks PNA less than 2 weeks (20mg/kg every 12 hours) GA less than 32 weeks PNA 2 weeks or older (20mg/kg every 8 hours) GA 32 weeks or older PNA less than 2 weeks (20mg/kg every 8 hours)  GA 32 weeks or older PNA 2 weeks or older (30mg/kg every 8 hours) Overall CL (L/h/kg)   0.089  0.122  0.135  0.202  0.119  V (L/kg)  0.489  0.467  0.463  0.451  0.468  AUC0-24 (mcg-h/mL)  448  491  445  444  467  Cmax (mcg/mL)  44.3  46.5  44.9  61  46.9  Cmin (mcg/mL)  5.36  6.65  4.84  2.1  5.65  T1/2 (h)  3.82  2.68  2.33  1.58  2.68
Drug Interactions
Probenecid competes with meropenem for active tubular secretion and thus inhibits the renal excretion of meropenem. Following administration of probenecid with meropenem, the mean systemic exposure increased 56% and the mean elimination half-life increased 38%. Co-administration of probenecid with meropenem is not recommended.
12.4Microbiology
Mechanism of Action
The bactericidal activity of meropenem results from the inhibition of cell wall synthesis. Meropenem penetrates the cell wall of most Gram-positive and Gram-negative bacteria to reach penicillin-binding-protein (PBP) targets. Meropenem binds to PBPs 2, 3 and 4 of Escherichia coli and Pseudomonas aeruginosa; and PBPs 1, 2 and 4 of Staphylococcus aureus. Bactericidal concentrations (defined as a 3 log10 reduction in cell counts within 12 to 24 hours) are typically 1-2 times the bacteriostatic concentrations of meropenem, with the exception of Listeria monocytogenes, against which lethal activity is not observed.
Meropenem has significant stability to hydrolysis by beta-lactamases, both penicillinases and cephalosporinases produced by Gram-positive and Gram-negative bacteria.
Meropenem does not have in-vitro activity against methicillin-resistant Staphylococcus aureus (MRSA) or methicillin-resistant Staphylococcus epidermidis (MRSE).
Resistance
There are several mechanisms of resistance to carbapenems: 1) decreased permeability of the outer membrane of Gram-negative bacteria (due to diminished production of porins) causing reduced bacterial uptake, 2) reduced affinity of the target PBPs, 3) increased expression of efflux pump components, and 4) production of antibacterial drug-destroying enzymes (carbapenemases, metallo-beta-lactamases).
Cross-Resistance
Cross-resistance is sometimes observed with isolates resistant to other carbapenems.
Interaction with Other Antimicrobials
I n vitro tests show meropenem to act synergistically with aminoglycoside antibacterial drugs against some isolates of Pseudomonas aeruginosa.
Antimicrobial Activity
Meropenem has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections [see Indications and Usage (1)].
Gram-positive bacteria
- Enterococcus faecalis (vancomycin-susceptible isolates only)
- Staphylococcus aureus (methicillin-susceptible isolates only)
- Streptococcus agalactiae
- Streptococcus pneumoniae (penicillin-susceptible isolates only)
- Streptococcus pyogenes
- Viridans group streptococci
Gram-negative bacteria
- Escherichia coli
- Haemophilus influenzae
- Klebsiella pneumoniae
- Neisseria meningitidis
- Proteus mirabilis
- Pseudomonas aeruginosa
Anaerobic bacteria
- Bacteroides fragilis
- Bacteroides thetaiotaomicron
- Peptostreptococcus species
The following in vitro data are available, but their clinical significance is unknown. At least 90 percent of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for meropenem against isolates of similar genus or organism group. However, the efficacy of meropenem in treating clinical infections caused by these microorganisms has not been established in adequate and well-controlled clinical trials.
Gram-positive bacteria
- Staphylococcus epidermidis (methicillin-susceptible isolates only)
Gram-negative bacteria
- Aeromonas hydrophila
- Campylobacter jejuni
- Citrobacter freundii
- Citrobacter koseri
- Enterobacter cloacae
- Hafnia alvei
- Klebsiella oxytoca
- Moraxella catarrhalis
- Morganella morganii
- Pasteurella multocida
- Proteus vulgaris
- Serratia marcescens
Anaerobic bacteria
- Bacteroides ovatus
- Bacteroides uniformis
- Bacteroides ureolyticus
- Bacteroides vulgatus
- Clostridioides difficile
- Clostridium perfringens
- Eggerthella lenta
- Fusobacterium species
- Parabacteroides distasonis
- Porphyromonas asaccharolytica
- Prevotella bivia
- Prevotella intermedia
- Prevotella melaninogenica
- Propionibacterium acnes
Susceptibility Test Methods
For specific information regarding susceptibility test interpretive criteria, and associated test methods and quality control standards recognized by FDA for this drug, please see: http://www.fda.gov/STIC.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairmentof Fertility
Carcinogenesis:
Carcinogenesis studies have not been performed.
Mutagenesis:
Genetic toxicity studies were performed with meropenem using the bacterial reverse mutation test, the Chinese hamster ovary HGPRT assay, cultured human lymphocytes cytogenic assay, and the mouse micronucleus test. There was no evidence of mutagenic potential found in any of these tests.
Impairment of Fertility:
Reproductive studies performed with meropenem in rats at doses up to 1000 mg/kg/day, (approximately 1.8 times the human exposure at a dose of 1 gram every 8 hours based on AUC) showed no evidence of fertility impairment.
14 Clinical Studies
14.1 Complicated Skin and Skin Structure Infections
Adult patients with complicated skin and skin structure infections including complicated cellulitis, complex abscesses, perirectal abscesses, and skin infections requiring intravenous antimicrobials, hospitalization, and surgical intervention were enrolled in a randomized, multi-center, international, double-blind trial. The study evaluated meropenem at doses of 500 mg administered intravenously every 8 hours and imipenem-cilastatin at doses of 500 mg administered intravenously every 8 hours. The study compared the clinical response between treatment groups in the clinically evaluable population at the follow-up visit (test-of-cure). The trial was conducted in the United States, South Africa, Canada, and Brazil. At enrollment, approximately 37% of the patients had underlying diabetes, 12% had underlying peripheral vascular disease and 67% had a surgical intervention. The study included 510 patients randomized to meropenem and 527 patients randomized to imipenem-cilastatin. Two hundred and sixty one (261) patients randomized to meropenem and 287 patients randomized to imipenem-cilastatin were clinically evaluable. The success rates in the clinically evaluable patients at the follow-up visit were 86% (225/261) in the meropenem arm and 83% (238/287) in imipenem-cilastatin arm.
The success rates for clinically evaluable population are provided in Table 5.
Table 5: Success Rates at Test-of-Cure Visit for Clinically Evaluable Population with Complicated Skin and Skin Structure Infections
 Population  Meropenem for Injection n n=number of patients with satisfactory response. /NN=number of patients in the clinically evaluable population or respective subgroup within treatment groups. (%)  Imipenem-cilastatin n /N (%)  Total   225/261 (86)  238/287 (83)  Diabetes mellitus  83/97 (86)  76/105 (72)  No diabetes mellitus  142/164 (87)  162/182 (89)  Less than 65 years of age  190/218 (87) 205/241 (85)  65 years of age and older  35/43 (81)   33/46 (72)  Men  130/148 (88)  137/172 (80)  Women 95/113 (84) 101/115 (88)
The clinical efficacy rates by pathogen are provided in Table 6. The values represent the number of patients clinically cured/number of clinically evaluable patients at the post-treatment follow-up visit, with the percent cure in parentheses (Fully Evaluable analysis set).
Table 6: Clinical Efficacy Rates by Pathogen for Clinically Evaluable Population
 MICROORGANISMS Patients may have more than one pretreatment pathogen.  Meropenem for Injectionn n=number of patients with satisfactory response. /NN=number of patients in the clinically evaluable population or subgroup within treatment groups. (%)%= Percent of satisfactory clinical response at follow-up evaluation.   Imipenem-cilastatinn /N (%)    Gram-positive aerobes      Staphylococcus aureus, methicillin susceptible  82/88 (93)  84/100 (84)  Streptococcus pyogenes (Group A)  26/29 (90)  28/32 (88)  Streptococcus agalactiae (Group B)  12/17 (71)  16/19 (84)  Enterococcus faecalis  9/12 (75)  14/20 (70)  Viridans group streptococci  11/12 (92)  5/6 (83)  Gram-negative aerobes      Escherichia coli  12/15 (80)  15/21 (71)  Pseudomonas aeruginosa  11/15 (73)  13/15 (87)  Proteus mirabilis  11/13 (85)  6/7 (86)  Anaerobes      Bacteroides fragilis  10/11 (91)  9/10 (90)  Peptostreptococcus spp.  10/13 (77)  14/16 (88)
The proportion of patients who discontinued study treatment due to an adverse event was similar for both treatment groups (meropenem, 2.5% and imipenem-cilastatin, 2.7%).
14.2 Complicated Intra-Abdominal Infections
One controlled clinical study of complicated intra-abdominal infection was performed in the United States where meropenem was compared with clindamycin/tobramycin. Three controlled clinical studies of complicated intra-abdominal infections were performed in Europe; meropenem was compared with imipenem (two trials) and cefotaxime/metronidazole (one trial).
Using strict evaluability criteria and microbiologic eradication and clinical cures at follow-up which occurred 7 or more days after completion of therapy, the presumptive microbiologic eradication/clinical cure rates and statistical findings are provided in Table 7.
Table 7: Presumptive Microbiologic Eradication and Clinical Cure Rates at Test-of-Cure Visit in the Evaluable population with Complicated intra-abdominal infections
Treatment Arm  No. evaluable/No. enrolled (%) Microbiologic Eradication Rate Clinical Cure Rate Outcome  meropenem  146/516 (28%)  98/146 (67%)  101/146 (69%)    imipenem  65/220 (30%)  40/65 (62%)  42/65 (65%)  Meropenem equivalent to control  cefotaxime/metronidazole  26/85 (30%)  22/26 (85%)  22/26 (85%)  Meropenem not equivalent to control  clindamycin/tobramycin  50/212 (24%)  38/50 (76%)  38/50 (76%)  Meropenem equivalent to control
The finding that meropenem was not statistically equivalent to cefotaxime/metronidazole may have been due to uneven assignment of more seriously ill patients to the meropenem arm. Currently there is no additional information available to further interpret this observation.
14.3 Bacterial Meningitis
Four hundred forty-six patients (397 pediatric patients 3 months of age and older to below 17 years of age) were enrolled in 4 separate clinical trials and randomized to treatment with meropenem (n=225) at a dose of 40 mg/kg every 8 hours or a comparator drug, i.e., cefotaxime (n=187) or ceftriaxone (n=34), at the approved dosing regimens. A comparable number of patients were found to be clinically evaluable (ranging from 61-68%) and with a similar distribution of pathogens isolated on initial CSF culture.
Patients were defined as clinically not cured if any one of the following three criteria were met:
- At the 5-7 week post-completion of therapy visit, the patient had any one of the following: moderate to severe motor, behavior or development deficits, hearing loss of greater than 60 decibels in one or both ears, or blindness.
- During therapy the patient’s clinical status necessitated the addition of other antibacterial drugs.
- Either during or post-therapy, the patient developed a large subdural effusion needing surgical drainage, or a cerebral abscess, or a bacteriologic relapse.
Using the definition, the following efficacy rates were obtained, per organism (noted in Table 8). The values represent the number of patients clinically cured/number of clinically evaluable patients, with the percent cure in parentheses.
Table 8: Efficacy Rates by Pathogen in the Clinically Evaluable Population with Bacterial Meningitis
 MICROORGANISMS  MEROPENEM FOR INJECTION COMPARATOR    S. pneumoniae 17/24 (71) 19/30 (63)    H. influenzae (+) (+) beta-lactamase-producing  8/10 (80) 6/6 (100)    H. influenzae (-/NT) (-/NT) non-beta-lactamase-producing or not tested  44/59 (75) 44/60 (73)    N. meningitidis 30/35 (86)   35/39 (90)    Total (including others) 102/131 (78)   108/140 (77)  
Sequelae were the most common reason patients were assessed as clinically not cured.
Five patients were found to be bacteriologically not cured, 3 in the comparator group (1 relapse and 2 patients with cerebral abscesses) and 2 in the meropenem group (1 relapse and 1 with continued growth of Pseudomonas aeruginosa).
With respect to hearing loss, 263 of the 271 evaluable patients had at least one hearing test performed post-therapy. The following table shows the degree of hearing loss between the meropenem-treated patients and the comparator-treated patients.
Table 9: Hearing Loss at Post-Therapy in the Evaluable Population treated with Meropenem
Degree of Hearing Loss (in one or both ears)    Meropenem n = 128 Comparator n = 135    No loss  61%  56%  20-40 decibels  20%  24% greater than 40-60 decibels  8%  7% greater than 60 decibels  9%  10%
15 References
Cockcroft DW, MH Gault, 1976, Prediction of creatinine clearance from serum creatinine, Nephron, 16:31-41.
Kawamura S, AW Russell, SJ Freeman, and RA Siddall, 1992, Reproductive and Developmental Toxicity of Meropenem in Rats, Chemotherapy, 40:S238-250.
16 How Supplied/storage And Handling
Meropenem for Injection USP and Sodium Chloride Injection USP in the DUPLEX¬ģ Container is a flexible dual chamber single-dose container supplied in two concentrations. The diluent chamber contains approximately 50 mL of 0.9% Sodium Chloride Injection USP. After reconstitution, the¬†delivered doses are equivalent to 500Anhydrous basis. mg and 1gram meropenem.
Meropenem for Injection USP and Sodium Chloride Injection USP is supplied sterile and nonpyrogenic in the DUPLEX¬ģ Container¬†packaged 24 units per case.
 NDC  REF  Dose  Volume  0264-3183-11  3183-11  500 mg  50 mL  0264-3185-11  3185-11  1 gram  50 mL
Store the unactivated unit at 20¬įC‚Äď25¬įC (68¬įF‚Äď77¬įF). Excursion permitted to 15¬įC-30¬įC. [See USP Controlled Room Temperature.] Protect from freezing.
Use only if prepared solution is clear and free from particulate matter.
17 Patient Counseling Information
- Patients should be counseled that antibacterial drugs including Meropenem for Injection and Sodium Chloride Injection should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Meropenem for Injection and Sodium Chloride Injection is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Meropenem for Injection and Sodium Chloride Injection or other antibacterial drugs in the future. 
- Counsel patients that diarrhea is a common problem caused by antibacterial drugs which usually ends when the antibacterial drug is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial drug. If this occurs, patients should contact their physician as soon as possible [see Warnings and Precautions (5.5)].
- Counsel patients to inform their physician if they are taking valproic acid or divalproex sodium. Valproic acid concentrations in the blood may drop below the therapeutic range upon co-administration with Meropenem for Injection and Sodium Chloride Injection. If treatment with Meropenem for Injection and Sodium Chloride Injection is necessary and continued, alternative or supplemental anti-convulsant medication to prevent and/or treat seizures may be needed [see Warnings and Precautions (5.4)].
- Patients receiving Meropenem for Injection and Sodium Chloride Injection on an outpatient basis must be alerted of adverse events such as seizures, delirium, headaches and/or paresthesias that could interfere with mental alertness and/or cause motor impairment. Until it is reasonably well established that Meropenem for Injection and Sodium Chloride Injection is well tolerated, patients should not operate machinery or motorized vehicles [see Warnings and Precautions (5.9)].
- Meropenem for Injection and Sodium Chloride Injection contains a high sodium load. Instruct patients to inform or report symptoms of difficulty breathing, swelling, or increased weight [see Warnings and Precautions (5.10)].
DUPLEX is a registered trademark of B. Braun Medical Inc.ATCC is a registered trademark of the American Type Culture Collection
Manufactured for: B. Braun Medical Inc. Bethlehem, PA 18018-3524 USA1-800-227-2862
Manufactured by:ACS Dobfar S.p.A.Prepared in Italy. API from Italy and Austria.
Y36-003-008 LD-244-4
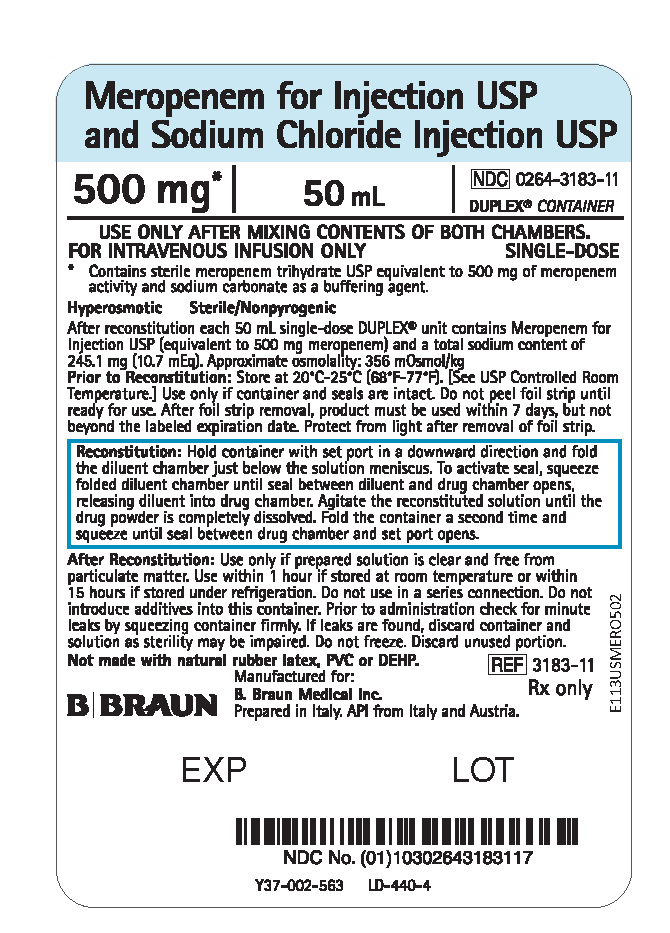
Principal Display Panel - 500 Mg
Meropenem for Injection USP and Sodium Chloride Injection USP
500 mg*
50 mL
NDC  0264-3183-11
DUPLEX¬ģ CONTAINER
USE ONLY AFTER MIXING CONTENTS OF BOTH CHAMBERS.
FOR INTRAVENOUS INFUSION ONLY
SINGLE-DOSE
*  Contains sterile meropenem trihydrate USP equivalent to 500 mg of meropenem activity and sodium carbonate as a buffering agent.
Hyperosmotic              Sterile/Nonpyrogenic
After reconstitution each 50 mL single-dose DUPLEX¬ģ unit contains Meropenem for Injection USP (equivalent to 500 mg meropenem) and a total sodium content of 245.1 mg (10.7 mEq). Approximate osmolality: 356 mOsmol/kg
Prior to Reconstitution: Store at 20¬įC-25¬įC (68¬įF-77¬įF). [See USP Controlled Room Temperature.] Use only if container and seals are intact. Do not peel foil strip until ready for use. After foil strip removal, product must be used within 7 days, but not beyond the labeled expiration date. Protect from light after removal of foil strip.
Reconstitution: Hold container with set port in a downward direction and fold the diluent chamber just below the solution meniscus. To activate seal, squeeze folded diluent chamber until seal between diluent and drug chamber opens, releasing diluent into drug chamber. Agitate the reconstituted solution until the drug powder is completely dissolved. Fold the container a second time and squeeze until seal between drug chamber and set port opens.
After Reconstitution: Use only if prepared solution is clear and free from particulate matter. Use within 1 hour if stored at room temperature or within 15 hours if stored under refrigeration. Do not use in a series connection. Do not introduce additives into this container. Prior to administration check for minute leaks by squeezing container firmly. If leaks are found, discard container and solution as sterility may be impaired. Do not freeze. Discard unused portion.
Not made with natural rubber latex, PVC or DEHP.
REF  3183-11
Rx only
E113USMERO502
Manufactured for: B. Braun Medical Inc.
Prepared in Italy. API from Italy and Austria.
Y37-002-563     LD-440-4
EXP
LOT
Principal Display Panel - 1 G
Meropenem for Injection USP and Sodium Chloride Injection USP
1 g*
50 mL
NDC  0264-3185-11
DUPLEX¬ģ CONTAINER
USE ONLY AFTER MIXING CONTENTS OF BOTH CHAMBERS.
FOR INTRAVENOUS INFUSION ONLY
SINGLE-DOSE
*  Contains sterile meropenem trihydrate USP equivalent to 1 g of meropenem activity and sodium carbonate as a buffering agent.
Hyperosmotic           Sterile/Nonpyrogenic
After reconstitution each 50 mL single-dose DUPLEX¬ģ unit contains Meropenem for Injection USP (equivalent to 1 g meropenem) and a total sodium content of 290.2 mg (12.6 mEq). Approximate osmolality: 417 mOsmol/kg
Prior to Reconstitution: Store at 20¬įC-25¬įC (68¬įF-77¬įF).¬† [See USP Controlled Room Temperature.] Use only if container and seals are intact. Do not peel foil strip until ready for use. After foil strip removal, product must be used within 7 days, but not beyond the labeled expiration date. Protect from light after removal of foil strip.
Reconstitution: Hold container with set port in a downward direction and fold the diluent chamber just below the solution meniscus. To activate seal, squeeze folded diluent chamber until seal between diluent and drug chamber opens, releasing diluent into drug chamber. Agitate the reconstituted solution until the drug powder is completely dissolved. Fold the container a second time and squeeze until seal between drug chamber and set port opens.
After Reconstitution: Use only if prepared solution is clear and free from particulate matter. Use within 1 hour if stored at room temperature or within 15 hours if stored under refrigeration. Do not use in a series connection. Do not introduce additives into this container. Prior to administration check for minute leaks by squeezing container firmly. If leaks are found, discard container and solution as sterility may be impaired. Do not freeze. Discard unused portion.
Not made with natural rubber latex, PVC or DEHP.
REF  3185-11
Rx only
E113USMERO102
Manufactured for: B. Braun Medical Inc.
Prepared in Italy. API from Italy and Austria.
Y37-002-564     LD-439-4
EXP
LOT

Package Label.principal Display Panel
PEEL HERE
Drug Chamber Discard unit if foil strip is damaged. Peel foil strip only when ready for use. Visually inspect drug prior to reconstitution.
See package insert for complete directions for reconstitution and administration.
LD-336-1  X27-001-485

DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site

