Nortrel 7/7/7 (nitroglycerin 0.6 mg) Dailymed
Generic: norethindrone and ethinyl estradiol is used for the treatment of Breast Neoplasms Cerebral Arterial Diseases Coronary Artery Disease Hypertension Hypogonadism Liver Diseases Menopause, Premature Menorrhagia Neoplasms, Hormone-Dependent Pregnancy Prostatic Neoplasms Thromboembolism Thrombophlebitis Osteoporosis, Postmenopausal Primary Ovarian Insufficiency Endometrial Neoplasms Hot Flashes Tobacco Use Acne Vulgaris Endometrial Hyperplasia Endometriosis Osteoporosis Pulmonary Embolism Uterine Hemorrhage Venous Thrombosis
IMPRINT: N 6
SHAPE: round
COLOR: white
All Imprints
frovatriptan succinate 2.5 mg - e 2 5 round white
dipyridamole 75 mg - 19 round orange
aspirin 325 mg - aspirin 44 249 round white
valsartan 80 mg - 7432 tv round pink
calcium fluoride 30 [hp_x] - round white
captopril 100 mg - w 905 round white
levodopa 50 mgentacapone 200 mgcarbidopa 12.5 mg - w782 round brown
calcium acetate 667 mg - p113 round white
lithium carbonate 300 mg - ww 300 round white
cyclophosphamide 25 mg - 54 639 round blue
methylphenidate hydrochloride 10 mg - ciba 3 round green
desloratadine 5 mg - 5 round blue
carvedilol 25 mg - zc42 round white
iloperidone 8 mg - 8 round white
glyburide 2.5 mg - cor 124 round yellow
bismuth subsalicylate 262 mg - rh046 round pink
moexipril hydrochloride 7.5 mg - apo moe 7 5 round white
- r221 round orange
venlafaxine hydrochloride 50 mg - ip 303 round orange
pseudoephedrine hydrochloride 30 mg - tcl016 round red
donepezil hydrochloride 5 mg - i 24 round white
methadone hydrochloride 5 mg - u41 round white
donepezil hydrochloride 10 mg - i 21 round yellow
amlodipine besylate 2.5 mgatorvastatin calcium trihydrate 20 mg - pfizer cdt 252 round white
chlorpheniramine maleate 4 mg - 44 194 round yellow
tamoxifen citrate 20 mg - m 274 round white
hydrochlorothiazide 50 mg - h 3 round orange
pitavastatin calcium 4.18 mg - 4 kc round white
venlafaxine hydrochloride 25 mg - 6147 v round orange
docusate sodium 50 mgsennosides a and b 8.6 mg - tcl081 round orange
quinidine gluconate 324 mg - mp 66 round white
oxycodone hydrochloride 7.5 mgacetaminophen 325 mg - watson 933 round white
cyclobenzaprine hydrochloride 5 mg - tl 211 round orange
trihexyphenidyl hydrochloride 2 mg - 5971 v round white
lamotrigine 50 mg - h009 round orange
rabeprazole sodium 20 mg - 107 round yellow
carbamazepine 200 mg - t 200 mg round pink
enalapril maleate 5 mghydrochlorothiazide 12.5 mg - apo 5 12 5 round red
diclofenac sodium 100 mg - r 717 round yellow
minoxidil 10 mg - dan 5643 10 round white
acetaminophen 500 mg - ap 013 round white
levonorgestrel 0.1 mgethinyl estradiol 0.02 mg - b 965 round pink
clonazepam 0.5 mg - 832 teva round yellow
oxcarbazepine 300 mg - 54 515 round orange
fludrocortisone acetate 0.1 mg - 7033 round white
atovaquone 250 mgproguanil hydrochloride 100 mg - gx cm3 round pink
lamotrigine 50 mg - lamictal xr 50 round green
maprotiline hydrochloride 75 mg - 9 2 m round white
candesartan cilexetil 4 mg - acf 004 round white
memantine hydrochloride 5 mg - m5 v round white
lamotrigine 150 mg - lam 150 apo round yellow
acarbose 50 mg - precose 50 round white
docusate sodium 50 mgsennosides 8.6 mg - tcl 131 round purple
dextroamphetamine saccharate 3.75 mgamphetamine aspartate monohydrate 3.75 mgdextroamphetamine sulfate 3.75 mgamphetamine sulfate 3.75 mg - b 777 1 5 round orange
paroxetine hydrochloride hemihydrate 25 mg - gsk 25 round pink
bupropion hydrochloride 100 mg - wellbutrin 100 round red
memantine hydrochloride 10 mg - m10 x round white
dextroamphetamine saccharate 2.5 mgamphetamine aspartate monohydrate 2.5 mgdextroamphetamine sulfate 2.5 mgamphetamine sulfate 2.5 mg - 1 0 dp round blue
nifedipine 60 mg - 60 adalat cc round pink
lisinopril 10 mghydrochlorothiazide 12.5 mg - lh1 m round white
alprazolam 1 mg - cor 188 round yellow
liothyronine sodium 50 ug - 50 223 round white
venlafaxine hydrochloride 75 mg - 6150 v round orange
metoprolol tartrate 50 mg - c 74 round pink
prednisone 10 mg - west ward 473 round white
trandolapril 2 mg - fx round yellow
pitavastatin calcium 1 mg - 1 kc round white
dextroamphetamine saccharate 3.125 mgamphetamine aspartate monohydrate 3.125 mgdextroamphetamine sulfate 3.125 mgamphetamine sulfate 3.125 mg - 12 5 d p round orange
benztropine mesylate 2 mg - b 1116 round white
chlorpheniramine maleate 12 mg - chlorphen 12 round orange
lisinopril 10 mg - ww 267 round pink
paroxetine hydrochloride hemihydrate 37.5 mg - gsk 37 5 round blue
naproxen 250 mg - 93 147 round red
morphine sulfate 60 mg - m ms 60 round orange
hydrocodone bitartrate 7.5 mgibuprofen 200 mg - 3585 v round white
warfarin sodium 2 mg - ig w 2 round purple
galantamine hydrobromide 12 mg - janssen g 12 round brown
methazolamide 50 mg - eff 20 round white
simvastatin 10 mg - sv 10 round pink
norethindrone 1 mgethinyl estradiol 0.035 mg - b 949 round yellow
potassium chloride 600 mg - ktab round yellow
famciclovir 250 mg - 8118 93 round white
progesterone 100 mg - sv round orange
isosorbide dinitrate 10 mg - gg26 round white
flecainide acetate 50 mg - an 641 round white
buspirone hydrochloride 10 mg - teva 54 round white
topiramate 50 mg - apo tp 50 round yellow
simvastatin 40 mg - sv 40 round pink
isosorbide dinitrate 5 mg - bpi 152 round pink
- b 247 round brown
clonazepam 0.25 mg - b 95 1 4 round white
prednisolone sodium phosphate 30 mg - ora 30 round white
nifedipine 30 mg - m 475 round pink
alendronate sodium 5 mg - 93 5140 round white
chloroquine phosphate 250 mg - 0115 2790 round white
acarbose 25 mg - precose 25 round white
bumetanide 1 mg - e 129 round yellow
levomefolate calcium 0.451 mg - m round orange
flavoxate hydrochloride 100 mg - 58 round white
verapamil hydrochloride 80 mg - watson 343 round white
desipramine hydrochloride 10 mg - 68 7 round blue
levonorgestrel 0.15 mgethinyl estradiol 0.02 mg - tv 076 round pink
atenolol 25 mg - 787 teva round white
dipyridamole 75 mg - c83 round white
hydrocortisone 10 mg - cp 332 round white
desipramine hydrochloride 75 mg - e 722 round blue
citalopram hydrobromide 10 mg - mx31 round orange
lamotrigine 150 mg - taro lmt 150 round white
- 54-980 round blue
topiramate 25 mg - ig 278 round white
hydroxyzine hydrochloride 50 mg - tv 309 round white
cefuroxime axetil 250 mg - w 921 round white
acarbose 25 mg - 54 311 round white
lamotrigine 100 mg - j 246 round white
sennosides a and b 8.6 mg - gpi w2 round brown
metformin hydrochloride 500 mg - h 102 round white
olanzapine 5 mg - m oe1 round yellow
zolpidem tartrate 12.5 mg - a1 round yellow
bupropion hydrochloride 100 mg - g 2442 round yellow
- dan 5540 round white
hydromorphone hydrochloride 4 mg - m 4 round white
phytonadione 5 mg - aton 405 mephyton round yellow
nifedipine 30 mg - 30 adalat cc round pink
tramadol hydrochloride 200 mg - 200 er round white
cinchona officinalis bark 30 [hp_c]coffea arabica fruit 6 [hp_c]strychnos nux-vomica seed 30 [hp_c]matricaria chamomilla flowering top oil 6 [hp_c]artemisia cina flower 30 [hp_c] - none round white
paroxetine hydrochloride hemihydrate 10 mg - zc 15 round white
hydralazine hydrochloride 50 mg - par 028 round orange
benazepril hydrochloride 10 mg - apo be 10 round yellow
propafenone hydrochloride 225 mg - 5125 v round white
eszopiclone 1 mg - 93 e7 round blue
carbinoxamine maleate 4 mg - bp 605 round white
metronidazole 250 mg - 3969 wpi round white
oxybutynin chloride 10 mg - g342 round pink
ethinyl estradiol 0.01 mg - b 556 round yellow
hydrochlorothiazide 6.25 mgbisoprolol fumarate 2.5 mg - ul l round yellow
metoprolol tartrate 100 mg - re 76 round white
aripiprazole 30 mg - tv 7583 round pink
ropinirole hydrochloride 2 mg - 54 231 round orange
- west-ward 248 round yellow
acetaminophen 300 mgcodeine phosphate 15 mg - 2 m round white
calcium carbonate 750 mg - fc round green
levocetirizine dihydrochloride 5 mg - 161 h round white
glipizide 2.5 mg - wpi 900 round orange
torsemide 20 mg - pa 917 round white
olanzapine 7.5 mg - m 335 round white
metformin hydrochloride 500 mg - andrx 674 500 round white
norethindrone acetate 1.5 mgethinyl estradiol 30 ug - b 978 round pink
azathioprine 50 mg - 54 043 round yellow
bupropion hydrochloride 100 mg - apo bup 100 round purple
estradiol 0.5 mg - watson 528 round white
olanzapine 20 mg - tv u4 20 round yellow
levonorgestrel 1.5 mg - g00 round white
nitazoxanide 500 mg - alinia 500 round yellow
zolmitriptan 5 mg - f11 round white
paroxetine hydrochloride hemihydrate 30 mg - m n3 round blue
doxazosin mesylate 8 mg - n 598 8 round white
hydrochlorothiazide 50 mg - 3572 v round orange
levonorgestrel 0.075 mgethinyl estradiol 0.040 mg - dp 511 round white
glipizide 10 mg - 10 round white
norethindrone acetate 1 mgethinyl estradiol 20 ug - b 711 round pink
imipramine hydrochloride 50 mg - par 56 round green
repaglinide 1 mg - p241 round yellow
felodipine 2.5 mg - 450 plendil round green
ciprofloxacin hydrochloride 250 mg - cr 250 round white
pravastatin sodium 10 mg - teva 771 round pink
prednisone 20 mg - tl175 round pink
ethinyl estradiol 0.01 mg - dp 457 round yellow
calcium carbonate 420 mg - az 036 round white
alprazolam 0.5 mg - cor 187 round white
haloperidol 0.5 mg - mylan 351 round orange
midodrine hydrochloride 5 mg - g 422 round orange
carvedilol 12.5 mg - zc41 round white
metformin hydrochloride 850 mg - andrx 675 850 round white
desipramine hydrochloride 25 mg - e 19 round blue
olanzapine 5 mg - tv u1 5 round yellow
felodipine 10 mg - 452 plendil round red
flecainide acetate 50 mg - rx794 round white
fosinopril sodium 40 mg - 202 ig round white
rabeprazole sodium 20 mg - aciphex 20 round yellow
zolpidem tartrate 5 mg - m z1 round purple
metoprolol succinate 100 mg - a ms round white
leucovorin calcium 15 mg - 54 650 round yellow
amoxapine 50 mg - dan 50 5714 round orange
clozapine 100 mg - clozaril 100 round yellow
leucovorin calcium 25 mg - 54 013 round yellow
tramadol hydrochloride 300 mg - 300 er round white
tolterodine tartrate 2 mg - dt round white
doxycycline 50 mg - lci 1335 round yellow
minoxidil 10 mg - 10 mp 89 round white
aspirin 81 mg - az 013 round orange
lorazepam 2 mg - 242 2 watson round white
trandolapril 4 mg - tn4 round white
propranolol hydrochloride 60 mg - 54 85 v round pink
dimethicone 80 mgcalcium carbonate 750 mg - dr round pink
prochlorperazine maleate 10 mg - tl115 round green
dexamethasone 1.5 mg - 54 943 round pink
ranitidine hydrochloride 150 mg - gg 705 round pink
sodium fluoride 0.5 mg - sci 1007 round white
prednisone 5 mg - westward 475 round white
alprazolam 2 mg - sp 324 2 round white
pioglitazone hydrochloride 15 mg - actos 15 round white
aspirin 162 mgacetaminophen 110 mgsalicylamide 152 mgcaffeine 32.4 mg - fr2 round orange
meloxicam 7.5 mg - zc 25 round yellow
metolazone 2.5 mg - m 172 round orange
amlodipine besylate 5 mgolmesartan medoxomil 40 mg - c75 round white
ondansetron hydrochloride 8 mg - r 154 round yellow
diclofenac sodium 75 mgmisoprostol 200 ug - 0398 round white
sitagliptin phosphate 100 mg - 277 round brown
acarbose 25 mg - e71 round white
albuterol sulfate 4 mg - mp 88 round white
topiramate 50 mg - omn 50 round yellow
dextroamphetamine saccharate 5 mgamphetamine aspartate monohydrate 5 mgdextroamphetamine sulfate 5 mgamphetamine sulfate 5 mg - e 401 round orange
trifluoperazine hydrochloride 2 mg - m t4 round white
oxycodone hydrochloride 20 mg - op 20 round pink
citalopram hydrobromide 10 mg - 206 ig round yellow
trazodone hydrochloride 100 mg - pliva 434 round white
zolmitriptan 2.5 mg - zomig 25 round yellow
desipramine hydrochloride 50 mg - e 721 round blue
dextroamphetamine saccharate 7.5 mgamphetamine aspartate monohydrate 7.5 mgdextroamphetamine sulfate 7.5 mgamphetamine sulfate 7.5 mg - e 404 round orange
trazodone hydrochloride 100 mg - apo t100 round white
hydralazine hydrochloride 100 mg - hp 4 round pink
meclizine hydrochloride 25 mg - m mcz 25 round white
levetiracetam 250 mg - m 613 round white
alendronate sodium 35 mg - 637 round white
dexamethasone 0.5 mg - 54 299 round yellow
carbidopa 25 mglevodopa 100 mg - apo 25 100 round yellow
norethindrone 0.5 mgethinyl estradiol 0.035 mg - b 941 round yellow
irbesartan 75 mg - m in1 round white
calcium ascorbate 50 mgcalcium threonate 50 mgcholecalciferol 6 ug.alpha.-tocopherol acetate, dl- 3.5 [iu]pyridoxine hydrochloride 2 mgfolic acid 1 mgcalcium carbonate 250 mgferrous fumarate 40 mgmagnesium oxide 50 mgzinc oxide 15 mgcupric oxide 2 mg - tl014 round grey
hydromorphone hydrochloride 2 mg - p 2 round orange
norethindrone acetate 1 mgethinyl estradiol .02 mg - 93 912 round white
sodium starch glycolate type a corn 3.61 mgpovidone k30 5.415 mgstearic acid 1.805 mgacetaminophen 324.9 mgstarch, corn 25.27 mg - 325 round white
megestrol acetate 20 mg - par 289 round white
propranolol hydrochloride 40 mg - 54 84 v round green
tinidazole 250 mg - tm 250 round pink
lisinopril 40 mg - 3761 round white
escitalopram oxalate 10 mg - 11 36 round white
amitriptyline hydrochloride 75 mg - m 37 round blue
medroxyprogesterone acetate 2.5 mg - g3740 round orange
amlodipine besylate 5 mgvalsartan 160 mghydrochlorothiazide 25 mg - tv 7037 round yellow
trihexyphenidyl hydrochloride 2 mg - dan dan 5335 round white
amitriptyline hydrochloride 100 mg - 2105 v round red
acarbose 100 mg - e73 round white
norethindrone 1 mgethinyl estradiol 0.035 mg - b 943 round orange
lorazepam 2 mg - mylan 777 round white
bisoprolol fumarate 5 mghydrochlorothiazide 6.25 mg - b 50 round pink
oxycodone hydrochloride 15 mg - m 15 round green
repaglinide 1 mg - 745 c round yellow
butalbital 50 mgacetaminophen 325 mgcaffeine 40 mg - lci 1695 round blue
aripiprazole 30 mg - a 011 30 round pink
levonorgestrel 0.15 mgethinyl estradiol 0.03 mg - b 555 round blue
glipizide 10 mg - glipizide xl 10 round white
olanzapine 2.5 mg - m 157 round orange
promethazine hydrochloride 50 mg - zc03 round white
zolmitriptan 5 mg - zomig 5 round pink
acetaminophen 300 mgcodeine phosphate 30 mg - 3 tv 150 round white
nadolol 80 mgbendroflumethiazide 5 mg - kpi 284 corzide 80 5 round white
lamotrigine 200 mg - lamictal xr 200 round blue
albuterol sulfate 2 mg - m 255 round white
bupropion hydrochloride 75 mg - wellbutrin 75 round yellow
carisoprodol 350 mg - dan 5513 round white
hydrochlorothiazide 50 mg - 112 s g round white
cyclophosphamide 50 mg - 54 980 round blue
benztropine mesylate 0.5 mg - cor 143 round white
norethindrone acetate 1 mgethinyl estradiol 20 ug - b 977 round yellow
perindopril erbumine 2 mg - d 5 7 round white
propranolol hydrochloride 10 mg - pliva 467 round orange
pramipexole dihydrochloride 0.25 mg - p2 round blue
amitriptyline hydrochloride 100 mg - gg461 round orange
ropinirole 2 mg - 93 5285 round pink
olanzapine 10 mg - lilly 4117 round white
trihexyphenidyl hydrochloride 2 mg - w 4 round white
repaglinide 0.5 mg - p240 round white
nifedipine 30 mg - eln 30 round brown
trandolapril 4 mg - lu h03 round red
warfarin sodium 10 mg - ig w 10 round white
bismuth subsalicylate 262 mg - ap 045 round pink
ropinirole hydrochloride 4 mg - m re4 round brown
dipyridamole 25 mg - 17 round orange
lithium carbonate 450 mg - 224 g breakline round yellow
estradiol 1 mgnorethindrone acetate 0.5 mg - novo 288 round white
venlafaxine hydrochloride 75 mg - 759 round
enalapril maleate 10 mg - elp 10 round brown
carvedilol 25 mg - g41 25 round white
metoprolol tartrate 50 mg - 477 round white
pitavastatin calcium 2 mg - 2 kc round white
folic acid 1 mg - ig 210 round yellow
meloxicam 7.5 mg - 7 5 round yellow
bupropion hydrochloride 100 mg - a 171 round yellow
chlorpromazine hydrochloride 25 mg - gg476 25 round orange
carbidopa 25 mglevodopa 250 mg - m c53 round green
pramipexole dihydrochloride 0.125 mg - 91 round white
dimenhydrinate 50 mg - 0111 v round white
chlorpromazine hydrochloride 200 mg - gg457 200 round orange
ranitidine hydrochloride 150 mg - apo ran 150 round pink
tramadol hydrochloride 50 mg - m t7 round white
citalopram hydrobromide 40 mg - 208 ig round white
carvedilol 6.25 mg - zc40 round white
labetalol hydrochloride 200 mg - cl38 200 round white
diclofenac potassium 50 mg - 93 948 round orange
fosinopril sodium 20 mg - 201 ig round white
clonazepam 0.125 mg - b 94 1 8 round white
carisoprodol 350 mg - 2410 v round white
candesartan cilexetil 8 mg - acg 008 round pink
risperidone 0.25 mg - 93 221 round yellow
tamoxifen citrate 10 mg - m 144 round white
pyridostigmine bromide 60 mg - mestinon v 60 round white
carbidopa 25 mglevodopa 100 mg - apo 131 round brown
citalopram hydrobromide 10 mg - a 05 round orange
spironolactone 100 mg - searle 1031 aldactone 100 round orange
glipizide 10 mg - 9200 teva round white
nisoldipine 17 mg - sci 501 round yellow
promethazine hydrochloride 25 mg - an 521 round white
olanzapine 7.5 mg - lilly 4116 round white
spironolactone 100 mg - 58 82 v round white
oxycodone hydrochloride 10 mg - op 10 round white
propranolol hydrochloride 80 mg - 54 86 v round yellow
amiodarone hydrochloride 100 mg - as 100 round yellow
levonorgestrel 0.050 mgethinyl estradiol 0.030 mg - dp 510 round pink
mebendazole 100 mg - 93 107 round orange
sennosides a and b 8.6 mg - az217 round brown
estradiol valerate 2 mgdienogest 3 mg - dh round yellow
amlodipine besylate 2.5 mgatorvastatin calcium trihydrate 10 mg - r 407 round white
meloxicam 15 mg - m 89 round yellow
nifedipine 60 mg - b 60 round red
methocarbamol 500 mg - west ward 290 round white
metformin hydrochloride 850 mg - bms 6070 850 round white
aspirin 81 mg - heart round yellow
aripiprazole 15 mg - a 009 15 round yellow
clomiphene citrate 50 mg - watson 781 round white
olanzapine 2.5 mg - c 45 round yellow
dexmethylphenidate hydrochloride 5 mg - 93 5276 round yellow
quinapril hydrochloride 20 mg - lu f03 round yellow
ethynodiol diacetate 1 mgethinyl estradiol 35 ug - b 14 round yellow
griseofulvin 500 mg - ortho 214 round white
cefprozil 250 mg - 93 1077 round orange
felodipine 5 mg - e137 round pink
propranolol hydrochloride 10 mg - mylan 182 10 round orange
eltrombopag olamine 25 mg - gs nx3 25 round orange
clonazepam 2 mg - b 98 2 round white
allopurinol 300 mg - m 71 round white
estradiol 0.5 mg - e 3 m round white
spironolactone 50 mg - mp 542 round white
- 3m tr 50 round white
metoprolol tartrate 100 mg - c 75 round blue
pioglitazone hydrochloride 15 mg - 31 h round white
salsalate 500 mg - bp 507 round yellow
bethanechol chloride 50 mg - lci 1329 round yellow
codeine phosphate 15 mgacetaminophen 300 mg - 2063 v 2 round white
methimazole 5 mg - bp 655 round white
tolterodine tartrate 1 mg - to round white
atovaquone 62.5 mgproguanil hydrochloride 25 mg - gx cg7 round pink
lamotrigine 200 mg - l124 round white
levonorgestrel 0.15 mgethinyl estradiol 0.03 mg - b 992 round pink
metoclopramide hydrochloride 10 mg - teva 2203 round white
venlafaxine hydrochloride 37.5 mg - 6148 v round orange
irbesartan 150 mghydrochlorothiazide 12.5 mg - 54 857 round red
diclofenac sodium 100 mg - dx 41 round pink
risedronate sodium monohydrate 35 mg - teva 7389 round orange
ethinyl estradiol 0.01 mg - tv 077 round yellow
aspirin 325 mg - aspirin 44157 round white
ropinirole hydrochloride 2 mg - 975 hh round pink
nilutamide 150 mg - 168d round white
carbidopa 25 mglevodopa 100 mg - 93 293 teva round yellow
doxycycline 100 mg - i63 round orange
testosterone 30 mg - a round white
benazepril hydrochloride 20 mg - lotensin 20 round pink
simvastatin 40 mg - rx792 round red
trifluoperazine hydrochloride 5 mg - gg55 5 round purple
albuterol sulfate 4 mg - v 4 round green
metformin hydrochloride 500 mg - a 12 round white
topiramate 200 mg - ig 281 round pink
quinidine sulfate 200 mg - dan dan 5438 round white
doxycycline 50 mg - i61 round orange
metformin hydrochloride 500 mg - 574 round white
carbamazepine 100 mg - taro 16 round white
hydrochlorothiazide 50 mg - hp 46 round white
trifluoperazine hydrochloride 5 mg - m t5 round purple
imipramine hydrochloride 50 mg - v13 lu round brown
lamotrigine 25 mg - taro lmt 25 round white
aripiprazole 10 mg - 10 18 round white
propranolol hydrochloride 80 mg - dan 5557 80 round yellow
benztropine mesylate 0.5 mg - b 1114 round white
hydrochlorothiazide 12.5 mglisinopril 10 mg - ww 62 round blue
aspirin 81 mg - 81 round yellow
doxazosin mesylate 1 mg - m d9 round white
mitotane 500 mg - bl l1 round white
lamotrigine 100 mg - par 563 round brown
cetirizine hydrochloride 5 mgpseudoephedrine hydrochloride 120 mg - 5029 5 120 round white
linagliptin 5 mg - d5 round red
estradiol 2 mg - watson 488 round green
bumetanide 2 mg - e 130 round brown
lamotrigine 25 mg - lmt 25 round white
alprazolam 2 mg - r 87 round pink
nifedipine 60 mg - ku 261 round pink
norethindrone acetate 1.5 mgethinyl estradiol 0.03 mg - watson 631 round green
doxycycline hyclate 100 mg - dan 5553 round orange
carvedilol 6.25 mg - m c32 round white
atenolol 100 mg - z 67 round white
demeclocycline hydrochloride 150 mg - an 54 round red
risperidone 0.5 mg - 93 225 round red
bethanechol chloride 50 mg - bcl 50 832 round yellow
bisacodyl 5 mg - tcl 003 round orange
bupropion hydrochloride 150 mg - 141 round white
morphine sulfate 30 mg - m 30 round purple
azilsartan kamedoxomil 80 mg - asl 80 round white
dextroamphetamine sulfate 10 mg - 953 10 b round pink
neomycin sulfate 500 mg - zynova 01 round white
quetiapine fumarate 100 mg - apo que 100 round yellow
quetiapine fumarate 200 mg - apo que 200 round white
finasteride 5 mg - ig 412 round blue
clonidine hydrochloride 0.1 mg - 241 round pink
glipizide 5 mg - gxl 5 round white
- deltasone 20 round orange
guaifenesin 600 mg - l498 round white
amlodipine besylate 5 mg - m a9 round blue
desipramine hydrochloride 10 mg - 341 round white
captopril 12.5 mg - w 7 round white
diclofenac sodium 100 mg - m 355 round yellow
metoprolol tartrate 100 mg - 93 734 round blue
anastrozole 1 mg - adx1 round white
haloperidol 10 mg - mylan 334 round green
imipramine hydrochloride 50 mg - gg 42 round green
desipramine hydrochloride 75 mg - gg166 round white
chlorpromazine hydrochloride 200 mg - 832 200 round brown
adefovir dipivoxil 10 mg - 3 round white
dipyridamole 50 mg - c82 round white
methimazole 10 mg - bp 656 round white
montelukast sodium 5 mg - 54 741 round pink
ramelteon 8 mg - tak ram 8 round orange
fluvastatin sodium 80 mg - lescol xl 80 round yellow
hyoscyamine sulfate 0.125 mg - pad h round white
azilsartan kamedoxomil 40 mgchlorthalidone 12.5 mg - ac 40 12 5 round red
clonazepam 0.5 mg - r 33 round pink
zidovudine 300 mg - 54 777 round white
lovastatin 20 mg - 20 round orange
moexipril hydrochloride 15 mg - g 208 round brown
desogestrel 0.15 mgethinyl estradiol 0.02 mg - dp 021 round white
bupropion hydrochloride 100 mg - e over 410 round blue
fosinopril sodium 40 mg - ig 202 round white
pilocarpine hydrochloride 5 mg - lan 1313 round white
hydrocodone bitartrate 7.5 mgibuprofen 200 mg - 5161 round white
bisoprolol fumarate 5 mghydrochlorothiazide 6.25 mg - e 704 round red
moexipril hydrochloride 7.5 mg - g 209 round pink
hydrocortisone 5 mg - cp 331 round white
olanzapine\ 7.5 mg - 7654 round white
metoprolol tartrate 100 mg - m 47 round blue
propranolol hydrochloride 20 mg - dan 5555 20 round blue
lisinopril 20 mghydrochlorothiazide 25 mg - lh3 m round green
spironolactone 100 mg - an 515 round brown
thioridazine hydrochloride 100 mg - mp 160 round yellow
ascorbic acid 100 mgthiamine mononitrate 1.5 mgriboflavin 1.7 mgniacinamide 20 mgpyridoxine hydrochloride 10 mgfolic acid 1 mgcobalamin 6 ugbiotin 300 ugcalcium pantothenate 10 mgzinc citrate 50 mg - h round yellow
glycopyrrolate 1 mg - k 400 round white
allopurinol 100 mg - zyloprim 100 round white
norethindrone acetate 1 mgethinyl estradiol 0.02 mg - pd 915 round white
doxazosin mesylate 2 mg - m d10 round pink
acetazolamide 125 mg - t52 round white
ribavirin 200 mg - zc19 round pink
clozapine 100 mgaspartame 12.4 mg - a08 round yellow
bisoprolol fumarate 5 mghydrochlorothiazide 6.25 mg - m 503 round blue
estropipate 3 mg - watson 416 round blue
dimethicone 125 mg - ap 040 round white
hydrocortisone 20 mg - ww 254 round white
haloperidol 2 mg - mylan 214 round orange
desipramine hydrochloride 100 mg - e 736 round blue
phenobarbital 16.2 mg - 5011 v round white
aripiprazole 15 mg - ari 15 apo round yellow
ciprofloxacin hydrochloride 250 mg - y101 round white
alprazolam 0.5 mg - r 83 round white
- 3m tr 100 round white
desmopressin acetate 0.2 mg - 0 2 37 av round white
naproxen 250 mg - ip188 250 round white
amlodipine besylate 2.5 mgatorvastatin calcium trihydrate 40 mg - pfizer cdt 254 round white
clobazam 5 mg - lu 5 round white
propafenone hydrochloride 225 mg - mp 512 round white
nifedipine 30 mg - b 30 round red
atovaquone 250 mgproguanil hydrochloride 100 mg - 404 g round pink
buprenorphine hydrochloride 2 mgnaloxone hydrochloride dihydrate 0.5 mg - 154 round white
lisinopril 20 mghydrochlorothiazide 12.5 mg - a 28 round yellow
torsemide 5 mg - pa 915 round white
penicillin v potassium 250 mg - gg949 pvk250 round white
chlorambucil 2 mg - gx eg3 l round brown
pioglitazone hydrochloride 45 mg - actos 45 round white
trazodone hydrochloride 100 mg - mp 114 round white
ketoconazole 200 mg - janssen nizoral round white
prednisone 20 mg - dan dan 5443 round orange
norethindrone 0.5 mgethinyl estradiol 0.035 mg - b 951 round yellow
hydroxyzine hydrochloride 25 mg - 3616 v round green
atenolol 50 mg - d 22 round white
finasteride 5 mg - h 37 round blue
propafenone hydrochloride 150 mg - 5124 v round white
allopurinol 300 mg - n021 round orange
metolazone 5 mg - 644 5 round blue
clopidogrel bisulfate 75 mg - apo cl 75 round pink
morphine sulfate 30 mg - m ms 30 round purple
codeine sulfate 60 mg - 60 54 412 round white
zinc acetate 2 [hp_x]zinc gluconate 2 [hp_x] - rd round red
primidone 50 mg - lan 1301 round white
lamotrigine 150 mg - j 247 round white
simvastatin 5 mg - ll c01 round brown
promethazine hydrochloride 25 mg - gg 225 round white
dimenhydrinate 50 mg - 44 198 round white
simvastatin 40 mg - ll c04 round red
doxycycline hyclate 20 mg - mp 573 round white
potassium chloride 600 mg - kc 8 round blue
chlorpromazine hydrochloride 50 mg - sz 203 round brown
- dp 519 round green
amlodipine besylate 10 mg - s25 round white
alendronate sodium 5 mg - m a6 round white
risperidone 4 mg - p 403 round white
- b 343 round pink
quetiapine fumarate 100 mg - 93 8162 round orange
guanfacine hydrochloride 1 mg - watson 444 round pink
hydrocortisone 5 mg - cortef 5 round white
acyclovir 400 mg - m 253 round white
mirtazapine 45 mg - m 545 round brown
norethindrone 0.75 mgethinyl estradiol 0.035 mg - b 942 round blue
amlodipine besylate 10 mgolmesartan medoxomil 20 mg - c74 round orange
methylphenidate hydrochloride 20 mg - dan 20 5884 round orange
betaxolol hydrochloride 20 mg - e39 round white
thyroid, porcine 15 mg - a tc round brown
busulfan 2 mg - gx ef3 m round white
solifenacin succinate 5 mg - 150 round yellow
perindopril erbumine 8 mg - d 5 9 round white
risperidone 2 mg - 93 7241 round orange
bumetanide 0.5 mg - e 128 round green
terbinafine hydrochloride 250 mg - lamisil 250 round yellow
midodrine hydrochloride 10 mg - e 149 round
isosorbide mononitrate 10 mg - 10 ku 106 round white
levothyroxine sodium 25 ug - synthroid 25 round orange
metformin hydrochloride 500 mg - 397 round white
hydrochlorothiazide 50 mg - westward 257 round orange
dextroamphetamine saccharate 5 mgamphetamine aspartate monohydrate 5 mgdextroamphetamine sulfate 5 mgamphetamine sulfate 5 mg - 2 0 dp round orange
topiramate 50 mg - m t12 round white
bupropion hydrochloride 150 mg - e over 415 round purple
liothyronine sodium 50 ug - kpi 117 round white
baclofen 10 mg - lci 1330 round white
dexmethylphenidate hydrochloride 2.5 mg - 93 5275 round blue
amiodarone hydrochloride 200 mg - as 200 round yellow
carbidopa 10 mglevodopa 100 mg - r 538 round blue
aripiprazole 20 mg - ari 20 apo round white
metronidazole 250 mg - 93 851 round white
bicalutamide 50 mg - bcm 50 round white
prednisone 20 mg - west ward 477 round red
acetaminophen 325 mgchlorpheniramine maleate 4 mgphenylephrine hydrochloride 10 mg - xl3 forte round yellow
iloperidone 12 mg - 12 round white
losartan potassium 25 mg - 11 round white
sumatriptan succinate 25 mg - m s4 round white
cyclobenzaprine hydrochloride 10 mg - pliva 563 round yellow
losartan potassium 100 mghydrochlorothiazide 25 mg - 54 557 round yellow
glycopyrrolate 2 mg - 3181 v round white
glipizide 5 mg - 9201 teva round white
bupropion hydrochloride 100 mg - m 435 round blue
aminocaproic acid 500 mg - vp 045 round white
metformin hydrochloride 850 mg - sg 106 round white
valsartan 160 mghydrochlorothiazide 12.5 mg - m v22 round orange
labetalol hydrochloride 100 mg - watson 605 round brown
guanfacine hydrochloride 3 mg - 853 round yellow
bupropion hydrochloride 150 mg - wellbutrin xl 150 round white
losartan potassium 100 mg - sz 214 round pink
citalopram hydrobromide 10 mg - rdy 342 round brown
erythromycin stearate 250 mg - es round pink
propranolol hydrochloride 80 mg - mylan 185 80 round yellow
metolazone 5 mg - zaroxolyn 5 round blue
glycopyrrolate 2 mg - horizon 205 round white
terbinafine hydrochloride 250 1 - 209 ig round white
bupropion hydrochloride 150 mg - m bu1 round green
risperidone 0.5 mg - sz z1 round pink
carbidopa 25 mglevodopa 250 mg - r 540 round blue
simvastatin 40 mg - a 03 round pink
phenazopyridine hydrochloride 200 mg - 612 round brown
doxycycline 75 mg - lci 1535 round yellow
- 405 n round pink
terbutaline sulfate 5 mg - lci 1311 round white
ketoconazole 200 milligram in 1 tablet - ket 200 apo round white
nadolol 80 mg - 80 z 4237 round white
bisoprolol fumarate 5 mg - m 523 round purple
nifedipine 90 mg - b 90 round yellow
clonazepam 1 mg - r 34 round yellow
donepezil hydrochloride 5 mg - teva 738 round white
amlodipine besylate 5 mgvalsartan 160 mg - tv j2 round yellow
cilostazol 100 mg - m c42 round white
cilostazol 50 mg - e 123 round white
diltiazem hydrochloride 30 mg - m 23 round white
ropinirole hydrochloride 8 mg - m re8 round red
enalapril maleate 2.5 mg - t 2 round yellow
morphine sulfate 15 mg - abg 15 round blue
benazepril hydrochloride 10 mg - e 53 round orange
amiloride hydrochloride 5 mghydrochlorothiazide 50 mg - 555 483 barr round yellow
desipramine hydrochloride 25 mg - 342 round blue
paroxetine hydrochloride hemihydrate 25 mg - m p4 round purple
clonidine hydrochloride 0.2 mg - r128 round orange
glipizide 10 mg - wpi 845 round white
bisoprolol fumarate 10 mg - 93 5271 round white
- b 944 round white
amitriptyline hydrochloride 50 mg - 2103 v round brown
venlafaxine hydrochloride 50 mg - zc 66 round orange
bethanechol chloride 25 mg - pliva 325 round yellow
toremifene citrate 60 mg - to 60 round white
leflunomide 10 mg - hp 43 round white
oxycodone hydrochloride 5 mg - 4810 v round white
amitriptyline hydrochloride 75 mg - 2104 v round orange
guaifenesin 400 mg - 44 532 round blue
labetalol hydrochloride 200 mg - 4365 teva round white
risperidone 0.5 mg - m r5 round brown
meclizine hydrochloride 25 mg - 21g round pink
nadolol 20 mg - kpi 232 corgard 20 round blue
ropinirole hydrochloride 2 mg - cor 204 round pink
lovastatin 20 mg - cti 142 round white
thioridazine hydrochloride 10 mg - mp 12 round yellow
clozapine 25 mg - c 7 m round orange
propafenone hydrochloride 150 mg - gs tf5 round white
melphalan 2 mg - gx eh3 a round white
dicyclomine hydrochloride 20 mg - m d6 round blue
lithium carbonate 300 mg - 54 452 round white
enalapril maleate 20 mg - m e18 round blue
acetaminophen 300 mgcodeine phosphate 30 mg - 3 m round white
bupropion hydrochloride 200 mg - 738 round white
amitriptyline hydrochloride 100 mg - m 38 round orange
primaquine phosphate 15 mg - w p97 round pink
estradiol 1 mg - watson 487 round grey
aripiprazole 20 mg - a 010 20 round white
eletriptan hydrobromide 40 mg - rep40 pfizer round orange
dexamethasone 2 mg - 54 662 round white
digoxin 250 ug - lanoxin x3a round white
fluvoxamine maleate 100 mg - e 157 round brown
lisinopril 5 mg - m l23 round orange
propranolol hydrochloride 20 mg - mylan 183 20 round blue
thioridazine hydrochloride 50 mg - m 59 50 round orange
doxazosin mesylate 1 mg - apo 093 round white
flecainide acetate 50 mg - b 859 round white
doxycycline hyclate 100 mg - ww 112 round orange
dicyclomine hydrochloride 20 mg - lan 1282 round blue
lisinopril 20 mg - w 941 round yellow
triamterene 75 mghydrochlorothiazide 50 mg - watson 348 round yellow
ondansetron 4 mg - z4 round white
propranolol hydrochloride 60 mg - mylan pr60 60 round purple
mirtazapine 30 mg - 93 7304 round white
dronabinol 10 mg - um round orange
nystatin 500000 [usp'u] - mp 83 round brown
risperidone 3 mg - sz z5 round pink
bupropion hydrochloride 200 mg - wpi 3385 round white
lisinopril 2.5 mg - watson 405 round white
lovastatin 10 mg - 926 teva round orange
oxybutynin chloride 5 mg - m o 5 round green
- 633 round white
topiramate 50 mg - ig 279 round yellow
meperidine hydrochloride 100 mg - 382 b round white
azilsartan kamedoxomil 40 mg - asl 40 round white
lovastatin 40 mg - 635 round yellow
bethanechol chloride 5 mg - bcl 5 832 round white
alendronate sodium 70 mg - 638 round white
bupropion hydrochloride 100 mg - wellbutrin sr 100 round blue
nadolol 80 mg - sz467 round white
bupropion hydrochloride 150 mg - a 133 round yellow
- 54-639 round blue
saxagliptin hydrochloride 5 mg - 5 4215 round pink
- dp 331 round green
medroxyprogesterone acetate 10 mg - provera 10 round white
metformin hydrochloride 500 mg - i45 round white
furosemide 80 mg - lasix 80 round white
clarithromycin 250 mg - 54 271 round white
methazolamide 25 mg - eff 21 round white
levonorgestrel 90 ugethinyl estradiol 20 ug - 295 watson round white
hydrochlorothiazide 25 mg - d 27 round pink
mirtazapine 15 mg - tz 1 round white
venlafaxine hydrochloride 225 mg - os304 round white
lisinopril 40 mg - rx535 round yellow
imatinib mesylate 100 mg - nvr sa round yellow
aspirin 325 mg - t round orange
lisinopril 20 mghydrochlorothiazide 12.5 mg - lh2 m round yellow
hydrocortisone 20 mg - cortef 20 round white
oxycodone hydrochloride 5 mgacetaminophen 325 mg - endo 602 round white
atenolol 50 mgchlorthalidone 25 mg - m 63 round white
metoclopramide hydrochloride 5 mg - bl 92 round white
amlodipine besylate 2.5 mg - 2108 v round white
ropinirole hydrochloride 4 mg - 977 hh round brown
phenylephrine hydrochloride 5 mg - fr4 round pink
clonidine hydrochloride 0.2 mgchlorthalidone 15 mg - m 27 round yellow
risperidone 1 mg - m r11 round white
amoxicillin 200 mgclavulanate potassium 28.5 mg - ggn2 round pink
flavoxate hydrochloride 100 mg - e58 round white
aspirin 81 mg - l467 round orange
hydroxyzine hydrochloride 50 mg - pa 309 round white
levonorgestrel 0.15 mgethinyl estradiol 0.03 mg - tv 074 round purple
donepezil hydrochloride 5 mg - 5 aricept round white
carbamazepine 100 mg - t 100 mg round yellow
bupropion hydrochloride 150 mg - g 2444 round yellow
clozapine 25 mg - clozaril 25 round yellow
phenobarbital 64.8 mg - 5013 v round white
benztropine mesylate 2 mg - cor 145 round white
tranylcypromine sulfate 10 mg - 250 k round pink
darifenacin 15 mg - df 15 round orange
olmesartan medoxomil 20 mgamlodipine besylate 5 mghydrochlorothiazide 12.5 mg - c51 round orange
escitalopram oxalate 5 mg - f 53 round white
fenofibrate 50 mg - fh 50 round white
enalapril maleate 2.5 mg - m e15 round white
diclofenac sodium 75 mg - cti 103 round white
amitriptyline hydrochloride 50 mg - gg431 round brown
hydroxyzine hydrochloride 25 mg - m h25 round blue
cyclobenzaprine hydrochloride 5 mg - m 771 round blue
glipizide 5 mg - mylan g1 round white
alendronate sodium 5 mg - a 5 round white
mirtazapine 30 mg - tz 2 round white
glipizide 2.5 mg - gxl 2 5 round blue
oxybutynin chloride 15 mg - ku 272 round white
calcium carbonate 750 mg - as round
dextroamphetamine saccharate 1.25 mgamphetamine aspartate monohydrate 1.25 mgdextroamphetamine sulfate 1.25 mgamphetamine sulfate 1.25 mg - 5 dp round white
finasteride 1 mg - 714 round red
donepezil hydrochloride 10 mg - 10 aricept round yellow
- tolinase 100 round white
nisoldipine 25.5 mg - m ne 25 round orange
desipramine hydrochloride 10 mg - e 29 round white
- 428 round orange
amitriptyline hydrochloride 50 mg - m 36 round brown
metformin hydrochloride 500 mg - e 213 round white
prednisone 5 mg - dan dan 5052 round white
donepezil hydrochloride 10 mg - x 12 round yellow
quetiapine fumarate 100 mg - seroquel 100 round yellow
ciprofloxacin hydrochloride 250 mg - p 250 round white
diclofenac potassium 50 mg - gg977 round white
amiloride hydrochloride anhydrous 5 mg - par 117 round yellow
escitalopram oxalate 20 mg - 251 ig round white
famotidine 20 mg - m f1 round yellow
lamotrigine 150 mg - l123 round white
lorazepam 0.5 mg - 240 0 5 watson round white
timolol maleate 10 mg - m 221 round green
bupropion hydrochloride 300 mg - wpi 3332 round white
fexofenadine hydrochloride 180 mg - 93 7253 round orange
flavoxate hydrochloride 100 mg - g 181 round white
bupropion hydrochloride 100 mg - 736 round white
metoprolol tartrate 25 mg - c 73 round white
naproxen sodium 220 mg - 220 round blue
atenolol 50 mg - 93 752 teva round white
oxybutynin chloride 10 mg - ku 271 round white
tiagabine hydrochloride 4 mg - c 404 round yellow
hydralazine hydrochloride 25 mg - pliva 327 round orange
famotidine 40 mg - cti 122 round white
norethindrone 1 mgethinyl estradiol 0.035 mg - b 342 round white
carbamazepine 200 mg - 109 teva round white
- dan 5552 round white
amantadine hydrochloride 100 mg - 832 amt round orange
lovastatin 40 mg - 40 round orange
clopidogrel bisulfate 75 mg - r 196 round white
glipizide 10 mg - apo glp 10 round white
pioglitazone hydrochloride 30 mg - teva 7272 round white
prochlorperazine maleate 5 mg - gg952 5 round yellow
rifaximin 200 mg - sx round pink
labetalol hydrochloride 300 mg - e118 round white
sertraline hydrochloride 25 mg - s 21 round white
flecainide acetate 100 mg - 54070 round white
chlorothiazide 250 mg - westward 209 round white
atenolol 100 mgchlorthalidone 25 mg - tenoretic 117 round white
diltiazem hydrochloride 30 mg - marion 1771 round green
acamprosate calcium 333 mg - 435 round white
escitalopram oxalate 20 mg - ig 251 round white
bupropion hydrochloride 200 mg - a161 round red
escitalopram oxalate 5 mg - ig 249 round white
prasugrel hydrochloride 5 mg - s77 round pink
bupropion hydrochloride 300 mg - a102 round white
hyoscyamine sulfate 0.125 mg - 644 round white
venlafaxine hydrochloride 37.5 mg - y02 round pink
escitalopram oxalate 10 mg - 5851 10 round white
levothyroxine sodium 0.175 mg - jsp 563 round purple
metoclopramide hydrochloride 5 mg - tv 2204 round white
acetaminophen 500 mg - fr1 round white
hyoscyamine sulfate 0.12 mgsodium phosphate, monobasic, monohydrate 40.8 mgphenyl salicylate 36.2 mgmethenamine 81.6 mgmethylene blue 10.8 mg - 293 round purple
chlorpheniramine maleate 4 mgphenylephrine hydrochloride 10 mg - 44 525 round white
demeclocycline hydrochloride 300 mg - an 55 round red
calcium acetate 667 mg - cyp910 round white
naltrexone hydrochloride 50 mg - b 50 902 round white
hydralazine hydrochloride 50 mg - pliva 328 round orange
promethazine hydrochloride 25 mg - z c 0 2 round white
pioglitazone hydrochloride 30 mgmetformin hydrochloride 1000 mg - 4833x 30 1000 round white
meprobamate 400 mg - 591 a round white
adefovir dipivoxil 10 mg - gilead 10 round white
propranolol hydrochloride 80 mg - pliva 471 round yellow
clonazepam 2 mg - 834 teva round white
fluphenazine hydrochloride 10 mg - gg490 round brown
indapamide 1.25 mg - m 69 round pink
diclofenac sodium 100 mg - gg 904 round pink
metformin hydrochloride 1000 mg - g 45 1000 round white
benztropine mesylate 2 mg - 2327 v round white
eszopiclone 3 mg - s193 round blue
trospium chloride 20 mg - l 1 round yellow
midodrine hydrochloride 10 mg - mh 3 m round white
captopril 25 mg - ww 172 round white
meperidine hydrochloride 50 mg - 381 b round white
nifedipine 30 mg - ku 260 round pink
chloroquine phosphate 500 mg - cn500 round white
venlafaxine hydrochloride 100 mg - y05 round pink
acetaminophen 300 mgcodeine phosphate 60 mg - 4 93 350 round white
risedronate sodium 150 mg - apo ris 150 round blue
lamotrigine 200 mg - lamictal 200 round white
glipizide 5 mg - wpi 844 round orange
olanzapine 5 mg - apo ola 5 round white
cyproheptadine hydrochloride 4 mg - par 043 round white
nifedipine 60 mg - eln 60 round brown
carvedilol 3.125 mg - g round white
ibuprofen 200 1 - ibu 200 round brown
bethanechol chloride 10 mg - an 572 round white
levonorgestrel 0.15 mgethinyl estradiol 0.025 mg - tv 075 round pink
naproxen sodium 275 mg - nps 275 round blue
fosinopril sodium 10 mghydrochlorothiazide 12.5 mg - i 3 round white
levothyroxine sodium 125 ug - synthroid 125 round brown
metoclopramide hydrochloride 5 mg - wpi 2228 round green
sumatriptan succinate 50 mg - sa 50 round white
venlafaxine hydrochloride 25 mg - 9 3 199 round orange
terbinafine hydrochloride 250 mg - c134 round white
acetazolamide 250 mg - lan 1050 round white
exemestane 25 mg - 2858 round white
anastrozole 1 mg - m 34 round white
desloratadine 5 mg - m d17 round red
olmesartan medoxomil 40 mgamlodipine besylate 10 mghydrochlorothiazide 12.5 mg - c55 round red
demeclocycline hydrochloride 150 mg - c 115 round pink
letrozole 2.5 mg - 54 753 round white
sumatriptan succinate 50 mg - m s7 round white
repaglinide 2 mg - 747 c round pink
prochlorperazine maleate 5 mg - 93 9643 round yellow
folic acid 1 mg - 3162 v round yellow
midodrine hydrochloride 10 mg - us 10 213 round purple
felodipine 2.5 mg - mp 771 round green
ropinirole hydrochloride 12 mg - m re12 round green
hydroxyzine hydrochloride 10 mg - 3615 v round orange
labetalol hydrochloride 200 mg - watson 606 round white
- b 143 round white
paroxetine hydrochloride hemihydrate 12.5 mg - m p3 round white
albuterol sulfate 2 mg - mp 47 round white
donepezil hydrochloride 10 mg - zf 15 round white
imipramine hydrochloride 10 mg - mp 4 round yellow
timolol maleate 5 mg - m 55 round green
amlodipine besylate 10 mg - z 5 round white
anastrozole 1 mg - teva a10 round white
morphine sulfate 30 mg - abg 30 round purple
bupropion hydrochloride 100 mg - wpi 858 round white
medroxyprogesterone acetate 5 mg - 555 873 b round white
furosemide 20 mg - 54 840 round white
hydroxyzine hydrochloride 10 mg - a 75 round white
hydroxychloroquine sulfate 200 mg - ww28 round white
hydroxyzine hydrochloride 10 mg - k 10 round white
captopril 100 mg - m c4 round white
morphine sulfate 15 mg - e652 15 round blue
dicyclomine hydrochloride 20 mg - ww 27 round blue
trihexyphenidyl hydrochloride 5 mg - dan dan 5337 round white
nifedipine 90 mg - 90 adalat cc round pink
orphenadrine citrate 100 mg - nl4 round white
desogestrel 0.15 mgethinyl estradiol 0.025 mg - b 335 round pink
amlodipine besylate 10 mgolmesartan medoxomil 40 mg - c77 round red
pilocarpine hydrochloride 7.5 mg - lci 1407 round blue
nifedipine 30 mg - m ne 30 round white
amlodipine besylate 5 mg - 2109 v round white
progesterone 100 mg - ak round pink
oxybutynin chloride 5 mg - 4853 v round blue
amlodipine besylate 2.5 mg - 237 ig round white
lovastatin 60 mg - 60 round orange
pravastatin sodium 40 mg - apo pra 40 round green
promethazine hydrochloride 50 mg - gg 235 round pink
hydrochlorothiazide 25 mg - lci 1413 round orange
diclofenac sodium 50 mg - gg738 round brown
amitriptyline hydrochloride 25 mg - gg44 round green
zafirlukast 10 mg - r 625 round pink
clonidine hydrochloride 0.2 mg - mp 658 round white
acarbose 25 mg - p210 25 round white
- deltasone 2.5 round pink
lisinopril 20 mghydrochlorothiazide 12.5 mg - rx537 round yellow
desipramine hydrochloride 50 mg - norpramin 50 round green
diclofenac sodium 75 mg - r 551 round white
drospirenone 3 mgethinyl estradiol 0.03 mg - do round yellow
nitroglycerin 0.6 mg - n 6 round white
nitroglycerin 0.4 mg - n 4 round white
nitroglycerin 0.3 mg - n 3 round white
Go PRO for all pill images
MARCH 200431090110105
 Rx only
Description
0.5/0.035 mg, 0.75/0.035 mg, and 1/0.035 mg
(21 Day Regimen) and (28 Day Regimen)
Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
COMBINATION ORAL CONTRACEPTIVES:
Each of the following products is a combination oral contraceptive containing the progestational compound norethindrone and the estrogenic compound ethinyl estradiol:
Nortrel™ 7/7/7 (norethindrone and ethinyl estradiol tablets, USP 0.5/0.035 mg, 0.75/0.035 mg, and 1/0.035 mg) (21 Day Regimen and 28 Day Regimen): Each light yellow tablet contains 0.5 mg of norethindrone and 0.035 mg of ethinyl estradiol and the inactive ingredients include D&C yellow #10, lactose monohydrate, magnesium stearate and pregelatinized starch. Each blue tablet contains 0.75 mg of norethindrone and 0.035 mg of ethinyl estradiol and the inactive ingredients include FD&C blue no. 1 (aluminum lake), lactose monohydrate, magnesium stearate and pregelatinized starch. Each peach tablet contains 1 mg of norethindrone and 0.035 mg of ethinyl estradiol and the inactive ingredients include FD&C yellow no. 6 (aluminum lake), lactose monohydrate, magnesium stearate and pregelatinized starch. Each white tablet in the (28) package contains only inert ingredients as follows: lactose monohydrate, magnesium stearate, and pregelatinized starch.
The chemical name for norethindrone is 17-hydroxy-19-nor-17α-pregn-4-en-20-yn-3-one, for ethinyl estradiol is 19-nor-17α -pregna-1,3,5(10)-trien-20-yne-3, 17-diol.
The structural formulas are as follows:
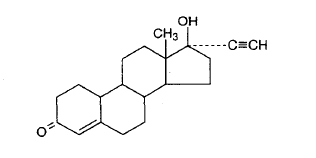
Norethindrone C20H26O2 Molecular Weight: 298.43 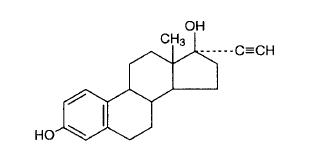
Ethinyl Estradiol C20H24O2 Molecular Weight: 296.41
Clinical Pharmacology
COMBINATION ORAL CONTRACEPTIVES
Combination oral contraceptives act by suppression of gonadotropins. Although the primary mechanism of this action is inhibition of ovulation, other alterations include changes in the cervical mucus (which increase the difficulty of sperm entry into the uterus) and the endometrium (which reduce the likelihood of implantation).
Indications And Usage
Nortrel™ 7/7/7 (norethindrone and ethinyl estradiol tablets, USP 0.5/0.035 mg, 0.75/0.035 mg, and 1/0.035 mg) (21 Day Regimen and 28 Day Regimen) are indicated for the prevention of pregnancy in women who elect to use this product as a method of contraception.
Oral contraceptives are highly effective. Table I uls the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.
TABLE I: PERCENTAGE OF WOMEN EXPERIENCING AN UNINTENDED PREGNANCY DURING THE FIRST YEAR OF TYPICAL USE AND THE FIRST YEAR OF PERFECT USE OF CONTRACEPTION AND THE PERCENTAGE CONTINUING USE AT THE END OF THE FIRST YEAR. UNITED STATES Adapted from Hatcher et al., 1998 Ref. #1. % of Women Experiencing an Unintended Pregnancy within the First Year of Use % of Women Continuing Use at One YearÂ
Method
(1)
Typical Use
(2)
Perfect Use
(3)(4) Chance 85 85 Spermicides 26 6 40 Periodic abstinence 25 63 Calendar 9 Ovulation Method 3 Sympto-Thermal 2 Post-Ovulation 1 Withdrawal 19 4 Cap  With spermicidal cream or jelly. Parous Women 40 26 42 Nulliparous Women 20 9 56 Sponge Parous Women 40 20 42 Nulliparous Women 20 9 56 Diaphragm  20 6 56 Condom Female (Reality) 21 5 56 Male 14 3 61 Pill 5 71 Progestin Only 0.5 Combined 0.1 IUD Progesterone T 2.0 1.5 81 Copper T380A 0.8 0.6 78 LNg 20 0.1 0.1 81 Depo-Provera 0.3 0.3 70 Norplant and Norplant-2 0.05 0.05 88 Female Sterilization 0.5 0.5 100 Male Sterilization 0.15 0.10 100
Contraindications
Oral contraceptives should not be used in women who currently have the following conditions:
- Thrombophlebitis or thromboembolic disorders
- A past history of deep vein thrombophlebitis or thromboembolic disorders
- Cerebral vascular or coronary artery disease
- Known or suspected carcinoma of the breast
- Carcinoma of the endometrium or other known or suspected estrogen-dependent neoplasia
- Undiagnosed abnormal genital bleeding
- Cholestatic jaundice of pregnancy or jaundice with prior pill use
- Hepatic adenomas or carcinomas
- Known or suspected pregnancy
Warnings
Boxed Warning section
Cigarette smoking increases the risk of serious cardiovascular side effects from oral contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should be strongly advised not to smoke.
The use of oral contraceptives is associated with increased risks of several serious conditions including myocardial infarction, thromboembolism, stroke, hepatic neoplasia, and gallbladder disease, although the risk of serious morbidity or mortality is very small in healthy women without underlying risk factors. The risk of morbidity and mortality increases significantly in the presence of other underlying risk factors such as hypertension, hyperlipidemias, obesity and diabetes.
Practitioners prescribing oral contraceptives should be familiar with the following information relating to these risks.
The information contained in this package insert is principally based on studies carried out in patients who used oral contraceptives with higher formulations of estrogens and progestogens than those in common use today. The effect of long-term use of the oral contraceptives with lower formulations of both estrogens and progestogens remains to be determined.
Throughout this labeling, epidemiological studies reported are of two types: retrospective or case control studies and prospective or cohort studies. Case control studies provide a measure of the relative risk of a disease, namely, a ratio of the incidence of a disease among oral contraceptive users to that among nonusers. The relative risk does not provide information on the actual clinical occurrence of a disease. Cohort studies provide a measure of attributable risk, which is the difference in the incidence of disease between oral contraceptive users and nonusers. The attributable risk does provide information about the actual occurrence of a disease in the population (adapted from refs. 2 and 3 with the author's permission). For further information, the reader is referred to a text on epidemiological methods.
1. Thromboembolic disorders and other vascular problems
a. Myocardial Infarction
An increased risk of myocardial infarction has been attributed to oral contraceptive use. This risk is primarily in smokers or women with other underlying risk factors for coronary artery disease such as hypertension, hypercholesterolemia, morbid obesity, and diabetes. The relative risk of heart attack for current oral contraceptive users has been estimated to be two to six.4-10 The risk is very low under the age of 30.
Smoking in combination with oral contraceptive use has been shown to contribute substantially to the incidence of myocardial infarctions in women in their mid-thirties or older with smoking accounting for the majority of excess cases.11 Mortality rates associated with circulatory disease have been shown to increase substantially in smokers, especially in those 35 years of age and older among women who use oral contraceptives.
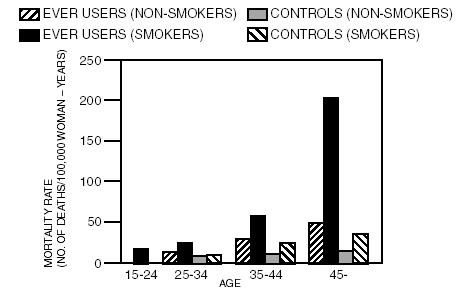
TABLE II: CIRCULATORY DISEASE MORTALITY RATES PER 100,000 WOMAN-YEARS BY AGE, SMOKING STATUS AND ORAL CONTRACEPTIVE USE (Adapted from P.M. Layde and V. Beral, ref. #12.)
Oral contraceptives may compound the effects of well-known risk factors, such as hypertension, diabetes, hyperlipidemias, age and obesity.13 In particular, some progestogens are known to decrease HDL cholesterol and cause glucose intolerance, while estrogens may create a state of hyperinsulinism.14-18 Oral contraceptives have been shown to increase blood pressure among users (see section 9 in WARNINGS). Similar effects on risk factors have been associated with an increased risk of heart disease. Oral contraceptives must be used with caution in women with cardiovascular disease risk factors.
b. Thromboembolism
An increased risk of thromboembolic and thrombotic disease associated with the use of oral contraceptives is well established. Case control studies have found the relative risk of users compared to nonusers to be 3 for the first episode of superficial venous thrombosis, 4 to 11 for deep vein thrombosis or pulmonary embolism, and 1.5 to 6 for women with predisposing conditions for venous thromboembolic disease.2,3,19-24 Cohort studies have shown the relative risk to be somewhat lower, about 3 for new cases and about 4.5 for new cases requiring hospitalization.25 The risk of thromboembolic disease associated with oral contraceptives is not related to length of use and disappears after pill use is stopped.2
A two- to four-fold increase in relative risk of post-operative thromboembolic complications has been reported with the use of oral contraceptives.9 The relative risk of venous thrombosis in women who have predisposing conditions is twice that of women without such medical conditions.26 If feasible, oral contraceptives should be discontinued at least four weeks prior to and for two weeks after elective surgery of a type associated with an increase in risk of thromboembolism and during and following prolonged immobilization. Since the immediate postpartum period is also associated with an increased risk of thromboembolism, oral contraceptives should be started no earlier than four weeks after delivery in women who elect not to breast feed or four weeks after a second trimester abortion.
c. Cerebrovascular diseases
Oral contraceptives have been shown to increase both the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes), although, in general, the risk is greatest among older (>35 years), hypertensive women who also smoke. Hypertension was found to be a risk factor for both users and nonusers, for both types of strokes, and smoking interacted to increase the risk of stroke.27-29
In a large study, the relative risk of thrombotic strokes has been shown to range from 3 for normotensive users to 14 for users with severe hypertension.30 The relative risk of hemorrhagic stroke is reported to be 1.2 for non-smokers who used oral contraceptives, 2.6 for smokers who did not use oral contraceptives, 7.6 for smokers who used oral contraceptives, 1.8 for normotensive users and 25.7 for users with severe hypertension.30 The attributable risk is also greater in older women.3
d. Dose-related risk of vascular disease from oral contraceptives
A positive association has been observed between the amount of estrogen and progestogen in oral contraceptives and the risk of vascular disease.31-33 A decline in serum high density lipoproteins (HDL) has been reported with many progestational agents.14-16 A decline in serum high density lipoproteins has been associated with an increased incidence of ischemic heart disease. Because estrogens increase HDL cholesterol, the net effect of an oral contraceptive depends on a balance achieved between doses of estrogen and progestogen and the activity of the progestogen used in the contraceptive. The activity and amount of both hormones should be considered in the choice of an oral contraceptive.
Minimizing exposure to estrogen and progestogen is in keeping with good principles of therapeutics. For any particular estrogen/progestogen combination, the dosage regimen prescribed should be one which contains the least amount of estrogen and progestogen that is compatible with a low failure rate and the needs of the individual patient. New acceptors of oral contraceptive agents should be started on preparations containing 0.035 mg or less of estrogen.
e. Persistence of risk of vascular disease
There are two studies which have shown persistence of risk of vascular disease for ever-users of oral contraceptives. In a study in the United States, the risk of developing myocardial infarction after discontinuing oral contraceptives persists for at least 9 years for women 40-49 years who had used oral contraceptives for five or more years, but this increased risk was not demonstrated in other age groups.8 In another study in Great Britain, the risk of developing cerebrovascular disease persisted for at least 6 years after discontinuation of oral contraceptives, although excess risk was very small.34 However, both studies were performed with oral contraceptive formulations containing 50 micrograms or higher of estrogens.
2. Estimates of mortality from contraceptive use
One study gathered data from a variety of sources which have estimated the mortality rate associated with different methods of contraception at different ages (Table III). These estimates include the combined risk of death associated with contraceptive methods plus the risk attributable to pregnancy in the event of method failure. Each method of contraception has its specific benefits and risks. The study concluded that with the exception of oral contraceptive users 35 and older who smoke, and 40 and older who do not smoke, mortality associated with all methods of birth control is low and below that associated with childbirth. The observation of an increase in risk of mortality with age for oral contraceptive users is based on data gathered in the 1970's.35 Current clinical recommendation involves the use of lower estrogen dose formulations and a careful consideration of risk factors. In 1989, the Fertility and Maternal Health Drugs Advisory Committee was asked to review the use of oral contraceptives in women 40 years of age and over. The Committee concluded that although cardiovascular disease risks may be increased with oral contraceptive use after age 40 in healthy non-smoking women (even with the newer low-dose formulations), there are also greater potential health risks associated with pregnancy in older women and with the alternative surgical and medical procedures which may be necessary if such women do not have access to effective and acceptable means of contraception. The Committee recommended that the benefits of low-dose oral contraceptive use by healthy non-smoking women over 40 may outweigh the possible risks.
Of course, older women, as all women who take oral contraceptives, should take an oral contraceptive which contains the least amount of estrogen and progestogen that is compatible with a low failure rate and individual patient needs.
TABLE III: ANNUAL NUMBER OF BIRTH-RELATED OR METHOD-RELATED DEATHS ASSOCIATED WITH CONTROL OF FERTILITY PER 100,000 NONSTERILE WOMEN, BY FERTILITY CONTROL METHOD ACCORDING TO AGE Adapted from H.W. Ory, ref. #35. Method of control and outcome 15-19 20-24 25-29 30-34 35-39 40-44 No fertility control methods Deaths are birth-related 7.0 7.4 9.1 14.8 25.7 28.2 Oral contraceptives non-smoker Deaths are method-related 0.3 0.5 0.9 1.9 13.8 31.6 Oral contraceptives smoker 2.2 3.4 6.6 13.5 51.1 117.2 IUD 0.8 0.8 1.0 1.0 1.4 1.4 Condom 1.1 1.6 0.7 0.2 0.3 0.4 Diaphragm/spermicide 1.9 1.2 1.2 1.3 2.2 2.8 Periodic abstinence 2.5 1.6 1.6 1.7 2.9 3.6 3. Carcinoma of the reproductive organs and breasts
Numerous epidemiological studies have been performed on the incidence of breast, endometrial, ovarian and cervical cancer in women using oral contraceptives. While there are conflicting reports, most studies suggest that use of oral contraceptives is not associated with an overall increase in the risk of developing breast cancer. Some studies have reported an increased relative risk of developing breast cancer particularly at a younger age. This increased relative risk has been reported to be related to duration of use. 36-44, 79-89
A meta-analysis of 54 studies reports that women who are currently using combined oral contraceptives or have used them in the past 10 years are at a slightly increased risk of having breast cancer diagnosed although the additional cancers tend to be localized to the breast. There is no evidence of an increased risk of having breast cancer diagnosed 10 or more years after cessation of use.90
Some studies suggest that oral contraceptive use has been associated with an increase in the risk of cervical intraepithelial neoplasia in some populations of women.45-48 However, there continues to be controversy about the extent to which such findings may be due to differences in sexual behavior and other factors.
4. Hepatic neoplasia
Benign hepatic adenomas are associated with oral contraceptive use, although the incidence of benign tumors is rare in the United States. Indirect calculations have estimated the attributable risk to be in the range of 3.3 cases/100,000 for users, a risk that increases after four or more years of use especially with oral contraceptives of higher dose.49 Rupture of benign, hepatic adenomas may cause death through intra-abdominal hemorrhage.50, 51
Studies have shown an increased risk of developing hepatocellular carcinoma 52-54, 91 in oral contraceptive users. However, these cancers are rare in the U.S.
5. Ocular lesions
There have been clinical case reports of retinal thrombosis associated with the use of oral contraceptives. Oral contraceptives should be discontinued if there is unexplained partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or retinal vascular lesions. Appropriate diagnostic and therapeutic measures should be undertaken immediately.
6. Oral contraceptive use before or during early pregnancy
Extensive epidemiological studies have revealed no increased risk of birth defects in women who have used oral contraceptives prior to pregnancy.56,57 The majority of recent studies also do not indicate a teratogenic effect, particularly in so far as cardiac anomalies and limb reduction defects are concerned, 55,56,58,59 when taken inadvertently during early pregnancy.
The administration of oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion.
It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out before continuing oral contraceptive use. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period. Oral contraceptive use should be discontinued until pregnancy is ruled out.
7. Gallbladder disease
Earlier studies have reported an increased lifetime relative risk of gallbladder surgery in users of oral contraceptives and estrogens.60,61 More recent studies, however, have shown that the relative risk of developing gallbladder disease among oral contraceptive users may be minimal.62-64 The recent findings of minimal risk may be related to the use of oral contraceptive formulations containing lower hormonal doses of estrogens and progestogens.
8. Carbohydrate and lipid metabolic effects
Oral contraceptives have been shown to cause a decrease in glucose tolerance in a significant percentage of users.17 This effect has been shown to be directly related to estrogen dose.65 Progestogens increase insulin secretion and create insulin resistance, this effect varying with different progestational agents.17,66 However, in the non-diabetic woman, oral contraceptives appear to have no effect on fasting blood glucose.67 Because of these demonstrated effects, prediabetic and diabetic women in particular should be carefully monitored while taking oral contraceptives.
A small proportion of women will have persistent hypertriglyceridemia while on the pill. As discussed earlier (see WARNINGS 1a and 1d), changes in serum triglycerides and lipoprotein levels have been reported in oral contraceptive users.
9. Elevated blood pressure
An increase in blood pressure has been reported in women taking oral contraceptives68 and this increase is more likely in older oral contraceptive users69 and with extended duration of use.61 Data from the Royal College of General Practitioners12 and subsequent randomized trials have shown that the incidence of hypertension increases with increasing progestational activity.
Women with a history of hypertension or hypertension-related diseases, or renal disease70 should be encouraged to use another method of contraception. If women elect to use oral contraceptives, they should be monitored closely and if significant elevation of blood pressure occurs, oral contraceptives should be discontinued. For most women, elevated blood pressure will return to normal after stopping oral contraceptives, and there is no difference in the occurrence of hypertension between former and never users.68-71
10. Headache
The onset or exacerbation of migraine or development of headache with a new pattern which is recurrent, persistent or severe requires discontinuation of oral contraceptives and evaluation of the cause.
11. Bleeding irregularities
Breakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. Nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If pathology has been excluded, time or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out.
Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was preexistent.
12. Ectopic pregnancy
Ectopic as well as intrauterine pregnancy may occur in contraceptive failures.
Precautions
1. Physical examination and follow-up
It is good medical practice for all women to have annual history and physical examinations, including women using oral contraceptives. The physical examination, however, may be deferred until after initiation of oral contraceptives if requested by the woman and judged appropriate by the clinician. The physical examination should include special reference to blood pressure, breasts, abdomen and pelvic organs, including cervical cytology, and relevant laboratory tests. In case of undiagnosed, persistent or recurrent abnormal vaginal bleeding, appropriate measures should be conducted to rule out malignancy. Women with a strong family history of breast cancer or who have breast nodules should be monitored with particular care.
2. Lipid disorders
Women who are being treated for hyperlipidemias should be followed closely if they elect to use oral contraceptives. Some progestogens may elevate LDL levels and may render the control of hyperlipidemias more difficult.
3. Liver function
If jaundice develops in any woman receiving such drugs, the medication should be discontinued. Steroid hormones may be poorly metabolized in patients with impaired liver function.
4. Fluid retention
Oral contraceptives may cause some degree of fluid retention. They should be prescribed with caution, and only with careful monitoring, in patients with conditions which might be aggravated by fluid retention.
5. Emotional disorders
Women with a history of depression should be carefully observed and the drug discontinued if depression recurs to a serious degree.
6. Contact lenses
Contact lens wearers who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.
7. Drug interactions
Reduced efficacy and increased incidence of breakthrough bleeding and menstrual irregularities have been associated with concomitant use of rifampin. A similar association, though less marked, has been suggested with barbiturates, phenylbutazone, phenytoin sodium, carbamazepine, and possibly with griseofulvin, ampicillin and tetracyclines.72
8. Interactions with laboratory tests
Certain endocrine and liver function tests and blood components may be affected by oral contraceptives:
 a. Increased prothrombin and factors VII, VIII, IX, and X; decreased antithrombin 3; increased norepinephrine-induced platelet aggregability. b. Increased thyroid binding globulin (TBG) leading to increased circulating total thyroid hormone, as measured by protein-bound iodine (PBI), T4 by column or by radioimmunoassay. Free T3 resin uptake is decreased, reflecting the elevated TBG, free T4 concentration is unaltered. c. Other binding proteins may be elevated in serum. d. Sex-binding globulins are increased and result in elevated levels of total circulating sex steroids and corticoids; however, free or biologically active levels remain unchanged. e. Triglycerides may be increased. f. Glucose tolerance may be decreased. g. Serum folate levels may be depressed by oral contraceptive therapy. This may be of clinical significance if a woman becomes pregnant shortly after discontinuing oral contraceptives.9. Carcinogenesis
See WARNINGS section.
10. Pregnancy
Pregnancy Category X. See CONTRAINDICATIONS and WARNINGS sections.
11. Nursing Mothers
Small amounts of oral contraceptive steroids have been identified in the milk of nursing mothers and a few adverse effects on the child have been reported, including jaundice and breast enlargement. In addition, combination oral contraceptives given in the postpartum period may interfere with lactation by decreasing the quantity and quality of breast milk. If possible, the nursing mother should be advised not to use combination oral contraceptives but to use other forms of contraception until she has completely weaned her child.
12. Pediatric Use
Safety and efficacy of norethindrone and ethinyl estradiol tablets has been established in women of reproductive age. Safety and efficacy are expected to be the same for postpubertal adolescents under the age of 16 years and for users 16 years and older. Use of this product before menarche is not indicated.
13. Sexually transmitted diseases
Patients should be counseled that this product does not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Information For The Patient
See Patient Labeling printed below
Adverse Reactions
An increased risk of the following serious adverse reactions has been associated with the use of oral contraceptives (see WARNINGS section).
- Thrombophlebitis and venous thrombosis with or without embolism
- Arterial thromboembolism
- Pulmonary embolism
- Myocardial infarction
- Cerebral hemorrhage
- Cerebral thrombosis
- Hypertension
- Gallbladder disease
- Hepatic adenomas or benign liver tumors
The following adverse reactions have been reported in patients receiving oral contraceptives and are believed to be drug-related:
- Nausea
- Vomiting
- Gastrointestinal symptoms (such as abdominal cramps and bloating)
- Breakthrough bleeding
- Spotting
- Change in menstrual flow
- Amenorrhea
- Temporary infertility after discontinuation of treatment
- Edema
- Melasma which may persist
- Breast changes: tenderness, enlargement, secretion
- Change in weight (increase or decrease)
- Change in cervical erosion and secretion
- Diminution in lactation when given immediately postpartum
- Cholestatic jaundice
- Migraine
- Rash (allergic)
- Mental depression
- Reduced tolerance to carbohydrates
- Vaginal candidiasis
- Change in corneal curvature (steepening)
- Intolerance to contact lenses
The following adverse reactions have been reported in users of oral contraceptives and the association has been neither confirmed nor refuted:
- Pre-menstrual syndrome
- Cataracts
- Changes in appetite
- Cystitis-like syndrome
- Headache
- Nervousness
- Dizziness
- Hirsutism
- Loss of scalp hair
- Erythema multiforme
- Erythema nodosum
- Hemorrhagic eruption
- Vaginitis
- Porphyria
- Impaired renal function
- Hemolytic uremic syndrome
- Acne
- Changes in libido
- Colitis
- Budd-Chiari Syndrome
Overdosage
Serious ill effects have not been reported following acute ingestion of large doses of oral contraceptives by young children. Overdosage may cause nausea, and withdrawal bleeding may occur in females.
Non-contraceptive Health Benefits
The following non-contraceptive health benefits related to the use of combination oral contraceptives are supported by epidemiological studies which largely utilized oral contraceptive formulations containing estrogen doses exceeding 0.035 mg of ethinyl estradiol or 0.05 mg mestranol.73-78
Effects on menses:
- increased menstrual cycle regularity
- decreased blood loss and decreased incidence of iron deficiency anemia
- decreased incidence of dysmenorrhea
Effects related to inhibition of ovulation:
- decreased incidence of functional ovarian cysts
- decreased incidence of ectopic pregnancies
Other effects:
- decreased incidence of fibroadenomas and fibrocystic disease of the breast
- decreased incidence of acute pelvic inflammatory disease
- decreased incidence of endometrial cancer
- decreased incidence of ovarian cancer
Dosage And Administration
To achieve maximum contraceptive effectiveness, Nortrel 7/7/7 tablets must be taken exactly as directed and at intervals not exceeding 24 hours. Nortrel 7/7/7 tablets are available in the Buler Pack Tablet Dispenser which is preset for a Sunday Start. Day 1 Start is also available.
21-Day Regimen (Sunday Start):
When taking Nortrel 7/7/7 the first tablet should be taken on the first Sunday after menstruation begins. If period begins on Sunday, the first tablet is taken on that day. One tablet is taken daily for 21 days. For subsequent cycles, no tablets are taken for 7 days, then a tablet is taken the next day (Sunday). For the first cycle of a Sunday Start regimen, another method of contraception should be used until after the first 7 consecutive days of administration.
If the patient misses one (1) active tablet in Weeks 1, 2, or 3, the tablet should be taken as soon as she remembers. If the patient misses two (2) active tablets in Week 1 or Week 2, the patient should take two (2) tablets the day she remembers and two (2) tablets the next day; and then continue taking one (1) tablet a day until she finishes the pack. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills. If the patient misses two (2) active tablets in the third week or misses three (3) or more active tablets in a row, the patient should continue taking one tablet every day until Sunday. On Sunday the patient should throw out the rest of the pack and start a new pack that same day. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills.
Complete instructions to facilitate patient counseling on proper pill usage may be found in the Detailed Patient Labeling (“HOW TO TAKE THE PILL” section).
21-Day Regimen (Day 1 Start):
The dosage of Nortrel 7/7/7 for the initial cycle of therapy is one tablet administered daily from the 1st day through the 21st day of the menstrual cycle, counting the first day of menstrual flow as “Day 1.” For subsequent cycles, no tablets are taken for 7 days, then a new course is started of one tablet a day for 21 days. The dosage regimen then continues with 7 days of no medication, followed by 21 days of medication, instituting a three-weeks-on, one-week-off dosage regimen.
If the patient misses one (1) active tablet in Weeks 1, 2, or 3, the tablet should be taken as soon as she remembers. If the patient misses two (2) active tablets in Week 1 or Week 2, the patient should take two (2) tablets the day she remembers and two (2) tablets the next day; and then continue taking one (1) tablet a day until she finishes the pack. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills. If the patient misses two (2) active tablets in the third week or misses three (3) or more active tablets in a row, the patient should throw out the rest of the pack and start a new pack that same day. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills.
Complete instructions to facilitate patient counseling on proper pill usage may be found in the Detailed Patient Labeling (“HOW TO TAKE THE PILL” section).
28-Day Regimen (Sunday Start):
When taking Nortrel 7/7/7 the first tablet should be taken on the first Sunday after menstruation begins. If period begins on Sunday, the first tablet should be taken that day. Take one active tablet daily for 21 days followed by one white placebo tablet daily for 7 days. After 28 tablets have been taken, a new course is started the next day (Sunday). For the first cycle of a Sunday Start regimen, another method of contraception should be used until after the first 7 consecutive days of administration.
If the patient misses one (1) active tablet in Weeks 1, 2, or 3, the tablet should be taken as soon as she remembers. If the patient misses two (2) active tablets in Week 1 or Week 2, the patient should take two (2) tablets the day she remembers and two (2) tablets the next day; and then continue taking one (1) tablet a day until she finishes the pack. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills. If the patient misses two (2) active tablets in the third week or misses three (3) or more active tablets in a row, the patient should continue taking one tablet every day until Sunday. On Sunday the patient should throw out the rest of the pack and start a new pack that same day. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills.
Complete instructions to facilitate patient counseling on proper pill usage may be found in the Detailed Patient Labeling (“HOW TO TAKE THE PILL” section).
28-Day Regimen (Day 1 Start):
The dosage of Nortrel 7/7/7, for the initial cycle of therapy is one active tablet administered daily from the 1st through the 21st day of the menstrual cycle, counting the first day of menstrual flow as “Day 1” followed by one white tablet daily for 7 days. Tablets are taken without interruption for 28 days. After 28 tablets have been taken, a new course is started the next day.
If the patient misses one (1) active tablet in Weeks 1, 2, or 3, the tablet should be taken as soon as she remembers. If the patient misses two (2) active tablets in Week 1 or Week 2, the patient should take two (2) tablets the day she remembers and two (2) tablets the next day; and then continue taking one (1) tablet a day until she finishes the pack. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills. If the patient misses two (2) active tablets in the third week or misses three (3) or more active tablets in a row, the patient should throw out the rest of the pack and start a new pack that same day. The patient should be instructed to use a back-up method of birth control if she has sex in the seven (7) days after missing pills.
Complete instructions to facilitate patient counseling on proper pill usage may be found in the Detailed Patient Labeling (“HOW TO TAKE THE PILL” section).
The use of Nortrel 7/7/7 for contraception may be initiated 4 weeks postpartum in women who elect not to breast feed. When the tablets are administered during the postpartum period, the increased risk of thromboembolic disease associated with the postpartum period must be considered. (See CONTRAINDICATIONS and WARNINGS concerning thromboembolic disease. See also PRECAUTIONS for “ Nursing mothers .”) The possibility of ovulation and conception prior to initiation of medication should be considered.
(See Discussion of Dose-related risk of vascular disease from oral contraceptives.)
Additional Instructions For All Dosing Regimens:
Breakthrough bleeding, spotting, and amenorrhea are frequent reasons for patients discontinuing oral contraceptives. In breakthrough bleeding, as in all cases of irregular bleeding from the vagina, nonfunctional causes should be borne in mind. In undiagnosed persistent or recurrent abnormal bleeding from the vagina, adequate diagnostic measures are indicated to rule out pregnancy or malignancy. If pathology has been excluded, time or a change to another formulation may solve the problem. Changing to an oral contraceptive with a higher estrogen content, while potentially useful in minimizing menstrual irregularity, should be done only if necessary since this may increase the risk of thromboembolic disease.
Use of oral contraceptives in the event of a missed menstrual period:
- If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period and oral contraceptive use should be discontinued until pregnancy is ruled out.
- If the patient has adhered to the prescribed regimen and misses two consecutive periods, pregnancy should be ruled out before continuing oral contraceptive use.
How Supplied
Nortrel™ 7/7/7 (norethindrone and ethinyl estradiol tablets, USP 0.5/0.035 mg, 0.75/0.035 mg, and 1/0.035 mg) (28 Day Regimen) are available in a tablet dispenser containing 28 tablets as follows; 7 light yellow tablets, 7 blue tablets, and 7 peach tablets as described under the 21 Day Regimen uled above, and the 7 white tablets contain inert ingredients. (NDC 54868-5286-0).
References
- Trussel J. Contraceptive efficacy. In Hatcher RA, Trussel J, Stewart F, Cates W, Stewart GK, Kowal D, Guest F, Contraceptive Technology: Seventeenth Revised Edition. New York NY: Irvington Publishers, 1998, in press.
- Stadel BV. Oral contraceptives and cardiovascular disease.(Pt. 1). N Engl J Med 1981; 305:612-618.
- Stadel BV. Oral contraceptives and cardiovascular disease. (Pt. 2). N Engl J Med 1981; 305:672-677.
- Adam SA, Thorogood M. Oral contraception and myocardial infarction revisited: the effects of new preparations and prescribing patterns. Br J Obstet Gynaecol 1981; 88:838-845.
- Mann JI, Inman WH. Oral contraceptives and death from myocardial infarction. Br Med J 1975; 2(5965):245-248.
- Mann JI, Vessey MP, Thorogood M, Doll R. Myocardial infarction in young women with special reference to oral contraceptive practice. Br Med J 1975; 2(5956):241-245.
- Royal College of General Practitioners' Oral Contraception Study: further analyses of mortality in oral contraceptive users. Lancet 1981; 1:541-546.
- Slone D, Shapiro S, Kaufman DW, Rosenberg L, Miettinen OS, Stolley PD. Risk of myocardial infarction in relation to current and discontinued use of oral contraceptives. N Engl J Med 1981; 305:420-424.
- Vessey MP. Female hormones and vascular disease - an epidemiological overview. Br J Fam Plann 1980; 6(Supplement):1-12.
- Russell-Briefel RG, Ezzati TM, Fulwood R, Perlman JA, Murphy RS. Cardiovascular risk status and oral contraceptive use, United States, 1976-80. Prevent Med 1986; 15:352-362.
- Goldbaum GM, Kendrick JS, Hogelin GC, Gentry EM. The relative impact of smoking and oral contraceptive use on women in the United States. JAMA 1987; 258:1339-1342.
- Layde PM, Beral V. Further analyses of mortality in oral contraceptive users; Royal College of General Practitioners' Oral Contraception Study. (Table 5) Lancet 1981; 1:541-546.
- Knopp RH. Arteriosclerosis risk: the roles of oral contraceptives and postmenopausal estrogens. J Reprod Med 1986; 31(9) (Supplement):913-921.
- Krauss RM, Roy S. Mishell DR, Casagrande J, Pike MC. Effects of two low-dose oral contraceptives on serum lipids and lipoproteins: Differential changes in highdensity lipoproteins subclasses. Am J Obstet 1983; 145:446-452.
- Wahl P, Walden C, Knopp R, Hoover J, Wallace R, Heiss G, Rifkind B. Effect of estrogen/progestin potency on lipid/lipoprotein cholesterol. N Engl J Med 1983; 308:862-867.
- Wynn V, Niththyananthan R. The effect of progestin in combined oral contraceptives on serum lipids with special reference to high density lipoproteins. Am J Obstet Gynecol 1982; 142:766-771.
- Wynn V, Godsland I. Effects of oral contraceptives on carbohydrate metabolism. J Reprod Med 1986; 31(9)(Supplement):892-897.
- La Rosa JC. Atherosclerotic risk factors in cardiovascular disease. J. Reprod Med 1986; 31(9)(Supplement):906-912.
- Inman WH, Vessey MP. Investigation of death from pulmonary, coronary, and cerebral thrombosis and embolism in women of child-bearing age. Br Med J 1968; 2(5599):193-199.
- Maguire MG, Tonascia J, Sartwell PE, Stolley PD, Tockman MS. Increased risk of thrombosis due to oral contraceptives: a further report. Am J Epidemiol 1979; 110(2):188-195.
- Petitti DB, Wingerd J, Pellegrin F, Ramacharan S. Risk of vascular disease in women: smoking, oral contraceptives, noncontraceptive estrogens, and other factors. JAMA 1979; 242:1150-1154.
- Vessey MP, Doll R. Investigation of relation between use of oral contraceptives and thromboembolic disease. Br Med J 1968; 2(5599):199-205.
- Vessey MP, Doll R. Investigation of relation between use of oral contraceptives and thromboembolic disease. A further report. Br Med J 1969; 2(5658):651-657.
- Porter JB, Hunter JR, Danielson DA, Jick H. Stergachis A. Oral contraceptives and non-fatal vascular disease - recent experience. Obstet Gynecol 1982; 59(3):299-302.
- Vessey M, Doll R, Peto R, Johnson B, Wiggins P. A long-term follow-up study of women using different methods of contraception: an interim report. J Biosocial Sci 1976; 8:375-427.
- Royal College of General Practitioners: Oral Contraceptives, venous thrombosis, and varicose veins. J Royal Coll Gen Pract 1978; 28:393-399.
- Collaborative Group for the Study of Stroke in Young Women: Oral contraception and increased risk of cerebral ischemia or thrombosis. N Engl J Med 1973; 288:871-878.
- Petitti DB, Wingerd J. Use of oral contraceptives, cigarette smoking, and risk of subarachnoid hemorrhage. Lancet 1978; 2:234-236.
- Inman WH. Oral contraceptives and fatal subarachnoid hemorrhage. Br Med J 1979; 2(6203):1468-1470.
- Collaborative Group for the Study of Stroke in Young Women: Oral Contraceptives and stroke in young women: associated risk factors. JAMA 1975; 231:718-722.
- Inman WH, Vessey MP, Westerholm B, Engelund A. Thromboembolic disease and the steroidal content of oral contraceptives. A report to the Committee on Safety of Drugs. Br Med J 1970; 2:203-209.
- Meade TW, Greenberg G, Thompson SG. Progestogens and cardiovascular reactions associated with oral contraceptives and a comparison of the safety of 50- and 35-mcg oestrogen preparations. Br Med J 1980; 280(6224):1157-1161.
- Kay CR. Progestogens and arterial disease - evidence from the Royal College of General Practitioners' Study. Am J Obstet Gynecol 1982; 142:762-765.
- Royal College of General Practitioners: Incidence of arterial disease among oral contraceptive users. J Royal Coll Gen Pract 1983; 33:75-82.
- Ory HW. Mortality associated with fertility and fertility control: 1983. Family Planning Perspectives 1983; 15:50-56.
- The Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development: Oral contraceptive use and the risk of breast cancer. N Engl J Med 1986; 315:405-411.
- Pike MC, Henderson BE, Krailo MD, Duke A, Roy S. Breast cancer in young women and use of oral contraceptives: possible modifying effect of formulation and age at use. Lancet 1983; 2:926-929.
- Paul C, Skegg DG, Spears GFS, Kaldor JM. Oral contraceptives and breast cancer: A national study. Br Med J 1986; 293:723-725.
- Miller DR, Rosenberg L, Kaufman DW, Schottenfeld D, Stolley PD, Shapiro S. Breast cancer risk in relation to early oral contraceptive use. Obstet Gynecol 1986; 68:863-868.
- Olson H, Olson KL, Moller TR, Ranstam J, Holm P. Oral contraceptive use and breast cancer in young women in Sweden (letter). Lancet 1985; 2:748-749.
- McPherson K, Vessey M, Neil A, Doll R, Jones L, Roberts M. Early contraceptive use and breast cancer: Results of another case-control study. Br J Cancer 1987; 56:653-660.
- Huggins GR, Zucker PF. Oral contraceptives and neoplasia: 1987 update. Fertil Steril 1987; 47:733-761.
- McPherson K, Drife JO. The pill and breast cancer: why the uncertainty? Br Med J 1986; 293:709-710.
- Shapiro S. Oral contraceptives - time to take stock. N Engl J Med 1987; 315:450-451.
- Ory H, Naib Z, Conger SB, Hatcher RA, Tyler CW. Contraceptive choice and prevalence of cervical dysplasia and carcinoma in situ. Am J Obstet Gynecol 1976; 124:573-577.
- Vessey MP, Lawless M, McPherson K, Yeates D. Neoplasia of the cervix uteri and contraception: a possible adverse effect of the pill. Lancet 1983; 2:930.
- Brinton LA, Huggins GR, Lehman HF, Malli K, Savitz DA, Trapido E, Rosenthal J, Hoover R. Long term use of oral contraceptives and risk of invasive cervical cancer. Int J Cancer 1986; 38:339-344.
- WHO Collaborative Study of Neoplasia and Steroid Contraceptives: Invasive cervical cancer and combined oral contraceptives. Br Med J 1985; 290:961-965.
- Rooks JB, Ory HW, Ishak KG, Strauss LT, Greenspan JR, Hill AP, Tyler CW. Epidemiology of hepatocellular adenoma: the role of oral contraceptive use. JAMA 1979; 242:644-648.
- Bein NN, Goldsmith HS. Recurrent massive hemorrhage from benign hepatic tumors secondary to oral contraceptives. Br J Surg 1977; 64:433-435.
- Klatskin G, Hepatic tumors: possible relationship to use of oral contraceptives. Gastroenterology 1977; 73:386-394.
- Henderson BE, Preston-Martin S, Edmondson HA, Peters RL, Pike MC. Hepatocellular carcinoma and oral contraceptives. Br J Cancer 1983; 48:437-440.
- Neuberger J, Forman D, Doll R, Williams R. Oral contraceptives and hepatocellular carcinoma. Br Med J 1986; 292:1355-1357.
- Forman D, Vincent TJ, Doll R. Cancer of the liver and oral contraceptives. Br Med J 1986; 292:1357-1361.
- Harlap S, Eldor J. Births following oral contraceptive failures. Obstet Gynecol 1980; 55:447-452.
- Savolainen E, Saksela E, Saxen L. Teratogenic hazards of oral contraceptives analyzed in a national malformation register. Am J Obstet Gynecol 1981; 140:521-524.
- Janerich DT, Piper JM, Glebatis DM. Oral contraceptives and birth defects. Am J Epidemiol 1980; 112:73-79.
- Ferencz C, Matanoski GM, Wilson PD, Rubin JD, Neill CA, Gutberlet R. Maternal hormone therapy and congenital heart disease. Teratology 1980; 21:225-239.
- Rothman KJ, Fyler DC, Goldblatt A, Kreidberg MB. Exogenous hormones and other drug exposures of children with congenital heart disease. Am J Epidemiol 1979; 109:433-439.
- Boston Collaborative Drug Surveillance Program: Oral contraceptives and venous thromboembolic disease, surgically confirmed gallbladder disease, and breast tumors. Lancet 1973; 1:1399-1404.
- Royal College of General Practitioners: Oral contraceptives and health. New York, Pittman 1974.
- Layde PM, Vessey MP, Yeates D. Risk of gallbladder disease: a cohort study of young women attending family planning clinics. J Epidemiol Community Health 1982; 36:274-278.
- Rome Group for Epidemiology and Prevention of Cholelithiasis (GREPCO): Prevalence of gallstone disease in an Italian adult female population. Am J Epidemiol 1984; 119:796-805.
- Storm BL, Tamragouri RT, Morse ML, Lazar EL, West SL, Stolley PD, Jones JK. Oral contraceptives and other risk factors for gallbladder disease. Clin Pharmacol Ther 1986; 39:335-341.
- Wynn V, Adams PW, Godsland IF, Melrose J, Niththyananthan R, Oakley NW, Seedj A. Comparison of effects of different combined oral contraceptive formulations on carbohydrate and lipid metabolism. Lancet 1979; 1:1045-1049.
- Wynn V. Effect of progesterone and progestins on carbohydrate metabolism. In: Progesterone and Progestin. Bardin CW, Milgrom E, Mauvis-Jarvis P. eds. New York, Raven Press 1983; pp. 395-410.
- Perlman JA, Roussell-Briefel RG, Ezzati TM, Lieberknecht G. Oral glucose tolerance and the potency of oral contraceptive progestogens. J Chronic Dis 1985; 38:857-864.
- Royal College of General Practitioners' Oral Contraception Study: Effect on hypertension and benign breast disease of progestogen component in combined oral contraceptives. Lancet 1977; 1:624.
- Fisch IR, Frank J. Oral contraceptives and blood pressure. JAMA 1977; 237:2499-2503.
- Laragh AJ. Oral contraceptive induced hypertension - nine years later. Am J Obstet Gynecol 1976; 126:141-147.
- Ramcharan S, Peritz E, Pellegrin FA, Williams WT. Incidence of hypertension in the Walnut Creek Contraceptive Drug Study cohort: In: Pharmacology of steroid contraceptive drugs. Garattini S, Berendes HW. Eds. New York, Raven Press, 1977; pp. 277-288, (Monographs of the Mario Negri Institute for Pharmacological Research Milan).
- Stockley I. Interactions with oral contraceptives. J Pharm 1976; 216:140-143.
- The Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development: Oral contraceptive use and the risk of ovarian cancer. JAMA 1983; 249:1596-1599.
- The Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development: Combination oral contraceptive use and the risk of endometrial cancer. JAMA 1987; 257:796-800.
- Ory HW. Functional ovarian cysts and oral contraceptives: negative association confirmed surgically. JAMA 1974; 228:68-69.
- Ory WH, Cole P, MacMahon B, Hoover R. Oral contraceptives and reduced risk of benign breast disease. N Engl J Med 1976; 294:419-422.
- Ory HW. The noncontraceptive health benefits from oral contraceptive use. Fam Plann Perspect 1982; 14:182-184.
- Ory HW, Forrest JD, Lincoln R. Making choices: Evaluating the health risks and benefits of birth control methods. New York, The Alan Guttmacher Institute, 1983; p. 1.
- Schlesselman J, Stadel BV, Murray P, Lai S. Breast cancer in relation to early use of oral contraceptives. JAMA 1988; 259:1828-1833.
- Hennekens CH, Speizer FE, Lipnick RJ, Rosner B, Bain C, Belanger C, Stampfer MJ, Willett W, Peto R. A case-control study of oral contraceptive use and breast cancer. JNCI 1984; 72:39-42.
- LaVecchia C, DeCarli A, Fasoli M, Francheschi S, Gentile A, Negri E, Parazzini F, Tognoni G. Oral contraceptives and cancers of the breast and of the female genital tract. Interim results from a case-control study. Br J Cancer 1986; 54:311-317.
- Meirik O, Lund E, Adami H, Bergstrom R, Christoffersen T, Bergsjo P. Oral contraceptive use and breast cancer in young women. A Joint National Case-control study in Sweden and Norway. Lancet 1986; 11:650-654.
- Kay CR, Hannaford PC. Breast cancer and the pill - A further report from the Royal College of General Practitioners' oral contraception study. Br J Cancer 1988; 58:675-680.
- Stadel BV, Lai S, Schlesselman JJ, Murray P. Oral contraceptives and premenopausal breast cancer in nulliparous women. Contraception 1988; 38:287-299.
- Miller DR, Rosenberg L, Kaufman DW, Stolley P, Warshauer ME, Shapiro S. Breast cancer before age 45 and oral contraceptive use: New Findings. Am J Epidemiol 1989; 129:269-280.
- The UK National Case-Control Study Group, Oral contraceptive use and breast cancer risk in young women. Lancet 1989; 1:973-982.
- Schlesselman JJ. Cancer of the breast and reproductive tract in relation to use of oral contraceptives. Contraception 1989; 40:1-38.
- Vessey MP, McPherson K, Villard - Mackintosh L, Yeates D. Oral contraceptives and breast cancer: latest findings in a large cohort study. Br J Cancer 1989; 59: 613-617.
- Jick SS, Walker AM, Stergachis A, Jick H. Oral contraceptives and breast cancer. Br J Cancer 1989; 59:618-621.
- Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53,297 women with breast cancer and 100,239 women without breast cancer from 54 epidemiological studies. Lancet 1996; 347:1713-1727.
- Palmer JR, Rosenberg L, Kaufman DW, Warshauer ME, Stolley P, Shapiro S. Oral contraceptive Use and Liver Cancer. Am J Epidemiol 1989; 130:878-882.
Brief Summary Patient Package Insert
Oral contraceptives, also known as “birth control pills” or “the pill”, are taken to prevent pregnancy and when taken correctly, have a failure rate of less than 1% per year when used without missing any pills. The typical failure rate of large numbers of pill users is less than 3% per year when women who miss pills are included. For most women oral contraceptives are also free of serious or unpleasant side effects. However, forgetting to take pills considerably increases the chances of pregnancy.
For the majority of women, oral contraceptives can be taken safely. But there are some women who are at high risk of developing certain serious diseases that can be fatal or may cause temporary or permanent disability. The risks associated with taking oral contraceptives increase significantly if you:
- Smoke
- have high blood pressure, diabetes, high cholesterol
- have or have had clotting disorders, heart attack, stroke, angina pectoris, cancer of the breast or sex organs, jaundice or malignant or benign liver tumors.
Although cardiovascular disease risks may be increased with oral contraceptive use after age 40 in healthy, non-smoking women (even with the newer low-dose formulations), there are also greater potential health risks associated with pregnancy in older women.
You should not take the pill if you suspect you are pregnant or have unexplained vaginal bleeding.
Boxed Warning section
Cigarette smoking increases the risk of serious cardiovascular side effects from oral contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives are strongly advised not to smoke.
Most side effects of the pill are not serious. The most common such effects are nausea, vomiting, bleeding between menstrual periods, weight gain, breast tenderness, and difficulty wearing contact lenses. These side effects, especially nausea and vomiting, may subside within the first three months of use.
The serious side effects of the pill occur very infrequently, especially if you are in good health and are young. However, you should know that the following medical conditions have been associated with or made worse by the pill:
- Blood clots in the legs (thrombophlebitis), lungs (pulmonary embolism), stoppage or rupture of a blood vessel in the brain (stroke), blockage of blood vessels in the heart (heart attack or angina pectoris) or other organs of the body. As mentioned above, smoking increases the risk of heart attacks and strokes and subsequent serious medical consequences.
- In rare cases, oral contraceptives can cause benign but dangerous liver tumors. These benign liver tumors can rupture and cause fatal internal bleeding. In addition, some studies report an increased risk of developing liver cancer. However, liver cancers are rare.
- High blood pressure, although blood pressure usually returns to normal when the pill is stopped.
The symptoms associated with these serious side effects are discussed in the detailed leaflet given to you with your supply of pills. Notify your doctor or health care provider if you notice any unusual physical disturbances while taking the pill. In addition, drugs such as rifampin, as well as some anticonvulsants and some antibiotics may decrease oral contraceptive effectiveness.
There is conflict among studies regarding breast cancer and oral contraceptive use. Some studies have reported an increase in the risk of developing breast cancer, particularly at a younger age. This increased risk appears to be related to duration of use. The majority of studies have found no overall increase in the risk of developing breast cancer. Some studies have found an increase in the incidence of cancer of the cervix in women who use oral contraceptives. However, this finding may be related to factors other than the use of oral contraceptives. There is insufficient evidence to rule out the possibility that pills may cause such cancers.
Taking the combination pill provides some important non-contraceptive benefits. These include less painful menstruation, less menstrual blood loss and anemia, fewer pelvic infections, and fewer cancers of the ovary and the lining of the uterus.
Be sure to discuss any medical condition you may have with your health care provider. Your health care provider will take a medical and family history before prescribing oral contraceptives and will examine you. The physical examination may be delayed to another time if you request it and the health care provider believes that it is a good medical practice to postpone it. You should be reexamined at least once a year while taking oral contraceptives. Your pharmacist should have given you the detailed patient information labeling which gives you further information which you should read and discuss with your health care provider.
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted diseases such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
Detailed Patient Labeling
PLEASE NOTE: This labeling is revised from time to time as important new medical information becomes available. Therefore, please review this labeling carefully.
The following oral contraceptive products contain a combination of an estrogen and progestogen, the two kinds of female hormones:
Nortrel™ 7/7/7 (norethindrone and ethinyl estradiol tablets, USP 0.5/0.035 mg, 0.75/0.035 mg, and 1/0.035 mg) (21 Day Regimen and 28 Day Regimen): Each light yellow tablet contains 0.5 mg norethindrone and 0.035 mg ethinyl estradiol. Each blue tablet contains 0.75 mg norethindrone and 0.035 mg ethinyl estradiol. Each peach tablet contains 1 mg norethindrone and 0.035 mg ethinyl estradiol. Each white tablet in the (28) day regimen contains inert ingredients.
INTRODUCTION:
Any woman who considers using oral contraceptives (the birth control pill or the pill) should understand the benefits and risks of using this form of birth control. This patient labeling will give you much of the information you will need to make this decision and will also help you determine if you are at risk of developing any of the serious side effects of the pill. It will tell you how to use the pill properly so that it will be as effective as possible. However, this labeling is not a replacement for a careful discussion between you and your health care provider. You should discuss the information provided in this labeling with him or her, both when you first start taking the pill and during your revisits. You should also follow your health care provider's advice with regard to regular check-ups while you are on the pill.
EFFECTIVENESS OF ORAL CONTRACEPTIVES:
Oral contraceptives or “birth control pills” or “the pill” are used to prevent pregnancy and are more effective than other non-surgical methods of birth control. When they are taken correctly, the chance of becoming pregnant is less than 1% (1 pregnancy per 100 women per year of use) when used perfectly, without missing any pills. Typical failure rates are actually 3% per year. The chance of becoming pregnant increases with each missed pill during a menstrual cycle.
In comparison, typical failure rates for other non-surgical methods of birth control during the first year of use are as follows:
Implant: <1%
Injection: <1%
IUD: 1 to 2%
Diaphragm with spermicides: 20%
Spermicides alone: 26%
Vaginal sponge: 20 to 40%
Female sterilization: <1%
Male sterilization: <1%
Cervical Cap with spermicides: 20 to 40%
Condom alone (male): 14%
Condom alone (female): 21%
Periodic abstinence: 25%
Withdrawal: 19%
No methods: 85%
WHO SHOULD NOT TAKE ORAL CONTRACEPTIVES:
Boxed Warning section
Cigarette smoking increases the risk of serious cardiovascular side effects from oral contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives are strongly advised not to smoke.
Some women should not use the pill. For example, you should not take the pill if you are pregnant or think you may be pregnant. You should also not use the pill if you have any of the following conditions:
- A history of heart attack or stroke
- Blood clots in the legs (thrombophlebitis), lungs (pulmonary embolism), or eyes
- A history of blood clots in the deep veins of your legs
- Chest pain (angina pectoris)
- Known or suspected breast cancer or cancer of the lining of the uterus, cervix or vagina
- Unexplained vaginal bleeding (until a diagnosis is reached by your doctor)
- Yellowing of the whites of the eyes or of the skin (jaundice) during pregnancy or during previous use of the pill
- Liver tumor (benign or cancerous)
- Known or suspected pregnancy
Tell your health care provider if you have ever had any of these conditions. Your health care provider can recommend a safer method of birth control.
OTHER CONSIDERATIONS BEFORE TAKING ORAL CONTRACEPTIVES:
Tell your health care provider if you have or have had:
- Breast nodules, fibrocystic disease of the breast, an abnormal breast x-ray or mammogram
- Diabetes
- Elevated cholesterol or triglycerides
- High blood pressure
- Migraine or other headaches or epilepsy
- Mental depression
- Gallbladder, heart or kidney disease
- History of scanty or irregular menstrual periods
Women with any of these conditions should be checked often by their health care provider if they choose to use oral contraceptives.
Also, be sure to inform your doctor or health care provider if you smoke or are on any medications.
RISKS OF TAKING ORAL CONTRACEPTIVES:
- Risk of developing blood clots Blood clots and blockage of blood vessels are one of the most serious side effects of taking oral contraceptives and can cause death or serious disability. In particular, a clot in the legs can cause thrombophlebitis and a clot that travels to the lungs can cause a sudden blocking of the vessel carrying blood to the lungs. Rarely, clots occur in the blood vessels of the eye and may cause blindness, double vision, or impaired vision.If you take oral contraceptives and need elective surgery, need to stay in bed for a prolonged illness or have recently delivered a baby, you may be at risk of developing blood clots. You should consult your doctor about stopping oral contraceptives three to four weeks before surgery and not taking oral contraceptives for two weeks after surgery or during bed rest. You should also not take oral contraceptives soon after delivery of a baby. It is advisable to wait for at least four weeks after delivery if you are not breast feeding or four weeks after a second trimester abortion. If you are breast feeding, you should wait until you have weaned your child before using the pill. (See also the section on Breast feeding in GENERAL PRECAUTIONS.)The risk of circulatory disease in oral contraceptive users may be higher in users of high-dose pills and may be greater with longer duration of oral contraceptive use. In addition, some of these increased risks may continue for a number of years after stopping oral contraceptives. The risk of abnormal blood clotting increases with age in both users and nonusers of oral contraceptives, but the increased risk from the oral contraceptive appears to be present at all ages. For women aged 20 to 44, it is estimated that about 1 in 2,000 using oral contraceptives will be hospitalized each year because of abnormal clotting. Among nonusers in the same age group, about 1 in 20,000 would be hospitalized each year. For oral contraceptive users in general, it has been estimated that in women between the ages of 15 and 34 the risk of death due to a circulatory disorder is about 1 in 12,000 per year, whereas for nonusers the rate is about 1 in 50,000 per year. In the age group 35 to 44, the risk is estimated to be about 1 in 2,500 per year for oral contraceptive users and about 1 in 10,000 per year for nonusers.
- Heart attacks and strokes Oral contraceptives may increase the tendency to develop strokes (stoppage or rupture of blood vessels in the brain) and angina pectoris and heart attacks (blockage of blood vessels in the heart). Any of these conditions can cause death or serious disability.Smoking greatly increases the possibility of suffering heart attacks and strokes. Furthermore, smoking and the use of oral contraceptives greatly increase the chances of developing and dying of heart disease.
- Gallbladder disease Oral contraceptive users probably have a greater risk than nonusers of having gallbladder disease, although this risk may be related to pills containing high doses of estrogens.
- Liver tumors In rare cases, oral contraceptives can cause benign but dangerous liver tumors. These benign liver tumors can rupture and cause fatal internal bleeding. In addition, some studies report an increased risk of developing liver cancer. However, liver cancers are rare.
- Cancer of the reproductive organs and breasts There is conflict among studies regarding breast cancer and oral contraceptive use. Some studies have reported an increase in the risk of developing breast cancer, particularly at a younger age. This increased risk appears to be related to duration of use. The majority of studies have found no overall increase in the risk of developing breast cancer.A meta-analysis of 54 studies found a small increase in the frequency of having breast cancer diagnosed for women who were currently using combined oral contraceptives or had used them within the past ten years. This increase in the frequency of breast cancer diagnosis, within ten years of stopping use, was generally accounted for by cancers localized to the breast. There was no increase in the frequency of having breast cancer diagnosed ten or more years after cessation of use.Some studies have found an increase in the incidence of cancer of the cervix in women who use oral contraceptives. However, this finding may be related to factors other than the use of oral contraceptives. There is insufficient evidence to rule out the possibility that pills may cause such cancers.
ESTIMATED RISK OF DEATH FROM A BIRTH CONTROL METHOD OR PREGNANCY:
All methods of birth control and pregnancy are associated with a risk of developing certain diseases which may lead to disability or death. An estimate of the number of deaths associated with different methods of birth control and pregnancy has been calculated and is shown in the following table.
ANNUAL NUMBER OF BIRTH-RELATED OR METHOD-RELATED DEATHS ASSOCIATED WITH CONTROL OF FERTILITY PER 100,000 NONSTERILE WOMEN, BY FERTILITY CONTROL METHOD ACCORDING TO AGE Method of control and outcome 15-19 20-24 25-29 30-34 35-39 40-44 No fertility control methods Deaths are birth-related 7.0 7.4 9.1 14.8 25.7 28.2 Oral contraceptives non-smoker Deaths are method-related 0.3 0.5 0.9 1.9 13.8 31.6 Oral contraceptives smoker 2.2 3.4 6.6 13.5 51.1 117.2 IUD 0.8 0.8 1.0 1.0 1.4 1.4 Condom 1.1 1.6 0.7 0.2 0.3 0.4 Diaphragm/spermicid 1.9 1.2 1.2 1.3 2.2 2.8 Periodic abstinence 2.5 1.6 1.6 1.7 2.9 3.6
In the above table, the risk of death from any birth control method is less than the risk of childbirth, except for oral contraceptive users over the age of 35 who smoke and pill users over the age of 40 even if they do not smoke. It can be seen in the table that for women aged 15 to 39, the risk of death was highest with pregnancy (7-26 deaths per 100,000 women, depending on age). Among pill users who do not smoke, the risk of death was always lower than that associated with pregnancy for any age group, although over the age of 40, the risk increases to 32 deaths per 100,000 women, compared to 28 associated with pregnancy at that age. However, for pill users who smoke and are over the age of 35, the estimated number of deaths exceed those for other methods of birth control. If a woman is over the age of 40 and smokes, her estimated risk of death is four times higher (117/100,000 women) than the estimated risk associated with pregnancy (28/100,000 women) in that age group.
The suggestion that women over 40 who do not smoke should not take oral contraceptives is based on information from older, higher-dose pills. An Advisory Committee of the FDA discussed this issue in 1989 and recommended that the benefits of low-dose oral contraceptive use by healthy, non-smoking women over 40 years of age may outweigh the possible risks.
WARNING SIGNALS:
If any of these adverse effects occur while you are taking oral contraceptives, call your doctor immediately:
- Sharp chest pain, coughing of blood, or sudden shortness of breath (indicating a possible clot in the lung)
- Pain in the calf (indicating a possible clot in the leg)
- Crushing chest pain or heaviness in the chest (indicating a possible heart attack)
- Sudden severe headache or vomiting, dizziness or fainting, disturbances of vision or speech, weakness, or numbness in an arm or leg (indicating a possible stroke)
- Sudden partial or complete loss of vision (indicating a possible clot in the eye)
- Breast lumps (indicating possible breast cancer or fibrocystic disease of the breast; ask your doctor or health care provider to show you how to examine your breasts)
- Severe pain or tenderness in the stomach area (indicating a possibly ruptured liver tumor)
- Difficulty in sleeping, weakness, lack of energy, fatigue, or change in mood (possibly indicating severe depression)
- Jaundice or a yellowing of the skin or eyeballs, accompanied frequently by fever, fatigue, loss of appetite, dark colored urine, or light colored bowel movements (indicating possible liver problems)
SIDE EFFECTS OF ORAL CONTRACEPTIVES:
- Vaginal bleeding Irregular vaginal bleeding or spotting may occur while you are taking the pills. Irregular bleeding may vary from slight staining between menstrual periods to breakthrough bleeding which is a flow much like a regular period. Irregular bleeding occurs most often during the first few months of oral contraceptive use, but may also occur after you have been taking the pill for some time. Such bleeding may be temporary and usually does not indicate any serious problems. It is important to continue taking your pills on schedule. If the bleeding occurs in more than one cycle or lasts for more than a few days, talk to your doctor or health care provider.
- Contact lenses If you wear contact lenses and notice a change in vision or an inability to wear your lenses, contact your doctor or health care provider.
- Fluid retention Oral contraceptives may cause edema (fluid retention) with swelling of the fingers or ankles and may raise your blood pressure. If you experience fluid retention, contact your doctor or health care provider.
- Melasma A spotty darkening of the skin is possible, particularly of the face, which may persist.
- Other side effects Other side effects may include nausea and vomiting, change in appetite, headache, nervousness, depression, dizziness, loss of scalp hair, rash, and vaginal infections.
If any of these side effects bother you, call your doctor or health care provider.
GENERAL PRECAUTIONS:
1. Missed periods and use of oral contraceptives before or during early pregnancy
There may be times when you may not menstruate regularly after you have completed taking a cycle of pills. If you have taken your pills regularly and miss one menstrual period, continue taking your pills for the next cycle but be sure to inform your health care provider before doing so. If you have not taken the pills daily as instructed and missed a menstrual period, you may be pregnant. If you missed two consecutive menstrual periods, you may be pregnant. Check with your health care provider immediately to determine whether you are pregnant. Do not continue to take oral contraceptives until you are sure you are not pregnant, but continue to use another method of contraception.
There is no conclusive evidence that oral contraceptive use is associated with an increase in birth defects, when taken inadvertently during early pregnancy. Previously, a few studies had reported that oral contraceptives might be associated with birth defects, but these findings have not been seen in more recent studies. Nevertheless, oral contraceptives or any other drugs should not be used during pregnancy unless clearly necessary and prescribed by your doctor. You should check with your doctor about risks to your unborn child of any medication taken during pregnancy.
2. While breast feeding
If you are breast feeding, consult your doctor before starting oral contraceptives. Some of the drug will be passed on to the child in the milk. A few adverse effects on the child have been reported, including yellowing of the skin (jaundice) and breast enlargement. In addition, combination oral contraceptives may decrease the amount and quality of your milk. If possible, do not use combination oral contraceptives while breast feeding. You should use another method of contraception since breast feeding provides only partial protection from becoming pregnant and this partial protection decreases significantly as you breast feed for longer periods of time. You should consider starting combination oral contraceptives only after you have weaned your child completely.
3. Laboratory tests
If you are scheduled for any laboratory tests, tell your doctor you are taking birth control pills. Certain blood tests may be affected by birth control pills.
4. Drug interactions
Certain drugs may interact with birth control pills to make them less effective in preventing pregnancy or cause an increase in breakthrough bleeding. Such drugs include rifampin, drugs used for epilepsy such as barbiturates (for example, phenobarbital), anticonvulsants such as carbamazepine (Tegretol is one brand of this drug), phenytoin (Dilantin is one brand of this drug), phenylbutazone (Butazolidin is one brand), and possibly certain antibiotics. You may need to use additional contraception when you take drugs which can make oral contraceptives less effective.
5. Sexually transmitted diseases
This product (like all oral contraceptives) is intended to prevent pregnancy. It does not protect against transmission of HIV (AIDS) and other sexually transmitted diseases such as chlamydia, genital herpes, genital warts, gonorrhea, hepatitis B, and syphilis.
HOW TO TAKE THE PILL
IMPORTANT POINTS TO REMEMBER
BEFORE YOU START TAKING YOUR PILLS:
- BE SURE TO READ THESE DIRECTIONS:Before you start taking your pills.Anytime you are not sure what to do.
- THE RIGHT WAY TO TAKE THE PILL IS TO TAKE ONE PILL EVERY DAY AT THE SAME TIME.If you miss pills you could get pregnant. This includes starting the pack late. The more pills you miss, the more likely you are to get pregnant.
- MANY WOMEN HAVE SPOTTING OR LIGHT BLEEDING, OR MAY FEEL SICK TO THEIR STOMACH DURING THE FIRST 1-3 PACKS OF PILLS. If you feel sick to your stomach, do not stop taking the pill. The problem will usually go away. If it doesn't go away, check with your doctor or clinic.
- MISSING PILLS CAN ALSO CAUSE SPOTTING OR LIGHT BLEEDING, even when you make up these missed pills.On the days you take 2 pills to make up for missed pills, you could also feel a little sick to your stomach.
- IF YOU HAVE VOMITING OR DIARRHEA, for any reason, or IF YOU TAKE SOME MEDICINES, including some antibiotics, your pills may not work as well.Use a back-up method (such as condoms, foam, or sponge) until you check with your doctor or clinic.
- IF YOU HAVE TROUBLE REMEMBERING TO TAKE THE PILL, talk to your doctor or clinic about how to make pill-taking easier or about using another method of birth control.
- IF YOU HAVE ANY QUESTIONS OR ARE UNSURE ABOUT THE INFORMATION IN THIS LEAFLET, call your doctor or clinic.
BEFORE YOU START TAKING YOUR PILLS
- DECIDE WHAT TIME OF DAY YOU WANT TO TAKE YOUR PILL.It is important to take it at about the same time every day.
- LOOK AT YOUR PILL PACK TO SEE IF IT HAS 21 OR 28 PILLS.The 21-pill pack has 21 “active” pills (with hormones) to take for 3 weeks. This is followed by 1 week without pills.The 28-pill pack has 21 “active” pills (with hormones) to take for 3 weeks. This is followed by 1 week of “reminder” white pills (without hormones). Nortrel 7/7/7: There are 7 light yellow “active” pills, 7 blue “active” pills and 7 peach “active” pills.
- ALSO FIND:1) where on the pack to start taking pills,2) in what order to take the pills.CHECK ADDITIONAL INSTRUCTIONS FOR USING THIS PACKAGE IN THE BRIEF SUMMARY PATIENT PACKAGE INSERT.
- BE SURE YOU HAVE READY AT ALL TIMES:ANOTHER KIND OF BIRTH CONTROL (such as condoms, foam, or sponge) to use as a back-up method in case you miss pills.AN EXTRA, FULL PILL PACK.
WHEN TO START THE FIRST PACK OF PILLS
You have a choice of which day to start taking your first pack of pills. Nortrel 7/7/7 are available in the Buler Pack Tablet Dispenser which is preset for a Sunday Start. Day 1 Start is also provided. Decide with your doctor or clinic which is the best day for you. Pick a time of day which will be easy to remember.
SUNDAY START:
Nortrel 7/7/7: Take the first “active” light yellow pill of the first pack on the Sunday after your period starts, even if you are still bleeding. If your period begins on Sunday, start the pack the same day.
Use another method of birth control as a back-up method if you have sex anytime from the Sunday you start your first pack until the next Sunday (7 days). Condoms, foam, or the sponge are good back-up methods of birth control.
DAY 1 START:
Nortrel 7/7/7: Take the first “active” light yellow pill of the first pack during the first 24 hours of your period.
You will not need to use a back-up method of birth control, since you are starting the pill at the beginning of your period.
WHAT TO DO DURING THE MONTH
- TAKE ONE PILL AT THE SAME TIME EVERY DAY UNTIL THE PACK IS EMPTY. Do not skip pills even if you are spotting or bleeding between monthly periods or feel sick to your stomach (nausea). Do not skip pills even if you do not have sex very often.
- WHEN YOU FINISH A PACK OR SWITCH YOUR BRAND OF PILLS: 21 pills: Wait 7 days to start the next pack. You will probably have your period during that week. Be sure that no more than 7 days pass between 21-day packs. 28 pills: Start the next pack on the day after your last “reminder” pill. Do not wait any days between packs.
WHAT TO DO IF YOU MISS PILLS
Nortrel 7/7/7:
If you MISS 1 light yellow, blue or peach “active” pill:
- Take it as soon as you remember. Take the next pill at your regular time. This means you may take 2 pills in 1 day.
- You do not need to use a back-up birth control method if you have sex.
If you MISS 2 light yellow or blue “active” pills in a row in WEEK 1 OR WEEK 2 of your pack:
- Take 2 pills on the day you remember and 2 pills the next day.
- Then take 1 pill a day until you finish the pack.
- You MAY BECOME PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms, foam, or sponge) as a back-up method for those 7 days.
If you MISS 2 peach “active” pills in a row in THE 3RD WEEK:
- If you are a Sunday Starter: Keep taking 1 pill every day until Sunday. On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day. If you are a Day Starter: THROW OUT the rest of the pill pack and start a new pack that same day.
- You may not have your period this month but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
- You MAY BECOME PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms, foam, or sponge) as a back-up method for those 7 days.
If you MISS 3 OR MORE light yellow, blue or peach “active” pills in a row (during the first 3 weeks):
- If you are a Sunday Starter: Keep taking 1 pill every day until Sunday. On Sunday, THROW OUT the rest of the pack and start a new pack of pills that same day. If you are a Day 1 Starter: THROW OUT the rest of the pill pack and start a new pack that same day.
- You may not have your period this month but this is expected. However, if you miss your period 2 months in a row, call your doctor or clinic because you might be pregnant.
- You MAY BECOME PREGNANT if you have sex in the 7 days after you miss pills. You MUST use another birth control method (such as condoms, foam, or sponge) as a back-up method for those 7 days.
A REMINDER FOR THOSE ON 28-DAY PACKS
If you forget any of the 7 white “reminder” pills in Week 4:
THROW AWAY the pills you missed.
Keep taking 1 pill each day until the pack is empty.
You do not need a back-up method.
FINALLY, IF YOU ARE STILL NOT SURE WHAT TO DO ABOUT THE PILLS YOU HAVE MISSED:
Use a BACK-UP METHOD anytime you have sex.
KEEP TAKING ONE “ACTIVE” PILL EACH DAY until you can reach your doctor or clinic.
PREGNANCY DUE TO PILL FAILURE:
Combination Oral Contraceptives
The incidence of pill failure resulting in pregnancy is approximately one percent (i.e., one pregnancy per 100 women per year) if taken every day as directed, but more typical failure rates are about 3%. If failure does occur, the risk to the fetus is minimal.
PREGNANCY AFTER STOPPING THE PILL:
There may be some delay in becoming pregnant after you stop using oral contraceptives, especially if you had irregular menstrual cycles before you used oral contraceptives. It may be advisable to postpone conception until you begin menstruating regularly once you have stopped taking the pill and desire pregnancy.
There does not appear to be any increase in birth defects in newborn babies when pregnancy occurs soon after stopping the pill.
OVERDOSAGE:
Serious ill effects have not been reported following ingestion of large doses of oral contraceptives by young children. Overdosage may cause nausea and withdrawal bleeding in females. In case of overdosage, contact your health care provider or pharmacist.
OTHER INFORMATION:
Your health care provider will take a medical and family history before prescribing oral contraceptives and will examine you. The physical examination may be delayed to another time if you request it and the health care provider believes that it is a good medical practice to postpone it. You should be reexamined at least once a year. Be sure to inform your health care provider if there is a family history of any of the conditions uled previously in this leaflet. Be sure to keep all appointments with your health care provider, because this is a time to determine if there are early signs of side effects of oral contraceptive use.
Do not use the drug for any condition other than the one for which it was prescribed. This drug has been prescribed specifically for you; do not give it to others who may want birth control pills.
HEALTH BENEFITS FROM ORAL CONTRACEPTIVES:
In addition to preventing pregnancy, use of combination oral contraceptives may provide certain benefits. They are:
- menstrual cycles may become more regular
- blood flow during menstruation may be lighter and less iron may be lost. Therefore, anemia due to iron deficiency is less likely to occur.
- pain or other symptoms during menstruation may be encountered less frequently
- ectopic (tubal) pregnancy may occur less frequently
- noncancerous cysts or lumps in the breast may occur less frequently
- acute pelvic inflammatory disease may occur less frequently
- oral contraceptive use may provide some protection against developing two forms of cancer: cancer of the ovaries and cancer of the lining of the uterus.
If you want more information about birth control pills, ask your doctor or pharmacist. They have a more technical leaflet called the Professional Labeling, which you may wish to read. The professional labeling is also published in a book entitled Physicians' Desk Reference, available in many book stores and public libraries.
MANUFACTURED BYBARR LABORATORIES, INC.POMONA, NY 10970
MARCH 2004BR-9011, 9012
Additional barcode labeling by: Physicians Total Care, Inc.Tulsa, Oklahoma       74146
Principal Display Panel
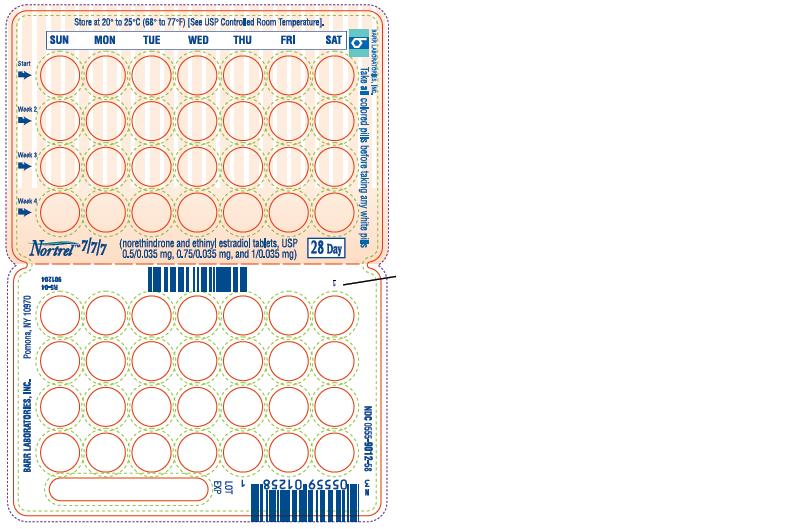
Foil Pouch Text
NDC 54868-5286-0
Nortrel 7/7/7 (norethindrone and ethinyl estradiol tablets, USP-triphasic regimen) Each light yellow tablet contains 0.5 mg norethindrone and 0.035 mg ethinyl estradiol. Each blue tablet contains 0.75 mg norethindrone and 0.035 mg ethinyl estradiol. Each peach tablet contains 1 mg norethindrone and 0.035 mg ethinyl estradiol. Each white tablet contains inert ingredients. 28 DAY REGIMENRx onlyTHIS PRODUCT (LIKE ALL ORAL CONTRACEPTIVES) IS INTENDED TO PREVENT PREGNANCY. IT DOES NOT PROTECT AGAINST HIV INFECTION (AIDS) AND OTHER SEXUALLY TRANSMITTED DISEASES.
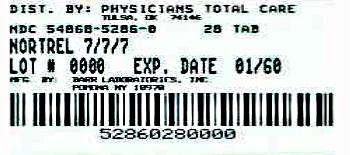
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site