NINLARO (ixazomib citrate 4 mg) Dailymed
Generic: ixazomib is used for the treatment of Multiple Myeloma
Go PRO for all pill images
Recent Major Changes Section
Warnings and Precautions, Cutaneous Reactions ( 5.5 )3/2024
1 Indications And Usage
NINLARO is indicated in combination with lenalidomide and dexamethasone for the treatment of patients with multiple myeloma who have received at least one prior therapy.
NINLARO is a proteasome inhibitor indicated in combination with lenalidomide and dexamethasone for the treatment of patients with multiple myeloma who have received at least one prior therapy. (1 )
Limitations of Use: NINLARO is not recommended for use in the maintenance setting or in newly diagnosed multiple myeloma in combination with lenalidomide and dexamethasone outside of controlled clinical trials. (1 )
Limitations of Use: NINLARO is not recommended for use in the maintenance setting or in newly diagnosed multiple myeloma in combination with lenalidomide and dexamethasone outside of controlled clinical trials [see Warnings and Precautions (5.9) and Clinical Studies (14.2, 14.3)].
2 Dosage And Administration
- Recommended starting dose of 4 mg taken orally on Days 1, 8, and 15 of a 28-day cycle. (
2.1 )- Dose should be taken at least one hour before or at least two hours after food. (
2.1 )2.1 Dosing and Administration Guidelines
NINLARO in combination with lenalidomide and dexamethasone
The recommended starting dose of NINLARO is 4 mg administered orally once a week on Days 1, 8, and 15 of a 28-day treatment cycle.
The recommended starting dose of lenalidomide is 25 mg administered daily on Days 1 through 21 of a 28-day treatment cycle.
The recommended starting dose of dexamethasone is 40 mg administered on Days 1, 8, 15, and 22 of a 28-day treatment cycle.
Table 1: Dosing Schedule for NINLARO taken with Lenalidomide and Dexamethasone ‚úĒ Take medicine 28-Day Cycle (a 4-week cycle) Week 1 Week 2 Week 3 Week 4 Day 1 Days 2-7 Day 8 Days 9-14 Day 15 Days 16-21 Day 22 Days 23-28 NINLARO ‚úĒ ‚úĒ ‚úĒ Lenalidomide ‚úĒ ‚úĒ Daily ‚úĒ ‚úĒ Daily ‚úĒ ‚úĒ Daily Dexamethasone ‚úĒ ‚úĒ ‚úĒ ‚úĒ
For additional information regarding lenalidomide and dexamethasone, refer to their prescribing information.
NINLARO should be taken once a week on the same day and at approximately the same time for the first three weeks of a four week cycle. The importance of carefully following all dosage instructions should be discussed with patients starting treatment. Instruct patients to take the recommended dosage as directed, because overdosage has led to deaths [see Overdosage (10)].
NINLARO should be taken at least one hour before or at least two hours after food [see Clinical Pharmacology (12.3)]. The whole capsule should be swallowed with water. The capsule should not be crushed, chewed or opened [see How Supplied/Storage and Handling (16)].
If a NINLARO dose is delayed or missed, the dose should be taken only if the next scheduled dose is ‚Č•72 hours away. A missed dose should not be taken within 72 hours of the next scheduled dose. A double dose should not be taken to make up for the missed dose.
If vomiting occurs after taking a dose, the patient should not repeat the dose. The patient should resume dosing at the time of the next scheduled dose.
Prior to initiating a new cycle of therapy:
- Absolute neutrophil count should be at least 1,000/mm3
- Platelet count should be at least 75,000/mm3
- Non-hematologic toxicities should, at the healthcare provider's discretion, generally be recovered to patient's baseline condition or Grade 1 or lower
Treatment should be continued until disease progression or unacceptable toxicity.
Concomitant Medications
Consider antiviral prophylaxis in patients being treated with NINLARO to decrease the risk of herpes zoster reactivation [see Adverse Reactions (6.1)].
2.2 Dosage Modification Guidelines
The NINLARO dose reduction steps are presented in Table 2 and the dosage modification guidelines are provided in Table 3.
Table 2: NINLARO Dose Reductions due to Adverse Reactions Recommended starting dose Recommended starting dose of 3 mg in patients with moderate or severe hepatic impairment, severe renal impairment or end-stage renal disease requiring dialysis [see Dosage and Administration (2.3, 2.4)]. First reduction to Second reduction to Discontinue   4 mg   3 mg   2.3 mg
An alternating dose modification approach is recommended for NINLARO and lenalidomide for thrombocytopenia, neutropenia, and rash as described in Table 3. Refer to the lenalidomide prescribing information if dose reduction is needed for lenalidomide.
Table 3: Dosage Modifications Guidelines for NINLARO in Combination with Lenalidomide and Dexamethasone Hematological Toxicities Recommended Actions Thrombocytopenia (Platelet Count) Platelet count less than 30,000/mm3
- Withhold NINLARO and lenalidomide until platelet count is at least 30,000/mm3.
- Following recovery, resume lenalidomide at the next lower dose according to its prescribing information and resume NINLARO at its most recent dose.
- If platelet count falls to less than 30,000/mm3 again, withhold NINLARO and lenalidomide until platelet count is at least 30,000/mm3.
- Following recovery, resume NINLARO at the next lower dose and resume lenalidomide at its most recent dose.
For additional occurrences, alternate dose modification of lenalidomide and NINLARO Neutropenia (Absolute Neutrophil Count) Absolute neutrophil count less than 500/mm3
- Withhold NINLARO and lenalidomide until absolute neutrophil count is at least 500/mm3. Consider adding G-CSF as per clinical guidelines.
- Following recovery, resume lenalidomide at the next lower dose according to its prescribing information and resume NINLARO at its most recent dose.
- If absolute neutrophil count falls to less than 500/mm3 again, withhold NINLARO and lenalidomide until absolute neutrophil count is at least 500/mm3.
- Following recovery, resume NINLARO at the next lower dose and resume lenalidomide at its most recent dose.
Non-Hematological Toxicities Recommended Actions Rash Grade Grading based on National Cancer Institute Common Terminology Criteria (CTCAE) Version 4.03 2 or 3
- Withhold lenalidomide until rash recovers to Grade 1 or lower.
- Following recovery, resume lenalidomide at the next lower dose according to its prescribing information.
- If Grade 2 or 3 rash occurs again, withhold NINLARO and lenalidomide until rash recovers to Grade 1 or lower.
- Following recovery, resume NINLARO at the next lower dose and resume lenalidomide at its most recent dose.
Grade 4 Discontinue treatment regimen. Peripheral Neuropathy Grade 1 Peripheral Neuropathy with Pain or Grade 2 Peripheral Neuropathy
- Withhold NINLARO until peripheral neuropathy recovers to Grade 1 or lower without pain or patient's baseline.
- Following recovery, resume NINLARO at its most recent dose.
Grade 2 Peripheral Neuropathy with Pain or Grade 3 Peripheral Neuropathy
- Withhold NINLARO. Toxicities should, at the healthcare provider's discretion, generally recover to patient's baseline condition or Grade 1 or lower prior to resuming NINLARO.
- Following recovery, resume NINLARO at the next lower dose.
Grade 4 Peripheral Neuropathy Discontinue treatment regimen. Other Non-Hematological Toxicities Other Grade 3 or 4 Non-Hematological Toxicities
- Withhold NINLARO. Toxicities should, at the healthcare provider's discretion, generally recover to patient's baseline condition or Grade 1 or lower prior to resuming NINLARO.
- If attributable to NINLARO, resume NINLARO at the next lower dose following recovery.
2.3 Dosage in Patients with Hepatic Impairment
Reduce the starting dose of NINLARO to 3 mg in patients with moderate (total bilirubin greater than 1.5-3 √ó ULN) or severe (total bilirubin greater than 3 √ó ULN) hepatic impairment [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.4 Dosage in Patients with Renal Impairment
Reduce the starting dose of NINLARO to 3 mg in patients with severe renal impairment (creatinine clearance less than 30 mL/min) or end-stage renal disease (ESRD) requiring dialysis. NINLARO is not dialyzable and therefore can be administered without regard to the timing of dialysis [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
Refer to the lenalidomide prescribing information for dosing recommendations in patients with renal impairment.
3 Dosage Forms And Strengths
NINLARO is available in the following capsules:
- 4 mg ixazomib: Light orange gelatin capsule imprinted with "Takeda" on the cap and "4 mg" on the body in black ink.
- 3 mg ixazomib: Light grey gelatin capsule imprinted with "Takeda" on the cap and "3 mg" on the body in black ink.
- 2.3 mg ixazomib: Light pink gelatin capsule imprinted with "Takeda" on the cap and "2.3 mg" on the body in black ink.
Capsules: 4 mg, 3 mg, and 2.3 mg (3 )
4 Contraindications
None.
None. (4 )
5 Warnings And Precautions
- Thrombocytopenia: Monitor platelet counts at least monthly during treatment and adjust dosing, as needed. (
2.2 ,5.1 )- Gastrointestinal Toxicities: Adjust dosing for severe diarrhea, constipation, nausea, and vomiting, as needed. (
2.2 ,5.2 )- Peripheral Neuropathy: Monitor patients for symptoms of peripheral neuropathy and adjust dosing, as needed. (
2.2 ,5.3 )- Peripheral Edema: Monitor for fluid retention. Investigate for underlying causes, when appropriate. Adjust dosing, as needed. (
2.2 ,5.4 )- Cutaneous Reactions: Monitor patients for rash and adjust dosing, as needed. (
2.2 ,5.5 )- Thrombotic Microangiopathy: Monitor for signs and symptoms. Discontinue NINLARO if suspected. (
5.6 )- Hepatotoxicity: Monitor hepatic enzymes during treatment. (
5.7 )- Embryo-Fetal Toxicity: NINLARO can cause fetal harm. Advise patients of the potential risk to a fetus and to use effective non-hormonal contraception. (
5.8 ,8.1 ,8.3 )- Increased Mortality in Patients Treated with NINLARO in the Maintenance Setting: Treatment of patients with NINLARO for multiple myeloma in the maintenance setting is not recommended outside of controlled trials. (
5.9 )5.1 Thrombocytopenia
Thrombocytopenia has been reported with NINLARO with platelet nadirs typically occurring between Days 14-21 of each 28-day cycle and recovery to baseline by the start of the next cycle [see Adverse Reactions (6.1)]. Grade 3 thrombocytopenia was reported in 17% of patients in the NINLARO regimen and Grade 4 thrombocytopenia was reported in 13% in the NINLARO regimen. The rate of platelet transfusions was 10% in the NINLARO regimen and 7% in the placebo regimen.
Monitor platelet counts at least monthly during treatment with NINLARO. Consider more frequent monitoring during the first three cycles. Manage thrombocytopenia with dose modifications [see Dosage and Administration (2.2)] and platelet transfusions as per standard medical guidelines.
5.2 Gastrointestinal Toxicities
Diarrhea, constipation, nausea, and vomiting have been reported with NINLARO, occasionally requiring use of antidiarrheal and antiemetic medications, and supportive care. Diarrhea was reported in 52% of patients in the NINLARO regimen and 43% in the placebo regimen, constipation in 35% and 28%, respectively, nausea in 32% and 23%, respectively, and vomiting in 26% and 13%, respectively. Diarrhea resulted in discontinuation of one or more of the three drugs in 3% of patients in the NINLARO regimen and 2% of patients in the placebo regimen [see Adverse Reactions (6.1)]. Adjust dosing for Grade 3 or 4 symptoms [see Dosage and Administration (2.2)].
5.3 Peripheral Neuropathy
The majority of peripheral neuropathy adverse reactions were Grade 1 (18% in the NINLARO regimen and 16% in the placebo regimen) and Grade 2 (11% in the NINLARO regimen and 6% in the placebo regimen) [see Adverse Reactions (6.1)]. Grade 3 adverse reactions of peripheral neuropathy were reported at 2% in both regimens.
The most commonly reported reaction was peripheral sensory neuropathy (24% and 17% in the NINLARO and placebo regimen, respectively). Peripheral motor neuropathy was not commonly reported in either regimen (<1%). Peripheral neuropathy resulted in discontinuation of one or more of the three drugs in 4% of patients in the NINLARO regimen and <1% of patients in the placebo regimen. Patients should be monitored for symptoms of neuropathy. Patients experiencing new or worsening peripheral neuropathy may require dose modification [see Dosage and Administration (2.2)].
5.4 Peripheral Edema
Peripheral edema was reported in 27% and 21% of patients in the NINLARO and placebo regimens, respectively. The majority of peripheral edema adverse reactions were Grade 1 (17% in the NINLARO regimen and 14% in the placebo regimen) and Grade 2 (7% in the NINLARO regimen and 6% in the placebo regimen).
Grade 3 peripheral edema was reported in 2% and 1% of patients in the NINLARO and placebo regimens, respectively [see Adverse Reactions (6.1)]. Peripheral edema resulted in discontinuation of one or more of the three drugs in <1% of patients in both regimens. Evaluate for underlying causes and provide supportive care, as necessary. Adjust dosing of dexamethasone per its prescribing information or NINLARO for Grade 3 or 4 symptoms [see Dosage and Administration (2.2)].
5.5 Cutaneous Reactions
Rash was reported in 27% of patients in the NINLARO regimen and 16% of patients in the placebo regimen. The majority of the rash adverse reactions were Grade 1 (15% in the NINLARO regimen and 9% in the placebo regimen) or Grade 2 (9% in the NINLARO regimen and 4% in the placebo regimen) [see Adverse Reactions (6.1)]. Grade 3 rash was reported in 3% of patients in the NINLARO regimen and 2% of patients in the placebo regimen. Serious adverse reactions of rash were reported in <1% of patients in the NINLARO regimen. The most common type of rash reported in both regimens included maculo-papular and macular rash. Rash resulted in discontinuation of one or more of the three drugs in <1% of patients in both regimens. Manage rash with supportive care or with dose modification if Grade 2 or higher [see Dosage and Administration (2.2)].
Stevens-Johnson syndrome and toxic epidermal necrolysis, including fatal cases, have been reported with NINLARO [see Adverse Reactions (6.1, 6.2)]. If Stevens-Johnson syndrome or toxic epidermal necrolysis occurs, discontinue NINLARO and manage as clinically indicated.
5.6Thrombotic Microangiopathy
Cases, sometimes fatal, of thrombotic microangiopathy, including thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (TTP/HUS), have been reported in patients who received NINLARO [see Adverse Reactions (6.1)]. Monitor for signs and symptoms of TTP/HUS. If the diagnosis is suspected, stop NINLARO and evaluate. If the diagnosis of TTP/HUS is excluded, consider restarting NINLARO. The safety of reinitiating NINLARO therapy in patients previously experiencing TTP/HUS is not known.
5.7 Hepatotoxicity
Drug-induced liver injury, hepatocellular injury, hepatic steatosis, hepatitis cholestatic and hepatotoxicity have each been reported in <1% of patients treated with NINLARO [see Adverse Reactions (6.1)]. Hepatotoxicity has been reported (10% in the NINLARO regimen and 9% in the placebo regimen). Monitor hepatic enzymes regularly and adjust dosing for Grade 3 or 4 symptoms [see Dosage and Administration (2.2)].
5.8 Embryo-Fetal Toxicity
NINLARO can cause fetal harm when administered to a pregnant woman based on the mechanism of action and findings in animal studies. Ixazomib caused embryo-fetal toxicity in pregnant rats and rabbits at doses resulting in exposures that were slightly higher than those observed in patients receiving the recommended dose. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective non-hormonal contraception during treatment with NINLARO and for 90 days following the last dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with NINLARO and for 90 days following the last dose [see Drug Interactions (7.1) and Use in Specific Populations (8.1, 8.3)].
5.9Increased Mortality in Patients Treated with NINLARO in the Maintenance Setting
In two prospective randomized clinical trials in multiple myeloma in the maintenance setting, treatment with NINLARO resulted in increased deaths. Treatment of patients with NINLARO for multiple myeloma in the maintenance setting is not recommended outside of controlled trials [see Clinical Studies (14.2)].
6 Adverse Reactions
The following adverse reactions are described in detail in other sections of the prescribing information:
- Thrombocytopenia [see Warnings and Precautions (5.1)]
- Gastrointestinal Toxicities [see Warnings and Precautions (5.2)]
- Peripheral Neuropathy [see Warnings and Precautions (5.3)]
- Peripheral Edema [see Warnings and Precautions (5.4)]
- Cutaneous Reactions [see Warnings and Precautions (5.5)]
- Thrombotic Microangiopathy [see Warnings and Precautions (5.6)]
- Hepatotoxicity [see Warnings and Precautions (5.7)]
The most common adverse reactions (‚Č•20%) are thrombocytopenia, neutropenia, diarrhea, constipation, peripheral neuropathy, nausea, peripheral edema, rash, vomiting, and bronchitis. (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals at 1-844-617-6468 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety population from the randomized, double-blind, placebo-controlled clinical study included 720 patients with relapsed and/or refractory multiple myeloma, who received NINLARO in combination with lenalidomide and dexamethasone (NINLARO regimen; N=361) or placebo in combination with lenalidomide and dexamethasone (placebo regimen; N=359).
The most frequently reported adverse reactions (‚Č•20% with a difference of ‚Č•5% compared to placebo) in the NINLARO regimen were thrombocytopenia, neutropenia, diarrhea, constipation, peripheral neuropathy, nausea, peripheral edema, rash, vomiting, and bronchitis. Serious adverse reactions reported in ‚Č•2% of patients in the NINLARO regimen included diarrhea (3%), thrombocytopenia (2%) and bronchitis (2%). One or more of the three drugs was permanently discontinued in 4% of patients reporting peripheral neuropathy, 3% of patients reporting diarrhea and 2% of patients reporting thrombocytopenia. Permanent discontinuation of NINLARO due to an adverse reaction occurred in 10% of patients.
Table 4 summarizes the non-hematologic adverse reactions occurring in at least 5% of patients with at least a 5% difference between the NINLARO regimen and the placebo regimen.
Table 4: Non-Hematologic Adverse Reactions Occurring in ‚Č•5% of Patients with a ‚Č•5% Difference Between the NINLARO Regimen and the Placebo Regimen (All Grades, Grade 3 and Grade 4) System Organ Class /Preferred Term NINLARO + Lenalidomide and DexamethasoneN=361 Placebo + Lenalidomide and DexamethasoneN=359 % % All Grades Grade 3 Grade 4 All Grades Grade 3 Grade 4 Note: Adverse reactions included as preferred terms are based on MedDRA version 23.0. Gastrointestinal disorders ¬†¬†Diarrhea 52 10 0 43 3 0 ¬†¬†Constipation 35 <1 0 28 <1 0 ¬†¬†Nausea 32 2 0 23 0 0 ¬†¬†Vomiting 26 1 0 13 <1 0 Nervous system disorders ¬†¬†Peripheral neuropathies Represents a pooling of preferred terms 32 2 0 24 2 0 Musculoskeletal and connective tissue disorders ¬†¬†Back pain At the time of the final analysis, these adverse reactions no longer met the criterion for a ‚Č•5% difference between the NINLARO regimen and the placebo regimen. 27 <1 0 24 3 0 Infections and infestations ¬†¬†Upper respiratory tract infection 27 1 0 23 1 0 ¬†¬†Bronchitis 22 2 0 17 2 <1 Skin and subcutaneous tissue disorders ¬†¬†Rash 27 3 0 16 2 0 General disorders and administration site conditions ¬†¬†Edema peripheral 27 2 0 21 1 0
Table 5 represents pooled information from adverse event and laboratory data.
Table 5: Thrombocytopenia and Neutropenia NINLARO + Lenalidomide and DexamethasoneN=361 Placebo + Lenalidomide and DexamethasoneN=359 % % Any Grade Grade 3-4 Any Grade Grade 3-4 Thrombocytopenia 85 30 67 14 Neutropenia 74 34 70 37
Herpes Zoster
Herpes zoster was reported in 6% of patients in the NINLARO regimen and 3% of patients in the placebo regimen. Antiviral prophylaxis was allowed at the healthcare provider's discretion. Patients treated in the NINLARO regimen who received antiviral prophylaxis had a lower incidence (1%) of herpes zoster infection compared to patients who did not receive prophylaxis (10%).
Eye Disorders
Eye disorders were reported with many different preferred terms but in aggregate, the frequency was 38% in patients in the NINLARO regimen. The most common adverse reactions of the eyes were cataract (15%), conjunctivitis (9%), blurred vision (7%), and dry eye (6%).
Other Clinical Trials Experience
The following serious adverse reactions have each been reported at a frequency of <1% in patients treated with NINLARO: acute febrile neutrophilic dermatosis (Sweet's syndrome), Stevens-Johnson syndrome, transverse myelitis, posterior reversible encephalopathy syndrome, tumor lysis syndrome, and thrombotic thrombocytopenic purpura.
6.2Postmarketing Experience
The following adverse reactions have been identified during post-approval use of NINLARO. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune system disorders: Angioedema
Skin and subcutaneous tissue disorders: Toxic epidermal necrolysis
7 Drug Interactions
Strong CYP3A inducers: Avoid concomitant use with NINLARO. (7.1 ,12.3 )
7.1 Strong CYP3A Inducers
Avoid concomitant administration of NINLARO with strong CYP3A inducers (such as rifampin, phenytoin, carbamazepine, and St. John's Wort) [see Clinical Pharmacology (12.3)].
8 Use In Specific Populations
- Hepatic Impairment: Reduce the NINLARO starting dose to 3 mg in patients with moderate or severe hepatic impairment. (
2.3 ,8.6 )- Renal Impairment: Reduce the NINLARO starting dose to 3 mg in patients with severe renal impairment or end-stage renal disease requiring dialysis. (
2.4 ,8.7 )- Lactation: Advise not to breastfeed. (
8.2 )8.1 Pregnancy
Risk Summary
Based on its mechanism of action [see Clinical Pharmacology (12.1)] and data from animal reproduction studies, NINLARO can cause fetal harm when administered to a pregnant woman. There are no available data on NINLARO use in pregnant women to evaluate drug-associated risk. Ixazomib caused embryo-fetal toxicity in pregnant rats and rabbits at doses resulting in exposures that were slightly higher than those observed in patients receiving the recommended dose (see Data). Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Data
Animal Data
In an embryo-fetal development study in pregnant rabbits there were increases in fetal skeletal variations/abnormalities (fused caudal vertebrae, number of lumbar vertebrae, and full supernumerary ribs) at doses that were also maternally toxic (‚Č•0.3 mg/kg). Exposures in the rabbit at 0.3 mg/kg were 1.9 times the clinical time averaged exposures at the recommended dose of 4 mg. In a rat dose range-finding embryo-fetal development study, at doses that were maternally toxic, there were decreases in fetal weights, a trend towards decreased fetal viability, and increased post-implantation losses at 0.6 mg/kg. Exposures in rats at the dose of 0.6 mg/kg was 2.5 times the clinical time averaged exposures at the recommended dose of 4 mg.
8.2 Lactation
Risk Summary
There are no data on the presence of ixazomib or its metabolites in human milk, the effects of the drug on the breast fed infant, or the effects of the drug on milk production. Because of the potential for serious adverse reactions from NINLARO in a breastfed infant, advise women not to breastfeed during treatment with NINLARO and for 90 days after the last dose.
8.3 Females and Males of Reproductive Potential
NINLARO can cause fetal harm when administered to pregnant women [see Use in Specific Populations (8.1)].
Pregnancy Testing
Verify pregnancy status in females of reproductive potential prior to initiating NINLARO.
Contraception
Females
Advise females of reproductive potential to use effective non-hormonal contraception during treatment with NINLARO and for 90 days after the last dose. Dexamethasone is known to be a weak to moderate inducer of CYP3A4 as well as other enzymes and transporters. Because NINLARO is administered with dexamethasone, the risk for reduced efficacy of contraceptives needs to be considered [see Drug Interactions (7.1)].
Males
Advise males with female partners of reproductive potential to use effective contraception during treatment with NINLARO and for 90 days after the last dose.
8.4 Pediatric Use
Safety and effectiveness of NINLARO have not been established in pediatric patients.
8.5 Geriatric Use
Of the total number of subjects in clinical studies of NINLARO, 55% were 65 and over, while 17% were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
In patients with moderate or severe hepatic impairment, the mean AUC increased by 20% when compared to patients with normal hepatic function. Reduce the starting dose of NINLARO in patients with moderate or severe hepatic impairment [see Dosage and Administration (2.3), Clinical Pharmacology (12.3)].
8.7 Renal Impairment
In patients with severe renal impairment or ESRD requiring dialysis, the mean AUC increased by 39% when compared to patients with normal renal function. Reduce the starting dose of NINLARO in patients with severe renal impairment or ESRD requiring dialysis. NINLARO is not dialyzable and therefore can be administered without regard to the timing of dialysis [see Dosage and Administration (2.4), Clinical Pharmacology (12.3)].
10 Overdosage
Overdosage, including fatal overdosage, has been reported in patients taking NINLARO. Manifestations of overdosage include adverse reactions reported at the recommended dosage [see Dosage and Administration (2.1), Adverse Reactions (6.1)]. Serious adverse reactions reported with overdosage include severe nausea, vomiting, diarrhea, aspiration pneumonia, multiple organ failure and death.
In the event of an overdosage, monitor for adverse reactions and provide appropriate supportive care. NINLARO is not dialyzable.
11 Description
Ixazomib is a proteasome inhibitor. Ixazomib citrate, a prodrug, rapidly hydrolyzes under physiological conditions to its biologically active form, ixazomib. The chemical name of ixazomib citrate is 1,3,2-dioxaborolane-4,4-diacetic acid, 2-[(1R)-1-[[2-[(2,5-dichlorobenzoyl)amino]acetyl]amino]-3-methylbutyl]-5-oxo- and the structural formula is:
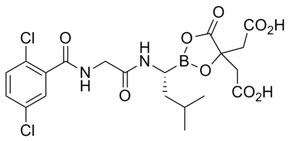
The molecular formula for ixazomib citrate is C20H23BCl2N2O9 and its molecular weight is 517.12. Ixazomib citrate has one chiral center and is the R-stereoisomer. The solubility of ixazomib citrate in 0.1N HCl (pH 1.2) at 37¬įC is 0.61 mg/mL (reported as ixazomib). The solubility increases as the pH increases.
NINLARO (ixazomib) capsules for oral use contain 4, 3 or 2.3 mg of ixazomib equivalent to 5.7, 4.3 or 3.3 mg of ixazomib citrate, respectively. Inactive ingredients include microcrystalline cellulose, magnesium stearate, and talc. Capsule shells contain gelatin and titanium dioxide. The 4 mg capsule shell contains red and yellow iron oxide, the 3 mg capsule shell contains black iron oxide and the 2.3 mg capsule shell contains red iron oxide. The printing ink contains shellac, propylene glycol, potassium hydroxide, and black iron oxide.
12 Clinical Pharmacology
12.1 Mechanism of Action
Ixazomib is a reversible proteasome inhibitor. Ixazomib preferentially binds and inhibits the chymotrypsin-like activity of the beta 5 subunit of the 20S proteasome.
Ixazomib induced apoptosis of multiple myeloma cell lines in vitro. Ixazomib demonstrated in vitro cytotoxicity against myeloma cells from patients who had relapsed after multiple prior therapies, including bortezomib, lenalidomide, and dexamethasone. The combination of ixazomib and lenalidomide demonstrated synergistic cytotoxic effects in multiple myeloma cell lines. In vivo, ixazomib demonstrated antitumor activity in a mouse multiple myeloma tumor xenograft model.
12.2 Pharmacodynamics
Cardiac Electrophysiology
NINLARO did not prolong the QTc interval at clinically relevant exposures based on pharmacokinetic-pharmacodynamic analysis of data from 245 patients.
12.3 Pharmacokinetics
Absorption
After oral administration, the median time to achieve peak ixazomib plasma concentrations was one hour. The mean absolute oral bioavailability was 58%, based on population PK analysis. Ixazomib AUC increases in a dose proportional manner over a dose range of 0.2 to 10.6 mg.
A food effect study conducted in patients with a single 4 mg dose of ixazomib showed that a high-fat meal decreased ixazomib AUC by 28% and Cmax by 69% [see Dosage and Administration (2.1)].
Distribution
Ixazomib is 99% bound to plasma proteins and distributes into red blood cells with a blood-to-plasma ratio of 10. The steady-state volume of distribution is 543 L.
Elimination
Based on a population PK analysis, systemic clearance was approximately 1.9 L/hr with inter-individual variability of 44%. The terminal half-life (t1/2) of ixazomib was 9.5 days. Following weekly oral dosing, the accumulation ratio was determined to be 2-fold.
Metabolism
After oral administration of a radiolabeled dose, ixazomib represented 70% of total drug-related material in plasma. Metabolism by multiple CYP enzymes and non-CYP proteins is expected to be the major clearance mechanism for ixazomib. At clinically relevant ixazomib concentrations, in vitro studies using human cDNA-expressed cytochrome P450 isozymes showed that no specific CYP isozyme predominantly contributes to ixazomib metabolism. At higher than clinical concentrations, ixazomib was metabolized by multiple CYP isoforms with estimated relative contributions of 3A4 (42%), 1A2 (26%), 2B6 (16%), 2C8 (6%), 2D6 (5%), 2C19 (5%) and 2C9 (<1%).
Excretion
After administration of a single oral dose of 14C-ixazomib to 5 patients with advanced cancer, 62% of the administered radioactivity was excreted in urine and 22% in the feces. Unchanged ixazomib accounted for <3.5% of the administered dose recovered in urine.
Specific Populations
There was no clinically meaningful effect of age (range 23-91 years), sex, body surface area (range 1.2-2.7 m2), or race on the clearance of ixazomib based on population PK analysis.
Patients with Hepatic Impairment
The PK of ixazomib was similar in patients with normal hepatic function and in patients with mild hepatic impairment (total bilirubin ‚ȧ ULN and AST >ULN or total bilirubin >1-1.5 √ó ULN and any AST) based on population PK analysis.
The PK of ixazomib was characterized in patients with normal hepatic function at 4 mg (N=12), moderate hepatic impairment at 2.3 mg (total bilirubin >1.5-3 √ó ULN, N=13) or severe hepatic impairment at 1.5 mg (total bilirubin >3 √ó ULN, N=18). Dose-normalized mean AUC was 20% higher in patients with moderate or severe hepatic impairment as compared to patients with normal hepatic function [see Dosage and Administration (2.3)].
Patients with Renal Impairment
The PK of ixazomib was similar in patients with normal renal function and in patients with mild or moderate renal impairment (creatinine clearance ‚Č•30 mL/min) based on population PK analysis.
The PK of ixazomib was characterized at a dose of 3 mg in patients with normal renal function (creatinine clearance ‚Č•90 mL/min, N=18), severe renal impairment (creatinine clearance <30 mL/min, N=14), or ESRD requiring dialysis (N=6). Mean AUC was 39% higher in patients with severe renal impairment or ESRD requiring dialysis as compared to patients with normal renal function. Pre- and post-dialyzer concentrations of ixazomib measured during the hemodialysis session were similar, suggesting that ixazomib is not dialyzable [see Dosage and Administration (2.4)].
Drug Interaction Studies
Effect of Other Drugs on NINLARO
Effect of NINLARO on Other Drugs
Ixazomib is neither a reversible nor a time-dependent inhibitor of CYPs 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4/5. Ixazomib did not induce CYP1A2, CYP2B6, and CYP3A4/5 activity or corresponding immunoreactive protein levels. NINLARO is not expected to produce drug-drug interactions via CYP inhibition or induction.
Transporter-Based Interactions
Ixazomib is a low affinity substrate of P-gp. Ixazomib is not a substrate of BCRP, MRP2 or hepatic OATPs. Ixazomib is not an inhibitor of P-gp, BCRP, MRP2, OATP1B1, OATP1B3, OCT2, OAT1, OAT3, MATE1, or MATE2-K. NINLARO is not expected to cause transporter-mediated drug-drug interactions.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Ixazomib was not mutagenic in a bacterial reverse mutation assay (Ames assay). Ixazomib was considered positive in an in vitro clastogenicity test in human peripheral blood lymphocytes. However, in vivo, ixazomib was not clastogenic in a bone marrow micronucleus assay in mice and was negative in an in vivo comet assay in mice, as assessed in the stomach and liver. No carcinogenicity studies have been performed with ixazomib.
Developmental toxicity studies in rats and rabbits did not show direct embryo-fetal toxicity below maternally toxic doses of ixazomib. Studies of fertility and early embryonic development and pre- and postnatal toxicology were not conducted with ixazomib, but evaluation of reproductive tissues was conducted in the general toxicity studies. There were no effects due to ixazomib treatment on male or female reproductive organs in studies up to 6-months duration in rats and up to 9-months duration in dogs.
14 Clinical Studies
14.1Multiple Myeloma in Patients Who Have Received at Least One Prior Therapy
The efficacy and safety of NINLARO in combination with lenalidomide and dexamethasone was evaluated in a randomized, double-blind, placebo-controlled, multicenter study in patients with relapsed and/or refractory multiple myeloma who had received at least one prior line of therapy. Patients who were refractory to lenalidomide or proteasome inhibitors were excluded from the study.
A total of 722 patients were randomized in a 1:1 ratio to receive either the combination of NINLARO, lenalidomide and dexamethasone (N=360; NINLARO regimen) or the combination of placebo, lenalidomide and dexamethasone (N=362; placebo regimen) until disease progression or unacceptable toxicity. Randomization was stratified according to number of prior lines of therapy (1 versus 2 or 3), myeloma International Staging System (ISS) (stage I or II versus III), and previous therapy with a proteasome inhibitor (exposed or na√Įve). Twenty three percent (N=166) of the patients had light chain disease and 12% (N=87) of patients had free light chain-measurable only disease.
Thromboprophylaxis was recommended for all patients in both treatment groups according to the lenalidomide prescribing information. Antiemetics were used in 19% of patients in the NINLARO regimen and 12% of patients in the placebo regimen; antivirals in 64% and 60%, respectively, and antihistamines in 27% and 19%, respectively. These medications were given to patients at the healthcare provider's discretion as prophylaxis and/or management of symptoms.
Patients received NINLARO 4 mg or placebo on Days 1, 8, and 15 plus lenalidomide (25 mg) on Days 1 through 21 and dexamethasone (40 mg) on Days 1, 8, 15, and 22 of a 28-day cycle. Patients with renal impairment received a starting dose of lenalidomide according to its prescribing information. Treatment continued until disease progression or unacceptable toxicities.
Table 6 summarizes the baseline patient and disease characteristics in the study. The baseline demographics and disease characteristics were balanced and comparable between the study regimens.
Table 6: Baseline Patient and Disease Characteristics NINLARO + Lenalidomide and Dexamethasone(N = 360) Placebo + Lenalidomide and Dexamethasone(N = 362) Patient Characteristics Median age in years (range) 66 (38, 91) 66 (30, 89) Gender (%) Male/ Female 58/42 56/44 Age Group (% [<65/ ‚Č•65 years]) 41/59 43/57 Race n (%) ¬†¬†White 310 (86) 301 (83) ¬†¬†Black 7 (2) 6 (2) ¬†¬†Asian 30 (8) 34 (9) ¬†¬†Other or Not Specified 13 (4) 21 (6) ECOG performance status, n (%) ¬†¬†0 or 1 336 (93) 334 (92) ¬†¬†2 18 (5) 24 (7) ¬†¬†Missing 6 (2) 4 (1) Creatinine clearance, n (%) ¬†¬†<30 mL/min 5 (1) 5 (1) ¬†¬†30-59 mL/min 74 (21) 95 (26) ¬†¬†‚Č•60 mL/min 281 (78) 261 (72) Disease Characteristics Myeloma ISS stage, n (%) ¬†¬†Stage I or II 315 (87) 320 (88) ¬†¬†Stage III 45 (13) 42 (12) Prior line therapies n (%) ¬†¬†Median (range) 1 (1, 3) 1 (1,3) ¬†¬†1 224 (62) 217 (60) ¬†¬†2 or 3 136 (38) 145 (40) Status at Baseline n (%) ¬†¬†Relapsed 276 (77) 280 (77) ¬†¬†Refractory Primary refractory, defined as best response of stable disease or disease progression on all prior lines of therapy, was documented in 7% and 6% of patients in the NINLARO regimen and placebo regimens, respectively. 42 (12) 40 (11) ¬†¬†Relapsed and Refractory 41 (11) 42 (12) Type of Prior Therapy n (%) ¬†¬†Bortezomib containing 248 (69) 250 (69) ¬†¬†Carfilzomib containing 1 (<1) 4 (1) ¬†¬†Thalidomide containing 157 (44) 170 (47) ¬†¬†Lenalidomide containing 44 (12) 44 (12) ¬†¬†Melphalan containing 293 (81) 291 (80) ¬†¬†Stem cell transplantation 212 (59) 199 (55) High risk (deletion (del) 17, t(4:14) and/or t(14:16) 75 (21) 62 (17) ¬†¬†deletion del (17) 36 (10) 33 (9)
The efficacy of NINLARO was evaluated by progression-free survival (PFS) according to the 2011 International Myeloma Working Group (IMWG) Consensus Uniform Response Criteria as assessed by a blinded independent review committee (IRC) based on central lab results. Response was assessed every four weeks until disease progression.
The approval of NINLARO was based upon a statistically significant improvement in PFS of the NINLARO regimen compared to the placebo regimen. PFS results are summarized in Table 7 and shown in Figure 1.
Table 7: Progression-Free Survival and Response Rate NINLARO + Lenalidomide and Dexamethasone(N = 360) Placebo + Lenalidomide and Dexamethasone(N = 362) NE: Not evaluable. Progression-free Survival PFS Events, n (%) 129 (36) 157 (43) Median (months)(95% CI) 20.6(17.0, NE) 14.7(12.9, 17.6) Hazard Ratio Hazard ratio is based on a stratified Cox's proportional hazard regression model. A hazard ratio less than 1 indicates an advantage for the NINLARO regimen. (95% CI)0.74(0.59, 0.94) p-value P-value is based on the stratified log-rank test. 0.012 Response Rate Overall Response Rate, n (%) 282 (78) 259 (72)   Complete Response 42 (12) 24 (7)   Very Good Partial Response 131 (36) 117 (32)   Partial Response 109 (30) 118 (33)
The median time to response was 1.1 months in the NINLARO regimen and 1.9 months in the placebo regimen. The median duration of response was 20.5 months in the NINLARO regimen and 15 months in the placebo regimen for responders in the response evaluable population.
Figure 1: Kaplan-Meier Plot of Progression-Free Survival
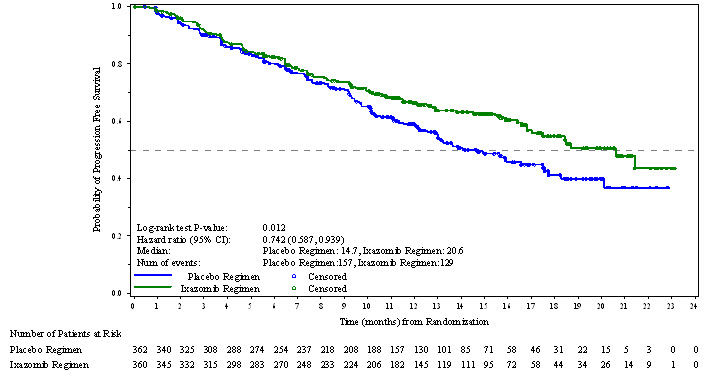
A non-inferential PFS analysis was conducted at a median follow up of 23 months with 372 PFS events. Hazard ratio of PFS was 0.82 (95% confidence interval [0.67, 1.0]) for NINLARO regimen versus placebo regimen, and estimated median PFS was 20 months in the NINLARO regimen and 15.9 months in the placebo regimen.
At the final analysis for OS at a median duration of follow up of approximately 85 months, median OS in the ITT population was 53.6 months for patients in the NINLARO regimen and 51.6 months for patients in the placebo regimen (HR = 0.94 [95% CI: 0.78, 1.13]).
14.2 Increased Mortality in Patients Treated with NINLARO in the Maintenance Setting
In C16019 (NCT02181413), newly diagnosed multiple myeloma patients who underwent autologous stem cell transplantation, continued on maintenance therapy for 24 months. There were 27% (105/395) deaths in the NINLARO arm compared with 26% (69/261) in the placebo arm. The hazard ratio for overall survival was 1.008 (95% CI: 0.744 - 1.367).
In C16021 (NCT02312258), newly diagnosed multiple myeloma patients, not treated with a stem cell transplant who achieved a partial response or better, continued on maintenance therapy for 24 months. There were 30% (127/425) deaths in the NINLARO arm compared with 27% (76/281) in the placebo arm. The hazard ratio for overall survival was 1.136 (95% CI: 0.853 - 1.514).
NINLARO is not recommended for use in the maintenance setting for multiple myeloma outside of controlled clinical trials [see Indications and Usage (1) and Warnings and Precautions (5.9)].
14.3Lack of Efficacy in Patients with Newly Diagnosed Multiple Myeloma
Lack of efficacy in patients with newly diagnosed multiple myeloma was determined in a prospective randomized clinical trial.
In C16014 (NCT01850524), in newly diagnosed multiple myeloma patients, the study did not meet the prespecified primary endpoint for PFS. There were 136 (39%) deaths in the NINLARO, lenalidomide, and dexamethasone arm compared to 148 (42%) in the lenalidomide and dexamethasone arm. The hazard ratio for overall survival was 0.998 (95% CI: 0.79 - 1.261).
NINLARO is not recommended for use in combination with lenalidomide and dexamethasone in newly diagnosed multiple myeloma outside of controlled clinical trials [see Indications and Usage (1)].
15 References
- OSHA Hazardous Drugs. OSHA. http://www.osha.gov/SLTC/hazardousdrugs/index.html
16 How Supplied/storage And Handling
How Supplied
NINLARO is supplied as follows:
Strength per Capsule Capsule Description Outer Carton 3 Count Buler Pack 1 Count Buler Pack NDC 4 mg Light orange, size 3, imprinted with "Takeda" on the cap and "4 mg" on the body in black ink. Three 4 mg capsules in a carton Each buler pack has three 4 mg capsules Each buler pack has one 4 mg capsule Outer carton NDC 63020-400-023 Count Buler Pack NDC 63020-400-031 Count Buler pack NDC 63020-400-01 3 mg Light grey, size 4, imprinted with "Takeda" on the cap and "3 mg" on the body in black ink. Three 3 mg capsules in a carton Each buler pack has three 3 mg capsules Each buler pack has one 3 mg capsule Outer carton NDC 63020-390-023 Count Buler Pack NDC 63020-390-031 Count Buler pack NDC 63020-390-01 2.3 mg Light pink, size 4, imprinted with "Takeda" on the cap and "2.3 mg" on the body in black ink. Three 2.3 mg capsules in a carton Each buler pack has three 2.3 mg capsules Each buler pack has one 2.3 mg capsule Outer carton NDC 63020-230-023 Count Buler Pack NDC 63020-230-031 Count Buler pack NDC 63020-230-01
Capsules are individually packaged in a PVC-Aluminum/Aluminum buler.
STORAGE AND HANDLING SECTION
Storage
Store NINLARO at room temperature. Do not store above 30¬įC (86¬įF). Do not freeze.
Store capsules in original packaging until immediately prior to use.
STORAGE AND HANDLING SECTION
Handling and Disposal
NINLARO is a hazardous drug. Follow applicable special handling and disposal procedures1.
Do not open or crush capsules. Avoid direct contact with the capsule contents. In case of capsule breakage, avoid direct contact of capsule contents with the skin or eyes. If contact occurs with the skin, wash thoroughly with soap and water. If contact occurs with the eyes, flush thoroughly with water.
Any unused medicinal product or waste material should be disposed in accordance with local requirements.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Dosing Instructions
- Instruct patients to take NINLARO exactly as prescribed.
- Advise patients to take NINLARO once a week on the same day and at approximately the same time for the first three weeks of a four week cycle. The importance of carefully following all dosage instructions should be discussed with patients starting treatment. Advise patients to take the recommended dosage as directed, because overdosage has led to deaths [see Overdosage (10)].
- Advise patients to take NINLARO at least one hour before or at least two hours after food.
- Advise patients that NINLARO and dexamethasone should not be taken at the same time, because dexamethasone should be taken with food and NINLARO should not be taken with food.
- Advise patients to swallow the capsule whole with water. The capsule should not be crushed, chewed or opened.
- Advise patients that direct contact with the capsule contents should be avoided. In case of capsule breakage, avoid direct contact of capsule contents with the skin or eyes. If contact occurs with the skin, wash thoroughly with soap and water. If contact occurs with the eyes, flush thoroughly with water.
- If a patient misses a dose, advise them to take the missed dose as long as the next scheduled dose is ‚Č•72 hours away. Advise patients not to take a missed dose if it is within 72 hours of their next scheduled dose.
- If a patient vomits after taking a dose, advise them not to repeat the dose but resume dosing at the time of the next scheduled dose.
- Advise patients to store capsules in original packaging, and not to remove the capsule from the packaging until just prior to taking NINLARO. [see Dosage and Administration (2.1)]
Thrombocytopenia
Advise patients that they may experience low platelet counts (thrombocytopenia). Signs of thrombocytopenia may include bleeding and easy bruising. [see Warnings and Precautions (5.1)].
Gastrointestinal Toxicities
Advise patients they may experience diarrhea, constipation, nausea and vomiting and to contact their healthcare providers if these adverse reactions persist. [see Warnings and Precautions (5.2)].
Peripheral Neuropathy
Advise patients to contact their healthcare providers if they experience new or worsening symptoms of peripheral neuropathy such as tingling, numbness, pain, a burning feeling in the feet or hands, or weakness in the arms or legs. [see Warnings and Precautions (5.3)].
Peripheral Edema
Advise patients to contact their healthcare providers if they experience unusual swelling of their extremities or weight gain due to swelling [see Warnings and Precautions (5.4)].
Cutaneous Reactions
Advise patients to contact their healthcare providers immediately if they experience new or worsening rash [see Warnings and Precautions (5.5)].
Thrombotic Microangiopathy
Advise patients to seek immediate medical attention if any signs or symptoms of thrombotic microangiopathy occur [see Warnings and Precautions (5.6)].
Hepatotoxicity
Advise patients to contact their healthcare providers if they experience jaundice or right upper quadrant abdominal pain [see Warnings and Precautions (5.7)].
Other Adverse Reactions
Advise patients to contact their healthcare providers if they experience signs and symptoms of acute febrile neutrophilic dermatosis (Sweet's syndrome), Stevens-Johnson syndrome, transverse myelitis, posterior reversible encephalopathy syndrome, tumor lysis syndrome, herpes zoster, cataracts, dry eyes, blurred vision, conjunctivitis and thrombotic thrombocytopenic purpura [see Adverse Reactions (6.1)].
Embryo-Fetal Toxicity
Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.8) and Use in Specific Populations (8.1)].
Advise females of reproductive potential to use effective contraception during treatment with NINLARO and for 90 days following the last dose. Advise women using hormonal contraceptives to also use a barrier method of contraception [see Use in Specific Populations (8.1)].
Advise males with female partners of reproductive potential to use effective contraception during treatment with NINLARO and for 90 days following the last dose [see Use in Specific Populations (8.1)].
Lactation
Advise women not to breastfeed during treatment with NINLARO and for 90 days after the last dose [see Use in Specific Populations (8.2)].
Concomitant Medications
Advise patients to speak with their healthcare providers about any other medication they are currently taking and before starting any new medications.
Distributed by: Takeda Pharmaceuticals America, Inc. Cambridge, MA 02142
NINLARO is a registered trademark of Millennium Pharmaceuticals, Inc.
©2024 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
For more information, you may also go to www.NINLARO.com or call 1-844-617-6468.
IXB349 R10
Spl Patient Package Insert Section
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: July/2024 PATIENT INFORMATION NINLARO¬ģ (nin-LAR-oh)(ixazomib)capsules NINLARO is used with two other prescription medicines called REVLIMID ¬ģ (lenalidomide) and dexamethasone. Read the Medication Guide that comes with REVLIMID ¬ģ (lenalidomide). You can ask your healthcare provider or pharmacist for information about dexamethasone. What is NINLARO? NINLARO is a prescription medicine used to treat multiple myeloma in combination with the medicines REVLIMID¬ģ (lenalidomide) and dexamethasone, in people who have received at least one prior treatment for their multiple myeloma.NINLARO should not be used to treat people: It is not known if NINLARO is safe and effective in children.
- who are receiving maintenance treatment, or
- who have been newly diagnosed with multiple myeloma, unless they are participants in a controlled clinical trial.
Before taking NINLARO, tell your healthcare provider about all of your medical conditions, including if you: Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Talk to your healthcare provider before starting any new medicines during treatment with NINLARO.
- have liver problems
- have kidney problems or are on dialysis
- are pregnant or plan to become pregnant. NINLARO can harm your unborn baby. Females who are able to become pregnant:
Males with female partners who are able to become pregnant:
- Avoid becoming pregnant during treatment with NINLARO.
- Your healthcare provider will do a pregnancy test before you start treatment with NINLARO.
- You should use effective non-hormonal birth control during treatment and for 90 days after your last dose of NINLARO. If using hormonal contraceptives (for example, birth control pills), you should also use an additional barrier method of contraception (for example, diaphragm or condom). Talk to your healthcare provider about birth control methods that may be right for you during this time.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with NINLARO.
- You should use effective birth control during treatment and for 90 days after your last dose of NINLARO.
- Tell your healthcare provider right away if your partner becomes pregnant or thinks she may be pregnant while you are being treated with NINLARO.
- are breastfeeding or plan to breastfeed. It is not known if NINLARO passes into breast milk, if it affects an infant who is breastfed, or breast milk production. Do not breastfeed during treatment with NINLARO and for 90 days after your last dose of NINLARO.
How should I take NINLARO?
- Take NINLARO exactly as your healthcare provider tells you to take it. Do not change your dose or stop taking NINLARO without talking to your healthcare provider first.
- NINLARO is taken in "cycles." Each cycle lasts 4 weeks (28 days).
- The usual dose of NINLARO is 1 capsule taken 1 time each week, on the same day of the week for the first 3 weeks of each cycle.
- Take each dose of NINLARO at about the same time of day.
- Take REVLIMID (lenalidomide) and dexamethasone exactly as your healthcare provider tells you to.
- Your healthcare provider will do blood tests during treatment with NINLARO to check for side effects.
- Your healthcare provider may change your dose or stop NINLARO, REVLIMID (lenalidomide), or dexamethasone if you have side effects.
- Take NINLARO at least 1 hour before or at least 2 hours after food.
- On the days that you take both NINLARO and dexamethasone, do not take NINLARO and dexamethasone at the same time. Take dexamethasone with food.
- Swallow NINLARO capsules whole with water. Do not crush, chew or open the capsule.
- Avoid direct contact with the capsule contents. If you accidentally get powder from the NINLARO capsule on your skin, wash the area well with soap and water. If you accidentally get powder from the NINLARO capsule in your eyes, flush your eyes well with water.
- If you miss a dose of NINLARO, or if you are late taking a dose, take the dose as long as the next scheduled dose is more than 3 days (72 hours) away. Do not take a missed dose of NINLARO if it is within 3 days (72 hours) of your next scheduled dose.
- If you vomit after taking a dose of NINLARO, do not repeat the dose. Take your next dose of NINLARO on the next scheduled day and time.
- Your healthcare provider may prescribe a medicine to take with NINLARO to decrease the risk of the chicken pox virus (herpes zoster) coming back (reactivation).
- Taking too much NINLARO (overdose) can cause serious side effects, including death. If you take more NINLARO than instructed by your healthcare provider, call your healthcare provider right away or go to the nearest hospital emergency room right away. Take your medicine pack with you.
What are the possible side effects of NINLARO? NINLARO may cause serious side effects, including:
- Low platelet counts (thrombocytopenia). Low platelet counts are common with NINLARO, and can sometimes be serious. You may need platelet transfusions if your counts are too low. Tell your healthcare provider if you have any signs of low platelet counts, including bleeding and easy bruising.
- Stomach and intestinal (gastrointestinal) problems. Diarrhea, constipation, nausea, and vomiting are common with NINLARO, and can sometimes be severe. Call your healthcare provider if you get any of these symptoms and they do not go away during treatment with NINLARO. Your healthcare provider may prescribe medicine to help treat your symptoms.
- Nerve problems. Nerve problems are common with NINLARO and may also be severe. Tell your healthcare provider if you get any new or worsening symptoms, including:
- tingling
- numbness
- pain
- a burning feeling in your feet or hands
- weakness in your arms or legs
- Swelling. Swelling is common with NINLARO and can sometimes be severe. Tell your healthcare provider if you develop swelling in your face, arms, hands, legs, ankles, or feet, or if you gain weight from swelling.
- Skin reactions. Rashes are common with NINLARO. NINLARO can cause rashes and other skin reactions that can be serious and can lead to death. Tell your healthcare provider right away if you get a new or worsening rash, severe bulering or peeling of the skin, or mouth sores.
- Thrombotic microangiopathy (TMA). This is a condition involving blood clots and injury to small blood vessels that may cause harm to your kidneys, brain, and other organs, and may lead to death. Get medical help right away if you get any of the following signs or symptoms during treatment with NINLARO:
- fever
- bruising
- nose bleeds
- tiredness
- decreased urination
Other common side effects of NINLARO include:
- Liver problems. Tell your healthcare provider if you get these signs of a liver problem:
- yellowing of your skin or the whites of your eyes
- pain in your right upper stomach-area (abdomen)
- low white blood cell counts (neutropenia)
- bronchitis
Tell your healthcare provider if you get new or worsening signs or symptoms of the following during treatment with NINLARO: These are not all the possible side effects of NINLARO. Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
- skin rash and pain (shingles) due to reactivation of the chicken pox virus (herpes zoster)
- blurred vision or other changes in your vision, dry eye and pink eye (conjunctivitis)
How should I store NINLARO? Keep NINLARO and all medicines out of the reach of children.
- Store NINLARO at room temperature. Do not store above 86¬įF (30¬įC).
- Do not freeze NINLARO.
- Store NINLARO capsules in the original packaging until just before each use.
- Ask your pharmacist or healthcare provider about how to dispose of (throw away) unused NINLARO.
General information about the safe and effective use of NINLARO. Medicines are sometimes prescribed for purposes other than those uled in a Patient Information leaflet. Do not use NINLARO for a condition for which it was not prescribed. Do not give NINLARO to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about NINLARO that is written for healthcare professionals. What are the ingredients in NINLARO? Active ingredient: ixazomib Inactive ingredients: microcrystalline cellulose, magnesium stearate, and talc Capsule shells: gelatin and titanium dioxide. The 4 mg capsule shell contains red and yellow iron oxide. The 3 mg capsule shell contains black iron oxide. The 2.3 mg capsule shell contains red iron oxide. The printing ink contains shellac, propylene glycol, potassium hydroxide, and black iron oxide. Distributed by: Takeda Pharmaceuticals America, Inc. Cambridge, MA 02142 NINLARO is a registered trademark of Millennium Pharmaceuticals, Inc. ©2024 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.For more information, you may also go to www.NINLARO.com or call 1-844-617-6468. IXB349 R10
Principal Display Panel - 4 Mg Capsule Blister Pack
Rx only          NDC 63020-400-03
NINLARO ¬ģ (ixazomib) capsules
4 mg per capsule
Contains 3 Capsules
Please read Package Insert before use.
Lift to Open
Takeda

Principal Display Panel - 3 Mg Capsule Blister Pack
Rx only          NDC 63020-390-03
NINLARO ¬ģ (ixazomib) capsules
3 mg per capsule
Contains 3 Capsules
Please read Package Insert before use.
Lift to Open
Takeda

Principal Display Panel - 2.3 Mg Capsule Blister Pack
Rx only          NDC 63020-230-03
NINLARO ¬ģ (ixazomib) capsules
2.3 mg per capsule
Contains 3 Capsules
Please read Package Insert before use.
Lift to Open
Takeda

DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


