Sotalol Hydrochloride (sotalol hydrochloride 80 mg) Dailymed
Generic: sotalol hydrochloride is used for the treatment of Asthma Atrial Fibrillation Atrial Flutter Bradycardia Heart Failure Hypokalemia Hypotension Long QT Syndrome Pulmonary Edema Shock, Cardiogenic Sick Sinus Syndrome Tachycardia, Supraventricular Ventricular Fibrillation Bronchial Hyperreactivity Tachycardia, Ventricular Renal Insufficiency Atrioventricular Block
Boxed Warning
Warning: Life Threatening Proarrhythmia
-
‚ÄĘ Sotalol can cause life threatening ventricular tachycardia associated with QT interval prolongation. -
‚ÄĘ If the QT interval prolongs to 500 msec or greater, reduce the dose, lengthen the dosing interval, or discontinue the drug. -
‚ÄĘ Initiate or reinitiate in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring. -
‚ÄĘ Adjust the dosing interval based on creatinine clearance.
Go PRO for all pill images
Warning: Life Threatening Proarrhythmia
To minimize the risk of drug-induced arrhythmia, initiate or reinitiate oral sotalol in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring.
Sotalol can cause life threatening ventricular tachycardia associated with QT interval prolongation.
If the QT interval prolongs to 500 msec or greater, reduce the dose, lengthen the dosing interval, or discontinue the drug.
Calculate creatinine clearance to determine appropriate dosing [see Dosage and Administration (2.5)].
WARNING: LIFE THREATENING PROARRHYTHMIA
See full prescribing information for complete boxed warning.
‚ÄĘ Sotalol can cause life threatening ventricular tachycardia associated with QT interval prolongation.‚ÄĘ If the QT interval prolongs to 500 msec or greater, reduce the dose, lengthen the dosing interval, or discontinue the drug.‚ÄĘ Initiate or reinitiate in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring.‚ÄĘ Adjust the dosing interval based on creatinine clearance.
1 Indications And Usage
Sotalol hydrochloride tablets are an antiarrhythmic indicated for:
‚ÄĘ the treatment of life threatening ventricular arrhythmias (1.1 )‚ÄĘ the maintenance of normal sinus rhythm in patients with atrial fibrillation or flutter (AFIB/AFL) (1.2 )
Limitations of Use
‚ÄĘ Avoid use in patients with asymptomatic ventricular premature contraction (1.1 )‚ÄĘ Avoid use in patients with minimally symptomatic or easily reversible AFIB/AFL (1.2 )1.1 Life-Threatening Ventricular Arrhythmias
Sotalol hydrochloride tablets are indicated for the treatment of life-threatening, documented ventricular arrhythmias, such as sustained ventricular tachycardia (VT).
Limitation of Use:
Sotalol hydrochloride tablets may not enhance survival in patients with ventricular arrhythmias. Because of the proarrhythmic effects of sotalol hydrochloride tablets, including a 1.5 to 2% rate of Torsade de Pointes (TdP) or new ventricular tachycardia/fibrillation (VT/VF) in patients with either non-sustained ventricular tachycardia (NSVT) or supraventricular arrhythmias (SVT), its use in patients with less severe arrhythmias, even if the patients are symptomatic, is generally not recommended. Avoid treatment of patients with asymptomatic ventricular premature contractions [see Warnings and Precautions (5.2)].
1.2 Delay in Recurrence of Atrial Fibrillation/Atrial Flutter (AFIB/AFL)
Sotalol hydrochloride tablets are indicated for the maintenance of normal sinus rhythm (delay in time to recurrence of AFIB/AFL) in patients with symptomatic AFIB/AFL who are currently in sinus rhythm.
Limitation of Use:
Because sotalol hydrochloride tablets can cause life-threatening ventricular arrhythmias, reserve its use for patients in whom AFIB/AFL is highly symptomatic. Patients with paroxysmal AFIB that is easily reversed (by Valsalva maneuver, for example) should usually not be given sotalol hydrochloride tablets.
2 Dosage And Administration
‚ÄĘ Sotalol hydrochloride tablets: Initial dosage in adults is 80 mg twice daily. Increase the dose as needed in increments of 80 mg/day, every 3 days to a maximum 320 mg total daily dose (2.2 )‚ÄĘ Pediatrics: Dosage depends on age (2.4 )2.1 General Safety Measures for Initiation of Oral Sotalol Therapy
Withdraw other antiarrhythmic therapy before starting sotalol hydrochloride tablets and monitor carefully for a minimum of 2 to 3 plasma half-lives if the patient's clinical condition permits [see Drug Interactions (7)].
Hospitalize patients initiated or re-initiated on sotalol for at least 3 days or until steady-state drug levels are achieved, in a facility that can provide cardiac resuscitation and continuous electrocardiographic monitoring. Initiate oral sotalol therapy in the presence of personnel trained in the management of serious arrhythmias. Perform a baseline ECG to determine the QT interval and measure and normalize serum potassium and magnesium levels before initiating therapy. Measure serum creatinine and calculate an estimated creatinine clearance in order to establish the appropriate dosing interval (insert cross ref to renal dosing). Continually monitor patients with each uptitration in dose, until they reach steady state. Determine QTc 2 to 4 hours after every dose.
Discharge patients on sotalol therapy from an in-patient setting with an adequate supply of sotalol to allow uninterrupted therapy until the patient can fill a sotalol prescription.
Advise patients who miss a dose to take the next dose at the usual time. Do not double the dose or shorten the dosing interval.
2.2 Adult Dose for Ventricular Arrhythmias
The recommended initial dose is 80 mg twice daily. This dose may be increased in increments of 80 mg per day every 3 days provided the QTc <500 msec [see Warnings and Precautions (5.1)]. Continually monitor patients until steady state blood levels are achieved. In most patients, a therapeutic response is obtained at a total daily dose of 160 to 320 mg/day, given in two or three divided doses (because of the long terminal elimination half-life of sotalol, dosing more than a two times a day is usually not necessary). Oral doses as high as 480 to 640 mg/day have been utilized in patients with refractory life-threatening arrhythmias.
2.3 Adult Dose for Prevention of Recurrence of AFIB/AFL
The recommended initial dose is 80 mg twice daily. This dose may be increased in increments of 80 mg per day every 3 days provided the QTc <500 msec [see Warnings and Precautions (5.1)]. Continually monitor patients until steady state blood levels are achieved. Most patients will have satisfactory response with 120 mg twice daily. Initiation of sotalol in patients with creatinine clearance < 40 ml/min or QTc >450 is contraindicated [see Contraindications (4)].
2.4 Pediatric Dose for Ventricular Arrhythmias or AFIB/AFL
Use the same precautionary measures for children as you would use for adults when initiating and re-initiating sotalol treatment.
For children aged about 2 years and older
For children aged about 2 years and older, with normal renal function, doses normalized for body surface area are appropriate for both initial and incremental dosing. Since the Class III potency in children is not very different from that in adults, reaching plasma concentrations that occur within the adult dose range is an appropriate guide [see Clinical Pharmacology (12.1, 12.3)].
From pediatric pharmacokinetic data the following is recommended:
For initiation of treatment, 30 mg/m2 three times a day (90 mg/m2 total daily dose) is approximately equivalent to the initial 160 mg total daily dose for adults. Subsequent titration to a maximum of 60 mg/m2 (approximately equivalent to the 360 mg total daily dose for adults) can then occur. Titration should be guided by clinical response, heart rate and QTc, with increased dosing being preferably carried out in-hospital. At least 36 hours should be allowed between dose increments to attain steady-state plasma concentrations of sotalol in patients with age-adjusted normal renal function.
For children aged about 2 years or younger
For children aged about 2 years or younger, the above pediatric dosage should be reduced by a factor that depends heavily upon age, as shown in the following graph, age plotted on a logarithmic scale in months.

For a child aged 20 months, the dosing suggested for children with normal renal function aged 2 years or greater should be multiplied by about 0.97; the initial starting dose would be (30 X 0.97)=29.1 mg/m2, administered three times daily. For a child aged 1 month, the starting dose should be multiplied by 0.68; the initial starting dose would be (30 X 0.68)=20 mg/m2, administered three times daily. For a child aged about 1 week, the initial starting dose should be multiplied by 0.3; the starting dose would be (30 X 0.3)=9 mg/m2. Use similar calculations for dose titration.
Since the half-life of sotalol decreases with decreasing age (below about 2 years), time to steady-state will also increase. Thus, in neonates the time to steady-state may be as long as a week or longer.
2.5 Dosage for Patients with Renal Impairment
Adults
Use of sotalol in any age group with decreased renal function should be at lower doses or increased intervals between doses. It will take much longer to reach steady-state with any dose and/or frequency of administration. Closely monitor heart rate and QTc.
Dose escalations in renal impairment should be done after administration of at least 5 doses at appropriate intervals (Table 1). Sotalol is partly removed by dialysis; specific advice is unavailable on dosing patients on dialysis.
The initial dose of 80 mg and subsequent doses should be administered at the intervals uled in Table 1 or Table 2.
Table 1: Dosing Intervals for treatment of Ventricular Arrhythmias in renal impairment
Creatinine Clearance mL/min
Dosing Interval (hours)
> 60
12
30 to 59
24
10 to 29
36 to 48
< 10
Dose should be individualized
Table 2: Dosing Intervals for treatment of AFIB/AFL in renal impairment
Creatinine Clearance mL/min
Dosing Interval (hours)
> 60
12
40 to 59
24
<40
Contraindicated
2.6 Preparation of Extemporaneous Oral Solution
Sotalol hydrochloride syrup 5 mg/mL can be compounded using Simple Syrup containing 0.1% sodium benzoate (Syrup, NF) as follows:
1. Measure 120 mL of Simple Syrup.2. Transfer the syrup to a 6-ounce amber plastic (polyethylene terephthalate [PET]) prescription bottle. An oversized bottle is used to allow for a headspace, so that there will be more effective mixing during shaking of the bottle.3. Add five (5) sotalol hydrochloride 120 mg tablets to the bottle. These tablets are added intact; it is not necessary to crush the tablets. The addition of the tablets can also be done first. The tablets can also be crushed if preferred. If the tablets are crushed, care should be taken to transfer the entire quantity of tablet powder into the bottle containing the syrup.4. Shake the bottle to wet the entire surface of the tablets. If the tablets have been crushed, shake the bottle until the endpoint is achieved.5. Allow the tablets to hydrate for at least two hours.6. After at least two hours have elapsed, shake the bottle intermittently over the course of at least another two hours until the tablets are completely disintegrated. The tablets can be allowed to hydrate overnight to simplify the disintegration process.
The endpoint is achieved when a dispersion of fine particles in the syrup is obtained.
This compounding procedure results in a solution containing 5 mg/mL of sotalol hydrochloride. The fine solid particles are the water-insoluble inactive ingredients of the tablets.
Stability studies indicate that the suspension is stable for three months when stored at 15¬įC to 30¬įC (59¬įF to 86¬įF) [see USP Controlled Room Temperature] and ambient humidity.
3 Dosage Forms And Strengths
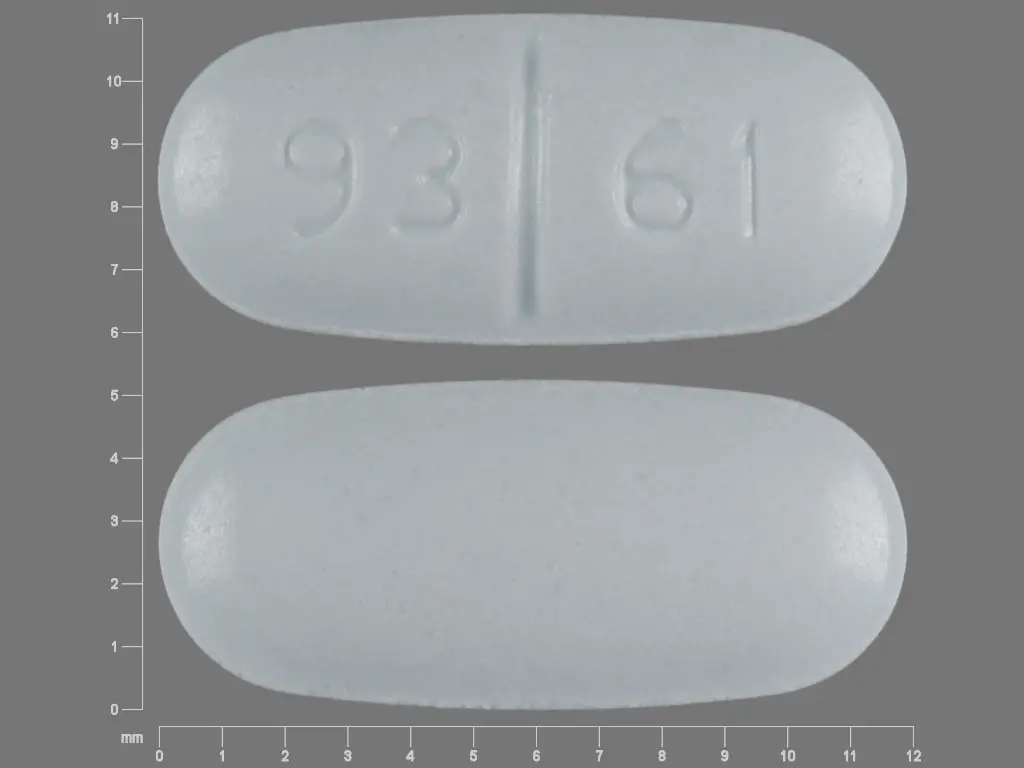
Sotalol hydrochloride tablets USP, 80 mg are available as light blue, oval-shaped tablets that are scored on one side and debossed with the numbers ‚Äú93‚ÄĚ and ‚Äú61‚ÄĚ on each side of the score, and plain on the other side.
Sotalol hydrochloride tablets USP, 120 mg are available as light blue, oval-shaped tablets that are scored on one side and debossed with the numbers ‚Äú93‚ÄĚ and ‚Äú1060‚ÄĚ on each side of the score, and plain on the other side.
Sotalol hydrochloride tablets USP, 160 mg are available as light blue, oval-shaped tablets that are scored on one side and debossed with the numbers ‚Äú93‚ÄĚ and ‚Äú62‚ÄĚ on each side of the score, and plain on the other side.
Sotalol hydrochloride tablets USP, 240 mg are available as light blue, oval-shaped tablets that are scored on one side and debossed with the numbers ‚Äú93‚ÄĚ and ‚Äú63‚ÄĚ on each side of the score, and plain on the other side.
80 mg, 120 mg, 160 mg, and 240 mg tablets (3 )
4 Contraindications
Sotalol hydrochloride tablets are contraindicated in patients with:
‚ÄĘ Sinus bradycardia, sick sinus syndrome, second and third degree AV block, unless a functioning pacemaker is present‚ÄĘ Congenital or acquired long QT syndromes‚ÄĘ Cardiogenic shock or decompensated heart failure‚ÄĘ Serum potassium <4 mEq/L‚ÄĘ Bronchial asthma or related bronchospastic conditions‚ÄĘ Hypersensitivity to sotalol
For the treatment of AFIB/AFL, sotalol hydrochloride tablets are also contraindicated in patients with:
‚ÄĘ Baseline QT interval >450 ms ‚ÄĘ Creatinine clearance <40 mL/min
For the treatment of AFIB/AFL or ventricular arrhythmias
‚ÄĘ Sinus bradycardia, 2nd or 3rd degree AV block, sick sinus syndrome (4 )‚ÄĘ Congenital or acquired long QT syndrome, (4 )‚ÄĘ Serum potassium <4 mEq/L (4 )‚ÄĘ Cardiogenic shock, decompensated heart failure (4 )‚ÄĘ Bronchial asthma or related bronchospastic conditions (4 )‚ÄĘ Hypersensitivity to sotalol (4 )
For the treatment of AFIB/AFL also contraindicated for:
‚ÄĘ QT interval >450 ms (4 )‚ÄĘ Creatine clearance <40 ml/min (4 )
5 Warnings And Precautions
‚ÄĘ QT prolongation, bradycardia, AV block, hypotension, worsening heart failure: Reduce dose or discontinue (5.1 )‚ÄĘ Acute exacerbation of coronary artery disease upon cessation of therapy: Do not abruptly discontinue (5.5 )‚ÄĘ Correct any electrolyte disturbances (5.1 )‚ÄĘ May mask symptoms of hypoglycemia or worsen hyperglycemia in diabetic patients; monitor (5.7 )5.1 QT Prolongation and Proarrhythmia
Sotalol hydrochloride can cause serious and potentially fatal ventricular arrhythmias such as sustained VT/VF, primarily Torsade de Pointes (TdP) type ventricular tachycardia, a polymorphic ventricular tachycardia associated with QT interval prolongation. Factors such as reduced creatinine clearance, female sex, higher doses, reduced heart rate and history of sustained VT/VF or heart failure increase the risk of TdP. The risk of TdP can be reduced by adjustment of the sotalol dose according to creatinine clearance and by monitoring the ECG for excessive increases in the QT interval [see Dosage and Administration (2.1)].
Correct hypokalemia or hypomagnesemia prior to initiating sotalol hydrochloride, as these conditions can exaggerate the degree of QT prolongation, and increase the potential for Torsade de Pointes. Special attention should be given to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or patients receiving concomitant diuretic drugs.
Proarrhythmic events must be anticipated not only on initiating therapy, but with every upward dose adjustment [see Dosage and Administration (2.1)].
In general, do not use sotalol with other drugs known to cause QT prolongation [see Drug Interactions (7.1)].
5.2 Bradycardia/Heart Block/Sick Sinus Syndrome
Sinus bradycardia (heart rate less than 50 bpm) occurred in 13% of patients receiving sotalol in clinical trials, and led to discontinuation in about 3% of patients. Bradycardia itself increases the risk of Torsade de Pointes. Sinus pause, sinus arrest and sinus node dysfunction occur in less than 1% of patients. The incidence of 2nd- or 3rd-degree AV block is approximately 1%.
Sotalol hydrochloride is contraindicated in patients with sick sinus syndrome because it may cause sinus bradycardia, sinus pauses or sinus arrest.
5.3 Hypotension
Sotalol produces significant reductions in both systolic and diastolic blood pressures and may result in hypotension. Monitor hemodynamics in patients with marginal cardiac compensation.
5.4 Heart Failure
New onset or worsening heart failure may occur during initiation or uptitration of sotalol because of its beta-blocking effects. Monitor for signs and symptoms of heart failure and discontinue treatment if symptoms occur.
5.5 Cardiac Ischemia after Abrupt Discontinuation
Following abrupt cessation of therapy with beta adrenergic blockers, exacerbations of angina pectoris and myocardial infarction may occur. When discontinuing chronically administered sotalol hydrochloride, particularly in patients with ischemic heart disease, gradually reduce the dosage over a period of 1 to 2 weeks, if possible, and monitor the patient. If angina markedly worsens or acute coronary ischemia develops, treat appropriately (consider use of an alternative beta blocker). Warn patients not to interrupt therapy without their physician’s advice. Because coronary artery disease may be common, but unrecognized, in patients treated with sotalol, abrupt discontinuation may unmask latent coronary insufficiency.
5.6 Bronchospasm
Patients with bronchospastic diseases (for example chronic bronchitis and emphysema) should not receive beta-blockers. If sotalol hydrochloride is to be administered, use the smallest effective dose, to minimize inhibition of bronchodilation produced by endogenous or exogenous catecholamine stimulation of beta 2 receptors.
5.7 Masked Signs of Hypoglycemia in Diabetics
Beta blockers may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected. Elevated blood glucose levels and increased insulin requirements can occur in diabetic patients.
5.8 Thyroid Abnormalities
Avoid abrupt withdrawal of beta-blockade in patients with thyroid disease because it may lead to an exacerbation of symptoms of hyperthyroidism, including thyroid storm. Beta-blockade may mask certain clinical signs (for example, tachycardia) of hyperthyroidism.
5.9 Anaphylaxis
While taking beta-blockers, patients with a history of anaphylactic reaction to a variety of allergens may have a more severe reaction on repeated challenge, either accidental, diagnostic or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat the allergic reaction.
5.10 Major Surgery
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery; however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
6 Adverse Reactions
The most common adverse reactions (‚Č•2%) for sotalol hydrochloride are: fatigue 4%, bradycardia (less than 50 bpm) 3%, dyspnea 3%, proarrhythmia 3%, asthenia 2%, and dizziness 2%. (6 )
To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-866-832-8537 or drug.safety@tevapharm.com; or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse reactions that are clearly related to sotalol are those which are typical of its Class II (beta-blocking) and Class III (cardiac action potential duration prolongation) effects and are dose related.
Ventricular Arrhythmias
Serious Adverse Reactions
In patients with a history of sustained ventricular tachycardia, the incidence of Torsade de Pointes during oral sotalol treatment was 4% and worsened VT was about 1%; in patients with other less serious ventricular arrhythmias the incidence of Torsade de Pointes was 1% and new or worsened VT was about 0.7%. Incidence of Torsade de Pointes arrhythmias in patients with VT/VF are shown in Table 3 below.
Table 3: Percent Incidence of Torsade de Pointes and Mean QTc Interval by Dose For Patients With Sustained VT/VF
Daily Dose (mg)
Torsade de Pointes Incidence
Mean QTchighest on-therapy value (msec)
80
0 (69)
463 (17)
160
0.5 (832)
467 (181)
320
1.6 (835)
473 (344)
480
4.4 (459)
483 (234)
640
3.7 (324)
490 (185)
>640
5.8 (103)
512 (62)
( ) Number of patients assessed
Table 4 below relates the incidence of Torsade de Pointes to on-therapy QTc and change in QTc from baseline in patients with ventricular arrhythmias. It should be noted, however, that the highest on-therapy QTc was in many cases the one obtained at the time of the Torsade de Pointes event, so that the table overstates the predictive value of a high QTc.
Table 4: Relationship Between QTc Interval Prolongation and Torsade de Pointes
On-Therapy QTc Interval (msec)
Incidence of Torsade de Pointes
Change from Baseline in QTc(msec)
Incidence of Torsade de Pointes
<500
1.3% (1787)
<65
1.6% (1516)
500 to 525
3.4% (236)
65 to 80
3.2% (158)
525 to 550
5.6% (125)
80 to 100
4.1% (146)
>550
10.8% (157)
100 to 130
5.2% (115)
>130
7.1% (99)
( ) Number of patients assessed
Table 5: Incidence (%) of Common Adverse Reactions (‚Č• 2% in the Placebo group and less frequent than in the sotalol hydrochloride groups) in a Placebo-controlled Parallel-group Comparison Study of Patients with Ventricular Ectopy
Body System/Adverse Reaction (Preferred Term)
Placebo
Sotalol hydrochloride Total Daily Dose
N = 37 (%)
320 mg N = 38 (%)
640 mg N = 39(%)
CARDIOVASCULAR
Chest Pain
5.4
7.9
15.4
Dyspnea
2.7
18.4
20.5
Palpitation
2.7
7.9
5.1
Vasodilation
2.7
0.0
5.1
NERVOUS SYSTEM
Asthenia
8.1
10.5
20.5
Dizziness
5.4
13.2
17.9
Fatigue
10.8
26.3
25.6
Headache
5.4
5.3
7.7
Lightheaded
8.1
15.8
5.1
Sleep Problem
2.7
2.6
7.7
RESPIRATORY
Upper Respiratory Tract Problem
2.7
2.6
12.8
SPECIAL SENSES
Visual Problem
2.7
5.3
0.0
The most common adverse reactions leading to discontinuation of sotalol hydrochloride in trials of patients with ventricular arrhythmias are: fatigue 4%, bradycardia (less than 50 bpm) 3%, dyspnea 3%, proarrhythmia 3%, asthenia 2%, and dizziness 2%. Incidence of discontinuation for these adverse reactions was dose related.
One case of peripheral neuropathy that resolved on discontinuation of sotalol hydrochloride and recurred when the patient was rechallenged with the drug was reported in an early dose tolerance study.
Pediatric Patients
In an unblinded multicenter trial of 25 pediatric patients with SVT and/or VT receiving daily doses of 30, 90 and 210 mg/m2 with dosing every 8 hours for a total of 9 doses, no Torsade de Pointes or other serious new arrhythmias were observed. One (1) patient, receiving 30 mg/m2 daily, was discontinued because of increased frequency of sinus pauses/bradycardia. Additional cardiovascular AEs were seen at the 90 and 210 mg/m2 daily dose levels. They included QT prolongation (2 patients), sinus pauses/bradycardia (1 patient), increased severity of atrial flutter and reported chest pain (1 patient). Values for QTc ‚Č• 525 msec were seen in 2 patients at the 210 mg/m2 daily dose level. Serious adverse events including death, Torsade de Pointes, other proarrhythmias, high-degree A-V blocks, and bradycardia have been reported in infants and/or children.
Atrial Fibrillation/Atrial Flutter
Placebo-controlled Clinical Trials
In a pooled clinical trial population consisting of 4 placebo-controlled studies with 275 patients with atrial fibrillation (AFIB)/atrial flutter (AFL) treated with 160 to 320 mg doses of sotalol hydrochloride (AF), the following adverse reactions presented in Table 6 occurred in at least 2% of placebo-treated patients and at a lesser rate than sotalol hydrochloride-treated patients. The data are presented by incidence of reactions in the sotalol hydrochloride (AF) and placebo groups by body system and daily dose.
Table 6: Incidence (%) of Common Adverse Reactions (‚Č• 2% in the Placebo group and less frequent than in the sotalol hydrochloride (AF) groups) in Four Placebo-controlled Studies of Patients with AFIB/AFL
Body System/Adverse Reaction (Preferred Term)
Placebo
Sotalol hydrochloride (AF) Total Daily Dose
N = 282 (%)
160 to 240 mg N = 153 (%)
> 240 to 320 mg N = 122 (%)
CARDIOVASCULAR
Bradycardia
2.5
13.1
12.3
GASTROINTESTINAL
Diarrhea
2.1
5.2
5.7
Nausea/Vomiting
5.3
7.8
5.7
Pain abdomen
2.5
3.9
2.5
GENERAL
Fatigue
8.5
19.6
18.9
Hyperhidrosis
3.2
5.2
4.9
Weakness
3.2
5.2
4.9
MUSCULOSKELETAL/CONNECTIVE TISSUE
Pain musculoskeletal
2.8
2.6
4.1
NERVOUS SYSTEM
Dizziness
12.4
16.3
13.1
Headache
5.3
3.3
11.5
RESPIRATORY
Cough
2.5
3.3
2.5
Dyspnea
7.4
9.2
9.8
Overall, discontinuation because of unacceptable adverse events was necessary in 17% of the patients, and occurred in 10% of patients less than two weeks after starting treatment. The most common adverse reactions leading to discontinuation of sotalol hydrochloride (AF) were: fatigue 4.6%, bradycardia 2.4%, proarrhythmia 2.2%, dyspnea 2%, and QT interval prolongation 1.4%.
6.2 Postmarketing Experience
The following adverse drug reactions have been identified during post-approval use of sotalol. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Voluntary reports since introduction include reports (less than one report per 10,000 patients) of: emotional lability, slightly clouded sensorium, incoordination, vertigo, paralysis, thrombocytopenia, eosinophilia, leukopenia, photosensitivity reaction, fever, pulmonary edema, hyperlipidemia, myalgia, pruritis, alopecia.
7 Drug Interactions
‚ÄĘ Class I or III Antiarrhythmics or other drugs that prolong the QT interval: Avoid concomitant use (7.1 )‚ÄĘ Digoxin, calcium channel blocker: increased risk of bradycardia, hypotension, heart failure (7.2 )‚ÄĘ Dosage of insulin or antidiabetic drugs may need adjustment (7.5 )‚ÄĘ Aluminum or magnesium-based antacids reduce sotalol exposure (7.7 )7.1 Antiarrhythmics and other QT Prolonging Drugs
Sotalol has not been studied with other drugs that prolong the QT interval such as antiarrhythmics, some phenothiazines, tricyclic antidepressants, certain oral macrolides and certain quinolone antibiotics. Discontinue Class I or Class III antiarrhythmic agents for at least three half-lives prior to dosing with sotalol. Class Ia antiarrhythmic drugs, such as disopyramide, quinidine and procainamide and other Class III drugs (for example, amiodarone) are not recommended as concomitant therapy with sotalol hydrochloride, because of their potential to prolong refractoriness [see Warnings and Precautions (5.2)]. There is only limited experience with the concomitant use of Class Ib or Ic antiarrhythmics. Additive Class II effects would also be anticipated with the use of other beta-blocking agents concomitantly with sotalol hydrochloride.
7.2 Digoxin
Proarrhythmic events were more common in sotalol treated patients also receiving digoxin; it is not clear whether this represents an interaction or is related to the presence of CHF, a known risk factor for proarrhythmia, in the patients receiving digoxin. Both digitalis glycosides and beta-blockers slow atrioventricular conduction and decrease heart rate. Concomitant use can increase the risk of bradycardia.
7.3 Calcium-Channel Blocking Drugs
Sotalol and calcium-blocking drugs can be expected to have additive effects on atrioventricular conduction or ventricular function. Monitor such patients for evidence of bradycardia and hypotension.
7.4 Catecholamine-Depleting Agents
Concomitant use of catecholamine-depleting drugs, such as reserpine and guanethidine, with a beta-blocker may produce an excessive reduction of resting sympathetic nervous tone. Monitor such patients for evidence of hypotension and/or marked bradycardia which may produce syncope.
7.5 Insulin and Oral Antidiabetics
Hyperglycemia may occur, and the dosage of insulin or antidiabetic drugs may require adjustment [see Warnings and Precautions 5.7)].
7.6 Clonidine
Concomitant use with sotalol increases the risk of bradycardia. Because beta-blockers may potentiate the rebound hypertension sometimes observed after clonidine discontinuation, withdraw sotalol several days before the gradual withdrawal of clonidine to reduce the risk of rebound hypertension.
7.7 Antacids
Avoid administration of oral sotalol within 2 hours of antacids containing aluminum oxide and magnesium hydroxide.
8 Use In Specific Populations
8.1 Pregnancy
Pregnancy Category B
There are no adequate and well-controlled studies in pregnant women. Sotalol has been shown to cross the placenta, and is found in amniotic fluid. In animal studies there was no increase in congenital anomalies, but an increase in early resorptions occurred at sotalol doses 18 times the maximum recommended human dose (MRHD, based on surface area). Animal reproductive studies are not always predictive of human response.
Reproduction studies in rats and rabbits during organogenesis at 9 and 7 times the MRHD (based on surface area), respectively, did not reveal any teratogenic potential associated with sotalol. In rabbits, a dose of sotalol 6 times the MRHD produced a slight increase in fetal death as well as maternal toxicity. This effect did not occur at sotalol dose 3 times the MRHD. In rats a sotalol dose 18 times the MRHD increased the number of early resorptions, while a dose 2.5 times the MRHD, produced no increase in early resorptions.
8.3 Nursing Mothers
Sotalol is excreted in the milk of laboratory animals and has been reported to be present in human milk. Discontinue nursing on sotalol hydrochloride.
8.4 Pediatric Use
The safety and effectiveness of sotalol in children have not been established. However, the Class III electrophysiologic and beta-blocking effects, the pharmacokinetics, and the relationship between the effects (QTc interval and resting heart rate) and drug concentrations have been evaluated in children aged between 3 days and 12 years old [see Dosage and Administration (2.4) and Clinical Pharmacology (12.2)].
8.6 Renal Impairment
Sotalol is mainly eliminated via the kidneys. Dosing intervals should be adjusted based on creatinine clearance [see Dosage and Administration (2.5)].
10 Overdosage
Intentional or accidental overdosage with sotalol has resulted in death.
Symptoms and Treatment of Overdosage
The most common signs to be expected are bradycardia, congestive heart failure, hypotension, bronchospasm and hypoglycemia. In cases of massive intentional overdosage (2 to 16 grams) of sotalol the following clinical findings were seen: hypotension, bradycardia, cardiac asystole, prolongation of QT interval, Torsade de Pointes, ventricular tachycardia, and premature ventricular complexes. If overdosage occurs, therapy with sotalol should be discontinued and the patient observed closely. Because of the lack of protein binding, hemodialysis is useful for reducing sotalol plasma concentrations. Patients should be carefully observed until QT intervals are normalized and the heart rate returns to levels >50 bpm.
The occurrence of hypotension following an overdose may be associated with an initial slow drug elimination phase (half-life of 30 hours) thought to be due to a temporary reduction of renal function caused by the hypotension. In addition, if required, the following therapeutic measures are suggested:
Bradycardia or Cardiac Asystole: Atropine, another anticholinergic drug, a beta-adrenergic agonist or transvenous cardiac pacing.
Heart Block: (second and third degree) transvenous cardiac pacemaker.
Hypotension: (depending on associated factors) epinephrine rather than isoproterenol or norepinephrine may be useful.
Bronchospasm: Aminophylline or aerosol beta-2-receptor stimulant. Higher than normal doses of beta-2 receptor stimulants may be required.
Torsade de Pointes: DC cardioversion, transvenous cardiac pacing, epinephrine, magnesium sulfate.
11 Description
Sotalol hydrochloride tablets USP contains sotalol hydrochloride, USP an antiarrhythmic drug with Class II (beta-adrenoreceptor blocking) and Class III (cardiac action potential duration prolongation) properties Sotalol hydrochloride tablets USP are supplied as a light blue, oval-shaped tablet for oral administration. Sotalol hydrochloride, USP is a white, crystalline solid with a molecular weight of 308.8. It is hydrophilic, soluble in water, propylene glycol and ethanol, but is only slightly soluble in chloroform. Chemically, sotalol hydrochloride, USP is d,l-N-[4-[1-hydroxy-2-[(1-methylethyl) amino]ethyl]phenyl]methane-sulfonamide monohydrochloride. The molecular formula is C12H20N2O3 S‚ąôHCl and is represented by the following structural formula:

Sotalol hydrochloride tablets USP contain the following inactive ingredients: corn starch, lactose monohydrate, magnesium stearate, povidone, and FD&C Blue No. 2.
12 Clinical Pharmacology
12.1 Mechanism of Action
Sotalol has both beta-adrenoreceptor blocking (Vaughan Williams Class II) and cardiac action potential duration prolongation (Vaughan Williams Class III) antiarrhythmic properties. The two isomers of sotalol have similar Class III antiarrhythmic effects, while the l-isomer is responsible for virtually all of the beta-blocking activity. The beta-blocking effect of sotalol is non-cardioselective, half maximal at about 80 mg/day and maximal at doses between 320 and 640 mg/day. Sotalol does not have partial agonist or membrane stabilizing activity. Although significant beta-blockade occurs at oral doses as low as 25 mg, significant Class III effects are seen only at daily doses of 160 mg and above.
In children, a Class III electrophysiologic effect can be seen at daily doses of 210 mg/m2 body surface area (BSA). A reduction of the resting heart rate due to the beta-blocking effect of sotalol is observed at daily doses ‚Č• 90 mg/m2 in children.
12.2 Pharmacodynamics
Cardiac Electrophysiological Effects
Sotalol hydrochloride prolongs the plateau phase of the cardiac action potential in the isolated myocyte, as well as in isolated tissue preparations of ventricular or atrial muscle (Class III activity). In intact animals it slows heart rate, decreases AV nodal conduction and increases the refractory periods of atrial and ventricular muscle and conduction tissue.
In man, the Class II (beta-blockade) electrophysiological effects of sotalol are manifested by increased sinus cycle length (slowed heart rate), decreased AV nodal conduction and increased AV nodal refractoriness. The Class III electrophysiological effects in man include prolongation of the atrial and ventricular monophasic action potentials, and effective refractory period prolongation of atrial muscle, ventricular muscle, and atrio-ventricular accessory pathways (where present) in both the anterograde and retrograde directions. With oral doses of 160 to 640 mg/day, the surface ECG shows dose-related mean increases of 40 to 100 msec in QT and 10 to 40 msec in QTc [see Warnings and Precautions (5.1)]. No significant alteration in QRS interval is observed.
In a small study (n=25) of patients with implanted defibrillators treated concurrently with sotalol hydrochloride, the average defibrillatory threshold was 6 joules (range 2 to 15 joules) compared to a mean of 16 joules for a nonrandomized comparative group primarily receiving amiodarone.
Twenty-five children in an unblinded, multicenter trial with SVT and/or ventricular tachyarrhythmias, aged between 3 days and 12 years (mostly neonates and infants), received an ascending titration regimen with daily doses of 30, 90 and 210 mg/m2 with dosing every 8 hours for a total 9 doses. During steady-state, the respective average increases above baseline of the QTc interval were 2, 14, and 29 msec at the 3 dose levels. The respective mean maximum increases above baseline of the QTc interval were 23, 36, and 55 msec at the 3 dose levels. The steady-state percent increases in the RR interval were 3, 9 and 12%. The smallest children (BSA<0.33 m2) showed a tendency for larger Class III effects (őĒQTc) and an increased frequency of prolongations of the QTc interval as compared with larger children (BSA ‚Č•0.33 m2). The beta-blocking effects also tended to be greater in the smaller children (BSA <0.33 m2). Both the Class III and beta-blocking effects of sotalol were linearly related to the plasma concentrations.
Hemodynamics
In a study of systemic hemodynamic function measured invasively in 12 patients with a mean LV ejection fraction of 37% and ventricular tachycardia (9 sustained and 3 non-sustained), a median dose of 160 mg twice daily of sotalol hydrochloride produced a 28% reduction in heart rate and a 24% decrease in cardiac index at 2 hours post-dosing at steady-state. Concurrently, systemic vascular resistance and stroke volume showed nonsignificant increases of 25% and 8%, respectively. One patient was discontinued because of worsening congestive heart failure. Pulmonary capillary wedge pressure increased significantly from 6.4 mmHg to 11.8 mmHg in the 11 patients who completed the study. Mean arterial pressure, mean pulmonary artery pressure and stroke work index did not significantly change. Exercise and isoproterenol induced tachycardia are antagonized by sotalol hydrochloride, and total peripheral resistance increases by a small amount.
In hypertensive patients, sotalol produces significant reductions in both systolic and diastolic blood pressures. Although sotalol is usually well-tolerated hemodynamically, deterioration in cardiac performance may occur in patients with marginal cardiac compensation [see Warnings and Precautions (5.3)].
12.3 Pharmacokinetics
The pharmacokinetics of the d and l enantiomers of sotalol are essentially identical.
Absorption
In healthy subjects, the oral bioavailability of sotalol is 90 to 100%. After oral administration, peak plasma concentrations are reached in 2.5 to 4 hours, and steady-state plasma concentrations are attained within 2 to 3 days (that is, after 5 to 6 doses when administered twice daily). Over the dosage range 160 to 640 mg/day sotalol displays dose proportionality with respect to plasma concentrations. When administered with a standard meal, the absorption of sotalol was reduced by approximately 20% compared to administration in fasting state.
Distribution
Sotalol does not bind to plasma proteins. Distribution occurs to a central (plasma) and to a peripheral compartment. Sotalol crosses the blood brain barrier poorly.
Metabolism
Sotalol is not metabolized and is not expected to inhibit or induce any CYP450 enzymes.
Excretion
Excretion of sotalol is predominantly via the kidney in the unchanged form, and therefore lower doses are necessary in conditions of renal impairment [see Dosage and Administration (2.5)]. The mean elimination half-life of sotalol is 12 hours. Dosing every 12 hours results in trough plasma concentrations which are approximately one-half of those at peak.
Specific Populations
Pediatric: The combined analysis of a single-dose study and a multiple-dose study with 59 children, aged between 3 days and 12 years, showed the pharmacokinetics of sotalol to be first order. A daily dose of 30 mg/m2 of sotalol was administered in the single dose study and daily doses of 30, 90 and 210 mg/m2 were administered every 8 hours in the multi-dose study. After rapid absorption with peak levels occurring on average between 2 to 3 hours following administration, sotalol was eliminated with a mean half-life of 9.5 hours. Steady-state was reached after 1 to 2 days. The average peak to trough concentration ratio was 2. BSA was the most important covariate and more relevant than age for the pharmacokinetics of sotalol. The smallest children (BSA<0.33m2) exhibited a greater drug exposure (+59%) than the larger children who showed a uniform drug concentration profile. The intersubject variation for oral clearance was 22%.
Geriatric: Age does not significantly alter the pharmacokinetics of sotalol hydrochloride, but impaired renal function in geriatric patients can increase the terminal elimination half-life, resulting in increased drug accumulation.
Renal Impairment: Sotalol is mainly eliminated via the kidneys through glomerular filtration and to a small degree by tubular secretion. There is a direct relationship between renal function, as measured by serum creatinine or creatinine clearance, and the elimination rate of sotalol. The half-life of sotalol is prolonged (up to 69 hours) in anuric patients. Doses or dosing intervals should be adjusted based on creatinine clearance [see Dosage and Administration (2.5)].
Hepatic Impairment: Patients with hepatic impairment show no alteration in clearance of sotalol.
Drug-Drug Interactions:
Antacids: Administration of oral sotalol within 2 hours of antacids may result in a reduction in Cmax and AUC of 26% and 20%, respectively, and consequently in a 25% reduction in the bradycardic effect at rest. Administration of the antacid two hours after oral sotalol has no effect on the pharmacokinetics or pharmacodynamics of sotalol.
No pharmacokinetic interactions were observed with hydrochlorothiazide or warfarin.
13 Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of carcinogenic potential was observed in rats during a 24-month study at 137 to 275 mg/kg/day (approximately 30 times the maximum recommended human oral dose (MRHD) as mg/kg or 5 times the MRHD as mg/m2) or in mice, during a 24-month study at 4141 to 7122 mg/kg/day (approximately 450 to 750 times the MRHD as mg/kg or 36 to 63 times the MRHD as mg/m2).
Sotalol has not been evaluated in any specific assay of mutagenicity or clastogenicity.
No significant reduction in fertility occurred in rats at oral doses of 1000 mg/kg/day (approximately 100 times the MRHD as mg/kg or 18 times the MRHD as mg/m2) prior to mating, except for a small reduction in the number of offspring per litter.
Reproduction studies in rats and rabbits during organogenesis at 100 and 22 times the MRHD as mg/kg (9 and 7 times the MRHD as mg/m2), respectively, did not reveal any teratogenic potential associated with sotalol HCl. In rabbits, a high dose of sotalol HCl (160 mg/kg/day) at 16 times the MRHD as mg/kg (6 times the MRHD as mg/m2) produced a slight increase in fetal death, and maternal toxicity. Eight times the maximum dose (80 mg/kg/day or 3 times the MRHD as mg/m2) did not result in an increased incidence of fetal deaths. In rats, 1000 mg/kg/day sotalol HCl, 100 times the MRHD (18 times the MRHD as mg/m2), increased the number of early resorptions, while at 14 times the maximum dose (2.5 times the MRHD as mg/m2), no increase in early resorptions was noted. However, animal reproduction studies are not always predictive of human response.
14 Clinical Studies
14.1 Ventricular Arrhythmias
Sotalol hydrochloride has been studied in life-threatening and less severe arrhythmias. In patients with frequent premature ventricular complexes (VPC), sotalol hydrochloride was significantly superior to placebo in reducing VPCs, paired VPCs and non-sustained ventricular tachycardia (NSVT); the response was dose-related through 640 mg/day with 80 to 85% of patients having at least a 75% reduction of VPCs. Sotalol hydrochloride was also superior, at the doses evaluated, to propranolol (40 to 80 mg TID) and similar to quinidine (200 to 400 mg QID) in reducing VPCs. In patients with life-threatening arrhythmias [sustained ventricular tachycardia/fibrillation (VT/VF)], sotalol hydrochloride was studied acutely [by suppression of programmed electrical stimulation (PES) induced VT and by suppression of Holter monitor evidence of sustained VT] and, in acute responders, chronically.
In a double-blind, randomized comparison of sotalol hydrochloride and procainamide given intravenously (total of 2 mg/kg sotalol hydrochloride vs. 19 mg/kg of procainamide over 90 minutes), sotalol hydrochloride suppressed PES induction in 30% of patients vs. 20% for procainamide (p=0.2).
In a randomized clinical trial [Electrophysiologic Study Versus Electrocardiographic Monitoring (ESVEM) Trial] comparing choice of antiarrhythmic therapy by PES suppression vs. Holter monitor selection (in each case followed by treadmill exercise testing) in patients with a history of sustained VT/VF who were also inducible by PES, the effectiveness acutely and chronically of sotalol hydrochloride was compared with that of 6 other drugs (procainamide, quinidine, mexiletine, propafenone, imipramine and pirmenol). Overall response, limited to first randomized drug, was 39% for sotalol hydrochloride and 30% for the pooled other drugs. Acute response rate for first drug randomized using suppression of PES induction was 36% for sotalol hydrochloride vs. a mean of 13% for the other drugs. Using the Holter monitoring endpoint (complete suppression of sustained VT, 90% suppression of NSVT, 80% suppression of VPC pairs, and at least 70% suppression of VPCs), sotalol hydrochloride yielded 41% response vs. 45% for the other drugs combined. Among responders placed on long-term therapy identified acutely as effective (by either PES or Holter), sotalol hydrochloride, when compared to the pool of other drugs, had the lowest two-year mortality (13% vs. 22%), the lowest two-year VT recurrence rate (30% vs. 60%), and the lowest withdrawal rate (38% vs. about 75 to 80%). The most commonly used doses of sotalol hydrochloride in this trial were 320 to 480 mg/day (66% of patients), with 16% receiving 240 mg/day or less and 18% receiving 640 mg or more.
It cannot be determined, however, in the absence of a controlled comparison of sotalol hydrochloride vs. no pharmacologic treatment (for example, in patients with implanted defibrillators) whether sotalol hydrochloride response causes improved survival or identifies a population with a good prognosis.
Sotalol hydrochloride has not been shown to enhance survival in patients with ventricular arrhythmias.
14.2 Clinical Studies in Supra-ventricular Arrhythmias
Sotalol hydrochloride (AF) has been studied in patients with symptomatic AFIB/AFL in two principal studies, one in patients with primarily paroxysmal AFIB/AFL, the other in patients with primarily chronic AFIB.
In one study, a U.S. multicenter, randomized, placebo-controlled, double-blind, dose-response trial of patients with symptomatic primarily paroxysmal AFIB/AFL, three fixed dose levels of sotalol hydrochloride (AF) (80 mg, 120 mg and 160 mg) twice daily and placebo were compared in 253 patients. In patients with reduced creatinine clearance (40 to 60 mL/min) the same doses were given once daily. Patients were excluded for the following reasons: QT >450 msec; creatinine clearance <40 mL/min; intolerance to beta-blockers; bradycardia-tachycardia syndrome in the absence of an implanted pacemaker; AFIB/AFL was asymptomatic or was associated with syncope, embolic CVA or TIA; acute myocardial infarction within the previous 2 months; congestive heart failure; bronchial asthma or other contraindications to beta-blocker therapy; receiving potassium losing diuretics without potassium replacement or without concurrent use of ACE-inhibitors; uncorrected hypokalemia (serum potassium <3.5 meq/L) or hypomagnesemia (serum magnesium <1.5 meq/L); received chronic oral amiodarone therapy for >1 month within previous 12 weeks; congenital or acquired long QT syndromes; history of Torsade de Pointes with other antiarrhythmic agents which increase the duration of ventricular repolarization; sinus rate <50 bpm during waking hours; unstable angina pectoris; receiving treatment with other drugs that prolong the QT interval; and AFIB/AFL associated with the Wolff-Parkinson-White (WPW) syndrome. If the QT interval increased to ‚Č•520 msec (or JT ‚Č•430 msec if QRS >100 msec) the drug was discontinued. The patient population in this trial was 64% male, and the mean age was 62 years. No structural heart disease was present in 43% of the patients. Doses were administered once daily in 20% of the patients because of reduced creatinine clearance.
Sotalol hydrochloride (AF) was shown to prolong the time to the first symptomatic, ECG-documented recurrence of AFIB/AFL, as well as to reduce the risk of such recurrence at both 6 and 12 months. The 120 mg dose was more effective than 80 mg, but 160 mg did not appear to have an added benefit. Note that these doses were given twice or once daily, depending on renal function. The results are shown in Figure 2, Table 7 and Table 8.
Figure 2: Study 1 ‚Äď Time to First ECG-Documented Recurrence of Symptomatic AFIB/AFL Since Randomization

Table 7: Study 1 ‚Äď Patient Status at 12 Months
Placebo
Sotalol hydrochloride (AF) Dose
80 mg
120 mg
160 mg
Randomized
69
59
63
62
On treatment in NSR at 12 months without recurrenceSymptomatic AFIB/AFL
23%
22%
29%
23%
RecurrenceEfficacy endpoint of Study 1; study treatment stopped.
67%
58%
49%
42%
D/C for AEs
6%
12%
18%
29%
Note that columns do not add up to 100% due to discontinuations (D/C) for ‚Äúother‚ÄĚ reasons.
Table 8: Study 1 ‚Äď Median Time to Recurrence of Symptomatic AFIB/AFL and Relative Risk (vs. Placebo) at 12 Months
Placebo n=69
Sotalol hydrochloride (AF) Dose
80 mg n=59
120 mg n=63
160 mg n=62
P-value vs. placebo
0.325
0.018
0.029
Relative Risk (RR) to placebo
0.81
0.59
0.59
Median time to recurrence (days)
27
106
229
175
Discontinuation because of adverse events was dose related.
In a second multicenter, randomized, placebo-controlled, double-blind study of 6 months duration in 232 patients with chronic AFIB, sotalol hydrochloride (AF) was titrated over a dose range from 80 mg/day to 320 mg/day. The patient population of this trial was 70% male with a mean age of 65 years. Structural heart disease was present in 49% of the patients. All patients had chronic AFIB for >2 weeks but <1 year at entry with a mean duration of 4.1 months. Patients were excluded if they had significant electrolyte imbalance, QTc >460 msec, QRS >140 msec, any degree of AV block or functioning pacemaker, uncompensated cardiac failure, asthma, significant renal disease (estimated creatinine clearance <50 mL/min), heart rate <50 bpm, myocardial infarction or open heart surgery in past 2 months, unstable angina, infective endocarditis, active pericarditis or myocarditis, ‚Č• 3 DC cardioversions in the past, medications that prolonged QT interval, and previous amiodarone treatment. After successful cardioversion patients were randomized to receive placebo (n=114) or sotalol hydrochloride (AF) (n=118), at a starting dose of 80 mg twice daily. If the initial dose was not tolerated it was decreased to 80 mg once daily, but if it was tolerated it was increased to 160 mg twice daily. During the maintenance period 67% of treated patients received a dose of 160 mg twice daily, and the remainder received doses of 80 mg once daily (17%) and 80 mg twice daily (16%).
Tables 9 and 10 show the results of the trial. There was a longer time to ECG-documented recurrence of AFIB and a reduced risk of recurrence at 6 months compared to placebo.
Table 9: Study 2 ‚Äď Patient Status at 6 Months
Placebo n=114
Sotalol hydrochloride (AF) n=118
On treatment in NSR at 6 months without recurrenceSymptomatic or asymptomatic AFIB/AFL
29%
45%
RecurrenceEfficacy endpoint of Study 2; study treatment stopped.
67%
49%
D/C for AEs
3%
6%
Death
1%
Table 10: Study 2 ‚Äď Median Time to Recurrence of Symptomatic AFIB/AFL/Death and Relative Risk (vs. Placebo) at 6 Months
Placebo n=114
Sotalol hydrochloride (AF) n=118
P-value vs. placebo
0.002
Relative Risk (RR) to placebo
0.55
Median time to recurrence (days)
44
>180
Figure 3: Study 2 ‚Äď Time to First ECG-Documented Recurrence of Symptomatic AFIB/AFL/Death Since Randomization
14.3 Clinical Studies in Patients with Myocardial Infarction
In a large double-blind, placebo controlled secondary prevention (postinfarction) trial (n=1,456); sotalol hydrochloride was given as a non-titrated initial dose of 320 mg once daily. Sotalol hydrochloride did not produce a significant increase in survival (7.3% mortality on sotalol hydrochloride vs. 8.9% on placebo, p=0.3), but overall did not suggest an adverse effect on survival. There was, however, a suggestion of an early (i.e., first 10 days) excess mortality (3% on sotalol hydrochloride vs. 2% on placebo).
In a second small trial (n=17 randomized to sotalol hydrochloride) where sotalol hydrochloride was administered at high doses (for example, 320 mg twice daily) to high-risk post-infarction patients (ejection fraction <40% and either >10 VPC/hr or VT on Holter), there were 4 fatalities and 3 serious hemodynamic/electrical adverse events within two weeks of initiating sotalol hydrochloride.
16 How Supplied/storage And Handling
Sotalol hydrochloride tablets USP, 80 mg are available as light blue, oval-shaped tablets that are scored on one side and debossed with the numbers ‚Äú93‚ÄĚ and ‚Äú61‚ÄĚ on each side of the score, and plain on the other side. They are available in bottles of 30 (NDC 71205-046-30), 60 (NDC 71205-046-60) and 90 (NDC 71205-046-90).
Store at 20¬į to 25¬įC (68¬į to 77¬įF) [See USP Controlled Room Temperature].
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
KEEP THIS AND ALL MEDICATIONS OUT OF THE REACH OF CHILDREN.
17 Patient Counseling Information
‚ÄĘ Advise patients to contact their healthcare provider in the event of syncope, pre-syncopal symptoms or cardiac palpitations.‚ÄĘ Advise patients that their electrolytes and ECG will be monitored during treatment [see Warnings and Precautions (5.1)].‚ÄĘ Advise patients to contact their healthcare provider in the event of conditions that could lead to electrolyte changes such as severe diarrhea, unusual sweating, vomiting, less appetite than normal or excessive thirst [see Warnings and Precautions (5.1)].‚ÄĘ Advise patients not to change the sotalol hydrochloride dose prescribed by their healthcare provider.‚ÄĘ Advise patients that they should not miss a dose, but if they do miss a dose they should not double the next dose to compensate for the missed dose: they should take the next dose at the regularly scheduled time [see Dosage and Administration (2)].‚ÄĘ Advise patients to not interrupt or discontinue sotalol hydrochloride without their physician‚Äôs advice, that they should get their prescription for sotalol filled and refilled on time so they do not interrupt treatment [see Dosage and Administration (2)].‚ÄĘ Advise patients to not start taking other medications without first discussing new medications with their healthcare provider.‚ÄĘ Advise patients that they should avoid taking sotalol hydrochloride within two hours of taking antacids that contain aluminum oxide or magnesium hydroxide [see Drug Interactions (7.7)].
All brand names uled are the registered trademarks of their respective owners and are not trademarks of Teva Pharmaceuticals USA.
Manufactured In Czech Republic By:
TEVA CZECH INDUSTRIES s.r.o.
Opava-Komarov, Czech Republic
Manufactured For:
TEVA PHARMACEUTICALS USA, INC.
North Wales, PA 19454
Rev. M 6/2016
Repackaged by:
Proficient Rx LP
Thousand Oaks, CA 91320
Package/label Display Panel

Sotalol Hydrochloride Tablets USP 80 mg 30s Label Text
NDC 71205-046-30
SOTALOL HYDROCHLORIDE Tablets USP 80 mg
Rx only
30 TABLETS
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site