Taclonex Scalp Dailymed
Generic: calcipotriene and betamethasone dipropionate is used for the treatment of Dermatitis, Atopic Facial Dermatoses Foot Dermatoses Hand Dermatoses Inflammation Leg Dermatoses Mycoses Pruritus Ani Psoriasis Scalp Dermatoses Dermatitis, Seborrheic Purpura, Thrombocytopenic, Idiopathic Hypercalcemia
Go PRO for all pill images
1 Indications And Usage
Enter section text here
Taclonex Scalp® Topical Suspension is a vitamin D analog and corticosteroid combination product indicated for the topical treatment of moderate to severe psoriasis vulgaris of the scalp in adults 18 years and older (1.1 )
Limitations of Use:
• Do not use on the face, axillae or groin (1.2 )
• Do no use if atrophy is present at the treatment site (1.2 )
1.1 Indication
Taclonex Scalp® Topical Suspension is indicated for the topical treatment of moderate to severe psoriasis vulgaris of the scalp in adults 18 years and older.
1.2 Limitations of Use
- Taclonex Scalp® Topical Suspension should not be used on the face, axillae or groin
- Taclonex Scalp® Topical Suspension should not be used if there is atrophy at the treatment site
2 Dosage And Administration
Enter section text here
Apply Taclonex Scalp® Topical Suspension to affected areas on the scalp once daily for 2 weeks or until cleared. Treatment may be continued for up to 8 weeks (2.1 ). The maximum weekly dose should not exceed 100 g (1.2 ). Shake before use (2 ).
Taclonex Scalp® Topical Suspension is not for oral, ophthalmic, or intravaginal use.
2.1 Usual Dosage and Administration
Apply Taclonex Scalp® Topical Suspension to affected areas on the scalp once daily for 2 weeks or until cleared. Treatment may be continued for up to 8 weeks. The maximum weekly dose should not exceed 100 g. Patients should shake the bottle prior to using the product. Patients should wash their hands after applying Taclonex Scalp® Topical Suspension.
Taclonex Scalp® Topical Suspension is not for oral, ophthalmic, or intravaginal use.
3 Dosage Forms And Strengths
Suspension.
Each gram of Taclonex Scalp® Topical Suspension contains 52.18 mcg of calcipotriene hydrate (equivalent to 50 mcg of calcipotriene) and 0.643 mg of betamethasone dipropionate (equivalent to 0.5 mg of betamethasone).
Suspension.
Each gram of Taclonex Scalp® Topical Suspension contains 52.18 mcg of calcipotriene hydrate (equivalent to 50 mcg of calcipotriene) and 0.643 mg of betamethasone dipropionate (equivalent to 0.5 mg of betamethasone) (3 )
4 Contraindications
None.
None (4 )
5 Warnings And Precautions
Enter section text here
- Hypercalcemia and hypercalciuria have been reported. If either occurs, discontinue until parameters of calcium metabolism normalize (
5.1 )- Topical corticosteroids can produce reversible HPA axis suppression, Cushing's syndrome and unmask latent diabetes (
5.2 )- Rate of adrenal suppression increased with treatment duration (
5.2 )- Systemic absorption may require evaluation for hypothalamic-pituitary-adrenal (HPA) axis suppression (
5.2 )- Modify use should HPA axis suppression develop (
5.2 )- Potent corticosteroids, use on large areas, prolonged use or occlusive use may increase systemic absorption (
5.1 )- Local adverse reactions may include atrophy, striae, irritation, acneiform eruptions, hypopigmentation, and allergic contact dermatitis and may be more likely with occlusive use or more potent corticosteroids (
5.3 ,6.1 )- Children may be more susceptible to systemic toxicity when treated with topical corticosteroids (
5.2 ,8.4 )5.1 Effects on Calcium Metabolism
Hypercalcemia and hypercalciuria have been observed with use of Taclonex Scalp® Topical Suspension. If hypercalcemia or hypercalciuria develop, treatment should be discontinued until parameters of calcium metabolism have normalized. The effects of Taclonex Scalp® Topical Suspension on calcium metabolism following treatment durations of more than 8 weeks have not been evaluated.
5.2 Effects on Endocrine System
Systemic absorption of topical corticosteroids can produce reversible hypothalamic-pituitary-adrenal (HPA) axis suppression with the potential for clinical glucocorticosteroid insufficiency. This may occur during treatment or upon withdrawal of the topical corticosteroid.
In a study of 32 subjects treated with Taclonex Scalp® Topical Suspension on the scalp and Taclonex® Ointment on the body, adrenal suppression was identified in 5 of 32 subjects (15.6%) after 4 weeks of treatment and in 2 of 11 subjects (18.2%) who continued treatment for 8 weeks. [See CLINICAL PHARMACOLOGY Pharmacodynamics (12.2)]
Because of the potential for systemic absorption, use of topical corticosteroids may require that patients be periodically evaluated for HPA axis suppression. Factors that predispose a patient using a topical corticosteroid to HPA axis suppression include the use of more potent steroids, use over large surface areas, use over prolonged periods, use under occlusion, use on an altered skin barrier, and use in patients with liver failure.
An ACTH stimulation test may be helpful in evaluating patients for HPA axis suppression. If HPA axis suppression is documented, an attempt should be made to gradually withdraw the drug, to reduce the frequency of application, or to substitute a less potent steroid. Manifestations of adrenal insufficiency may require supplemental systemic corticosteroids. Recovery of HPA axis function is generally prompt and complete upon discontinuation of topical corticosteroids.
Cushing’s syndrome, hyperglycemia, and unmasking of latent diabetes mellitus can also result from systemic absorption of topical corticosteroids.
Use of more than one corticosteroid-containing product at the same time may increase the total systemic corticosteroid exposure.
Pediatric patients may be more susceptible to systemic toxicity from use of topical corticosteroids. [See Use in Specific Populations (8.4)]
5.3 Local Adverse Reactions with Topical Corticosteroids
Local adverse reactions may be more likely to occur with occlusive use, prolonged use or use of higher potency corticosteroids. Reactions may include atrophy, striae, telangiectasias, burning, itching, irritation, dryness, folliculitis, acneiform eruptions, hypopigmentation, perioral dermatitis, allergic contact dermatitis, secondary infection, and miliaria. Some local adverse reactions may be irreversible.
5.4 Allergic Contact Dermatitis with Topical Corticosteroids
Allergic contact dermatitis to any component of topical corticosteroids is usually diagnosed by a failure to heal rather than a clinical exacerbation. Clinical diagnosis of allergic contact dermatitis can be confirmed by patch testing.
5.5 Allergic Contact Dermatitis with Topical Calcipotriene
Allergic contact dermatitis has been observed with use of topical calcipotriene. Clinical diagnosis of allergic contact dermatitis can be confirmed by patch testing.
5.6 Concomitant Skin Infections
Concomitant skin infections should be treated with an appropriate antimicrobial agent. If the infection persists, Taclonex Scalp® Topical Suspension should be discontinued until the infection has been adequately treated.
5.7 Unevaluated Uses
The safety and efficacy of Taclonex Scalp® Topical Suspension in patients with known or suspected disorders of calcium metabolism have not been evaluated.
The safety and efficacy of Taclonex Scalp® Topical Suspension in patients with erythrodermic, exfoliative or pustular psoriasis have not been evaluated.
The safety and efficacy of Taclonex Scalp® Topical Suspension in patients with severe renal insufficiency or severe hepatic disorders have not been evaluated.
5.8 Eye Exposures
Avoid eye exposures. Taclonex Scalp® Topical Suspension may cause eye irritation.
5.9 Ultraviolet Light Exposures
Patients who apply Taclonex Scalp® Topical Suspension to exposed skin (e.g. a bald scalp) should avoid excessive exposure to either natural or artificial sunlight, including tanning booths, sun lamps, etc. Physicians may wish to limit or avoid use of phototherapy to the scalp in patients who use Taclonex Scalp® Topical Suspension.
6 Adverse Reactions
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The most common adverse reactions (≥ 1%) are folliculitis and burning sensation of skin (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact LEO Pharma Inc at Phone 1-8877-494-4536 or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch .
6.1 Clinical Studies Experience
The rates of adverse reactions given below were derived from randomized, multicenter, prospective vehicle- and/or active-controlled clinical studies in subjects with scalp psoriasis. Subjects applied study product once daily for 8 weeks, and the median weekly
dose was 12.6 g.
Adverse reactions that occurred in ≥ 1% of subjects treated with Taclonex Scalp® Topical Suspension and at a rate higher than in subjects treated with vehicle are presented in Table 1:
Table 1
Number and Percentage of Patients with Adverse Reactions in Scalp
Psoriasis Studies
(Events Reported by ≥ 1% of Subjects and for Which a Relationship is Possible)Taclonex Scalp ® Topical Suspension N=1,953
Betamethasone dipropionate in vehicle
N=1,214Calcipotriene in vehicle N=979
Vehicle
N=173Event # of subjects (%) Folliculitis 16 (1%) 12 (1%) 5 (1%) 0 (0%) Burning sensation of skin 13 (1%) 10 (1%) 29 (3%) 0 (0.0%)
Other less common reactions (less than 1% but more than 0.1%) were, in decreasing order of incidence: acne, exacerbation of psoriasis, eye irritation, and pustular rash.
In a 52-week study, adverse reactions that were reported by greater than 1% of subjects treated with Taclonex Scalp® Topical Suspension were pruritus (3.6%), psoriasis (2.4%), erythema (2.1%), skin irritation (1.4%), and folliculitis (1.2%). The effects of Taclonex Scalp® Topical Suspension on calcium metabolism and the HPA axis were not investigated in the 52-week study.
8 Use In Specific Populations
Enter section text here
8.1 Pregnancy
Teratogenic Effects: Pregnancy Category C
Animal reproduction studies have not been conducted with Taclonex Scalp® Topical Suspension. Taclonex Scalp® Topical Suspension contains calcipotriene that has been shown to be fetotoxic and betamethasone dipropionate that has been shown to be teratogenic in animals when given systemically. There are no adequate and well-controlled studies in pregnant women. Taclonex Scalp® Topical Suspension should be used during pregnancy only if the potential benefit to the patient justifies the potential risk to the fetus.
Teratogenicity studies with calcipotriene were performed by the oral route in rats and rabbits. In rabbits, increased maternal and fetal toxicity were noted at a dosage of 12 mcg/kg/day (144 mcg/m2/day); a dosage of 36 mcg/kg/day (432 mcg/m2/day) resulted in a significant increase in the incidence of incomplete ossification of the pubic bones and forelimb phalanges of fetuses. In a rat study, a dosage of 54 mcg/kg/day (324 mcg/m2/day) resulted in a significantly increased incidence of skeletal abnormalities (enlarged fontanelles and extra ribs). The enlarged fontanelles were most likely due to the effect of calcipotriene upon calcium metabolism. The estimated maternal and fetal no-adverse effect levels (NOAEL) in the rat (108 mcg/m2/day) and rabbit (48 mcg/m2/day) derived from oral studies are lower than the maximum topical dose of calcipotriene in man (460 mcg/m2/day).
Corticosteroids are generally teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Betamethasone dipropionate has been shown to be teratogenic in mice and rabbits when given by the subcutaneous route at doses of 156 mcg/kg (468 mcg/m2/day) and 2.5 mcg/kg (30 mcg/m2/day), respectively. Those dose levels are lower than the maximum topical dose in man (about 5,950 mcg/m2/day). The abnormalities observed included umbilical hernia, exencephaly and cleft palate.
Pregnant women were excluded from the clinical studies conducted with Taclonex Scalp® Topical Suspension.
8.3 Nursing Mothers
Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects.
It is not known whether topically administered calcipotriene or corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk.
Because many drugs are excreted in human milk, caution should be exercised when Taclonex Scalp® Topical Suspension is administered to a nursing woman.
8.4 Pediatric Use
Safety and effectiveness of the use of Taclonex Scalp® Topical Suspension in pediatric patients have not been studied. Because of a higher ratio of skin surface area to body mass, children under the age of 12 years may be at particular risk of systemic adverse effects when they are treated with topical corticosteroids. [See Warnings and Precautions (5.2)]
HPA axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in children receiving topical corticosteroids. Manifestations of adrenal suppression in children include low plasma cortisol levels and absence of response to ACTH stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
8.5 Geriatric Use
Of the total number of patients in the controlled clinical studies of Taclonex Scalp® Topical Suspension, 334 were 65 years or older, while 84 were 75 years or older.
No overall differences in safety or effectiveness of Taclonex Scalp® Topical Suspension were observed between these patients and younger patients. All other reported clinical experience has not identified any differences in response between elderly and younger
patients.
10 Overdosage
Taclonex Scalp® Topical Suspension can be absorbed in sufficient amounts to produce systemic effects [See WARNINGS AND PRECAUTIONS (5.1)].
11 Description
Taclonex Scalp® Topical Suspension contains calcipotriene hydrate and betamethasone dipropionate. It is intended for topical use on the scalp.
Calcipotriene hydrate is a synthetic vitamin D3 analogue.
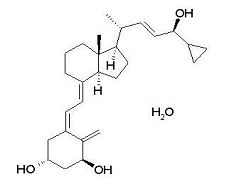
Chemically, calcipotriene hydrate is 9,10-Secochola-5,7,10(19),22- tetraene-1,3,24-triol,24-cyclo-propyl-, monohydrate, (1α,3ß,5Z,7E,22E,24S) with the empirical formula C27H40O3,H2O, a molecular weight of 430.6, and the following structural formula:
Calcipotriene hydrate is a white to almost white, crystalline compound.
Betamethasone dipropionate is a synthetic corticosteroid.
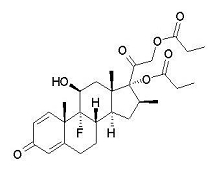
Betamethasone dipropionate has the chemical name Pregna-1,4- diene-3,20-dione-9-fluoro-11-hydroxy-16-methyl-17,21-bis(1-oxypropoxy)-(11Ăź,16Ăź), with the empirical formula C28H37FO7, a molecular weight of 504.6, and the following structural formula:
Betamethasone dipropionate is a white to almost white, crystalline powder.
Each gram of Taclonex Scalp® Topical Suspension contains 52.18 mcg of calcipotriene hydrate (equivalent to 50 mcg of calcipotriene) and 0.643 mg of betamethasone dipropionate (equivalent to 0.5 mg of betamethasone) in a base of hydrogenated castor oil, PPG-15 stearyl ether and mineral oil.
12 Clinical Pharmacology
Enter section text here
12.1 Mechanism of Action
Taclonex Scalp® Topical Suspension combines the pharmacological effects of calcipotriene hydrate as a synthetic vitamin D3 analogue and betamethasone dipropionate as a synthetic corticosteroid. However, while their pharmacologic and clinical effects are known, the exact mechanisms of their actions in psoriasis vulgaris are unknown.
12.2 Pharmacodynamics
Hypothalamic-Pituitary-Adrenal (HPA) Axis Suppression:
HPA axis suppression was evaluated in adult subjects (N=32) with extensive psoriasis involving at least 30% of the scalp and, in total, 15-30% of the body surface area. Treatment consisted of once daily application of Taclonex Scalp® Topical Suspension on the scalp in combination with Taclonex® Ointment on the body for 4 to 8 weeks. Adrenal suppression as indicated by a 30-minute post-stimulation cortisol level ≤ 18 mcg/dL was observed in 5 of 32 subjects (15.6%) after 4 weeks of treatment and in 2 of 11 subjects (18.2%) who continued treatment for 8 weeks.
Effects on Calcium Metabolism:
In the study described above, the effects of once daily application of Taclonex Scalp® Topical Suspension on the scalp in combination with Taclonex® Ointment on the body for 4 to 8 weeks on calcium metabolism were also examined. Following once daily application of Taclonex Scalp® Topical Suspension on the scalp in combination with Taclonex® Ointment on the body, elevated urinary calcium levels outside the normal range were observed in two subjects (one at 4 weeks and one at 8 weeks).
12.3 Pharmacokinetics
Absorption
Taclonex Scalp® Topical Suspension:
The systemic effect of Taclonex Scalp® Topical Suspension in extensive psoriasis was investigated in the study described above. In this study, the serum levels of calcipotriene and betamethasone dipropionate and their major metabolites were measured after 4 and 8 weeks of once daily application of Taclonex Scalp® Topical Suspension on the scalp in combination with Taclonex® Ointment on the body. Calcipotriene and betamethasone dipropionate were below the lower limit of quantification in all serum samples of the 34 subjects evaluated.
However, one major metabolite of calcipotriene (MC1080) was quantifiable in 10 of 34 (29.4%) subjects at week 4 and in five of 12 (41.7%) subjects at week 8. The major metabolite of betamethasone dipropionate, betamethasone 17-propionate (B17P) was also quantifiable in 19 of 34 (55.9%) subjects at week 4 and seven of 12 (58.3%) subjects at week 8. The serum concentrations for MC1080 ranged from 20-75 pg/mL. The clinical significance of this finding is unknown.
Metabolism
Calcipotriene:
Calcipotriene metabolism following systemic uptake is rapid and occurs in the liver. The primary metabolites of calcipotriene are less potent than the parent compound.
Calcipotriene is metabolized to MC1046 (the α,ß-unsaturated ketone analog of calcipotriene), which is metabolized further to MC1080 (a saturated ketone analog). MC1080 is the major metabolite in plasma. MC1080 is slowly metabolized to calcitroic acid.
Betamethasone dipropionate:
Betamethasone dipropionate is metabolized to betamethasone 17-propionate and betamethasone, including the 6Ăź-hydroxy derivatives of those compounds by hydrolysis. Betamethasone 17-propionate (B17P) is the primary metabolite.
13 Nonclinical Toxicology
Enter section text here
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
When calcipotriene was applied topically for up to 24 months at dosages of 3, 10 and 30 mcg/kg/day (corresponding to 9, 30 and 90 mcg/m2/day), no biologically significant changes in tumor incidence were observed when compared to control. In a study in which albino hairless mice were exposed to both ultra-violet radiation (UVR) and topically applied calcipotriene, a reduction in the time required for UVR to induce the formation of skin tumors was observed (statistically significant in males only), suggesting that calcipotriene may enhance the effect of UVR to induce skin tumors.
Long-term animal studies have not been performed to evaluate the carcinogenic potential of betamethasone dipropionate.
Calcipotriene did not elicit any genotoxic effects in the Ames mutagenicity assay, the mouse lymphoma TK locus assay, the human lymphocyte chromosome aberration test, or the mouse micronucleus test.
Betamethasone dipropionate did not elicit any genotoxic effect in the Ames mutagenicity assay, the mouse lymphoma TK locus assay, or in the rat micronucleus test.
Studies in rats at doses of up to 54 mcg/kg/day (324 mcg/m2/day) of calcipotriene indicated no impairment of fertility or general reproductive performance.
Studies in male rats at oral doses of up to 200 mcg/kg/day (1,200 mcg/m2/day), and in female rats at oral doses of up to 1,000 mcg/kg/day (6,000 mcg/m2/day) of betamethasone dipropionate indicated no impairment of fertility.
14 Clinical Studies
Enter section text here
14.1 Controlled Clinical Studies
Two multicenter, randomized, double-blind studies were conducted. In Study One, 1,407 subjects were randomized to one of four treatment groups: Taclonex Scalp® Topical Suspension, betamethasone dipropionate in the same vehicle, calcipotriene hydrate in the same vehicle, or the vehicle alone. Study Two did not include a vehicle arm; 1,280 subjects were randomized to one of three treatment groups: Taclonex Scalp® Topical Suspension, betamethasone dipropionate in the same vehicle, or calcipotriene hydrate in the same vehicle. Both studies enrolled subjects with moderate to very severe scalp psoriasis. The majority of subjects had disease of moderate severity at baseline. Subjects were treated once daily for 8 weeks.
Efficacy was assessed as the proportion of patients at Week 8 with absent or very mild disease according to an Investigator’s Global Assessment of Disease Severity. "Clear" was defined as no evidence of redness, thickness or scaling. "Almost clear" was defined as an overall clinical picture of lesions with the presence of minimal erythema. Table 2 contains the response rates in each of these two trials.
Table 2
Percentage of Patients with Clear or Almost Clear Disease
According to the Investigator’s Global Assessment of Disease Severity
Taclonex Scalp ®
Topical
SuspensionBetamethasone dipropionate in vehicle Calcipotriene in vehicle Vehicle
Study One
Week 2
(N = 494)
55.5%
(N = 531)
46.1%
(N = 256)
18.4%
(N = 126)
9.5%Week 8 70.0% 63.1% 36.7% 19.8%
Study Two
Week 2
(N = 512)
47.1%
(N = 517)
36.4%
(N = 251)
12.7%
-
-Week 8 67.2% 59.6% 41.0% -
16 How Supplied/storage And Handling
Enter section text here
16.1 How Supplied
Taclonex Scalp® Topical Suspension is available in bottles of:
60 g (NDC 54868-6091-0)
16.2 Storage
Store between 20-25°C (68-77°F); excursions permitted between 15-30°C (59-86°F).
Do not refrigerate. Keep the bottle in the outer carton when not in use.
The product should be used within three months after it has been opened.
16.3 Handling
Keep out of reach of children.
Shake before use.
Rx only.
17 Patient Counseling Information
This information is intended to aid in the safe and effective use of this medication. It is not a disclosure of all possible adverse or intended effects.
Patients using Taclonex Scalp® Topical Suspension should receive the following information and instructions.
17.1 Instructions for Use
This medication is to be used as directed by the physician. It is for external use only. Avoid contact with the face or eyes. As with any topical medication, patients should wash hands after application. This medication should not be used for any disorder other than that for which it has been prescribed. The treated skin area should not be bandaged or otherwise covered as to be occlusive, unless directed by the physician.
17.2 Adverse Reactions
Patients should report any signs of adverse reactions to their physician.
17.3 Concomitant Use of other Corticosteroids
Other products containing calcipotriene or a corticosteroid should not be used with Taclonex Scalp® Topical Suspension without first talking to the physician.
17.4 Excessive Exposure to Light
Patients who use Taclonex Scalp® Topical Suspension should avoid excessive exposure to either natural or artificial sunlight (including tanning booths, sun lamps, etc.). Physicians may wish to limit or avoid use of phototherapy in patients who use Taclonex Scalp® Topical Suspension.
Spl Patient Package Insert Section
PATIENT INFORMATION
Taclonex Scalp ® (pronounced TAK-lo-NEKS skalp)
(calcipotriene, 0.005% and betamethasone dipropionate, 0.064%)
Topical Suspension
Read the Patient Information that comes with Taclonex Scalp® Topical Suspension before you start using it and each time you refill your prescription. There may be new information. This leaflet does not take the place of talking with your doctor about your condition or treatment.
Important information: Taclonex Scalp® Topical Suspension is for use on the scalp only (topical use only). Do not use Taclonex Scalp® Topical Suspension on the face, under arms or on groin area. Do not swallow Taclonex Scalp ® Topical Suspension. Another product, Taclonex® Ointment contains the same medicine that is in Taclonex Scalp® Topical Suspension and is used to treat psoriasis vulgaris of the skin. If you use both medicines to treat your psoriasis vulgaris, be sure to follow your doctor’s directions carefully so that you do not use too much of one or both of these medicines.
What is Taclonex Scalp ® Topical Suspension?
Taclonex Scalp® Topical Suspension is a prescription medicine that is for use on the scalp only (a topical medicine). Taclonex Scalp® Topical Suspension is used to treat psoriasis vulgaris in adults 18 years of age and older. Taclonex Scalp® Topical Suspension is not recommended for use in children. Taclonex Scalp® Topical Suspension has not been studied in patients under the age of 18.
Who should not use Taclonex Scalp ® Topical Suspension?
Do not use Taclonex Scalp ® Topical Suspension if you:
- have a calcium metabolism disorder
- have one of the following types of psoriasis:
- erythrodermic psoriasis
- exfoliative psoriasis
- pustular psoriasis
- have severe kidney or liver disease.
What should I tell my doctor before using Taclonex Scalp ® Topical Suspension?
Tell your doctor about all of your health conditions, including if you:
- have a skin infection on your scalp. Your skin infection should be treated before you start using Taclonex Scalp® Topical Suspension
- have thin-skin (atrophy) at the site to be treated. You should not use Taclonex Scalp® Topical Suspension
- are getting phototherapy treatments (light therapy) for your psoriasis
- are pregnant or planning to become pregnant. It is not known if Taclonex Scalp® Topical Suspension can harm your unborn baby. You and your doctor will have to decide if Taclonex Scalp® Topical Suspension is right for you while pregnant
- are breastfeeding. It is not known if Taclonex Scalp® Topical Suspension passes into your milk and can harm your baby.
Tell your doctor about all the medicines you take, including prescription, and nonprescription medicines, vitamins and herbal supplements.
Taclonex Scalp® Topical Suspension and some other medicines may interact with each other. Especially tell your doctor if you use:
- other corticosteroid medicines
- other medicines for your psoriasis.
How should I use Taclonex Scalp ® Topical Suspension?
- Use Taclonex Scalp® Topical Suspension exactly as prescribed by your doctor.
- Do not use more than the maximum recommended weekly amount of 100 grams of Taclonex Scalp® Topical Suspension.
- Apply Taclonex Scalp® Topical Suspension to affected areas on the scalp once daily for 2 weeks or until cleared. Treatment may be continued for up to 8 weeks. Do not use Taclonex Scalp® Topical Suspension for more than 8 weeks unless prescribed by your doctor.
- Taclonex Scalp® Topical Suspension should only be used on the scalp. Do not use Taclonex Scalp® Topical Suspension on the face, under arms or on groin area. If you accidentally get Taclonex Scalp® Topical Suspension on your face or in your eyes wash the area with water right away.
- If you forget to use Taclonex Scalp® Topical Suspension, use it as soon as you remember. Then go on as before.
- Wash your hands well after using Taclonex Scalp® Topical Suspension.
- Do not wash your hair right after applying Taclonex Scalp® Topical Suspension. The medicine will not work as well to treat your psoriasis.
Using Taclonex Scalp ® Topical Suspension:
- Do not bandage or tightly cover or wrap the treated skin area.
- Do not apply Taclonex Scalp® Topical Suspension in the 12 hours before or after any chemical treatments to your hair. Since hair treatments may involve strong chemicals, talk with your doctor first.
- Shake the bottle before use.
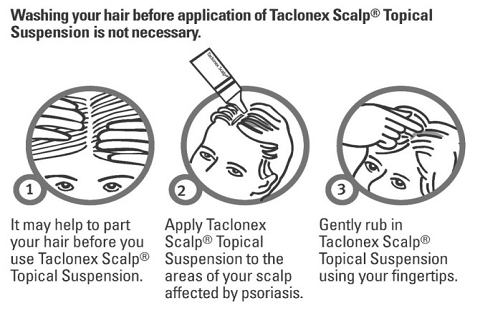
Remove the cap and apply Taclonex Scalp® Topical Suspension one time each day to the areas of your scalp affected by psoriasis, using the following steps (See the figures below).
What should I avoid while using Taclonex Scalp ® Topical Suspension?
Avoid spending a long time in sunlight. Avoid tanning booths and sun lamps. Use sunscreen and wear a hat if you have to be in sunlight. Talk to your doctor if you get a sunburn.
What are the possible side effects of Taclonex Scalp ® Topical Suspension?
Taclonex Scalp ® Topical Suspension may cause serious side effects.
Serious side effects are more likely to happen if you use too much Taclonex Scalp® Topical Suspension, use it for too long, or use it with other topical medicines that contain corticosteroids, calcipotriene, or certain other ingredients. Check with your health care professional before using other topical medicines. Taclonex Scalp® Topical Suspension can pass through your skin and be absorbed into the body.
Serious side effects may include:
- too much calcium in your blood
- adrenal gland problems
Your doctor may do special blood and urine tests to check your calcium levels and adrenal gland function while you are using Taclonex Scalp® Topical Suspension.
Other side effects include:
- itching
- inflamed hair pores (folliculitis)
- skin pain or irritation
- skin burning
- redness of the skin
- worsening of psoriasis
Call your doctor about any side effect that bothers you or that does not go away.
These are not all of the side effects with Taclonex Scalp® Topical Suspension. Ask your doctor or pharmacist for more information.
How should I store Taclonex Scalp ® Topical Suspension?
- Store Taclonex Scalp® Topical Suspension between 68-77°F (20-25°C). Do not refrigerate.
- Keep the bottle in the carton when not in use.
- Taclonex Scalp® Topical Suspension has an expiration date (exp.) marked on the bottom of the bottle. Do not use the topical suspension after this date.
- Use Taclonex Scalp® Topical Suspension within three months after it has been opened. After three months, safely throw away the bottle with any leftover Taclonex Scalp® Topical Suspension. If you need to keep using Taclonex Scalp® Topical Suspension or begin using it again, use a new bottle.
- Keep Taclonex Scalp ® Topical Suspension and all medicines out of the reach of children.
General information about Taclonex Scalp ® Topical Suspension.
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use Taclonex Scalp® Topical Suspension for a condition for which it was not prescribed. Do not give your Taclonex Scalp® Topical Suspension to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about Taclonex Scalp® Topical Suspension. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about Taclonex Scalp® Topical Suspension that is written for health professionals. For more information, please visit www.taclonex.com or call 1-877-494-4536.
What are the ingredients in Taclonex Scalp ® Topical Suspension?
Active ingredients: calcipotriene hydrate, betamethasone dipropionate.
Inactive ingredients: hydrogenated castor oil, PPG-15 stearyl ether and mineral oil.
Manufactured by:
LEO Pharmaceutical Products Ltd.,Ballerup, Denmark
LEO ®         Â Â
Distributed by:
LEO Pharma Inc.1 Sylvan Way, Parsippany, NJ 07054, USA1-877-494-4536
U.S. Patent Nos. RE39,706 E, 6,753,013 and 6,787,529.
024580-00
December 2009
Relabeling of "Additional Barcode" label by:
Physicians Total Care, Inc. Tulsa, Oklahoma   74146
Principal Display Panel
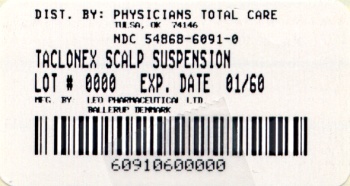
Rx only
TACLONEX SCALP® (calcipotriene 0.005% and betamethasone dipropionate 0.064%) Topical Suspension
For Topical Use Only
Net Wt. 60 g
Each gram contains 52.18 mcg of calcipotriene hydrate (equivalent to 50 mcg of calcipotriene) and 0.643 mg of betamethasone dipropionate (equivalent to 0.5 mg of betamethasone) in a base of hydrogenated castor oil, PPG-15 stearyl ether and mineral oil.
Store Taclonex Scalp® Topical Suspension between 20-25°C (68-77°F). Excursions permitted between 15-30°C (59-86°F). Do not refrigerate. Keep the bottle in the outer carton when not in use. Shake before use.
Discard product three months after opening.
Keep out of the reach of children.
Usual dosage: Apply once daily, or as directed by physician. See insert for complete information.Â
DISCLAIMER:
"This tool does not provide medical advice, and is for informational and educational purposes only, and is not a substitute for professional medical advice, treatment or diagnosis. Call your doctor to receive medical advice. If you think you may have a medical emergency, please dial 911."
"Do not rely on openFDA to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. We may limit or otherwise restrict your access to the API in line with our Terms of Service."
"This product uses publicly available data from the U.S. National Library of Medicine (NLM), National Institutes of Health, Department of Health and Human Services; NLM is not responsible for the product and does not endorse or recommend this or any other product."
PillSync may earn a commission via links on our site

