Rivastigmine Tartrate (rivastigmine tartrate 6 mg) Dailymed
Generic: rivastigmine tartrate is used for the treatment of Alzheimer Disease
IMPRINT: C 94
SHAPE: capsule
COLOR: red
All Imprints
rivastigmine tartrate 1.5 mg - c 91 capsule yellow
rivastigmine tartrate 6 mg - c 94 capsule red
rivastigmine tartrate 4.5 mg - c 93 capsule red
rivastigmine tartrate 3 mg - c 92 capsule orange
Go PRO for all pill images
1 Indicationsand Usage
Rivastigmine tartrate is an acetylcholinesterase inhibitor indicated for treatment of: ‚Äʬ†Mild-to-moderate dementia of the Alzheimer's type¬†(AD)¬†(1.1 ) ‚Äʬ†Mild-to-moderate dementia associated with Parkinson's disease (PD)¬†(1.2 )
1.1 Alzheimer's Disease
Rivastigmine tartrate capsules, USP are indicated for the treatment of mild-to-moderate dementia of the Alzheimer's type (AD).
1.2 Parkinson's Disease Dementia
Rivastigmine tartrate capsules, USP are indicated for the treatment of mild-to-moderate dementia associated with Parkinson's disease (PD).
2 Dosage And Administration
Alzheimer's Disease (2.1 ): ‚ÄĘ Initial Dose:¬†Initiate treatment with 1.5 mg twice a day ‚ÄĘ Dose Titration: After a minimum of 2 weeks, if tolerated, increase dose to 3 mg twice a day and further to 4.5 mg twice a day and 6 mg twice a day if tolerated with a minimum of 2 weeks at each dose (2.1 ) Parkinson's Disease Dementia (PDD) (2.2 ): ‚ÄĘ Initiate treatment with 1.5 mg twice a day ‚ÄĘ After a minimum of 4 weeks, if tolerated, increase dose to 3 mg twice a day and further to 4.5 mg twice a day and 6 mg twice a day if tolerated with a minimum of 4 weeks at each dose (2.2 ) Rivastigmine tartrate capsules should be taken with meals in divided doses in the morning and evening (2.1 ,2.2 ). Rivastigmine tartrate oral solution and rivastigmine tartrate capsules may be interchanged at equal doses. (2.5 )
2.1 Dosing in Alzheimer's Disease
Rivastigmine tartrate capsules should be taken with meals in divided doses in the morning and evening.
The recommended dosage of rivastigmine tartrate capsules in Alzheimer’s disease (AD) is 6 mg to 12 mg per day, administered twice a day (daily doses of 3 mg to 6 mg twice a day). There is evidence from the clinical trials that doses at the higher end of this range may be more beneficial.
Initial Dose
Initiate treatment with the 1.5 mg twice a day with rivastigmine tartrate capsules.
Dose Titration
After a minimum of 2 weeks and if well tolerated, increase the dose to 3 mg twice a day. Subsequent increases to 4.5 mg twice a day and 6 mg twice a day should be attempted after a minimum of 2 weeks at the previous dose and if well tolerated. The maximum dose is 6 mg twice a day (12 mg per day).
2.2 Dosing in Parkinson's Disease Dementia
Rivastigmine tartrate capsules should be taken with meals in divided doses in the morning and evening.
The dosage of rivastigmine tartrate capsules shown to be effective in the single controlled clinical trial conducted in dementia associated with Parkinson’s disease is 3 mg to 12 mg per day, administered twice a day (daily doses of 1.5 mg to 6 mg twice a day).
Initial Dose
Initiate treatment with the 1.5 mg twice a day with rivastigmine tartrate capsules.
Dose Titration
After a minimum of 4 weeks and if well tolerated, increase the dose to 3 mg twice a day. Subsequent increases to 4.5 mg twice a day and 6 mg twice a day should be attempted after a minimum of 4 weeks at the previous dose and if well tolerated. The maximum dose is 6 mg twice a day (12 mg per day).
2.3 Interruption of Treatment
"If adverse effects (e.g., nausea, vomiting, abdominal pain, loss of appetite) cause intolerance during treatment, the patient should be instructed to discontinue treatment for several doses and then restart at the same or next lower dose level.
If dosing is interrupted for 3 days or fewer, restart treatment with the same or lower dose of rivastigmine tartrate capsules. If dosing is interrupted for more than 3 days, treatment should be restarted with 1.5 mg twice a day and titrated as described above [ see Warnings and Precautions (5.1) ].
2.4 Dosing in Specific Populations
Dosing Modifications in Patients with Renal Impairment
Patients with moderate and severe renal impairment may be able to only tolerate lower doses.
Dosing Modifications in Patients with Hepatic Impairment
Patients with mild (Child-Pugh score 5 to 6) and moderate (Child-Pugh score 7 to 9) hepatic impairment may be able to only tolerate lower doses. No data are available on the use of rivastigmine in patients with severe hepatic impairment.
Dosing Modifications in Patients with Low Body Weight
Carefully titrate and monitor patients with low body weight (less than 50 kg) for toxicities (e.g., excessive nausea, vomiting), and consider reducing the dose if such toxicities develop.
2.5 Important Administration Instructions
Rivastigmine tartrate oral solution and rivastigmine tartrate capsules may be interchanged at equal doses.
3 Dosage Forms And Strengths
‚ÄĘ Capsules: 1.5 mg, 3 mg, 4.5 mg, or 6 mg (3.1 )
3.1 Rivastigmine tartrate capsules
Capsules, containing rivastigmine tartrate equivalent to 1.5 mg, 3 mg, 4.5 mg, or 6 mg of rivastigmine base, are available as follows:      1.5 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with yellow opaque color cap and yellow opaque color body imprinted "C 91".     3 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with orange opaque color cap and orange opaque color body imprinted "C 92".     4.5 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with red opaque color cap and red opaque color body imprinted "C 93".     6 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with red opaque color cap and orange opaque color body imprinted "C 94".
4 Contraindications
¬†Rivastigmine tartrate capsules are contraindicated in patients with: ‚ÄĘ known hypersensitivity to rivastigmine, other carbamate derivatives or other components of the formulation [see Description (11)]. ‚ÄĘ a previous history of application site reaction with rivastigmine transdermal patch suggestive of allergic contact dermatitis, in the absence of negative allergy testing [see Warnings and Precautions (5.2)]. Isolated cases of generalized skin reactions have been described in postmarketing experience [see Adverse Reactions (6.2)].
‚ÄĘ Known hypersensitivity to rivastigmine, other carbamate derivatives or other components of the formulation. (4 ) ‚ÄĘ History of application site reaction with rivastigmine transdermal patch suggestive of allergic contact dermatitis, in the absence of negative allergy testing. (4 ,5.2 )
5 Warnings And Precautions
‚ÄĘ Gastrointestinal adverse reactions may include significant nausea, vomiting, diarrhea, anorexia/decreased appetite, and weight loss, and may necessitate treatment interruption. Dehydration may result from prolonged vomiting or diarrhea and can be associated with serious outcomes. (5.1 ) ‚ÄĘ Discontinue rivastigmine in case of disseminated allergic dermatitis, which may occur after oral or transdermal administration (4 ,5.2 ). In patients with suspected allergic contact dermatitis after transdermal rivastigmine use, switch to oral rivastigmine only after negative allergy testing.
5.1 Gastrointestinal Adverse Reactions
Rivastigmine tartrate can cause gastrointestinal adverse reactions, including significant nausea, vomiting, diarrhea, anorexia/decreased appetite, and weight loss. Dehydration may result from prolonged vomiting or diarrhea and can be associated with serious outcomes. The incidence and severity of these reactions are dose-related [see Adverse Reactions (6.1)]. For this reason, patients should always be started at a dose of 1.5 mg twice a day and titrated to their maintenance dose.
If treatment is interrupted for longer than 3 days, treatment should be reinitiated with the lowest daily dose [ see Dosage and Administration (2.3) ] to reduce the possibility of severe vomiting and its potentially serious sequelae (e.g., there has been one postmarketing report of severe vomiting with esophageal rupture following inappropriate reinitiation of treatment with a 4.5 mg dose after 8 weeks of treatment interruption).
Inform caregivers to monitor for gastrointestinal adverse reactions and to inform the physician if they occur. It is critical to inform caregivers that if therapy has been interrupted for more than 3 days because of intolerance, the next dose should not be administered without contacting the physician regarding proper retitration.
5.2 Allergic Dermatitis
There have been isolated postmarketing reports of patients experiencing disseminated allergic dermatitis when administered rivastigmine irrespective of the route of administration (oral or transdermal). Treatment should be discontinued if disseminated allergic dermatitis occurs [see Contraindications (4)]. Patients and caregivers should be instructed accordingly [ see Patient Counseling Information (17)].
In patients who develop application site reactions, suggestive of allergic contact dermatitis to rivastigmine tartrate patch and who still require rivastigmine, treatment should be switched to oral rivastigmine only after negative allergy testing and under close medical supervision. It is possible that some patients sensitized to rivastigmine by exposure to rivastigmine patch may not be able to take rivastigmine in any form.
5.3 Other Adverse Reactions from Increased Cholinergic Activity
Neurologic Effects
Extrapyramidal Symptoms: Cholinomimetics, including rivastigmine may exacerbate or induce extrapyramidal symptoms. Worsening of parkinsonian symptoms, particularly tremor has been observed in patients with dementia associated with Parkinson’s disease who were treated with rivastigmine tartrate capsules.
Seizures: Drugs that increase cholinergic activity are believed to have some potential for causing seizures. However, seizure activity also may be a manifestation of Alzheimer's disease.
Peptic Ulcers/Gastrointestinal Bleeding
Cholinesterase inhibitors, including rivastigmine, may be expected to increase gastric acid secretion due to increased cholinergic activity. Monitor patients using rivastigmine tartrate for symptoms of active or occult gastrointestinal bleeding, especially those at increased risk for developing ulcers, e.g., those with a history of ulcer disease or those receiving concurrent nonsteroidal anti-inflammatory drugs (NSAIDs). Clinical studies of rivastigmine have shown no significant increase, relative to placebo, in the incidence of either peptic ulcer disease or gastrointestinal bleeding.
Use with Anesthesia
Rivastigmine, as a cholinesterase inhibitor, is likely to exaggerate succinylcholine-type muscle relaxation during anesthesia.
Cardiac Conduction Effects
Because rivastigmine increases cholinergic activity, use of rivastigmine may have vagotonic effects on heart rate (e.g., bradycardia). The potential for this action may be particularly important in patients with sick sinus syndrome or other supraventricular cardiac conduction conditions. In clinical trials, rivastigmine was not associated with any increased incidence of cardiovascular adverse events, heart rate or blood pressure changes, or electrocardiogram (ECG) abnormalities. Syncopal episodes have been reported in 3% of patients receiving 6 mg to 12 mg per day of rivastigmine tartrate, compared to 2% of placebo patients.
Genitourinary Effects
Although not observed in clinical trials of rivastigmine, drugs that increase cholinergic activity may cause urinary obstruction.
Pulmonary Effects
Drugs that increase cholinergic activity, including rivastigmine, should be used with care in patients with a history of asthma or obstructive pulmonary disease.
5.4 Impairment in Driving or Use of Machinery
Dementia may cause gradual impairment of driving performance or compromise the ability to use machinery. The administration of rivastigmine may also result in adverse reactions that are detrimental to these functions. During treatment with the rivastigmine tartrate capsules, routinely evaluate the patient’s ability to continue driving or operating machinery.
6 Adverse Reactions
The following adverse reactions are described below and elsewhere in the labeling:
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.1)]
- Allergic Dermatitis [see Warnings and Precautions (5.2)]
- Other Adverse Reactions from Increased Cholinergic Activity [see Warnings and Precautions (5.3)]
Most common adverse reactions (greater than 5% and 2 times greater than placebo): nausea, vomiting, anorexia, dyspepsia, and asthenia (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact Cadila Pharmaceuticals Limited at 1-202-355-9785 (fax 1-202-355-9784) or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch .
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Rivastigmine tartrate capsules have been administered to over 5,297 individuals during clinical trials worldwide. Of these, 4,326 patients have been treated for at least 3 months, 3,407 patients have been treated for at least 6 months, 2,150 patients have been treated for 1 year, 1,250 patients have been treated for 2 years, and 168 patients have been treated for over 3 years. With regard to exposure to the highest dose, 2,809 patients were exposed to doses of 10 mg to 12 mg, 2,615 patients treated for 3 months, 2,328 patients treated for 6 months, 1,378 patients treated for 1 year, 917 patients treated for 2 years, and 129 patients treated for over 3 years.
Mild-to-Moderate Alzheimer’s Disease
Most Common Adverse Reactions
The most common adverse reactions, defined as those occurring at a frequency of at least 5% and twice the placebo rate, are largely predicted by rivastigmine tartrate's cholinergic effects. These include nausea, vomiting, anorexia, dyspepsia, and asthenia.
Gastrointestinal Adverse Reactions
Rivastigmine tartrate use is associated with significant nausea, vomiting, and weight loss [see Warnings and Precautions (5.1)].
Discontinuation Rates
The rate of discontinuation due to adverse events in controlled clinical trials of rivastigmine tartrate was 15% for patients receiving 6 mg to 12 mg per day compared to 5% for patients on placebo during forced weekly dose titration. While on a maintenance dose, the rates were 6% for patients on rivastigmine tartrate compared to 4% for those on placebo.
The most common adverse reactions leading to discontinuation, defined as those occurring in at least 2% of patients and at twice the incidence seen in placebo patients, are shown in Table 1.
Table 1: Most Frequent Adverse Reactions Leading to Withdrawal from Clinical Trials during Titration and Maintenance in Patients Receiving 6 mg to 12 mg per day  Rivastigmine tartrate  Using a Forced-Dose Titration
Study Phase ¬† Titration¬† Maintenance¬† Overall¬† Rivastigmine tartrate ‚Č• 6 to 12 mg/day (n = 1,189) ¬† Placebo (n = 868) ¬† Rivastigmine tartrate¬†¬†¬†¬†¬†¬† ‚Č• 6 to 12 mg/day (n = 987) Placebo (n = 788) ¬† Rivastigmine tartrate¬†¬†¬†¬†¬†¬† ‚Č• 6¬†to 12 mg/day (n = 1,189) Placebo (n = 868) ¬† Event/% Discontinuing ¬† ¬† ¬† ¬† Nausea 8 <1 1 <1 8 1 Vomiting 4 <1 1 <1 5 <1 Anorexia 2 0 1 <1 3 <1 Dizziness 2 <1 1 <1 2 <1
Adverse Reactions Observed at an Incidence of at Least 2%
Table 2 uls adverse reactions that occurred in at least 2% of patients in placebo-controlled trials, and for which the rate of occurrence was greater for patients treated with rivastigmine tartratedoses of 6 mg to 12 mg per day than for those treated with placebo.
In general, adverse reactions were less frequent later in the course of treatment.
No systematic effect of race or age could be determined from the incidence of adverse reactions in the controlled studies. Nausea, vomiting and weight loss were more frequent in women than men.
Table 2: Proportion of Adverse Reactions Observed with a Frequency of Greater Than  or Equal to 2% and at a Rate Greater than Placebo in Clinical Trials
Body System/Adverse Reaction Rivastigmine tartrate (6-12 mg/day) (n = 1,189) Placebo (n = 868) Percent of Patients with any Adverse Event 92 79 Autonomic Nervous System Sweating IncreasedSyncope  43  12 Body as a Whole FatigueAstheniaMalaiseDecreased Weight**  9653  522< 1 Cardiovascular Disorders , General Hypertension  3  2 Central and Peripheral Nervous Sys tem DizzinessHeadacheSomnolenceTremor  211754  111231 Gastrointestinal System Nausea*Vomiting*DiarrheaAnorexia***Abdominal PainDyspepsia  47311917139  12611364 Psychiatric Disorders InsomniaConfusionDepressionAnxietyHallucinationAggressive Reaction  986543  774332 Resistance Mechanism Disorders Urinary Tract Infection  7  6
*Nausea and Vomiting: In the controlled clinical trials, 47% of the patients treated with rivastigmine tartrate dose in the therapeutic range of 6 mg to 12 mg per day (n = 1189) developed nausea (compared with 12% in placebo). A total of 31% of rivastigmine tartrate treated patients developed at least 1 episode of vomiting (compared with 6% for placebo). The rate of vomiting was higher during the titration phase (24% versus 3% for placebo) than in the maintenance phase (14% versus 3% for placebo). The rates were higher in women than men. Five percent of patients discontinued for vomiting, compared to less than 1% for patients on placebo. Vomiting was severe in 2% of rivastigmine tartrate treated patients and was rated as mild or moderate each in 14% of patients. The rate of nausea was higher during the titration phase (43% versus 9% for placebo) than in the maintenance phase (17% versus 4% for placebo).
**Weight Decreased: In the controlled trials, approximately 26% of women on high doses of rivastigmine tartrate (greater than 9 mg per day) had weight loss equal to or greater than 7% of their baseline weight compared to 6% in the placebo-treated patients. About 18% of the males in the high-dose group experienced a similar degree of weight loss compared to 4% in placebo-treated patients. It is not clear how much of the weight loss was associated with anorexia, nausea, vomiting, and the diarrhea associated with the drug.
***Anorexia: In the controlled clinical trials, of the patients treated with a rivastigmine tartrate dose of 6 mg to 12 mg per day, 17% developed anorexia compared to 3% of the placebo patients. Neither the time course nor the severity of the anorexia is known.
Mild-to-Moderate Parkinson’s Disease Dementia
Rivastigmine tartrate capsules have been administered to 779 individuals during clinical trials worldwide. Of these, 663 patients have been treated for at least 3 months, 476 patients have been treated for at least 6 months, and 313 patients have been treated for 1 year.
Most Common Adverse Reactions
The most common adverse reactions, defined as those occurring at a frequency of at least 5% and twice the placebo rate, are largely predicted by rivastigmine tartrate's cholinergic effects. These include nausea, vomiting, tremor, anorexia, and dizziness.
Discontinuation Rates
The rate of discontinuation due to adverse events in the single placebo-controlled trial of rivastigmine tartrate was 18% for patients receiving 3 mg to 12 mg per day compared to 11% for patients on placebo during the 24-week study.
The most frequent adverse reactions that led to discontinuation from this study, defined as those occurring in at least 1% of patients receiving rivastigmine tartrate and more frequent than those receiving placebo, were nausea (3.6% rivastigmine tartrate versus 0.6% placebo), vomiting (1.9% rivastigmine tartrate versus 0.6% placebo), and tremor (1.7% rivastigmine tartrate versus 0.0% placebo).
Adverse Reactions Observed at an Incidence of at Least 2%
Table 3 uls adverse reactions that occurred in at least 2% of patients in a single placebo-controlled trial and during the first 24 weeks of a 76-week open-label active-controlled trial for which the rate of occurrence was greater for patients treated with rivastigmine tartrate doses of 3 mg to 12 mg per day than for those treated with placebo in the placebo-controlled trial.
In general, adverse reactions were less frequent later in the course of treatment.
Table 3: Proportion of Adverse Reactions Observed at a Frequency Greater Than or Equal to 2% and Occurring at Rate Greater than Placebo in Clinical Trials
  Active-Controlled Study Placebo-Controlled Study Body System/Adverse Reaction rivastigmine tartrate (3 to 2 mg/day) (n = 294) rivastigmine tartrate (3 to 12 mg/day) (n = 362) Placebo (n = 179) Percent of Patients with any Adverse Event 88 84 71 Gastrointestinal     Disorders Nausea Vomiting Diarrhea Upper Abdominal Pain Salivary hypersecretion   3813842   2917741   112410 General Disorders and Administrative Site Conditions FallFatigue Asthenia    1054    642    631 Metabolism and Nutritional Disorders Anorexia  Decreased Appetite Dehydration   -51   682   351 Nervous System Disorders Tremor Dizziness Headache Somnolence Parkinson’s Disease (worsening) Bradykinesia Dyskinesia Cogwheel rigidity Hypokinesia Parkinsonism  23846-*   3332-  106443 31112  41331 21001 Psychiatric Disorders Anxiety Insomnia Restlessness  421  433  122 Skin and Subcutaneous Tissue Disorders Increased Sweating   2    2   1
*Parkinson’s disease (worsening) in the active-controlled study was assessed by reported pre-identified adverse events (tremor, cogwheel rigidity, fall), each of them uled with corresponding frequencies.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of rivastigmine tartrate capsules. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Cardiac Disorders: Tachycardia Hepatobiliary Disorders: Abnormal liver function tests, hepatitis Nervous System Disorders: seizure Psychiatric Disorders: Aggression, nightmares Skin and Subcutaneous Tissue Disorders: Allergic dermatitis, application site hypersensitivity (patch), buler, disseminated allergic dermatitis, Stevens-Johnson syndrome, urticaria
7 Drug Interactions
Concomitant use with metoclopramide, beta-blockers, or cholinomimetic and anticholinergic drugs is not recommended (7.1 ,7.2 ,7.3 )
7.1 Metoclopramide
Due to the risk of additive extrapyramidal adverse reactions, the concomitant use of metoclopramide and rivastigmine tartrate is not recommended.
7.2 Cholinomimetic and Anticholinergic Medications
Rivastigmine tartrate may increase the cholinergic effects of other cholinomimetic medications and may also interfere with the activity of anticholinergic medications (e.g., oxybutynin, tolterodine). Concomitant use of rivastigmine tartrate with medications having these pharmacologic effects is not recommended unless deemed clinically necessary [see Warnings and Precautions (5.3)].
7.3 Beta-blockers
Additive bradycardic effects resulting in syncope may occur when rivastigmine tartrate is used concomitantly with beta-blockers, especially cardioselective beta-blockers (including atenolol). Concomitant use of rivastigmine tartrate with beta-blockers is not recommended.
8 Use In Specific Populations
8.1 Pregnancy
Risk Summary There are no adequate data on the developmental risks associated with the use of rivastigmine tartrate in pregnant women. In animals, no adverse effects on embryo-fetal development were observed at oral doses 2-4 times the maximum recommended human dose (MRHD) (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
Data Animal Data Oral administration of rivastigmine to pregnant rats and rabbits throughout organogenesis produced no adverse effects on embryo-fetal development up to the highest dose tested (2.3 mg/kg/day), which is 2 and 4 times, respectively, the MRHD of 12 mg per day on a body surface area (mg/m2) basis.
8.2 Lactation
Risk Summary
There are no data on the presence of rivastigmine in human milk, the effects on the breastfed infant, or the effects of rivastigmine on milk production. Rivastigmine and its metabolites are excreted in rat milk following oral administration of rivastigmine; levels of rivastigmine plus metabolites in rat milk are approximately 2 times that in maternal plasma.
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for rivastigmine tarterate and any potential adverse effects on the breastfed infant from rivastigmine tarterate or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established. The use of rivastigmine tartrate in pediatric patients (below 18 years of age) is not recommended.
8.5 Geriatric Use
Of the total number of patients in clinical studies of rivastigmine tartrate, 86 % were 65 years and older while 46 % were 75 years and older. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
Patients with moderate to severe renal impairment may be able to only tolerate lower doses [see Dosage and Administration (2.4), and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Patients with mild or moderate hepatic impairment may be able to only tolerate lower doses [see Dosage and Administration (2.4), and Clinical Pharmacology (12.3)]. No data are available on the use of rivastigmine tartrate in patients with severe hepatic impairment.
8.8 Low or High Body Weight
Because rivastigmine blood levels vary with weight, careful titration and monitoring should be performed in patients with low or high body weights [see Dosage and Administration (2.4), and Clinical Pharmacology (12.3)].
10 Overdosage
Because strategies for the management of overdose are continually evolving, it is advisable to contact a Poison Control Center to determine the latest recommendations for the management of an overdose of any drug.
As rivastigmine has a short plasma half-life of about 1 hour and a moderate duration of acetylcholinesterase inhibition of 8 to 10 hours, it is recommended that in cases of asymptomatic overdoses, no further dose of rivastigmine tartrate should be administered for the next 24 hours.
As in any case of overdose, general supportive measures should be utilized.
Overdosage with cholinesterase inhibitors can result in cholinergic crisis characterized by severe nausea, vomiting, salivation, sweating, bradycardia, hypotension, respiratory depression, collapse and convulsions. Increasing muscle weakness is a possibility and may result in death if respiratory muscles are involved. Atypical responses in blood pressure and heart rate have been reported with other drugs that increase cholinergic activity when coadministered with quaternary anticholinergics such as glycopyrrolate. Additional symptoms associated with rivastigmine overdose are diarrhea, abdominal pain, dizziness, tremor, headache, somnolence, confusional state, hyperhidrosis, hypertension, hallucinations and malaise. Due to the short half-life of rivastigmine, dialysis (hemodialysis, peritoneal dialysis, or hemofiltration) would not be clinically indicated in the event of an overdose.
In overdoses accompanied by severe nausea and vomiting, the use of antiemetics should be considered. A fatal outcome has been rarely reported with rivastigmine.
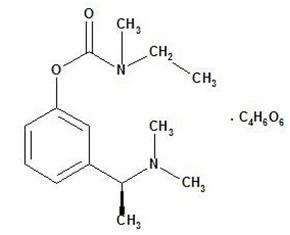
11 Description
Rivastigmine tartrate is a reversible cholinesterase inhibitor and is known chemically as (S)-N-Ethyl-N-methyl-3-[1-(dimethylamino)ethyl]-phenyl carbamate hydrogen-(2R,3R)-tartrate. Rivastigmine tartrate is commonly referred to in the pharmacological literature as SDZ ENA 713 or ENA 713. It has an empirical formula of C14H22N2O2 ‚ÄĘ C4H6O6 (hydrogen tartrate salt-hta salt) and a molecular weight of 400.43 g/mol (hta salt). Rivastigmine tartrate is a white to off-white, fine crystalline powder that is very soluble in water, soluble in ethanol and acetonitrile, slightly soluble in n-octanol and very slightly soluble in ethyl acetate.
The distribution coefficient at 37¬įC in n-octanol/phosphate buffer solution pH 7 is 3.0.
Rivastigmine tartrate capsules, USP contain rivastigmine tartrate, equivalent to 1.5 mg, 3 mg, 4.5 mg, and 6 mg of rivastigmine base for oral administration. Inactive ingredients are hydroxypropyl methylcellulose, magnesium stearate, microcrystalline cellulose, and colloidal silicon dioxide. Each hard-gelatin capsule contains gelatin, titanium dioxide and red and/or yellow iron oxides.
12 Clinical Pharmacology
12.1 Mechanism of Action
Although the precise mechanism of action of rivastigmine is unknown, it is thought to exert its therapeutic effect by enhancing cholinergic function. This is accomplished by increasing the concentration of acetylcholine through reversible inhibition of its hydrolysis by cholinesterase. Therefore, the effect of rivastigmine may lessen as the disease process advances and fewer cholinergic neurons remain functionally intact. There is no evidence that rivastigmine alters the course of the underlying dementing process.
12.2 Pharmacodynamics
After a 6 mg dose of rivastigmine, anticholinesterase activity is present in cerebrospinal fluid (CSF) for about 10 hours, with a maximum inhibition of about 60% 5 hours after dosing.
In vitro and in vivo studies demonstrate that the inhibition of cholinesterase by rivastigmine is not affected by the concomitant administration of memantine, an N-methyl-D-aspartate receptor antagonist.
12.3 Pharmacokinetics
Rivastigmine shows linear pharmacokinetics up to 3 mg twice a day but is nonlinear at higher doses. Doubling the dose from 3 mg to 6 mg twice a day results in a 3-fold increase in area under the curve (AUC). The elimination half-life is about 1.5 hours, with most elimination as metabolites via the urine.
Absorption
Rivastigmine is rapidly and completely absorbed. Peak plasma concentrations are reached in approximately 1 hour. Absolute bioavailability after a 3-mg dose is about 36%. Administration of rivastigmine tartrate with food delays absorption (Tmax) by 90 minutes lowers Cmax by approximately 30% and increases AUC by approximately 30%.
Distribution
Rivastigmine is weakly bound to plasma proteins (approximately 40%) over the therapeutic range. It readily crosses the blood-brain barrier, reaching CSF peak concentrations in 1.4 to 2.6 hours. It has an apparent volume of distribution (VD) in the range of 1.8 to 2.7 L/kg.
Metabolism
Rivastigmine is rapidly and extensively metabolized, primarily via cholinesterase-mediated hydrolysis to the decarbamylated metabolite. Based on evidence from in vitro and animal studies, the major cytochrome P450 isozymes are minimally involved in rivastigmine metabolism. Consistent with these observations is the finding that no drug interactions related to cytochrome P450 have been observed in humans.
Elimination
The major pathway of elimination is via the kidneys. Following administration of 14C-rivastigmine to 6 healthy volunteers, total recovery of radioactivity over 120 hours was 97% in urine and 0.4% in feces. No parent drug was detected in urine. The sulfate conjugate of the decarbamylated metabolite is the major component excreted in urine and represents 40% of the dose. Mean oral clearance of rivastigmine is 1.8 ¬Ī 0.6 L/min after 6 mg twice a day.
Age
Following a single 2.5-mg oral dose to elderly volunteers (60 years and older, n = 24) and younger volunteers (n = 24), mean oral clearance of rivastigmine was 30% lower in elderly (7 L/min) than in younger subjects (10 L/min). 
Gender and Race
Population pharmacokinetic analysis of oral rivastigmine indicated that neither gender (n = 277 males and 348 females) nor race (n = 575 Caucasian, 34 Black, 4 Asian, and 12 Other) affected clearance of the drug. 
Body Weight
A relationship between drug exposure at steady-state (rivastigmine and metabolite NAP226-90) and body weight was observed in Alzheimer's dementia patients. Rivastigmine exposure is higher in subjects with low body weight. Compared to a patient with a body weight of 65 kg, the rivastigmine steady-state concentrations in a patient with a body weight of 35 kg would be approximately doubled, while for a patient with a body weight of 100 kg the concentrations would be approximately halved. 
Renal Impairment
Following a single 3-mg dose, mean oral clearance of rivastigmine is 64% lower in moderately impaired renal patients (n = 8, GFR = 10 to 50 mL/min) than in healthy subjects (n = 10, GFR greater than or equal to 60 mL/min); CL/F=1.7 L/min and 4.8 L/min, respectively. In patients with severe renal impairment (n = 8, GFR less than 10 mL/min), mean oral clearance of rivastigmine is 43% higher than in healthy subjects (n = 10, GFR greater than or equal to 60 mL/min); CL/F = 6.9 L/min and 4.8 L/min, respectively. For unexplained reasons, the severely impaired renal patients had a higher clearance of rivastigmine than moderately impaired patients.
Hepatic Impairment
Following a single 3-mg dose, mean oral clearance of rivastigmine was 60% lower in hepatically impaired patients (n = 10, biopsy proven) than in healthy subjects (n = 10). After multiple 6-mg twice a day oral dosing, the mean clearance of rivastigmine was 65% lower in mild (n = 7, Child-Pugh score 5 to 6), and moderate (n = 3, Child-Pugh score 7 to 9) hepatically impaired patients (biopsy proven, liver cirrhosis) than in healthy subjects (n = 10).
Smoking
Following oral rivastigmine administration (up to 12 mg per day) with nicotine use, population pharmacokinetic analysis showed increased oral clearance of rivastigmine by 23% (n = 75 smokers and 549 nonsmokers).
Drug Interaction Studies
Effect of Rivastigmine on the Metabolism of Other Drugs
Rivastigmine is primarily metabolized through hydrolysis by esterases. Minimal metabolism occurs via the major cytochrome P450 isoenzymes. Based on in vitro studies, no pharmacokinetic drug interactions with drugs metabolized by the following isoenzyme systems are expected: CYP1A2, CYP2D6, CYP3A4/5, CYP2E1, CYP2C9, CYP2C8, CYP2C19, or CYP2B6.
No pharmacokinetic interaction was observed between rivastigmine taken orally and digoxin, warfarin, diazepam or fluoxetine in studies in healthy volunteers. The increase in prothrombin time induced by warfarin is not affected by administration of rivastigmine.
Effect of Other Drugs on the Metabolism of Rivastigmine
Drugs that induce or inhibit CYP450 metabolism are not expected to alter the metabolism of rivastigmine.
Population pharmacokinetic analysis with a database of 625 patients showed that the pharmacokinetics of rivastigmine taken orally were not influenced by commonly prescribed medications such as antacids (n = 77), antihypertensives (n = 72), beta-blockers (n = 42), calcium channel blockers (n = 75), antidiabetics (n = 21), NSAIDs (n = 79), estrogens (n = 70), salicylate analgesics (n = 177), antianginals (n = 35) and antihistamines (n = 15).
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis & Impairment of Fertility
Carcinogenesis
In oral carcinogenicity studies conducted at doses up to 1.1 mg/kg/day in rats and 1.6 mg/kg/day in mice, rivastigmine was not carcinogenic. These doses are less than the maximum recommended human dose (MRHD) of 12 mg per day on a mg/m2 basis.
Mutagenesis
Rivastigmine was clastogenic in in vitro chromosomal aberration assays in mammalian cells in the presence, but not the absence, of metabolic activation. Rivastigmine was negative in an in vitro bacterial reverse mutation (Ames) assay, an in vitro HGPRT assay, and in an in vivo mouse micronucleus test.
Impairment of Fertility
Rivastigmine had no effect on fertility or reproductive performance in rats at oral doses up to 1.1 mg/kg/day, a dose less than the MRHD on a mg/m2 basis.
14 Clinical Studies
Mild-to-Moderate Alzheimer's Disease The effectiveness of rivastigmine tartrate as a treatment for Alzheimer's disease is demonstrated by the results of 2 randomized, double-blind, placebo-controlled clinical investigations (Study 1 and Study 2) in patients with Alzheimer's disease [diagnosed by NINCDS-ADRDA and DSM-IV criteria, Mini-Mental State Examination (MMSE) greater than or equal to10 and less than or equal to 26, and the Global Deterioration Scale (GDS)]. The mean age of patients participating in rivastigmine tartrate trials was 73 years with a range of 41 to 95. Approximately 59% of patients were women and 41% were men. The racial distribution was Caucasian 87%, Black 4%, and other races 9%.
In each study, the effectiveness of rivastigmine tartrate was evaluated using a dual outcome assessment strategy.
The ability of rivastigmine tartrate to improve cognitive performance was assessed with the cognitive subscale of the Alzheimer's Disease Assessment Scale (ADAS-cog), a multi-li instrument that has been extensively validated in longitudinal cohorts of Alzheimer's disease patients. The ADAS-cog examines selected aspects of cognitive performance including elements of memory, orientation, attention, reasoning, language, and praxis. The ADAS-cog scoring range is from 0 to 70, with higher scores indicating greater cognitive impairment. Elderly normal adults may score as low as 0 or 1, but it is not unusual for non-demented adults to score slightly higher.
The patients recruited as participants in each study had mean scores on ADAS-cog of approximately 23 units, with a range from 1 to 61. Experience gained in longitudinal studies of ambulatory patients with mild-to-moderate Alzheimer's disease suggests that they gain 6 to 12 units a year on the ADAS-cog. Lesser degrees of change, however, are seen in patients with very mild or very advanced disease because the ADAS-cog is not uniformly sensitive to change over the course of the disease. The annualized rate of decline in the placebo patients participating in rivastigmine tartrate trials was approximately 3 to 8 units per year.
The ability of rivastigmine tartrate to produce an overall clinical effect was assessed using a Clinician's Interview-Based Impression of Change (CIBIC) that required the use of caregiver information, the CIBIC-Plus. The CIBIC-Plus is not a single instrument and is not a standardized instrument like the ADAS-cog. Clinical trials for investigational drugs have used a variety of CIBIC formats, each different in terms of depth and structure. As such, results from a CIBIC-Plus reflect clinical experience from the trial or trials in which it was used and cannot be compared directly with the results of CIBIC-Plus evaluations from other clinical trials. The CIBIC-Plus used in the rivastigmine tartrate trials was a structured instrument based on a comprehensive evaluation at baseline and subsequent time-points of 3 domains: patient cognition, behavior and functioning, including assessment of activities of daily living. It represents the assessment of a skilled clinician using validated scales based on his/her observation at interviews conducted separately with the patient and the caregiver familiar with the behavior of the patient over the interval rated. The CIBIC-Plus is scored as a 7-point categorical rating, ranging from a score of 1, indicating "markedly improved," to a score of 4, indicating "no change" to a score of 7, indicating "marked worsening." The CIBIC-Plus has not been systematically compared directly to assessments not using information from caregivers or other global methods.
U.S.26-Week Study of Rivastigmine tartrate in Mild-to-Moderate Alzheimer's Disease (Study 1)
In a study of 26 weeks duration, 699 patients were randomized to either a dose range of 1 mg to 4 mg or 6 mg to 12 mg of rivastigmine tartrate per day or to placebo, each given in divided doses. The 26-week study was divided into a 12-week forced-dose titration phase and a 14-week maintenance phase. The patients in the active treatment arms of the study were maintained at their highest tolerated dose within the respective range.
Figure 1 illustrates the time course for the change from baseline in ADAS-cog scores for all 3 dose groups over the 26 weeks of the study. At 26 weeks of treatment, the mean differences in the ADAS-cog change scores for the rivastigmine tartrate-treated patients compared to the patients on placebo were 1.9 and 4.9 units for the 1 mg to 4 mg and 6 mg to 12 mg treatments, respectively. Both treatments were statistically significantly superior to placebo and the 6 mg to 12 mg per day range was significantly superior to the 1 mg to 4 mg per day range. Figure 1: Time-course of the Change from Baseline in ADAS-cog Score for Patients Completing 26 Weeks of Treatment in Study 1
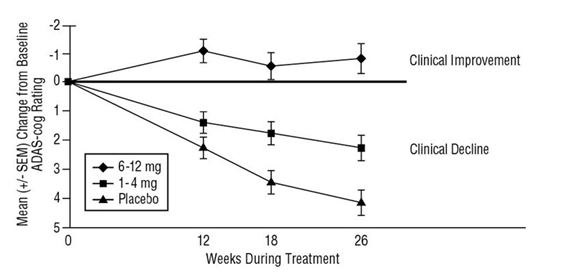
Figure 2 illustrates the cumulative percentages of patients from each of the 3 treatment groups who had attained at least the measure of improvement in ADAS-cog score shown on the x-axis. Three change scores, (7-point and 4-point reductions from baseline or no change in score) have been identified for illustrative purposes, and the percent of patients in each group achieving that result is shown in the inset table.
The curves demonstrate that both patients assigned to rivastigmine tartrate and placebo have a wide range of responses, but that the rivastigmine tartrate groups are more likely to show the greater improvements. A curve for an effective treatment would be shifted to the left of the curve for placebo, while an ineffective or deleterious treatment would be superimposed upon, or shifted to the right of the curve for placebo, respectively. Figure 2: Cumulative Percentage of Patients Completing 26 Weeks of Double-blind Treatment with Specified Changes from Baseline ADAS-cog Scores. The Percentages of Randomized Patients who Completed the Study were: Placebo 84 %, 1 mg-4 mg 85%, and 6 mg-12 mg 65%.
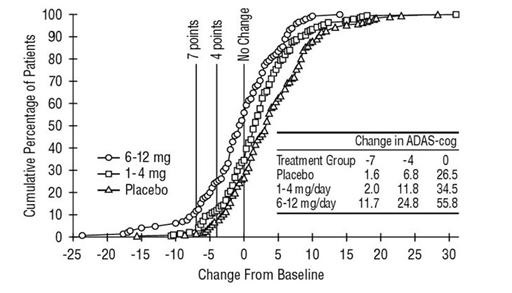
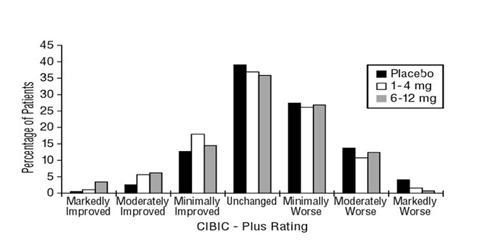
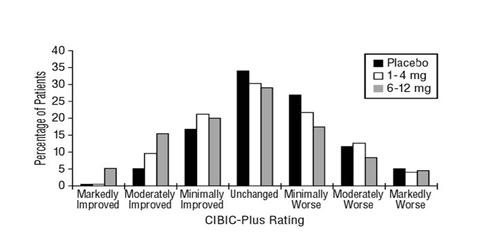
Figure 3 is a histogram of the frequency distribution of CIBIC-Plus scores attained by patients assigned to each of the 3 treatment groups who completed 26 weeks of treatment. The mean rivastigmine tartrate-placebo differences for these groups of patients in the mean rating of change from baseline were 0.32 units and 0.35 units for 1 mg to 4 mg and 6 mg to 12 mg of rivastigmine tartrate, respectively. The mean ratings for the 6 mg to 12 mg per day and 1 mg to 4 mg per day groups were statistically significantly superior to placebo. The differences between the 6 mg to 12 mg per day and the 1 mg to 4 mg per day groups were statistically significant.
Figure 3: Frequency Distribution of CIBIC-Plus Scores at Week 26 in Study 1  
 
Global 26-Week Study in Mild-to-Moderate Alzheimer's Disease (Study 2)
In a second study of 26 weeks duration, 725 patients were randomized to either a dose range of 1 mg to 4 mg or 6 mg to 12 mg of rivastigmine tartrate per day or to placebo, each given in divided doses. The 26-week study was divided into a 12-week forced-dose titration phase and a 14-week maintenance phase. The patients in the active treatment arms of the study were maintained at their highest tolerated dose within the respective range.  
Figure 4 illustrates the time course for the change from baseline in ADAS-cog scores for all 3 dose groups over the 26 weeks of the study. At 26 weeks of treatment, the mean differences in the ADAS-cog change scores for the rivastigmine tartrate-treated patients compared to the patients on placebo were 0.2 and 2.6 units for the 1 mg to 4 mg and 6 mg to 12 mg treatments, respectively. The 6 mg to 12 mg per day group was statistically significantly superior to placebo, as well as to the 1 mg to 4 mg per day group. The difference between the 1 mg to 4 mg per day group and placebo was not statistically significant. Figure 4: Time-course of the Change from Baseline in ADAS-cog Score for Patients Completing 26 Weeks of Treatment
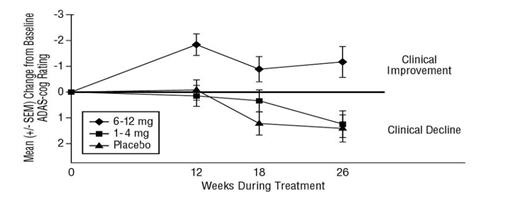
Figure 5 illustrates the cumulative percentages of patients from each of the 3 treatment groups who had attained at least the measure of improvement in ADAS-cog score shown on the x-axis. Similar to the U.S. 26-week study, the curves demonstrate that both patients assigned to rivastigmine tartrate and placebo have a wide range of responses, but that the 6 mg to 12 mg per day rivastigmine tartrate group is more likely to show the greater improvements. Figure 5: Cumulative Percentage of Patients Completing 26 Weeks of Double-blind Treatment with Specified Changes from Baseline ADAS-cog Scores. The Percentages of Randomized Patients who Completed the Study were: Placebo 87%, 1 mg-4 mg 86%, and 6 mg-12 mg 67%.
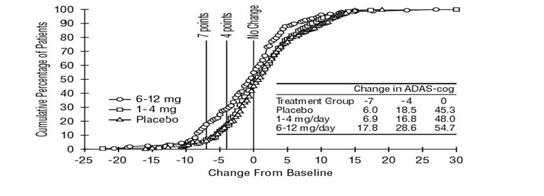
Figure 6 is a histogram of the frequency distribution of CIBIC-Plus scores attained by patients assigned to each of the 3 treatment groups who completed 26 weeks of treatment. The mean rivastigmine tartrate-placebo differences for these groups of patients for the mean rating of change from baseline were 0.14 units and 0.41 units for 1 mg to 4 mg and 6 mg to 12 mg of rivastigmine tartrate, respectively. The mean ratings for the 6 mg to 12 mg per day group were statistically significantly superior to placebo. The comparison of the mean ratings for the 1 mg to 4 mg per day group and placebo group was not statistically significant. Figure 6: Frequency Distribution of CIBIC-Plus Scores at Week 26 in Study 2
U.S. Fixed-Dose Study in Mild-to-Moderate Alzheimer's Disease (Study 3)
In a study of 26 weeks duration, 702 patients were randomized to doses of 3 mg, 6 mg, or 9 mg per day of rivastigmine tartrate or to placebo, each given in divided doses. The fixed-dose study design, which included a 12-week forced-dose titration phase and a 14-week maintenance phase, led to a high dropout rate in the 9 mg per day group because of poor tolerability. At 26 weeks of treatment, significant differences were observed for the ADAS-cog mean change from baseline for the 9 mg per day and 6 mg per day groups, compared to placebo. No significant differences were observed between any of the rivastigmine tartrate-dose groups and placebo for the analysis of the CIBIC-Plus mean rating of change. Although no significant differences were observed between rivastigmine tartrate treatment groups, there was a trend toward numerical superiority with higher doses.
Mild-to-Moderate Parkinsons Disease Dementia
International 24-Week Study (Study 4)
The effectiveness of rivastigmine tartrate as a treatment for dementia associated with¬†Parkinson's disease is demonstrated by the results of 1 randomized, double-blind, placebo-controlled clinical investigation in patients with mild-to-moderate dementia, with onset at least 2 years after the initial diagnosis of idiopathic¬†Parkinson's disease. The diagnosis of idiopathic¬†Parkinson's disease was based on the United Kingdom¬†Parkinson's Disease Society Brain Bank clinical criteria. The diagnosis of dementia was based on the criteria stipulated under the DSM-IV category ‚ÄúDementia Due To Other General Medical Condition‚ÄĚ (code 294.1x), but patients were not required to have a distinctive pattern of cognitive deficits as part of the dementia. Alternate causes of dementia were excluded by clinical history, physical and neurological examination, brain imaging, and relevant blood tests. Patients enrolled in the study had a MMSE score greater than or equal to 10 and less than or equal to 24 at entry. The mean age of patients participating in this trial was 72.7 years with a range of 50‚Äď91 years. Approximately, 35.1% of patients were women and 64.9% of patients were men. The racial distribution was 99.6% Caucasian and other races 0.4%.
This study used a dual outcome assessment strategy to evaluate the effectiveness of rivastigmine tartrate.
The ability of rivastigmine tartrate to improve cognitive performance was assessed with the ADAS-cog.
The ability of rivastigmine tartrate to produce an overall clinical effect was assessed using the Alzheimer's Disease Cooperative Study ‚Äď Clinician‚Äôs Global Impression of Change (ADCS-CGIC). The ADCS-CGIC is a more standardized form of CIBIC-Plus and is also scored as a 7-point categorical rating, ranging from a score of 1, indicating "markedly improved," to a score of 4, indicating "no change" to a score of 7, indicating "marked worsening".
In this study, 541 patients were randomized to a dose range of 3 mg to 12 mg of rivastigmine tartrate per day or to placebo in a ratio of 2:1, given in divided doses. The 24-week study was divided into a 16-week titration phase and an 8-week maintenance phase. The patients in the active treatment arm of the study were maintained at their highest tolerated dose within the specified dose range.
Figure 7 illustrates the time course for the change from baseline in ADAS-cog scores for both treatment groups over the 24-week study. At 24 weeks of treatment, the mean difference in the ADAS-cog change scores for the rivastigmine tartrate-treated patients compared to the patients on placebo was 3.8 points. This treatment difference was statistically significant in favor of rivastigmine tartrate when compared to placebo. Figure 7: Time Course of the Change from Baseline in ADAS-cog Score for Patients Completing 24 Weeks of Treatment in Study 4
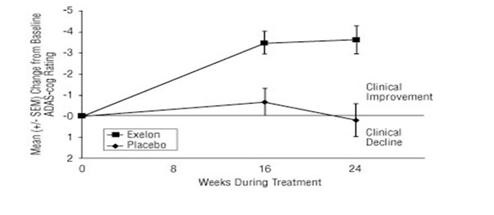
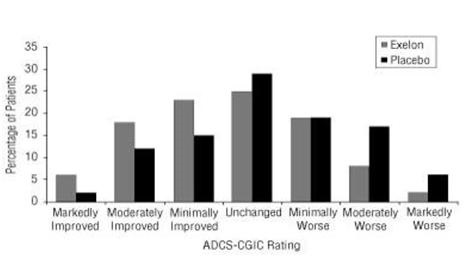
Figure 8 is a histogram of the distribution of patients' scores on the ADCS-CGIC (Alzheimer's Disease Cooperative Study - Clinician's Global Impression of Change) at 24 weeks. The mean difference in change scores between the rivastigmine tartrate and placebo groups from baseline was 0.5 points. This difference was statistically significant in favor of rivastigmine tartrate treatment.
Figure 8: Distribution of ADCS-CGIC Scores for Patients Completing 24 Weeks of Treatment in Study 4
Patients' age, gender, or race did not predict clinical outcome of rivastigmine tartrate treatment.
16 How Supplied/storage And Handling
Rivastigmine tartrate capsules
Rivastigmine tartrate capsules, USP equivalent to 1.5 mg, 3 mg, 4.5 mg, or 6 mg of rivastigmine base are available as follows:
1.5 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with yellow opaque color cap and yellow opaque color body imprinted "C 91".
 Bottles of 60                                       NDC 71209-012-03
 Bottles of 500                                     NDC 71209-012-10
3 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with orange opaque color cap and orange opaque color body imprinted "C 92".
Bottles of 60                                        NDC 71209-013-03
Bottles of 500                                      NDC 71209-013-10
4.5 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with red opaque color cap and red opaque color body imprinted "C 93".
Bottles of 60                                        NDC 71209-014-03
Bottles of 500                                      NDC 71209-014-10
6 mg capsule - white to off white powder filled in size "2" hard gelatin capsules with red opaque color cap and orange opaque color body imprinted "C 94".
Bottles of 60                                       NDC 71209-015-03
Bottles of 500                                     NDC 71209-015-10
Store at 25¬įC (77¬įF); excursions permitted to 15¬įC to 30¬įC (59¬įF to 86¬įF) [see USP Controlled Room Temperature]. Store in a tight container.
17 Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Instructions for Use).
Gastrointestinal Adverse Reactions
Caregivers should be advised of the high incidence of nausea and vomiting associated with the use of the drug along with the possibility of anorexia and weight loss. Caregivers should be encouraged to monitor for these adverse events and inform the physician if they occur. It is critical to inform caregivers that if therapy has been interrupted for more than several days, the next dose should not be administered until they have discussed this with the physician [see Warnings and Precautions (5.1)].
Skin Reactions
Caregivers and patients should be advised that allergic skin reactions have been reported in association with rivastigmine tartrate regardless of formulation (capsules, oral solution or transdermal patch). In case of skin reaction while taking rivastigmine tartrate, patients should consult with their physician immediately [ see Warnings and Precautions (5.2) ].
Concomitant Use of Drugs with Cholinergic Action
Caregivers and patients should be advised that cholinomimetics, including rivastigmine, may exacerbate or induce extrapyramidal symptoms. Worsening in patients with Parkinson's disease, including an increased incidence or intensity of tremor, has been observed [ see Warnings and Precautions (5.3) ].
Pregnancy
Advise patients to notify their healthcare provider if they are pregnant or plan to become pregnant.
Manufactured by:
Cadila Pharmaceuticals Limited
1389, Trasad Road,
Dholka ‚Äď 382225,
District - Ahmedabad, Gujarat, INDIA
Revised: January 2019
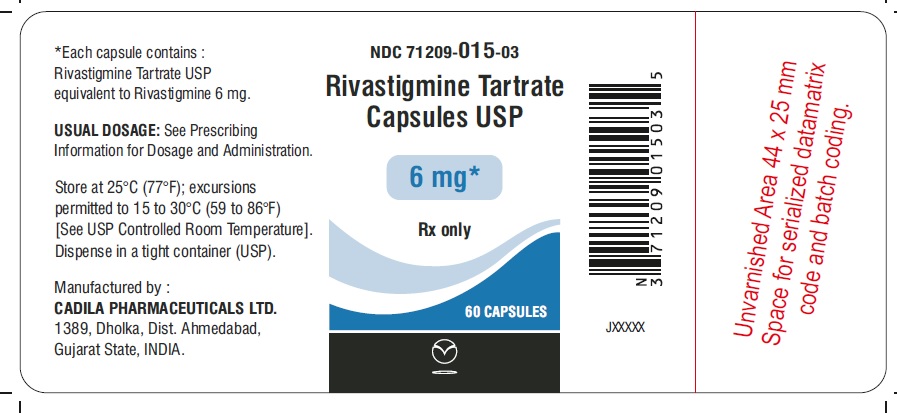
Package Label.principal Display Panel
Package Label ‚Äď 1.5 mg NDC 71209-012-03 Rivastigmine Tartrate Capsules USP 1.5 mg Rx Only 60 Capsules
Package Label.principal Display Panel
Package Label ‚Äď 3 mg NDC 71209-013-03 Rivastigmine Tartrate Capsules USP 3 mg Rx Only 60 Capsules
Package Label.principal Display Panel
Package Label ‚Äď 4.5 mg NDC 71209-014-03 Rivastigmine Tartrate Capsules USP 4.5 mg Rx Only 60 Capsules
Package Label.principal Display Panel
Package Label ‚Äď 6 mg NDC 71209-015-03 Rivastigmine Tartrate Capsules USP 6 mg¬† Rx Only 60 Capsules
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site


