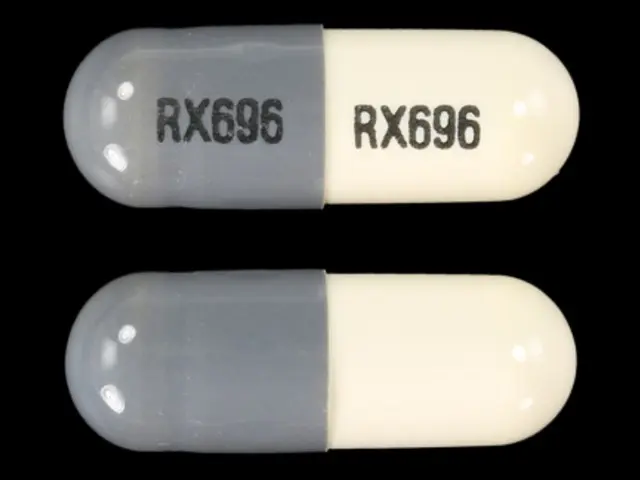
MINOCYCLINE HYDROCHLORIDE (minocycline hydrochloride 100 mg) Dailymed
Generic: minocycline hydrochloride is used for the treatment of Acne Vulgaris Anthrax Borrelia Infections Chancroid Cholera Escherichia coli Infections Hypersensitivity Meningococcal Infections Mycoplasma Infections Psittacosis Plague Pregnancy Respiratory Tract Infections Rocky Mountain Spotted Fever Trachoma Tularemia
Go PRO for all pill images
Indications & Usage Section
Pantoprazole sodium delayed-release tablets USP are indicated for:
1.1 Short-Term Treatment of Erosive Esophagitis Associated With Gastroesophageal Reflux Disease (GERD) Pantoprazole sodium delayed-release tablets USP are indicated in adults for the short-term treatment (up to 8 weeks) in the healing and symptomatic relief of erosive esophagitis. For those adult patients who have not healed after 8 weeks of treatment, an additional 8 week course of pantoprazole sodium delayed-release tablets USP may be considered. Safety of treatment beyond 8 weeks in pediatric patients has not been established.
1.2 Maintenance of Healing of Erosive Esophagitis Pantoprazole sodium delayed-release tablets USP are indicated for maintenance of healing of erosive esophagitis and reduction in relapse rates of daytime and nighttime heartburn symptoms in adult patients with GERD. Controlled studies did not extend beyond 12 months.
1.3 Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome Pantoprazole sodium delayed-release tablets USP are indicated for the long-term treatment of pathological hypersecretory conditions, including Zollinger-Ellison syndrome.
Dosage & Administration Section
2.1 Recommended Dosing Schedule
Pantoprazole sodium is supplied as delayed-release tablets. The recommended dosages are outlined inTable 1.
Table 1: Recommended Dosing Schedule for Pantoprazole Sodium Delayed-Release Tablets
* For adult patients who have not healed after 8 weeks of treatment, an additional 8 week course of pantoprazole sodium delayed-release tablets may be considered. †Controlled studies did not extend beyond 12 months ‡ Dosage regimens should be adjusted to individual patient needs and should continue for as long as clinically indicated. Doses up to 240 mg daily have been administered.
Indication
Dose
Frequency
Short-Term Treatment of Erosive Esophagitis Associated With GERD
Adults
40 mg
Once daily for up to 8 weeks*
Children (5 Years and Older)
≥ 15 kg to < 40 kg
20 mg
Once Daily for up to 8 wks
≥ 40 kg
40 mg
Maintenance of Healing of Erosive Esophagitis
Adults
40 mg
Once dailyâ€
Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
Adults
40 mg
Twice daily‡
2.2 Administration Instructions
Directions for method of administration are presented in Table 2.
Table 2: Administration Instructions
* Patients should be cautioned that pantoprazole sodium delayed-release tablets should not be split, chewed, or crushed.
Formulation
Route
Instructions*
Delayed-Release Tablets
Oral
Swallowed whole, with or without food
Pantoprazole Sodium Delayed-Release Tablets
Pantoprazole sodium delayed-release tablets should be swallowed whole, with or without food in the stomach. If patients are unable to swallow a 40 mg tablet, two 20 mg tablets may be taken. Concomitant administration of antacids does not affect the absorption of pantoprazole sodium delayed-release tablets.
Dosage Forms & Strengths Section
Delayed-Release Tablets:
• 20 mg: Yellow, oval shaped, unscored tablets imprinted with black ink on one side of the tablet “93/11” and plain on the other side. • 40 mg: Yellow, oval shaped, unscored tablets imprinted with black ink on one side of the tablet “93/12” and plain on the other side.
Contraindications Section
Pantoprazole sodium delayed-release tablets are contraindicated in patients with known hypersensitivity to any component of the formulation or any substituted benzimidazole. Hypersensitivity reactions may include anaphylaxis, anaphylactic shock, angioedema, bronchospasm, acute interstitial nephritis, and urticaria [see Adverse Reactions (6)].
Warnings And Precautions Section
5.1 Concurrent Gastric Malignancy Symptomatic response to therapy with pantoprazole does not preclude the presence of gastric malignancy.
5.2 Atrophic Gastritis Atrophic gastritis has been noted occasionally in gastric corpus biopsies from patients treated long-term with pantoprazole, particularly in patients who were H. pylori positive.
5.3 Acute Interstitial Nephritis Acute interstitial nephritis has been observed in patients taking PPIs including pantoprazole. Acute interstitial nephritis may occur at any point during PPI therapy and is generally attributed to an idiopathic hypersensitivity reaction. Discontinue pantoprazole if acute interstitial nephritis develops [see Contraindications (4)].
5.4 Cyanocobalamin (Vitamin B-12) Deficiency Generally, daily treatment with any acid-suppressing medications over a long period of time (e.g., longer than 3 years) may lead to malabsorption of cyanocobalamin (Vitamin B-12) caused by hypo- or achlorhydria. Rare reports of cyanocobalamin deficiency occurring with acid-suppressing therapy have been reported in the literature. This diagnosis should be considered if clinical symptoms consistent with cyanocobalamin deficiency are observed.
5.5 Clostridium difficile Associated Diarrhea Published observational studies suggest that PPI therapy like pantoprazole may be associated with an increased risk of Clostridium difficile associated diarrhea, especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve [see Adverse Reactions (6.2)].
Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
5.6 Bone Fracture Several published observational studies suggest that proton pump inhibitor (PPI) therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (2) and Adverse Reactions (6.2)].
5.7 Hypomagnesemia Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (6.2)].
5.8 Tumorigenicity Due to the chronic nature of GERD, there may be a potential for prolonged administration of pantoprazole. In long-term rodent studies, pantoprazole was carcinogenic and caused rare types of gastrointestinal tumors. The relevance of these findings to tumor development in humans is unknown [see Nonclinical Toxicology (13.1)].
5.9 Interference With Urine Screen for THC See Drug Interactions (7.5).
5.10 Concomitant Use of Pantoprazole With Methotrexate Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of the PPI may be considered in some patients [see Drug Interactions (7.6)].
Adverse Reactions Section
6.1 Clinical Trial Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Adults
Safety in nine randomized comparative U.S. clinical trials in patients with GERD included 1,473 patients on oral pantoprazole (20 mg or 40 mg), 299 patients on an H2-receptor antagonist, 46 patients on another proton pump inhibitor, and 82 patients on placebo. The most frequently occurring adverse reactions are uled in Table 3.
Table 3: Adverse Reactions Reported in Clinical Trials of Adult Patients With GERD at a Frequency of > 2% Pantoprazole
Comparators
Placebo
(n = 1473)
(n = 345)
(n = 82)
%
%
%
Headache
12.2
12.8
8.5
Diarrhea
8.8
9.6
4.9
Nausea
7.0
5.2
9.8
Abdominal pain
6.2
4.1
6.1
Vomiting
4.3
3.5
2.4
Flatulence
3.9
2.9
3.7
Dizziness
3.0
2.9
1.2
Arthralgia
2.8
1.4
1.2
Additional adverse reactions that were reported for pantoprazole in clinical trials with a frequency of ≤ 2% are uled below by body system:
Body as a Whole: allergic reaction, pyrexia, photosensitivity reaction, facial edema
Gastrointestinal: constipation, dry mouth, hepatitis
Hematologic: leukopenia, thrombocytopenia
Metabolic/Nutritional: elevated CK (creatine kinase), generalized edema, elevated triglycerides, liver enzymes elevated
Musculoskeletal: myalgia
Nervous: depression, vertigo
Skin and Appendages: urticaria, rash, pruritus
Special Senses: blurred vision
Pediatric Patients
Safety of pantoprazole in the treatment of Erosive Esophagitis (EE) associated with GERD was evaluated in pediatric patients ages 1 year through 16 years in three clinical trials. Safety trials involved pediatric patients with EE; however, as EE is uncommon in the pediatric population, 249 pediatric patients with endoscopically-proven or symptomatic GERD were also evaluated. All adult adverse reactions to pantoprazole are considered relevant to pediatric patients. In patients ages 1 year through 16 years, the most commonly reported (> 4%) adverse reactions include: URI, headache, fever, diarrhea, vomiting, rash, and abdominal pain.
For safety information in patients less than 1 year of age see Use in Specific Populations (8.4).
Additional adverse reactions that were reported for pantoprazole in pediatric patients in clinical trials with a frequency of ≤ 4% are uled below by body system:
Body as a Whole: allergic reaction, facial edema
Gastrointestinal: constipation, flatulence, nausea
Metabolic/Nutritional: elevated triglycerides, elevated liver enzymes, elevated CK (creatine kinase)
Musculoskeletal: arthralgia, myalgia
Nervous: dizziness, vertigo
Skin and Appendages: urticaria
The following adverse reactions seen in adults in clinical trials were not reported in pediatric patients in clinical trials, but are considered relevant to pediatric patients: photosensitivity reaction, dry mouth, hepatitis, thrombocytopenia, generalized edema, depression, pruritus, leukopenia, and blurred vision.
Zollinger-Ellison Syndrome
In clinical studies of Zollinger-Ellison syndrome, adverse reactions reported in 35 patients taking pantoprazole 80 mg/day to 240 mg/day for up to 2 years were similar to those reported in adult patients with GERD.
6.2 Postmarketing Experience The following adverse reactions have been identified during postapproval use of pantoprazole. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
These adverse reactions are uled below by body system:
General Disorders and Administration Conditions: asthenia, fatigue, malaise
Hematologic: pancytopenia, agranulocytosis
Hepatobiliary Disorders: hepatocellular damage leading to jaundice and hepatic failure
Immune System Disorders: anaphylaxis (including anaphylactic shock)
Infections and Infestations: Clostridium difficile associated diarrhea
Investigations: weight changes
Metabolism and Nutritional Disorders: hyponatremia, hypomagnesemia
Musculoskeletal Disorders: rhabdomyolysis, bone fracture
Nervous: ageusia, dysgeusia
Psychiatric Disorders: hallucination, confusion, insomnia, somnolence
Renal and Urinary Disorders: interstitial nephritis
Skin and Subcutaneous Tissue Disorders: severe dermatologic reactions (some fatal), including erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis (TEN, some fatal), and angioedema (Quincke’s edema)
Drug Interactions Section
7.1 Interference With Antiretroviral Therapy Concomitant use of atazanavir or nelfinavir with proton pump inhibitors is not recommended. Coadministration of atazanavir or nelfinavir with proton pump inhibitors is expected to substantially decrease atazanavir or nelfinavir plasma concentrations and may result in a loss of therapeutic effect and development of drug resistance.
7.2 Coumarin Anticoagulants There have been postmarketing reports of increased INR and prothrombin time in patients receiving proton pump inhibitors, including pantoprazole, and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly should be monitored for increases in INR and prothrombin time.
7.3 Clopidogrel Concomitant administration of pantoprazole and clopidogrel in healthy subjects had no clinically important effect on exposure to the active metabolite of clopidogrel or clopidogrel-induced platelet inhibition [see Clinical Pharmacology (12.3)]. No dose adjustment of clopidogrel is necessary when administered with an approved dose of pantoprazole.
7.4 Drugs for Which Gastric pH Can Affect Bioavailability Due to its effects on gastric acid secretion, pantoprazole can reduce the absorption of drugs where gastric pH is an important determinant of their bioavailability. Like with other drugs that decrease the intragastric acidity, the absorption of drugs such as ketoconazole, ampicillin esters, atazanavir, iron salts, erlotinib, and mycophenolate mofetil (MMF) can decrease.
Coadministration of pantoprazole in healthy subjects and in transplant patients receiving MMF has been reported to reduce the exposure to the active metabolite, mycophenolic acid (MPA), possibly due to a decrease in MMF solubility at an increased gastric pH. The clinical relevance of reduced MPA exposure on organ rejection has not been established in transplant patients receiving pantoprazole and MMF. Use pantoprazole with caution in transplant patients receiving MMF [see Clinical Pharmacology (12.3)].
7.5 False Positive Urine Tests for THC There have been reports of false positive urine screening tests for tetrahydrocannabinol (THC) in patients receiving proton pump inhibitors. An alternative confirmatory method should be considered to verify positive results.
7.6 Methotrexate Case reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose; see methotrexate prescribing information) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of Methotrexate with PPIs have been conducted [see Warnings and Precautions (5.10)].
Use In Specific Populations Section
8.1 Pregnancy Teratogenic Effects
Pregnancy Category B
Reproduction studies have been performed in rats at oral doses up to 88 times the recommended human dose and in rabbits at oral doses up to 16 times the recommended human dose and have revealed no evidence of impaired fertility or harm to the fetus due to pantoprazole. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed [see Nonclinical Toxicology (13.2)].
8.3 Nursing Mothers Pantoprazole and its metabolites are excreted in the milk of rats. Pantoprazole excretion in human milk has been detected in a study of a single nursing mother after a single 40 mg oral dose. The clinical relevance of this finding is not known. Many drugs which are excreted in human milk have a potential for serious adverse reactions in nursing infants. Based on the potential for tumorigenicity shown for pantoprazole in rodent carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the benefit of the drug to the mother.
8.4 Pediatric Use The safety and effectiveness of pantoprazole for short-term treatment (up to eight weeks) of erosive esophagitis (EE) associated with GERD have been established in pediatric patients 1 year through 16 years of age. Effectiveness for EE has not been demonstrated in patients less than 1 year of age. In addition, for patients less than 5 years of age, there is no appropriate dosage strength in an age-appropriate formulation available. Therefore, pantoprazole is indicated for the short-term treatment of EE associated with GERD for patients 5 years and older. The safety and effectiveness of pantoprazole for pediatric uses other than EE have not been established.
1 Year Through 16 Years of Age
Use of pantoprazole in pediatric patients 1 year through 16 years of age for short-term treatment (up to eight weeks) of EE associated with GERD is supported by: a) extrapolation of results from adequate and well-controlled studies that supported the approval of pantoprazole for treatment of EE associated with GERD in adults, and b) safety, effectiveness, and pharmacokinetic studies performed in pediatric patients [see Clinical Studies (14.1), and Clinical Pharmacology (12.3)].
Safety of pantoprazole in the treatment of EE associated with GERD in pediatric patients 1 through 16 years of age was evaluated in three multicenter, randomized, double-blind, parallel-treatment studies, involving 249 pediatric patients, including 8 with EE (4 patients ages 1 year to 5 years and 4 patients 5 years to 11 years). The children ages 1 year to 5 years with endoscopically diagnosed EE (defined as an endoscopic Hetzel-Dent score ≥ 2) were treated once daily for 8 weeks with one of two dose levels of pantoprazole (approximating 0.6 mg/kg or 1.2 mg/kg). All 4 of these patients with EE were healed (Hetzel-Dent score of 0 or 1) at 8 weeks. Because EE is uncommon in the pediatric population, predominantly pediatric patients with endoscopically-proven or symptomatic GERD were also included in these studies. Patients were treated with a range of doses of pantoprazole once daily for 8 weeks. For safety findings see Adverse Reactions (6.1). Because these pediatric trials had no placebo, active comparator, or evidence of a dose response, the trials were inconclusive regarding the clinical benefit of pantoprazole for symptomatic GERD in the pediatric population. The effectiveness of pantoprazole for treating symptomatic GERD in pediatric patients has not been established.
Although the data from the clinical trials support use of pantoprazole for the short-term treatment of EE associated with GERD in pediatric patients 1 year through 5 years, there is no commercially available dosage formulation appropriate for patients less than 5 years of age [see Dosage and Administration (2)].
In a population pharmacokinetic analysis, clearance values in the children 1 to 5 years old with endoscopically proven GERD had a median value of 2.4 L/h. Following a 1.2 mg/kg equivalent dose (15 mg for ≤ 12.5 kg and 20 mg for > 12.5 to < 25 kg), the plasma concentrations of pantoprazole were highly variable and the median time to peak plasma concentration was 3 to 6 hours. The estimated AUC for patients 1 to 5 years old was 37% higher than for adults receiving a single 40 mg tablet, with a geometric mean AUC value of 6.8 mcg•hr/mL.
Neonates to Less Than One Year of Age
Pantoprazole was not found to be effective in a multicenter, randomized, double-blind, placebo-controlled, treatment-withdrawal study of 129 pediatric patients 1 through 11 months of age. Patients were enrolled if they had symptomatic GERD based on medical history and had not responded to non-pharmacologic interventions for GERD for two weeks. Patients received pantoprazole daily for four weeks in an open-label phase, then patients were randomized in equal proportion to receive pantoprazole treatment or placebo for the subsequent four weeks in a double-blind manner. Efficacy was assessed by observing the time from randomization to study discontinuation due to symptom worsening during the four-week treatment-withdrawal phase. There was no statistically significant difference between pantoprazole and placebo in the rate of discontinuation.
In this trial, the adverse reactions that were reported more commonly (difference of ≥ 4%) in the treated population compared to the placebo population were elevated CK, otitis media, rhinitis, and laryngitis.
In a population pharmacokinetic analysis, the systemic exposure was higher in patients less than 1 year of age with GERD compared to adults who received a single 40 mg dose (geometric mean AUC was 103% higher in preterm infants and neonates receiving single dose of 2.5 mg of pantoprazole, and 23% higher in infants 1 through 11 months of age receiving a single dose of approximately 1.2 mg/kg). In these patients, the apparent clearance (CL/F) increased with age (median clearance: 0.6 L/hr, range: 0.03 to 3.2 L/hr).
These doses resulted in pharmacodynamic effects on gastric but not esophageal pH. Following once daily dosing of 2.5 mg of pantoprazole in preterm infants and neonates, there was an increase in the mean gastric pH (from 4.3 at baseline to 5.2 at steady-state) and in the mean % time that gastric pH was > 4 (from 60% at baseline to 80% at steady-state). Following once daily dosing of approximately 1.2 mg/kg of pantoprazole in infants 1 through 11 months of age, there was an increase in the mean gastric pH (from 3.1 at baseline to 4.2 at steady-state) and in the mean % time that gastric pH was > 4 (from 32% at baseline to 60% at steady-state). However, no significant changes were observed in mean intraesophageal pH or % time that esophageal pH was < 4 in either age group.
Because pantoprazole was not shown to be effective in the randomized, placebo-controlled study in this age group, the use of pantoprazole for treatment of symptomatic GERD in infants less than 1 year of age is not indicated.
8.5 Geriatric Use In short-term U.S. clinical trials, erosive esophagitis healing rates in the 107 elderly patients (≥ 65 years old) treated with pantoprazole were similar to those found in patients under the age of 65. The incidence rates of adverse reactions and laboratory abnormalities in patients aged 65 years and older were similar to those associated with patients younger than 65 years of age.
8.6 Gender Erosive esophagitis healing rates in the 221 women treated with pantoprazole sodium delayed-release tablets in U.S. clinical trials were similar to those found in men. In the 122 women treated long-term with pantoprazole 40 mg or 20 mg, healing was maintained at a rate similar to that in men. The incidence rates of adverse reactions were also similar for men and women.
8.7 Patients With Hepatic Impairment Doses higher than 40 mg/day have not been studied in patients with hepatic impairment [see Clinical Pharmacology (12.3)].
Overdosage Section
Experience in patients taking very high doses of pantoprazole (> 240 mg) is limited. Spontaneous postmarketing reports of overdose are generally within the known safety profile of pantoprazole.
Pantoprazole is not removed by hemodialysis. In case of overdosage, treatment should be symptomatic and supportive.
Single oral doses of pantoprazole at 709 mg/kg, 798 mg/kg, and 887 mg/kg were lethal to mice, rats, and dogs, respectively. The symptoms of acute toxicity were hypoactivity, ataxia, hunched sitting, limb-splay, lateral position, segregation, absence of ear reflex, and tremor.
Overdosage Section
Experience in patients taking very high doses of pantoprazole (> 240 mg) is limited. Spontaneous postmarketing reports of overdose are generally within the known safety profile of pantoprazole.
Pantoprazole is not removed by hemodialysis. In case of overdosage, treatment should be symptomatic and supportive.
Single oral doses of pantoprazole at 709 mg/kg, 798 mg/kg, and 887 mg/kg were lethal to mice, rats, and dogs, respectively. The symptoms of acute toxicity were hypoactivity, ataxia, hunched sitting, limb-splay, lateral position, segregation, absence of ear reflex, and tremor.
Clinical Pharmacology Section
12.1 Mechanism of Action Pantoprazole is a proton pump inhibitor (PPI) that suppresses the final step in gastric acid production by covalently binding to the (H+, K+)-ATPase enzyme system at the secretory surface of the gastric parietal cell. This effect leads to inhibition of both basal and stimulated gastric acid secretion, irrespective of the stimulus. The binding to the (H+, K+)-ATPase results in a duration of antisecretory effect that persists longer than 24 hours for all doses tested (20 mg to 120 mg).
12.2 Pharmacodynamics Antisecretory Activity
Under maximal acid stimulatory conditions using pentagastrin, a dose-dependent decrease in gastric acid output occurs after a single dose of oral (20 to 80 mg) or a single dose of intravenous (20 to 120 mg) pantoprazole in healthy volunteers. Pantoprazole given once daily results in increasing inhibition of gastric acid secretion. Following the initial oral dose of 40 mg pantoprazole, a 51% mean inhibition was achieved by 2.5 hours. With once-a-day dosing for 7 days, the mean inhibition was increased to 85%. Pantoprazole suppressed acid secretion in excess of 95% in half of the subjects. Acid secretion had returned to normal within a week after the last dose of pantoprazole; there was no evidence of rebound hypersecretion.
In a series of dose-response studies, pantoprazole, at oral doses ranging from 20 to 120 mg, caused dose-related increases in median basal gastric pH and in the percent of time gastric pH was > 3 and > 4. Treatment with 40 mg of pantoprazole produced significantly greater increases in gastric pH than the 20 mg dose. Doses higher than 40 mg (60, 80, 120 mg) did not result in further significant increases in median gastric pH. The effects of pantoprazole on median pH from one double-blind crossover study are shown in Table 4.
Table 4: Effect of Single Daily Doses of Oral Pantoprazole on Intragastric pH * Significantly different from placebo †Significantly different from 20 mg Median pH on Day 7
Time
Placebo
20 mg
40 mg
80 mg
8 a.m. to 8 a.m.
(24 Hours)
1.3
2.9*
3.8*,â€
3.9*,â€
8 a.m. to 10 p.m.
(Daytime)
1.6
3.2*
4.4*,â€
4.8*,â€
10 p.m. to 8 a.m.
(Nighttime)
1.2
2.1*
3.0*
2.6*
Serum Gastrin Effects
Fasting serum gastrin levels were assessed in two double-blind studies of the acute healing of erosive esophagitis (EE) in which 682 patients with gastroesophageal reflux disease (GERD) received 10, 20, or 40 mg of pantoprazole for up to 8 weeks. At 4 weeks of treatment there was an increase in mean gastrin levels of 7%, 35%, and 72% over pretreatment values in the 10, 20, and 40 mg treatment groups, respectively. A similar increase in serum gastrin levels was noted at the 8 week visit with mean increases of 3%, 26%, and 84% for the three pantoprazole dose groups. Median serum gastrin levels remained within normal limits during maintenance therapy with pantoprazole sodium delayed-release tablets.
In long-term international studies involving over 800 patients, a 2 to 3 fold mean increase from the pretreatment fasting serum gastrin level was observed in the initial months of treatment with pantoprazole at doses of 40 mg per day during GERD maintenance studies and 40 mg or higher per day in patients with refractory GERD. Fasting serum gastrin levels generally remained at approximately 2 to 3 times baseline for up to 4 years of periodic follow-up in clinical trials.
Following short-term treatment with pantoprazole, elevated gastrin levels return to normal by at least 3 months.
Enterochromaffin-Like (ECL) Cell Effects
In 39 patients treated with oral pantoprazole 40 mg to 240 mg daily (majority receiving 40 mg to 80 mg) for up to 5 years, there was a moderate increase in ECL-cell density, starting after the first year of use, which appeared to plateau after 4 years.
In a nonclinical study in Sprague-Dawley rats, lifetime exposure (24 months) to pantoprazole at doses of 0.5 to 200 mg/kg/day resulted in dose-related increases in gastric ECL cell proliferation and gastric neuroendocrine (NE)-cell tumors. Gastric NE-cell tumors in rats may result from chronic elevation of serum gastrin concentrations. The high density of ECL cells in the rat stomach makes this species highly susceptible to the proliferative effects of elevated gastrin concentrations produced by proton pump inhibitors. However, there were no observed elevations in serum gastrin following the administration of pantoprazole at a dose of 0.5 mg/kg/day. In a separate study, a gastric NE-cell tumor without concomitant ECL-cell proliferative changes was observed in 1 female rat following 12 months of dosing with pantoprazole at 5 mg/kg/day and a 9 month off-dose recovery [see Nonclinical Toxicology (13.1)].
12.3 Pharmacokinetics Pantoprazole sodium delayed-release tablets are prepared as enteric-coated tablets so that absorption of pantoprazole begins only after the tablet leaves the stomach. Peak serum concentration (Cmax) and area under the serum concentration time curve (AUC) increase in a manner proportional to oral and intravenous doses from 10 mg to 80 mg. Pantoprazole does not accumulate, and its pharmacokinetics are unaltered with multiple daily dosing. Following oral or intravenous administration, the serum concentration of pantoprazole declines biexponentially, with a terminal elimination half-life of approximately one hour.
In extensive metabolizers with normal liver function receiving an oral dose of the enteric-coated 40 mg pantoprazole tablet, the peak concentration (Cmax) is 2.5 mcg/mL; the time to reach the peak concentration (tmax) is 2.5 h, and the mean total area under the plasma concentration versus time curve (AUC) is 4.8 mcg•h/mL (range 1.4 to 13.3 mcg•h/mL). Following intravenous administration of pantoprazole to extensive metabolizers, its total clearance is 7.6 to 14.0 L/h, and its apparent volume of distribution is 11.0 to 23.6 L.
Absorption
After administration of a single or multiple oral 40 mg doses of pantoprazole sodium delayed-release tablets, the peak plasma concentration of pantoprazole was achieved in approximately 2.5 hours, and Cmax was 2.5 mcg/mL. Pantoprazole undergoes little first-pass metabolism, resulting in an absolute bioavailability of approximately 77%. Pantoprazole absorption is not affected by concomitant administration of antacids.
Administration of pantoprazole sodium delayed-release tablets with food may delay its absorption up to 2 hours or longer; however, the Cmax and the extent of pantoprazole absorption (AUC) are not altered. Thus, pantoprazole sodium delayed-release tablets may be taken without regard to timing of meals.
Distribution
The apparent volume of distribution of pantoprazole is approximately 11.0 to 23.6 L, distributing mainly in extracellular fluid. The serum protein binding of pantoprazole is about 98%, primarily to albumin.
Metabolism
Pantoprazole is extensively metabolized in the liver through the cytochrome P450 (CYP) system. Pantoprazole metabolism is independent of the route of administration (intravenous or oral). The main metabolic pathway is demethylation, by CYP2C19, with subsequent sulfation; other metabolic pathways include oxidation by CYP3A4. There is no evidence that any of the pantoprazole metabolites have significant pharmacologic activity.
Elimination
After a single oral or intravenous dose of 14C-labeled pantoprazole to healthy, normal metabolizer volunteers, approximately 71% of the dose was excreted in the urine, with 18% excreted in the feces through biliary excretion. There was no renal excretion of unchanged pantoprazole.
Geriatric
Only slight to moderate increases in pantoprazole AUC (43%) and Cmax (26%) were found in elderly volunteers (64 to 76 years of age) after repeated oral administration, compared with younger subjects. No dosage adjustment is recommended based on age.
Pediatric
The pharmacokinetics of pantoprazole were studied in children less than 16 years of age in four randomized, open-label clinical trials in pediatric patients with presumed/proven GERD. A pediatric granule formulation was studied in children through 5 years of age, and pantoprazole delayed-release tablets were studied in children older than 5 years.
In a population PK analysis, total clearance increased with increasing bodyweight in a non-linear fashion. The total clearance also increased with increasing age only in children under 3 years of age.
Neonate Through 5 Years of Age
See Use in Specific Populations (8.4).
Children and Adolescents 6 Through 16 Years of Age
The pharmacokinetics of pantoprazole delayed-release tablets were evaluated in children ages 6 through 16 years with a clinical diagnosis of GERD. The PK parameters following a single oral dose of 20 mg or 40 mg of pantoprazole tablets in children ages 6 through 16 years were highly variable (%CV ranges 40 to 80%). The geometric mean AUC estimated from population PK analysis after a 40 mg pantoprazole tablet in pediatric patients was about 39% and 10% higher respectively in 6 to 11 and 12 to 16 year-old children, compared to that of adults (Table 6).
Table 6: PK Parameters in Children and Adolescents 6 Through 16 Years With GERD Receiving 40 mg Pantoprazole Tablets * Geometric mean values †Median values 6 to 11 Years (n = 12)
12 to 16 Years (n = 11)
Cmax (mcg/mL)*
1.8
1.8
tmax (h)â€
2.0
2.0
AUC (mcg•h/mL)*
6.9
5.5
CL/F (L/h)â€
6.6
6.8
Gender
There is a modest increase in pantoprazole AUC and Cmax in women compared to men. However, weight-normalized clearance values are similar in women and men. No dosage adjustment is recommended based on gender. In pediatric patients ages 1 through 16 years there were no clinically relevant effects of gender on clearance of pantoprazole, as shown by population pharmacokinetic analysis.
Renal Impairment
In patients with severe renal impairment, pharmacokinetic parameters for pantoprazole were similar to those of healthy subjects. No dosage adjustment is necessary in patients with renal impairment or in patients undergoing hemodialysis.
Hepatic Impairment
In patients with mild to severe hepatic impairment (Child-Pugh A to C cirrhosis), maximum pantoprazole concentrations increased only slightly (1.5 fold) relative to healthy subjects. Although serum half-life values increased to 7 to 9 hours and AUC values increased by 5 to 7 fold in hepatic-impaired patients, these increases were no greater than those observed in CYP2C19 poor metabolizers, where no dosage adjustment is warranted. These pharmacokinetic changes in hepatic-impaired patients result in minimal drug accumulation following once-daily, multiple-dose administration. No dosage adjustment is needed in patients with mild to severe hepatic impairment. Doses higher than 40 mg/day have not been studied in hepatically impaired patients.
Drug-Drug Interactions
Pantoprazole is metabolized mainly by CYP2C19 and to minor extents by CYPs 3A4, 2D6, and 2C9. In in vivo drug-drug interaction studies with CYP2C19 substrates (diazepam [also a CYP3A4 substrate] and phenytoin [also a CYP3A4 inducer] and clopidogrel), nifedipine, midazolam, and clarithromycin (CYP3A4 substrates), metoprolol (a CYP2D6 substrate), diclofenac, naproxen and piroxicam (CYP2C9 substrates), and theophylline (a CYP1A2 substrate) in healthy subjects, the pharmacokinetics of pantoprazole were not significantly altered.
Clopidogrel: Clopidogrel is metabolized to its active metabolite in part by CYP2C19. In a crossover clinical study, 66 healthy subjects were administered clopidogrel (300 mg loading dose followed by 75 mg per day) alone and with pantoprazole (80 mg at the same time as clopidogrel) for 5 days. On Day 5, the mean AUC of the active metabolite of clopidogrel was reduced by approximately 14% (geometric mean ratio was 86%, with 90% CI of 79 to 93%) when pantoprazole was coadministered with clopidogrel as compared to clopidogrel administered alone. Pharmacodynamic parameters were also measured and demonstrated that the change in inhibition of platelet aggregation (induced by 5 ÎĽM ADP) was correlated with the change in the exposure to clopidogrel active metabolite. The clinical significance of this finding is not clear.
Mycophenolate Mofetil (MMF): Administration of pantoprazole 40 mg twice daily for 4 days and a single 1000 mg dose of MMF approximately one hour after the last dose of pantoprazole to 12 healthy subjects in a cross-over study resulted in a 57% reduction in the Cmax and 27% reduction in the AUC of MPA. Transplant patients receiving approximately 2000 mg per day of MMF (n = 12) were compared to transplant patients receiving approximately the same dose of MMF and pantoprazole 40 mg per day (n = 21). There was a 78% reduction in the Cmax and a 45% reduction in the AUC of MPA in patients receiving both pantoprazole and MMF.
In vivo studies also suggest that pantoprazole does not significantly affect the kinetics of the following drugs (cisapride, theophylline, diazepam [and its active metabolite, desmethyldiazepam], phenytoin, warfarin, metoprolol, nifedipine, carbamazepine, midazolam, clarithromycin, naproxen, piroxicam, and oral contraceptives [levonorgestrel/ethinyl estradiol]). Dosage adjustment of these drugs is not necessary when they are coadministered with pantoprazole. In other in vivo studies, digoxin, ethanol, glyburide, antipyrine, caffeine, metronidazole, and amoxicillin had no clinically relevant interactions with pantoprazole.
Based on studies evaluating possible interactions of pantoprazole with other drugs, no dosage adjustment is needed with concomitant use of the following: theophylline, cisapride, antipyrine, caffeine, carbamazepine, diazepam (and its active metabolite, desmethyldiazepam), diclofenac, naproxen, piroxicam, digoxin, ethanol, glyburide, an oral contraceptive (levonorgestrel/ethinyl estradiol), metoprolol, nifedipine, phenytoin, warfarin, midazolam, clarithromycin, metronidazole, or amoxicillin.
There was also no interaction with concomitantly administered antacids.
There have been postmarketing reports of increased INR and prothrombin time in patients receiving proton pump inhibitors, including pantoprazole, and warfarin concomitantly [see Drug Interactions (7.2)].
Although no significant drug-drug interactions have been observed in clinical studies, the potential for significant drug-drug interactions with more than once-daily dosing with high doses of pantoprazole has not been studied in poor metabolizers or individuals who are hepatically impaired.
Other Effects
In a clinical pharmacology study, pantoprazole 40 mg given once daily for 2 weeks had no effect on the levels of the following hormones: cortisol, testosterone, triiodothyronine (T3), thyroxine (T4), thyroid-stimulating hormone (TSH), thyronine-binding protein, parathyroid hormone, insulin, glucagon, renin, aldosterone, follicle-stimulating hormone, luteinizing hormone, prolactin, and growth hormone.
In a 1 year study of GERD patients treated with pantoprazole 40 mg or 20 mg, there were no changes from baseline in overall levels of T3, T4, and TSH.
12.4 Pharmacogenomics CYP2C19 displays a known genetic polymorphism due to its deficiency in some subpopulations (e.g., approximately 3% of Caucasians and African-Americans and 17% to 23% of Asians are poor metabolizers). Although these subpopulations of pantoprazole poor metabolizers have elimination half-life values of 3.5 to 10.0 hours in adults, they still have minimal accumulation (≤ 23%) with once-daily dosing. For adult patients who are CYP2C19 poor metabolizers, no dosage adjustment is needed.
Similar to adults, pediatric patients who have the poor metabolizer genotype of CYP2C19 (CYP2C19 *2/*2) exhibited greater than a 6 fold increase in AUC compared to pediatric extensive (CYP2C19 *1/*1) and intermediate (CYP2C19 *1/*x) metabolizers. Poor metabolizers exhibited approximately 10 fold lower apparent oral clearance compared to extensive metabolizers.
For known pediatric poor metabolizers, a dose reduction should be considered.
Package Label.principal Display Panel
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site