Oxybutynin Chloride Dailymed
Generic: oxybutynin chloride is used for the treatment of Urinary Bladder, Neurogenic Colitis, Ulcerative Intestinal Obstruction Megacolon, Toxic Myasthenia Gravis Ureteral Obstruction Urinary Incontinence Glaucoma, Angle-Closure Urinary Retention Gastroparesis Dysuria Glaucoma
All Imprints
oxybutynin chloride 5 mg - a13 round pink
oxybutynin chloride 15 mg - a15 round white
Go PRO for all pill images
1 Indications And Usage
Oxybutynin chloride is a muscarinic antagonist indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency.
Oxybutynin chloride extended-release tablets are also indicated for the treatment of pediatric patients aged 6 years and older with symptoms of detrusor overactivity associated with a neurological condition (e.g., spina bifida).
- Oxybutynin chloride extended-release tablets are a muscarinic antagonist indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency. (
1 )- Oxybutynin chloride extended-release tablets are also indicated for the treatment of pediatric patients aged 6 years and older with symptoms of detrusor overactivity associated with a neurological condition (e.g., spina bifida). (
1 )
2 Dosage And Administration
Oxybutynin chloride extended-release tablets must be swallowed whole with the aid of liquids, and must not be chewed, divided, or crushed.
Oxybutynin chloride extended-release tablets may be administered with or without food.
Oxybutynin chloride extended-release tablets must be swallowed whole with the aid of liquids, and must not be chewed, divided, or crushed.Oxybutynin chloride extended-release tablets may be administered with or without food. (2 )
- Adults:Start with 5 mg or 10 mg, once daily at approximately the same time every day. Dose should not exceed 30 mg per day. (
2.1 )- Pediatric patients (6 years of age or older):Start with 5 mg, once daily at approximately the same time every day. Dose should not exceed 20 mg per day. (
2.2 )2.1 Adults
The recommended starting dose of oxybutynin chloride extended-release tablets is 5 or 10 mg once daily at approximately the same time each day. Dosage may be adjusted in 5-mg increments to achieve a balance of efficacy and tolerability (up to a maximum of 30 mg/day). In general, dosage adjustment may proceed at approximately weekly intervals.
2.2 Pediatric Patients Aged 6 Years of Age and Older
The recommended starting dose of oxybutynin chloride extended-release tablets is 5 mg once daily at approximately the same time each day. Dosage may be adjusted in 5-mg increments to achieve a balance of efficacy and tolerability (up to a maximum of 20 mg/day).
3 Dosage Forms And Strengths
Oxybutynin chloride extended-release tablets, USP are available as 5,10 and 15 mg tablets for oral use:
5 mg: Light pink to pink, round, film-coated tablets, imprinted with ‘Λ13’ in black ink on one side and plain on the other side.
10 mg: Light pink to pink, round, film-coated tablets, imprinted with ‘Λ14’ in black ink on one side and plain on the other side.
15 mg: White to off-white, round, film-coated tablets, imprinted with ‘Λ15’ in black ink on one side and plain on the other side.
Extended release tablets 5 mg, 10 mg and 15 mg (3 )
4 Contraindications
Oxybutynin chloride extended-release tablets are contraindicated in patients with urinary retention, gastric retention and other severe decreased gastrointestinal motility conditions, uncontrolled narrow-angle glaucoma.
Oxybutynin chloride extended-release tablets are also contraindicated in patients who have demonstrated hypersensitivity to the drug substance or other components of the product. There have been reports of hypersensitivity reactions, including anaphylaxis and angioedema.
- Urinary retention (
4 )- Gastric Retention (
4 )- Uncontrolled narrow angle glaucoma (
4 )- Known hypersensitivity to oxybutynin chloride extended-release tablets, oxybutynin or any component of oxybutynin chloride extended-release tablets (
4 )
5 Warnings And Precautions
- Angioedema: Angioedema has been reported with oxybutynin. If symptoms of angioedema occur, discontinue oxybutynin chloride extended-release tablets immediately and initiate appropriate therapy. (
5.1 )- Central Nervous System (CNS) effects: CNS effects have been reported with oxybutynin. If patient experiences anticholinergic CNS effects, consider dose adjustment or discontinuation of oxybutynin chloride extended-release tablets. (
5.2 )- Use with caution due to aggravation of symptoms:
- Pre-existing dementia in patients treated with cholinesterase inhibitors (
5.2 ),- Parkinson's disease (
5.2 ),- Myasthenia gravis (
5.3 ), and- Decreased gastrointestinal motility in patients with autonomic neuropathy. (
5.4 ).- Urinary Retention: Use with caution in patients with clinically significant bladder outflow obstruction because of the risk of urinary retention (
5.5 )- Gastrointestinal Adverse Reactions: Use with caution in patients with gastrointestinal obstructive disorders or decreased intestinal motility due to risk of gastric retention. Use with caution in patients with gastroesophageal reflux or in patients concurrently taking drugs that can exacerbate esophagitis. (
5.6 )5.1 Angioedema
Angioedema of the face, lips, tongue and/or larynx has been reported with oxybutynin. In some cases, angioedema occurred after the first dose. Angioedema associated with upper airway swelling may be life-threatening. If involvement of the tongue, hypopharynx, or larynx occurs, oxybutynin should be promptly discontinued and appropriate therapy and/or measures necessary to ensure a patent airway should be promptly provided.
5.2 Central Nervous System Effects
Oxybutynin is associated with anticholinergic central nervous system (CNS) effects [see Adverse Reactions (6)] . A variety of CNS anticholinergic effects have been reported, including hallucinations, agitation, confusion and somnolence. Patients should be monitored for signs of anticholinergic CNS effects, particularly in the first few months after beginning treatment or increasing the dose. Advise patients not to drive or operate heavy machinery until they know how oxybutynin chloride extended-release tablets affects them. If a patient experiences anticholinergic CNS effects, dose reduction or drug discontinuation should be considered.
Oxybutynin chloride extended-release tablets should be used with caution in patients with preexisting dementia treated with cholinesterase inhibitors due to the risk of aggravation of symptoms.
Oxybutynin chloride extended-release tablets should be used with caution in patients with Parkinson's disease due to the risk of aggravation of symptoms.
5.3 Worsening of Symptoms of Myasthenia Gravis
Oxybutynin chloride extended-release tablets should be used with caution in patients with myasthenia gravis due to the risk of aggravation of symptoms.
5.4 Worsening of Symptoms of Decreased Gastrointestinal Motility in Patients with Autonomic Neuropathy
Oxybutynin chloride extended-release tablets should be used with caution in patients with autonomic neuropathy due to the risk of aggravation of symptoms of decreased gastrointestinal motility.
5.5 Urinary Retention
Oxybutynin chloride extended-release tablets should be administered with caution to patients with clinically significant bladder outflow obstruction because of the risk of urinary retention [see Contraindications (4)] .
5.6 Gastrointestinal Adverse Reactions
Oxybutynin chloride extended-release tablets should be administered with caution to patients with gastrointestinal obstructive disorders because of the risk of gastric retention [see Contraindications (4)] .
Oxybutynin chloride extended-release tablets, like other anticholinergic drugs, may decrease gastrointestinal motility and should be used with caution in patients with conditions such as ulcerative colitis and intestinal atony.
Oxybutynin chloride extended-release tablets should be used with caution in patients who have gastroesophageal reflux and/or who are concurrently taking drugs (such as bisphosphonates) that can cause or exacerbate esophagitis.
As with any other nondeformable material, caution should be used when administering oxybutynin chloride extended-release tablets to patients with preexisting severe gastrointestinal narrowing (pathologic or iatrogenic). There have been rare reports of obstructive symptoms in patients with known strictures in association with the ingestion of other drugs in nondeformable controlled-release formulations.
6 Adverse Reactions
The most common (incidence ≥5%) adverse reactions were dry mouth, constipation, diarrhea, headache, somnolence, and dizziness. (6 )
To report SUSPECTED ADVERSE REACTIONS, contact Advagen Pharma Ltd, at 866-488-0312 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety and efficacy of oxybutynin chloride extended-release tablets (5 to 30 mg/day) was evaluated in 774 adult subjects who participated in five double-blind, controlled clinical trials. In four of the five studies, Ditropan IR (5 to 20 mg/day in 199 subjects) was an active comparator. Adverse reactions reported by ≥ 1% of subjects are shown in Table 1.
Table 1: Adverse Drug Reactions Reported by ≥ 1% of oxybutynin chloride extended-release tablets-treated Adult Subjects in Five Double-blind, Controlled Clinical Trials of oxybutynin chloride extended-release tablets System/Organ Class Preferred Term Oxybutynin ER Tablets 5 to 30 mg/day n=774 % Oxybutynin IR Tablets IR = immediate release 5 to 20 mg/day n=199 %Psychiatric Disorders   Insomnia 3.0 5.5 Nervous System Disorders   Headache 7.5 8.0   Somnolence 5.6 14.1   Dizziness 5.0 16.6   Dysgeusia 1.6 1.5 Eye Disorders   Vision blurred 4.3 9.6   Dry eye 3.1 2.5 Respiratory, Thoracic and Mediastinal Disorders   Cough 1.9 3.0   Oropharyngeal pain 1.9 1.5   Dry throat 1.7 2.5   Nasal dryness 1.7 4.5 Gastrointestinal Disorders   Dry mouth 34.9 72.4   Constipation 8.7 15.1   Diarrhea 7.9 6.5   Dyspepsia 4.5 6.0   Nausea 4.5 11.6   Abdominal pain 1.6 2.0   Vomiting 1.3 1.5   Flatulence 1.2 2.5   Gastro-esophageal reflux disease 1.0 0.5 Skin and Subcutaneous Tissue Disorders   Dry skin 1.8 2.5   Pruritus 1.3 1.5 Renal and Urinary Disorders   Dysuria 1.9 2.0   Urinary hesitation 1.9 8.5   Urinary retention 1.2 3.0 General Disorders and Administration Site Conditions   Fatigue 2.6 3.0 Investigations   Residual urine volume The bundled term residual urine volume consists of the preferred terms residual urine volume and residual urine volume increased. 2.3 3.5
The discontinuation rate due to adverse reactions was 4.4% with Oxybutynin ER tablets compared to 0% with Oxybutynin IR tablets. The most frequent adverse reaction causing discontinuation of study medication was dry mouth (0.7%).
The following adverse reactions were reported by <1% of oxybutynin chloride extended-release tablets-treated patients and at a higher incidence than placebo in clinical trials: Metabolism and Nutrition Disorders:anorexia, fluid retention; Vascular disorders:hot flush; Respiratory, thoracic and mediastinal disorders:dysphonia; Gastrointestinal Disorders:dysphagia, frequent bowel movements; General disorders and administration site conditions:chest discomfort, thirst.
6.2 Postmarketing Experience
The following additional adverse reactions have been reported from worldwide postmarketing experience with oxybutynin chloride extended-release tablets. Because postmarketing reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Infections and Infestations:Urinary tract infection; Psychiatric Disorders:psychotic disorder, agitation, confusional state, hallucinations, memory impairment, abnormal behavior; Nervous System Disorders:convulsions; Eye Disorders:glaucoma; Respiratory, Thoracic and Mediastinal Disorders:nasal congestion; Cardiac Disorders:arrhythmia, tachycardia, palpitations, QT interval prolongation; Vascular Disorders:flushing, hypertension; Skin and Subcutaneous Tissue Disorders:rash; Renal and Urinary Disorders:impotence; General Disorders and Administration Site Conditions:hypersensitivity reactions, including angioedema with airway obstruction, urticaria, and face edema; anaphylactic reactions requiring hospitalization for emergency treatment; Injury, poisoning and procedural complications:fall.
Additional adverse events reported with some other oxybutynin chloride formulations include: cycloplegia, mydriasis, and suppression of lactation. In one reported case, concomitant use of oxybutynin with carbamazepine and dantrolene was associated with adverse events of vomiting, drowsiness, confusion, unsteadiness, slurred speech and nystagmus, suggestive of carbamazepine toxicity.
7 Drug Interactions
The concomitant use of oxybutynin with other anticholinergic drugs or with other agents which produce dry mouth, constipation, somnolence (drowsiness), and/or other anticholinergic-like effects may increase the frequency and/or severity of such effects.
Anticholinergic agents may potentially alter the absorption of some concomitantly administered drugs due to anticholinergic effects on gastrointestinal motility. This may be of concern for drugs with a narrow therapeutic index. Anticholinergic agents may also antagonize the effects of prokinetic agents, such as metoclopramide.
Mean oxybutynin plasma concentrations were approximately 2 fold higher when oxybutynin chloride extended-release tablets were administered with ketoconazole, a potent CYP3A4 inhibitor. Other inhibitors of the cytochrome P450 3A4 enzyme system, such as antimycotic agents (e.g., itraconazole and miconazole) or macrolide antibiotics (e.g., erythromycin and clarithromycin), may alter oxybutynin mean pharmacokinetic parameters (i.e., C maxand AUC). The clinical relevance of such potential interactions is not known. Caution should be used when such drugs are co-administered.
- Co-administration with other anticholinergic drugs may increase the frequency and/or severity of anticholinergic-like effects. (
7 )- Co-administration with strong cytochrome P450 (CYP) 3A4 inhibitors (e.g., ketoconazole) increases the systemic exposure of oxybutynin. (
7 )
8 Use In Specific Populations
- Pediatric Use: Oxybutynin chloride extended-release tablets are not recommended in pediatric patients who cannot swallow the tablet whole without chewing, dividing or crushing, or in children under the age of 6 years. (
8.4 )- Renal or Hepatic Impairment: There have been no studies conducted in patients with renal or hepatic impairment. (
8.6 ,8.7 )8.1 Pregnancy
Risk Summary
There are no adequate data on oxybutynin chloride extended-release tablets use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
8.2 Lactation
Risk Summary
There are no data on the presence of oxybutynin in human milk, the effects on the breastfed infant, or the effects of oxybutynin chloride extended-release tablets on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for oxybutynin chloride extended-release tablets and any potential adverse effects on the breastfed child from oxybutynin chloride extended-release tablets or from the underlying maternal condition.
8.4 Pediatric Use
The safety and efficacy of oxybutynin chloride extended-release tablets were studied in 60 children in a 24-week, open-label, non-randomized trial. Patients were aged 6-15 years, all had symptoms of detrusor overactivity in association with a neurological condition (e.g., spina bifida), all used clean intermittent catheterization, and all were current users of oxybutynin chloride. Study results demonstrated that administration of oxybutynin chloride extended-release tablets 5 to 20 mg/day was associated with an increase from baseline in mean urine volume per catheterization from 108 mL to 136 mL, an increase from baseline in mean urine volume after morning awakening from 148 mL to 189 mL, and an increase from baseline in the mean percentage of catheterizations without a leaking episode from 34% to 51%.
Urodynamic results were consistent with clinical results. Administration of oxybutynin chloride extended-release tablets resulted in an increase from baseline in mean maximum cystometric capacity from 185 mL to 254 mL, a decrease from baseline in mean detrusor pressure at maximum cystometric capacity from 44 cm H 2O to 33 cm H 2O, and a reduction in the percentage of patients demonstrating uninhibited detrusor contractions (of at least 15 cm H 2O) from 60% to 28%.
The pharmacokinetics of oxybutynin chloride extended-release tablets in these patients were consistent with those reported for adults [see Clinical Pharmacology (12.3)] .
Oxybutynin chloride extended-release tablets are not recommended in pediatric patients who cannot swallow the tablet whole without chewing, dividing, or crushing, or in children under the age of 6.
8.5 Geriatric Use
The rate and severity of anticholinergic effects reported by patients less than 65 years old and those 65 years and older were similar. The pharmacokinetics of oxybutynin chloride extended-release tablets were similar in all patients studied (up to 78 years of age).
8.6 Renal Impairment
There were no studies conducted with oxybutynin chloride extended-release tablets in patients with renal impairment.
8.7 Hepatic Impairment
There were no studies conducted with oxybutynin chloride extended-release tablets in patients with hepatic impairment.
10 Overdosage
The continuous release of oxybutynin from oxybutynin chloride extended-release tablets should be considered in the treatment of overdosage. Patients should be monitored for at least 24 hours. Treatment should be symptomatic and supportive. A cathartic may be administered.
Overdosage with oxybutynin chloride has been associated with anticholinergic effects including central nervous system excitation, flushing, fever, dehydration, cardiac arrhythmia, vomiting, and urinary retention.
Ingestion of 100 mg oxybutynin chloride in association with alcohol has been reported in a 13-year-old boy who experienced memory loss, and a 34-year-old woman who developed stupor, followed by disorientation and agitation on awakening, dilated pupils, dry skin, cardiac arrhythmia, and retention of urine. Both patients fully recovered with symptomatic treatment.
11 Description
Oxybutynin chloride is an antispasmodic, muscarinic antagonist. Each oxybutynin chloride extended-release tablets, USP contains 5 mg, 10 mg or 15 mg of oxybutynin chloride USP, formulated as a once-a-day controlled-release tablet for oral administration. Oxybutynin chloride is administered as a racemate of R- and S-enantiomers.
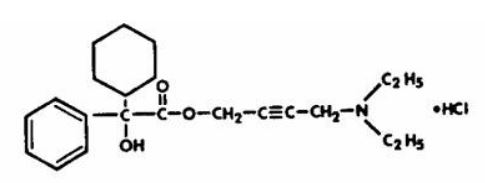
Chemically, oxybutynin chloride is d,l (racemic) 4-diethylamino-2-butynyl phenylcyclohexylglycolate hydrochloride. The empirical formula of oxybutynin chloride is C 22H 31NO 3•HCl.
Its structural formula is:
Oxybutynin chloride is a white crystalline solid with a molecular weight of 393.9. It is readily soluble in water and acids, but relatively insoluble in alkalis.
Oxybutynin chloride extended-release tablets, USP also contains the following inert ingredients: hypromellose, hydrogenated vegetable oil, microcrystalline cellulose, lactose monohydrate, povidone, colloidal silicon dioxide, magnesium stearate, methacrylic acid and ethyl acrylate co-polymer dispersion, triethyl citrate, talc, titanium dioxide, polyethylene glycol/macrogol, iron oxide yellow non-irradiated, isopropyl alcohol and iron oxide red non-irradiated. The ink contains shellac glaze (modified), black iron oxide non-irradiated, N-butyl alcohol, propylene glycol and ammonium hydroxide.
System Components and Performance
Oxybutynin chloride extended-release tablets, USP uses an enteric coated hydrophilic hydrogel matrix to deliver oxybutynin chloride at controlled rate over approximately 24 hours by diffusion mechanism. The system comprises of a core, which contains the drug, rate controlling hydrogel and other excipients. The core is surrounded by a partially or complete pH dependent membrane. Hence, when the drug reaches the acidic medium, in stomach minimal drug release will occur and when it reaches an environment of pH 5.5 and above, the outer membrane will be dissolved exposing the inner core. This inner core will partially hydrate to form a gel layer and the drug release will occur via diffusion mechanism from a gel layer and subsequently through gel erosion.
Meets USP Dissolution Method 4. FDA approved acceptance criteria differs from the USP acceptance criteria.
12 Clinical Pharmacology
12.1 Mechanism of Action
Oxybutynin relaxes bladder smooth muscle. Oxybutynin chloride exerts a direct antispasmodic effect on smooth muscle and inhibits the muscarinic action of acetylcholine on smooth muscle. No blocking effects occur at skeletal neuromuscular junctions or autonomic ganglia (antinicotinic effects).
Antimuscarinic activity resides predominantly in the R-isomer. A metabolite, desethyloxybutynin, has pharmacological activity similar to that of oxybutynin in in vitrostudies.
12.2 Pharmacodynamics
In patients with conditions characterized by involuntary bladder contractions, cystometric studies have demonstrated that oxybutynin increases bladder (vesical) capacity, diminishes the frequency of uninhibited contractions of the detrusor muscle, and delays the initial desire to void.
12.3 Pharmacokinetics
Absorption
Following the first dose of oxybutynin chloride extended-release tablets, oxybutynin plasma concentrations rise for 4 to 6 hours; thereafter steady concentrations are maintained for up to 24 hours, minimizing fluctuations between peak and trough concentrations associated with oxybutynin.
The relative bioavailabilities of R- and S-oxybutynin from oxybutynin chloride extended-release tablets are 156% and 187%, respectively, compared with oxybutynin. The mean pharmacokinetic parameters for R- and S-oxybutynin are summarized in Table 2. The plasma concentration-time profiles for R- and S-oxybutynin are similar in shape; Figure 1 shows the profile for R-oxybutynin.
Table 2: Mean (SD) R- and S-Oxybutynin Pharmacokinetic Parameters Following a Single Dose of oxybutynin chloride extended-release tablets 10 mg (n=43) Parameters (units)    R-Oxybutynin    S-Oxybutynin C max(ng/mL) 1.0 (0.6) 1.8 (1.0) T max(h) 12.7 (5.4) 11.8 (5.3) t 1/2(h) 13.2 (6.2) 12.4 (6.1) AUC (0–48)(ng∙h/mL) 18.4 (10.3) 34.2 (16.9) AUC inf(ng∙h/mL) 21.3 (12.2) 39.5 (21.2)
Figure 1: Mean R-oxybutynin plasma concentrations following a single dose of oxybutynin chloride extended-release tablets 10 mg and oxybutynin 5 mg administered every 8 hours (n=23 for each treatment).
Steady state oxybutynin plasma concentrations are achieved by Day 3 of repeated oxybutynin chloride extended-release tablets dosing, with no observed drug accumulation or change in oxybutynin and desethyloxybutynin pharmacokinetic parameters.
Oxybutynin chloride extended-release tablets steady state pharmacokinetics were studied in 19 children aged 5-15 years with detrusor overactivity associated with a neurological condition (e.g., spina bifida). The children were on oxybutynin chloride extended-release tablets total daily dose ranging from 5 to 20 mg (0.10 to 0.77 mg/kg). Sparse sampling technique was used to obtain serum samples. When all available data are normalized to an equivalent of 5 mg per day of oxybutynin chloride extended-release tablets, the mean pharmacokinetic parameters derived for R- and S-oxybutynin and R- and S-desethyloxybutynin are summarized in Table 3. The plasma-time concentration profiles for R- and S-oxybutynin are similar in shape; Figure 2 shows the profile for R-oxybutynin when all available data are normalized to an equivalent of 5 mg per day.
Table 3: Mean ± SD R- and S-Oxybutynin and R- and S-Desethyloxybutynin Pharmacokinetic Parameters in Children Aged 5–15 Following Administration of 5 to 20 mg oxybutynin chloride extended-release tablets Once Daily (n=19), All Available Data Normalized to an Equivalent of oxybutynin chloride extended-release tablets 5 mg Once Daily R-Oxybutynin S-Oxybutynin R- Desethyloxybutynin S- Desethyloxybutynin C max(ng/mL) 0.7 ± 0.4 1.3 ± 0.8 7.8 ± 3.7 4.2 ± 2.3 T max(h) 5.0 5.0 5.0 5.0 AUC (ng∙h/mL) 12.8 ± 7.0 23.7 ± 14.4 125.1 ± 66.7 73.6 ± 47.7
Figure 2: Mean steady state (± SD) R-oxybutynin plasma concentrations following administration of 5 to 20 mg oxybutynin chloride extended-release tablets once daily in children aged 5–15. Plot represents all available data normalized to an equivalent of oxybutynin chloride extended-release tablets 5 mg once daily.
Food Effects
The rate and extent of absorption and metabolism of oxybutynin are similar under fed and fasted conditions.
Distribution
Oxybutynin is widely distributed in body tissues following systemic absorption. The volume of distribution is 193 L after intravenous administration of 5 mg oxybutynin chloride. Both enantiomers of oxybutynin are highly bound (>99%) to plasma proteins. Both enantiomers of N-desethyloxybutynin are also highly bound (>97%) to plasma proteins. The major binding protein is alpha-1 acid glycoprotein.
Metabolism
Oxybutynin is metabolized primarily by the cytochrome P450 enzyme systems, particularly CYP3A4 found mostly in the liver and gut wall. Its metabolic products include phenylcyclohexylglycolic acid, which is pharmacologically inactive, and desethyloxybutynin, which is pharmacologically active. Following oxybutynin chloride extended-release tablets administration, plasma concentrations of R- and S-desethyloxybutynin are 73% and 92%, respectively, of concentrations observed with oxybutynin.
Excretion
Oxybutynin is extensively metabolized by the liver, with less than 0.1% of the administered dose excreted unchanged in the urine. Also, less than 0.1% of the administered dose is excreted as the metabolite desethyloxybutynin.
Dose Proportionality
Pharmacokinetic parameters of oxybutynin and desethyloxybutynin (Cmax and AUC) following administration of 5-20 mg of oxybutynin chloride extended-release tablets are dose proportional.
Use in Specific Populations
Pediatric
The pharmacokinetics of oxybutynin chloride extended-release tablets were evaluated in 19 children aged 5–15 years with detrusor overactivity associated with a neurological condition (e.g., spina bifida). The pharmacokinetics of oxybutynin chloride extended-release tablets in these pediatric patients were consistent with those reported for adults (see Tables 2and 3, and Figures 1and 2above).
Gender
There are no significant differences in the pharmacokinetics of oxybutynin in healthy male and female volunteers following administration of oxybutynin chloride extended-release tablets.
Race
Available data suggest that there are no significant differences in the pharmacokinetics of oxybutynin based on race in healthy volunteers following administration of oxybutynin chloride extended-release tablets.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
A 24-month study in rats at dosages of oxybutynin chloride of 20, 80, and 160 mg/kg/day showed no evidence of carcinogenicity. These doses are approximately 6, 25, and 50 times the maximum human exposure, based on a human equivalent dose taking into account normalization of body surface area.
Mutagenesis
Oxybutynin chloride showed no increase of mutagenic activity when tested in Schizosaccharomyces pompholiciformis, Saccharomyces cerevisiae, and Salmonella typhimuriumtest systems.
Impairment of fertility
No impairment of fertility was seen in rats at dosages up to 75 mg/kg/day (24 times the MRHD on a mg/m2 basis) when administered for 2 weeks prior to mating in females and for 9 weeks prior to mating in males.
14 Clinical Studies
Oxybutynin chloride extended-release tablets were evaluated for the treatment of patients with overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency in three controlled efficacy studies. The majority of patients were Caucasian (89.0%) and female (91.9%) with a mean age of 59 years (range, 18 to 98 years). Entry criteria required that patients have urge or mixed incontinence (with a predominance of urge) as evidenced by ≥ 6 urge incontinence episodes per week and ≥ 10 micturitions per day. Study 1 was a fixed-dose escalation design, whereas the other two studies used a dose-adjustment design in which each patient's final dose was adjusted to a balance between improvement of incontinence symptoms and tolerability of side effects. All three studies included patients known to be responsive to oxybutynin or other anticholinergic medications, and these patients were maintained on a final dose for up to 2 weeks.
The efficacy results for the three controlled trials are presented in the following Tables 4, 5and 6, and Figures 3, 4and 5
Table 4: Number of Urge Urinary Incontinence Episodes Per Week (Study 1) Study 1 n Oxybutynin ER n Placebo Mean Baseline 34 15.9 16 20.9 Mean (SD) Change from Baseline †34 -15.8 (8.9) 16 -7.6 (8.6) 95% Confidence Interval for Difference (-13.6, -2.8) * (Oxybutynin ER - Placebo)
*The difference between Oxybutynin ER and placebo was statistically significant.
†Covariate adjusted mean with missing observations set to baseline values
Figure 3: Mean Change (±SD) in Urge Urinary Incontinence Episodes Per Week from Baseline (Study 1)

* The difference between Oxybutynin ER and placebo was statistically significant.
Table 5: Number of Urge Urinary Incontinence Episodes Per Week (Study 2) Study 2 n Oxybutynin ER n oxybutynin Mean Baseline 53 27.6 52 23.0 Mean (SD) Change from Baseline †53 -17.6 (11.9) 52 -19.4 (11.9) 95% Confidence Interval for Difference (-2.8, 6.5) (Oxybutynin ER - oxybutynin)
†Covariate adjusted mean with missing observations set to baseline values
Figure 4: Mean Change (±SD) in Urge Urinary Incontinence Episodes Per Week from Baseline (Study 2)
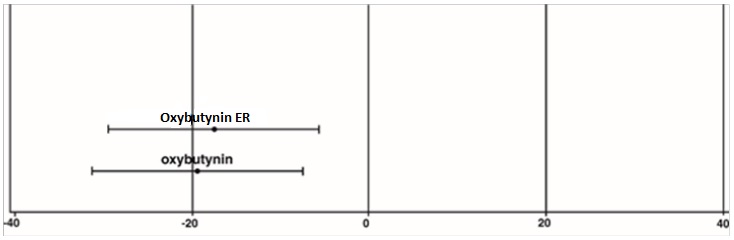
Table 6: Number of Urge Urinary Incontinence Episodes Per Week (Study 3) Study 3 n Oxybutynin ER n oxybutynin Mean Baseline 111 18.9 115 19.5 Mean (SD) Change from Baseline †111 -14.5 (8.7) 115 -13.8 (8.6) 95% Confidence Interval for Difference (-3.0, 1.6) ** (Oxybutynin ER - oxybutynin)
**The difference between Oxybutynin Extended Release Tablets and oxybutynin fulfilled the criteria for comparable efficacy,
†Covariate adjusted mean with missing observations set to baseline values
Figure 5: Mean Change (±SD) in Urge Urinary Incontinence Episodes Per Week from Baseline (Study 3)
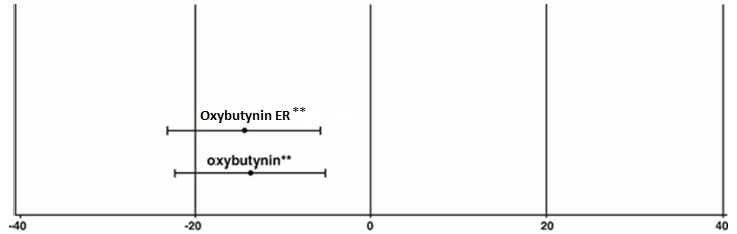
** The difference between oxybutynin ER and oxybutynin fulfilled the criteria for comparable efficacy.
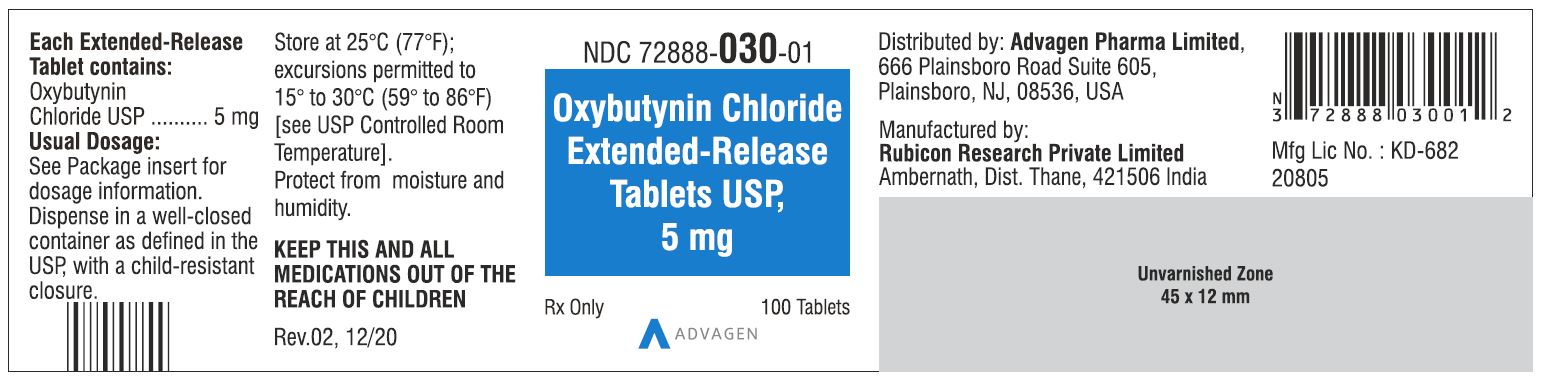
16 How Supplied/storage And Handling
Oxybutynin chloride extended-release tablets, USP are available in three dosage strengths, 5 mg (light pink to pink), 10 mg (light pink to pink) and 15 mg (white to off-white) and imprinted on one side with ‘Λ13’ or ‘Λ14’ or ‘Λ15’ with black ink respectively. Oxybutynin chloride extended-release tablets, USP are supplied in bottles as:
5 mg          100 count bottle                  NDC 72888-030-01
5 mg          500 count bottle                  NDC 72888-030-05
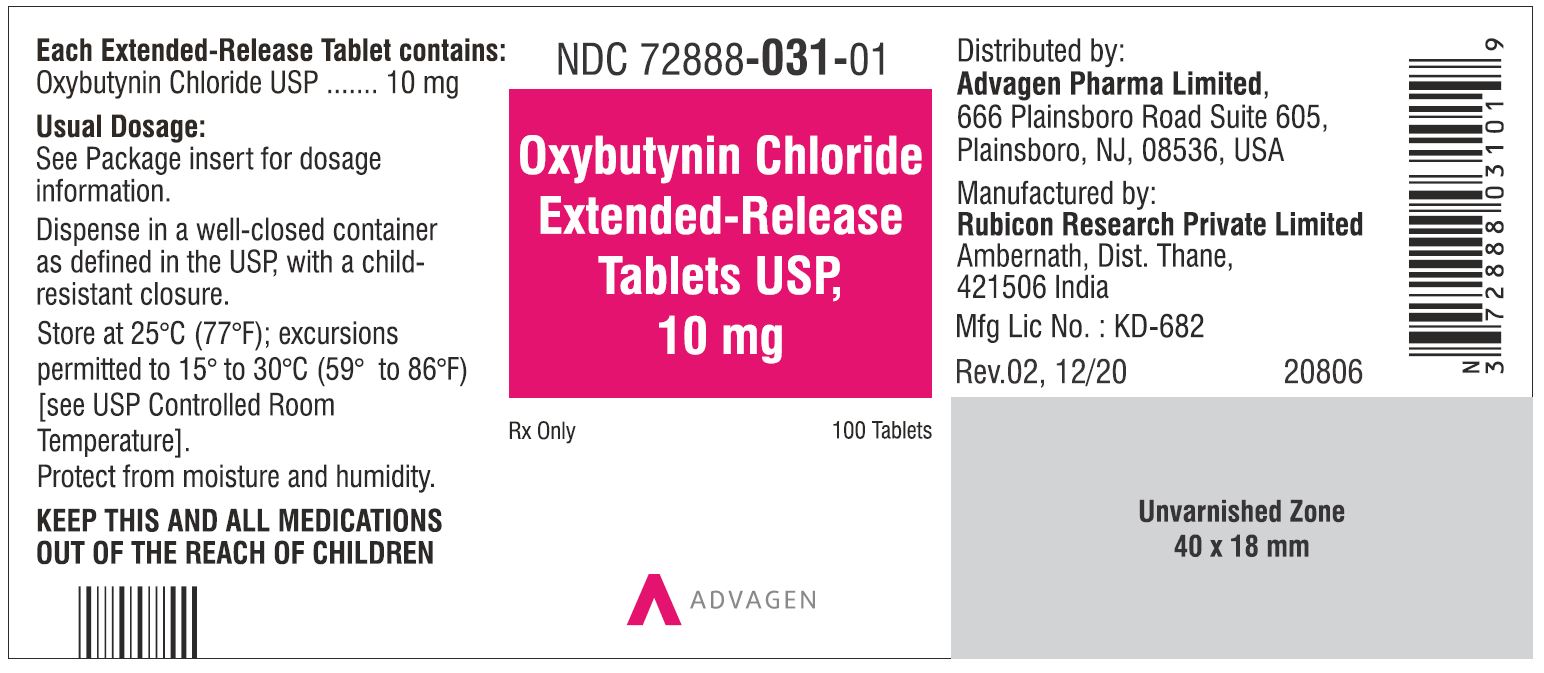
10 mg        100 count bottle                  NDC 72888-031-01
10 mg        500 count bottle                  NDC 72888-031-05
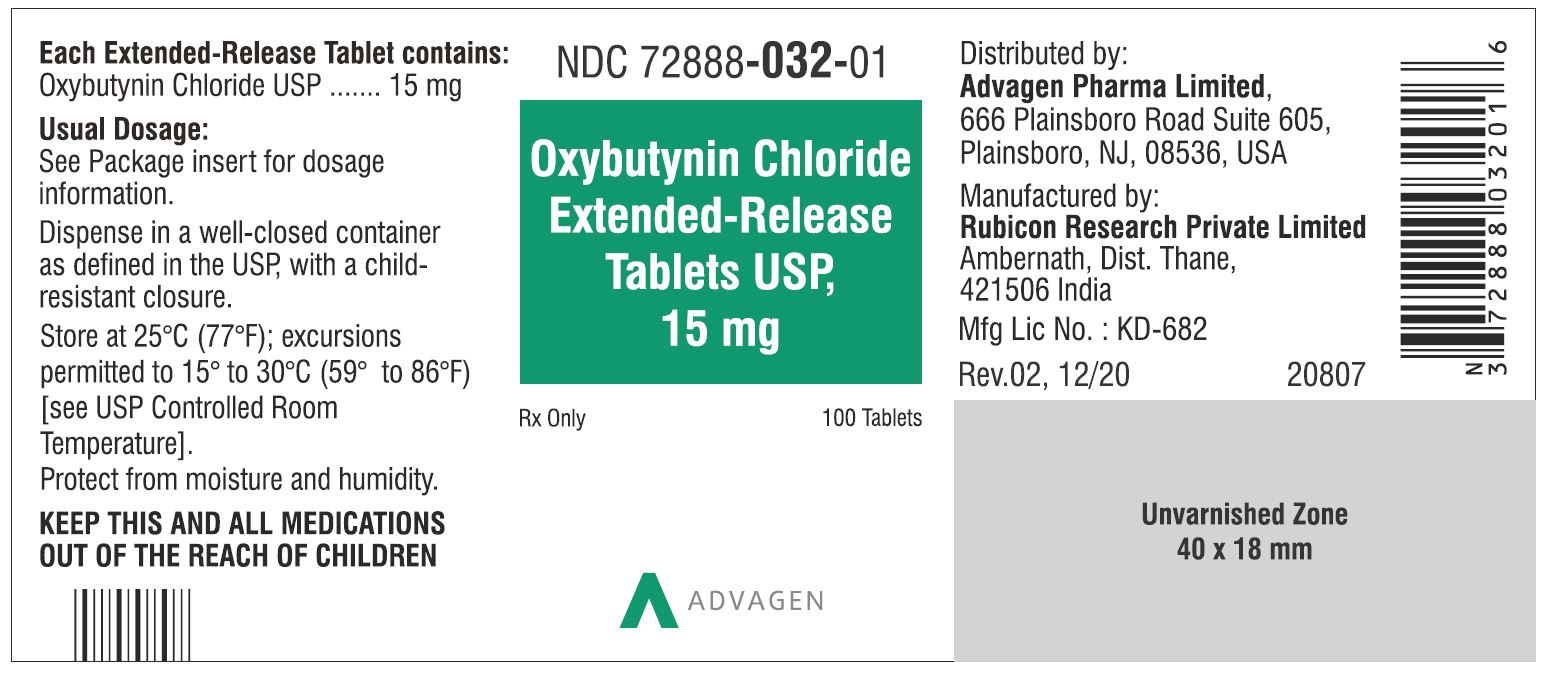
15 mg        100 count bottle                  NDC 72888-032-01
15 mg        500 count bottle                 NDC 72888-032-05
STORAGE AND HANDLING SECTION
Storage
Store at 25°C (77°F); excursions permitted to 15–30°C (59–86°F) [see USP Controlled Room Temperature]. Protect from moisture and humidity.
Keep out of reach of children.
17 Patient Counseling Information
- Patients should be informed that oxybutynin may produce angioedema that could result in life threatening airway obstruction. Patients should be advised to promptly discontinue oxybutynin therapy and seek immediate medical attention if they experience swelling of the tongue, edema of the laryngopharynx, or difficulty breathing.
- Patients should be informed that anticholinergic (antimuscarinic) agents such as oxybutynin chloride extended-release tablets, may produce clinically significant adverse reactions related to anticholinergic activity such as:
- Urinary retention and constipation
- Heat prostration due to decreased sweating. Heat prostration can occur when anticholinergic medicines are administered in the presence of high environmental temperature.
- Patients should be informed that anticholinergic medicines such as oxybutynin chloride extended-release tablets may produce drowsiness (somnolence), dizziness or blurred vision. Patients should be advised to exercise caution in decisions to engage in potentially dangerous activities until oxybutynin chloride extended- release tablets effects have been determined.
- Patients should be informed that alcohol may enhance the drowsiness caused by anticholinergic agents such as oxybutynin chloride extended- release tablets.
- Patients should be informed that oxybutynin chloride extended- release tablets should be swallowed whole with the aid of liquids. Patients should not chew, divide, or crush tablets.
- Oxybutynin chloride extended-release tablets should be taken at approximately the same time each day.
For more information call Advagen Pharma Ltd, at 866-488-0312.
All trademarks are the property of their respective owners.
Distributed by: Advagen Pharma Ltd., East Windsor, NJ 08520, USA
Manufactured by: Rubicon Research Pvt. Ltd., Thane 421506, India.
Rev.: 08, 02/2024
Principal Display Panel - Oxybutynin Chloride Extended Release Tablets, Usp 5 Mg, 10 Mg And 15 Mg
5 mg Tablet Bottle Label - NDC 72888-030-01 - 100 Tablets
5 mg Tablet Bottle Label - NDC 72888-030-05 - 500 Tablets

10 mg Tablet Bottle Label - NDC 72888-031-01 - 100 Tablets
10 mg Tablet Bottle Label - NDC 72888-031-05 - 500 Tablets

15 mg Tablet Bottle Label - NDC 72888-032-01 - 100 Tablets
15 mg Tablet Bottle Label - NDC 72888-032-05 - 500 Tablets

DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


